*NURSING > SHADOW HEALTH > NURSING MISC ANSWER KEY Sepsis-SKINNY Reasoning Urinary Tract Infection/Urosepsis (All)
NURSING MISC ANSWER KEY Sepsis-SKINNY Reasoning Urinary Tract Infection/Urosepsis
Document Content and Description Below
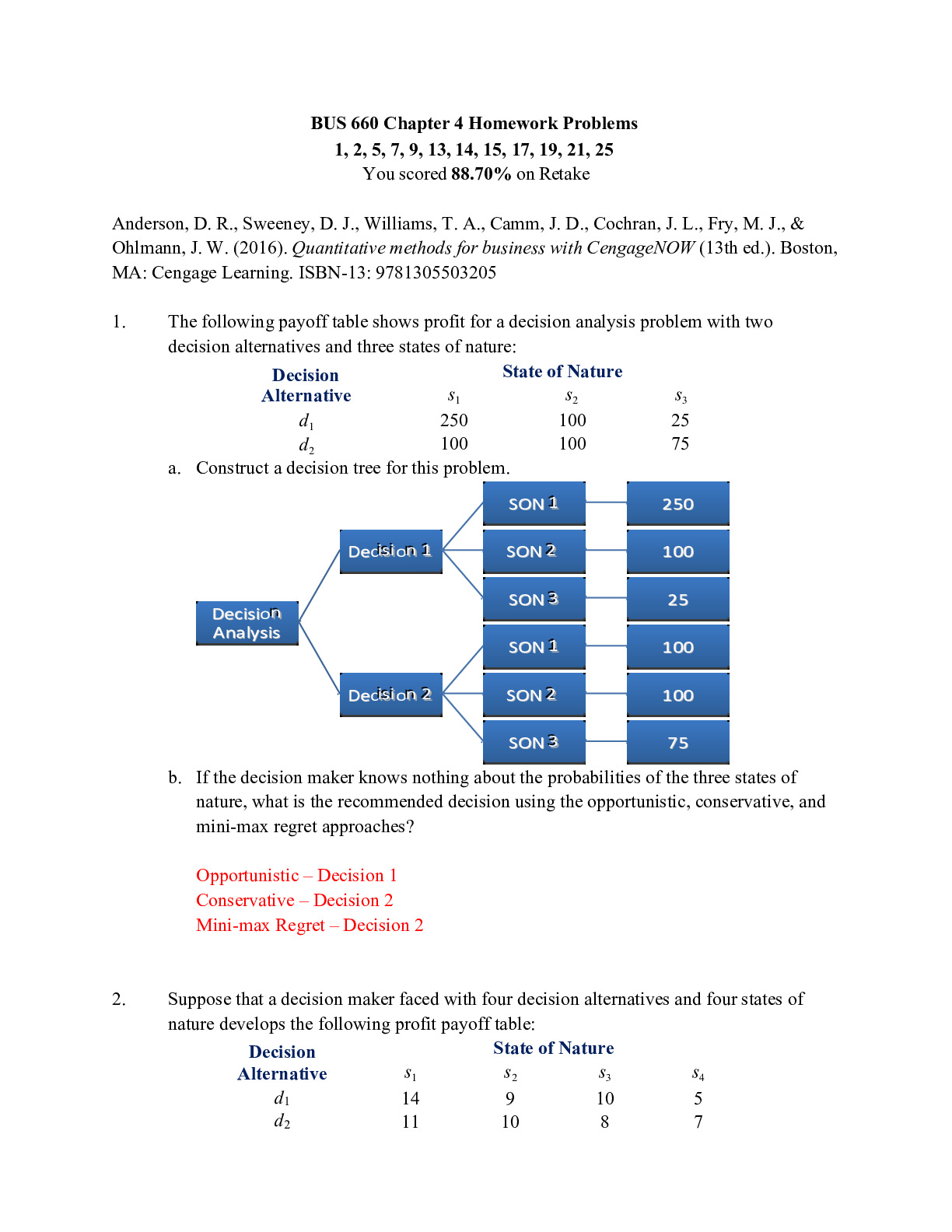
NURSING MISC ANSWER KEY Sepsis-SKINNY Reasoning Urinary Tract Infection/Urosepsis Urinary Tract Infection/Urosepsis SKINNY ReasoningJean Kelly, 82 years old Primary Concept Perfusion Interrelated... Concepts (In order of emphasis) • Infection • Clinical Judgment • Patient Education NCLEX Client Need Categories Percentage of Items from Each Category/Subcategory Covered in Case Study Safe and Effective Care Environment Management of Care 17-23% Safety and Infection Control 9-15% Health Promotion and Maintenance 6-12% Psychosocial Integrity 6-12% Physiological Integrity Basic Care and Comfort 6-12% Pharmacological and Parenteral Therapies 12-18% Reduction of Risk Potential 9-15% Physiological Adaptation 11-17% SKINNY Reasoning Part I: Recognizing RELEVANT Clinical Data History of Present Problem: Jean Kelly is an 82-year-old woman who has been feeling more fatigued the last three days and has had a fever the last twenty-four hours. She reports a painful, burning sensation when she urinates as well as frequency of urination the last week. Her daughter became concerned and brought her to the emergency department (ED) when she did not know what day it was. She is mentally alert with no history of confusion. While taking her bath today, she was weak and unable to get out of the tub and used her personal life alert button to call for medical assistance. Personal/Social History: Jean lives independently in a senior apartment retirement community. She is widowed and has two daughters who are active and involved in her life. What data from the histories are important and RELEVANT and have clinical significance for the nurse? RELEVANT Data from Present Problem: Clinical Significance: More fatigued for the last 3 days Fever the last 24 hours Though a general complaint, when clustered with the other symptoms of fever this is indicating that there is a likely PROBLEM present. Fever reflects the systemic inflammatory response initiated by the immune system and is there for a reason - to help the body fight off invading micro-organisms by increasing the production of neutrophils; the first responders of the immune system that are macrophages. The elevated temp also makes it less hospitable for bacteria to thrive and multiply.Painful, burning sensation when she urinates as well as frequency of urination the last week Did not know what day it was. She is mentally alert with no history of confusion While taking her bath today, she was weak and unable to get out of the tub and used the help button to call for medical assistance. These symptoms are classic with a urinary tract infection (UTI). Suspecting a urinary infection, the nurse needs to know that if a patient meets the SIRs criteria, they should suspect sepsis. With an infection of any kind, sepsis is identified by having 2 or more of the following criteria of Systemic Inflammatory Response Syndrome (SIRS): • Temp >100.4 or <96.8 • HR >90 • RR >20 • WBC >12,000 or <4000 • Bands >10% New onset of confusion is always a clinical RED FLAG in the elderly, and when CLUSTERED with other symptoms is not representing a neurologic problem, but is commonly seen with an infection such as a UTI. This confirms the weakness and fatigue she has had the past 3 days. It is severe weakness and a clinical RED FLAG if she is unable to get out of the bath tub and needed to call for assistance. RELEVANT Data from Social History: Clinical Significance: Jean lives independently in a senior apartment retirement community. She is widowed and has two daughters who are active and involved in her life. Is functioning at a high level for an 82-year-old woman and is independent at this time. It is important for the nurse to re-evaluate the functional status anytime there is a hospital admission to ensure safety. If there is ever a question, consult social services. Supportive family is a positive influence that will increase her ability to maintain current autonomy. Patient Care Begins: Current VS: P-Q-R-S-T Pain Assessment (5th VS): T: 101.8 F/38.8 C (oral) Provoking/Palliative: Nothing/Nothing P: 110 (regular) Quality: Ache R: 24 (regular) Region/Radiation: Right flank BP: 102/50 Severity: 5/10 O2 sat: 98% room air Timing: Continuous The nurse recognizes the need to validate his/her concern of fluid volume deficit and performs a set of orthostatic VS and obtains the following: Position: HR: BP: Supine 110 102/50 Standing 132 92/42 What VS data are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT VS Data: Clinical Significance:T: 101.8 F/38.8 C (oral) P: 110 reg. R: 24 BP : 102/50 MAP : 67 Right flank pain, continuous, 5/10 Ortho BPs: Supine: HR-110/BP-102/50 Standing: HR- 132/BP-92/42 With an infection of any kind, sepsis is identified by having 2 or more of the following criteria of Systemic Inflammatory Response Syndrome (SIRS): • Temp >100.4 or <96.8 • HR >90 • RR >20 • WBC >12,000 or <4000 • Bands >10% All three of these VS components meet systemic inflammatory response syndrome (SIRS) criteria. Therefore, the nurse must recognize that Jean is likely septic, and is at risk for progression to septic shock. This must be recognized by the nurse and is another clinical RED FLAG. Though this BP is technically within normal range, the nurse must recognize that it is in the LOW range of normal. When combined with what we know in this scenario regarding Jean’s fluid volume deficit and risk of sepsis, this warrants close observation and must be TRENDED closely. Jean also has a history of hypertension so this is probably “hypotension” for her. MAP is more important than the SBP and DBP because it gives the nurse a better clue as to organ perfusion. MAP >/=70 is goal. In this scenario with known dysuria, the presence of flank pain is clinically significant and must be recognized by the nurse. This is most likely due to pyelonephritis or the progression of the urinary infection in the lower tract, migrating to the kidneys. This makes her infection more serious and represents clinical progression of the infection in the urinary tract. Review abnormal orthostatic BP findings. An increase of 20 beats or more from lying baseline is by itself a POSITIVE finding and is usually seen in mild to moderate dehydration from my clinical experience. If a decrease in 20 points or more of mm/Hg in SBP is seen from lying to standing in addition to the increase in HR, this reflects moderate to severe fluid volume deficit/dehydration. Because she has both a drop of BP and increase in HR as well as being symptomatic, this confirms that you are seeing moderate to severe fluid volume depletion. Anticipate IV fluid resuscitation. *Remember that there are many physical exam findings that can be used to assess fluid volume status (i.e. dehydration). Other key assessment findings include: decreased urine output, dry mucus membranes, decreased skin turgor. Current Assessment: GENERAL APPEARANCE: Resting comfortably, appears in no acute distress RESP: Breath sounds clear with equal aeration bilaterally, nonlabored respiratory effortCARDIAC: Pink, warm and dry, no edema, heart sounds regular-S1S2, pulses strong, equal with palpation at radial/pedal/post-tibial landmarks NEURO: Alert and oriented x2-is not consistently oriented to date and place, c/o dizziness when she sits up GI: Abdomen soft/nontender, bowel sounds audible per auscultation in all four quadrants GU: Dysuria and frequency of urination persists, right flank tenderness to gentle palpation SKIN: Skin integrity intact, lips dry, oral mucosa tacky dry FYI: What assessment data is RELEVANT and must be recognized as clinically significant by the nurse? When sepsis initially presents, it is not uncommon to have a relatively normal physical assessment. Mrs. Kelly does not appear to be that sick. Because early recognition is crucial to prevent an adverse outcome, the VS data are especially relevant and indicate that Mrs. Kelly is already in sepsis/SIRS regardless of how benign her physical assessment may appear. What assessment data are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Assessment Data: Clinical Significance: NEUROLOGIC: Alert and oriented x2-is not consistently oriented to date and place c/o dizziness when she sits up GENITOURINARY: dysuria and frequency of urination persists, right flank tenderness to gentle palpation SKIN: Skin integrity intact, lips dry, oral mucosa tacky dry Orthostatic hypotension confirmed with BP measurements and her dizziness with position changes confirms this. She is not sure of the time/place which family reports is not her baseline and should be investigated further to be sure it is just part of the presentation of the UTI Consistent with UTI, flank tenderness and pain can possibly be indicative of kidney involvement/spread of infection beyond the urethra/bladder Dry mucous membranes is consistent with dehydration/fluid volume deficit Diagnostic Results: Basic Metabolic Panel (BMP) Na K Gluc. Creat. Current: 140 3.8 184 1.5 Most Recent: 138 3.9 128 1.1 Complete Blood Count (CBC) WBC HGB PLTs % Neuts Bands Current: 13.2 14.4 246 93 2 Most Recent: 8.8 144.6 140 68 1 MISC. Lactate Mg Current: 3.2 1.8 Most Recent: n/a 1.9 Urinalysis + UA Micro Color: Clarity: Sp. Gr. Protein Nitrite LET RBCs WBCs Bacteria EpithelialCurrent: Yellow Cloudy 1.032 2+ Pos Pos 1 >100 Large Few Most Recent: Yellow Clear 1.010 1+ Pos Pos 0 3 Few Few Radiology: Chest x-ray No infiltrates or other abnormalities. No changes from last previous. What data must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Physiologic Adaptation) RELEVANT Diagnostic Data: Clinical Significance: TREND: Improve/Worsening/Stable: Even if normal, because of their physiologic significance, the following labs must be noted as ALWAYS relevant by the nurse. Sodium: 140 Potassium: 3.8 • I consider Na+ the “Crystal-Light” electrolyte. Though this is simplistic, it does help to understand in principle how basic Na+ is to fluid balance • When you add one small packet of Crystal Light to your 16ounce bottle of water, the concentration is just right. This is where a normal Na+ will be (135-145) • Where free water goes, sodium will follow to a degree. Therefore if there is a fluid volume deficit due to dehydration, Na+ will typically be elevated because it’s concentrated (less water) • If there is fluid volume excess, Na+ will be diluted and will likely be low. It is the “foundational” fluid balance electrolyte! • Essential to normal cardiac electrical conduction, as is Mg+ • If too high or low can predispose to rhythm changes that can be life-threatening! STABLE STABLE Glucose: 184 Creatinine: 1.5 • K+ tends to deplete more quickly with loop diuretic usage than Mg+ • Required fuel for metabolism for every cell in the human body, especially the brain • Relevant to history of diabetes or stress hyperglycemia due to illness • Elevated levels post-op can increase the risk of infection/sepsis. • GOLD STANDARD for kidney function and adequacy of renal perfusion • The functioning of the renal system affects every body system; therefore, it is ALWAYS relevant! WORSENING WORSENING• Because there is no history of renal disease, this value is extremely significant. Because creatinine is a much more reliable indicator of kidney function/filtration of metabolic waste compared to BUN, it is elevated in Mrs. Kelly because of sepsis/septic shock and lack of perfusion to the kidneys. Regardless of the cause of hypotension, the kidneys will ultimately take a hit. If this lab is elevated, it must be trended carefully to see what direction the kidney function is going WBC: 13.2 Neutrophil %: 93 Hgb: 14.4 Platelets: 246 Bands: 2 • ALWAYS RELEVANT based on its correlation to the presence of inflammation or infection • Body is mounting systemic immune response to underlying infection. WBC elevation is due primarily to the increased production of neutrophils who are the “first responders” of the immune system in response to infection. • ALWAYS RELEVANT for same reason as WBCs • Most common leukocyte • FIRST RESPONDER to any bacterial infection within several hours or when the inflammatory response is activated • ALWAYS RELEVANT to determine anemia or acute/chronic blood loss • Relevant whenever there is a concern for anemia or blood loss or a patient on heparin • If platelets are low, it will obviously be significant and must be noted • Any patient on heparin products must also have this noted because of the clinical possibility of heparin-induced thrombocytopenia (HIT) • Develops when immune system forms antibodies against heparin that cause small clots and lower platelet levels • Immature neutrophils that are elevated in sepsis as the body attempts to fight infection and releases these prematurely • If elevated, it’s a clinical RED FLAG in the context of sepsis. If elevated to >8, it is considered a “shift to the left,” which indicates impending sepsis WORSENING WORSENING STABLE STABLE STABLE Lactate: 3.2 Remember Krebs cycle and lactic acidosis in A&P due to anaerobic metabolism? WORSENING Magnesium: 1.8 • GOLD STANDARD lab to trend with any shock state, especially sepsis! • Elevated levels correlate with higher likelihood of dying. For example, in septic shock, a level >4 reflects a 28 percent mortality Lactate builds up within the serum and can be seen as a marker of strained cellular metabolism • Essential to normal cardiac electrical conduction, as is K+ • If too high or low, can predispose to rhythm changes that can be life-threatening! STABLEColor: Yellow Clarity: Cloudy Specific Gravity: 1.032 Protein: 2+ Nitrite: Positive LET: Positive RBCs: 1 • Clear to pale yellow is usually seen with aggressive diuresis • Orange color typically due to bilirubin in urine with liver disease • Dark amber is commonly seen with dehydration or fluid volume deficit • Though the context here is a UA, students must recognize the importance of always evaluating the clarity in the tubing of any patient who has a Foley catheter • If urine is cloudy or has sediment, patient may have possible urinary tract infection (UTI) and UA should be obtained, especially if new finding • Measures the kidney’s ability to concentrate or dilute urine in relation to plasma • Increased with dehydration and decreased with diuresis • Relevant when positive in any patient with renal disease • If kidneys have been damaged or there is a new finding of renal failure, proteins, being a large colloid, should be filtered by glomerulus • If there is damage to the glomeruli, the inability to adequately filter urine will be present and therefore will be positive • However, in active young adolescent females, there is a phenomenon that produces a higher protein in the urine • A first voiding of the day should be measured with these individuals • To rule out UTI or determine its presence, nitrites, LET, and WBC micro must be assessed together • Nitrites are relevant because, if positive, they reflect the presence of gram-negative bacteria in the urinary tract, the most common being E. coli • By itself, it is not a predictable indicator of urinary infection • To rule out UTI or determine if present, nitrites, LET, and WBC micro must be assessed together • LET is relevant–it is an enzyme that is present if WBCs are in the urine • By itself is not a predictable indicator of urinary infection • Must be noted if UTI or renal calculi–this gives amount of RBCs present which can correlate with severity STABLE WORSENING WORSENING WORSENING WORSENING STABLE WORSENINGWBCs: >100 Bacteria: LARGE Epithelial: Few • ALWAYS RELEVANT and GOLD STANDARD that by itself indicates the presence of UTI if patient has symptoms • Most clinicians will diagnose UTI if >5 WBCs present in urine and symptomatic • Amount of WBCs present indicates severity • To rule out UTI or determine if present, nitrites, LET, and WBC micro must be clustered and assessed together • Has POSITIVE finding consistent with UTI • Does not consistently correlate to presence of infection, though it can be clustered with WBC, LET, and nitrites • Skin cells that are present in the urine. Epithelial cells are usually reported as "few," "moderate," or "many" present. Normally, a few epithelial cells can be found in the urine sediment. In urinary tract conditions such as infections, inflammation, and malignancies, an increased number of epithelial cells are present. WORSENING STABLE Chest x-ray: No infiltrates or other abnormalities. No changes from last previous. There is no pneumonia as the source of the infection and urine/urosepsis is still the source. STABLE Part II: Put it All Together to THINK Like a Nurse! 1. After interpreting relevant clinical data, what is the primary problem? (Management of Care/Physiologic Adaptation) Problem: Pathophysiology in OWN Words: Sepsis/urosepsi s This is a general step-by-step summary. I encourage you to review your nursing textbook or other clinical resources to DEEPEN your knowledge of this content. 1. Precipitating event…usually bacterial infection that has entered the bloodstream (sepsis). 2. Activation of widespread inflammatory response (SIRS). 3. Immune system initiates mediators of inflammatory response w/physiologic consequences (increased temperature…slightly increased HR, mild hypotension). a. Hypodynamic state due to decreased cardiac output (CO). 4. Increased capillary permeability…fluid leakage…third spacing (which results in TACHYCARDIA as the body begins to compensate for decreased cardiac output (CO) (remember CO=SVxHR!). a. Hyperdynamic state as body attempts to increase CO. Patient looks better but is actually worsening. 5. Vasodilation… further lowering of BP and persistent tachycardia. a. Compensation attempts wearing down resulting in more severe hypodynamic state. 6. Maldistribution of volume (third spacing that will also influence decreasing BP and increasing HR! 7. Decreased venous return…lowers PRELOAD as a determinant of CO (this too willlower BP due to decreased CO). 8. Decreased CO as a result of decreased preload as less venous return comes back to the right side of the heart. Collaborative Care: Medical Management 2. State the rationale and expected outcomes for the medical plan of care. (Pharm. and Parenteral Therapies) Medical Management: Rationale: Expected Outcome: Establish peripheral IV 0.9% NS 1000 mL IV bolus Acetaminophen 650 mg Ceftriaxone 1g IVPB…after blood/urine cultures obtained Morphine 2 mg IV push every 2 hours prn-pain Need IV access to initiate IV fluid resuscitation. Early fluid resuscitation is a standard of care in sepsis due to fluid volume deficit secondary to third spacing with inflammatory process as well as resultant vasodilation. Though a fever can be beneficial in sepsis, most care providers will order to promote patient comfort. As a third generation broad-spectrum cephalosporin, it binds to the bacterial cell wall membrane, causing cell death. Therapeutic Effects: Bactericidal action against susceptible bacteria. Spectrum: Similar to that of second-generation cephalosporins, but activity against staphylococci is less, while activity against gramnegative pathogens is greater. Opioid narcotic- Bind to opiate receptors in the CNS. Alter the perception of and response to painful stimuli while producing generalized CNS depression. IV established Improvement in fluid volume deficit manifested by decrease in HR and elevation in SBP. Lowering of fever Will not see immediate response in resolving infection, but would expect to see improvement over the next 24 hours Pain decreased Collaborative Care: Nursing 3. What nursing priority (ies) will guide your plan of care? (Management of Care) Nursing PRIORITY: Fluid volume deficit (C-circulation) • Ineffective tissue perfusion (C-circulation) • Risk for falls PRIORITY Nursing Interventions: Rationale: Fluid volume deficit Establish peripheral IV Meets THREE criteria for SIRS. The need for IV fluids and IV antibiotics must be recognized and anticipated by the nurse. Fluid volume resuscitation-ISOTONIC Early fluid resuscitation is a standard of care in solution-most common 0.9% NS. sepsis due to a fluid volume deficit, secondary to Anticipate at least one and likely two third spacing influenced by the inflammatory liters. process and vasodilation. Reassess VS within 15 minutes after each Determine if improvement in fluid volume status is IV bolus is administered. present by a decrease in HR and elevation in SBP. TREND closely to determine trajectory! Ineffective tissue perfusion: cardiac, renal, neuro (ANTICIPATE!) Closely TREND and monitor VS parameters condition is improving, HR will decrease and of BP, HR, RR as well as color/temp of skin. BP increase and RR should be <20 as cardiac output is improved through fluid resuscitation. If no systemic inflammatory response present Expected Outcome:IV established Fluid balance restored. HR decreases, BP increases from prior baseline See above HR will decrease and BP increase and RR should be <20 as cardiac output is 4. What psychosocial/holistic care PRIORITIES need to be addressed for this patient? Assess and trend creatinine and urine output closely. Assess mentation closely for any changes from current baseline. due to sepsis, temp will also trend downwards. To determine adequate renal perfusion. Confusion and worsening change are not uncommon with sepsis/infection and must be carefully trended as a general reflection of overall status. improved through fluid resuscitation. Creatinine trends downward as well as renal function improves. u/o >30 mL/hr Mentation/confusion improves as sepsis improves. Risk for falls Frequent/close observation. Place close to nursing station Use tab alarm prn Re-orient frequently Visualization is needed if acutely confused and makes attempts to get out of bed. Evaluate need for 1:1 as needed Loud audio alert to notify nurse this patient is on the move! Promote orientation to surroundings and decrease confusion Free from falls Free from falls Free from falls(Psychosocial Integrity/Basic Care and Comfort) Psychosocial PRIORITIES: Use your lens of practice as an educator to determine how you would establish a plan of care for each of the psychosocial priorities identified above. I have some general recommendations below that can be used to initiate dialogue and discussion. PRIORITY Nursing Interventions: Rationale: Expected Outcome: CARE/COMFORT: Caring/compassion as a nurse Discuss the following principles to effectively engage and communicate caring by showing that the patient matters to the nurse: Emotional support BE PRESENT and AVAILABLE to your patient. When this is made intentional to your patient, it communicates caring (Swanson, 1991). Providing/offering hope Hope is related to meaning and purpose in life, but its emphasis is on having a future hope or expectation. This is closely related to spiritual care (Swanson, 1991). Nurse Engagement The nurse must remain clinically curious and responsive to the patient’s story and situation. When distracted and not engaged, the nurse will be unable to invest the energy needed to recognize relevant and urgent clinical signs that may require intervention. When nurses are not engaged with the patient and their clinical problem, patient outcomes will suffer. Will feel valued and comforted Will feel valued and comfortedPhysical comfort measures Nurse Presence To be present means that the nurse is AVAILABLE and ACCESSIBLE and this is communicated to the patient. Presence can also be defined as “being with” and “being there” to meet their needs in a time of need. Other ways to define or explain presence include caring, nurturance, empathy, physical closeness, and physical touch. (Rex–Smith, 2007). Use of touch Touch is a fundamental human need and an appropriate intervention that nurses should integrate into their practice. Touch is a positive way to influence the patient’s physical environment. It uses nature to influence the patient’s well-being (Bush, 2001). Never underestimate the power of the “little things’ that are done for your patients. I have observed that the little things such as basic hygiene, shave, back rub, or obtaining the patient’s story, are the BIG things that communicate caring and also make them feel so much better! EMOTIONAL (How to develop a therapeutic relationship): Discuss the following principles needed as conditions essential for a therapeutic relationship: • Rapport • Trust • Respect • Genuineness • Empathy SPIRITUAL: • F-Faith or beliefs: What are your spiritual beliefs? Do you consider yourself spiritual? What things do you believe in that give meaning to life? • I-Importance and influence: Is faith important to you? How has your illness or hospitalization affected your belief practices? • C-Community: Are you connected to a faith center in the community? Does it provide support/comfort for you during times of stress? Is there a person/group who assists you in your spirituality? • A-Address: What can I do for you? These questions, if used in this scenario by the nurse, would naturally explore this patient’s spirituality. It is always best if the nurse has some comfort in the exploration of spirituality. Patients can sense discomfort or anxiety in approaching this portion of the assessment. The FICA model offers some open-ended questions to make spiritual assessment a natural part of the conversation. Use this spiritual assessment tool to make caring for the spirit an essential component of your nursing practice! Faith/beliefs are supportedWhat support can healthcare provide to support your spiritual beliefs/practices? CULTURAL Considerations (IF APPLICABLE) Since religious worldviews provide a window to the prevailing values and ethnic norms of any cultural group, knowledge, and understanding of the most dominant religions of ethnic groups in your community are essential and will facilitate cultural sensitivity. But remember that there will always be exceptions, so be careful not to make assumptions! Becoming knowledgeable about another cultural group and integrating this knowledge into your practice is the essence of becoming culturally competent. It means respecting each patient’s cultural diversity and examining how their beliefs may affect their health care. When nursing care does not intersect with the patient’s worldview or belief set, compliance with the proposed treatment plan will be less likely (Ward, 2012). Cultural beliefs are supported 5. What educational/discharge priorities need to be addressed to promote health and wellness for this patient and/or family? (Health Promotion and Maintenance) o Though sepsis is not entirely preventable, as it relates to fluid volume deficit, and PREVENTING a UTI, the importance of INCREASING fluid intake must also be addressed. o With the elderly, it is always important to address safety in the home. She will most likely be weak from the hospitalization so she may need to spend some time in a rehab facility. Also important to include family in the plan of care. o Other educational priorities that are indirectly related to decreasing risk of infection include excellent control of blood glucose. Reinforce foundational tenets of diabetes education: diet, medications, exercise, and monitoring blood glucose/frequency of daily checks.Author Keith Rischer, RN, MA, CEN, CCRN Reviewers • Linda L. Gilbert, MSN, RN, Clinical Coordinator, Goodwin College, East Hartford, Connecticut • Julie A. Hogue, RN, MSN, Nursing Instructor, Illinois Valley Community College, Oglesby, Illinois • Sarah R. Pierce, DNP, AGACNP-BC, CCRN, PLNC, Freed-Hardeman University, Henderson, Tennessee References Badlissi, F., Schumacher, H., Adebajo, A., & Underwood, M. (2015). Gout. Retrieved from www.epocrates.com Bush, E. (2001). The use of human touch to improve the well-being of older adults: A holistic nursing intervention. Journal of Holistic Nursing, (19)3, 256-270. Daniels, R., Richmond, L., Andrus, P., & Walker, D. (2015). Sepsis in adults. Retrieved from www.epocrates.com Neviere, R. (2016). Sepsis syndrome in adults. Epidemiology, definitions, clinical presentation, diagnosis, and prognosis. Retrieved from www.uptodate.com Rex-Smith, A. (2007). Something more than presence. Journal of Christian Nursing, 24(2), 82–87. Sommers, M.S. & Fannin, E. (2015). Diseases and disorders: A nursing therapeutic manual. (5th ed.). Philadelphia, PA: F.A. Davis Company. Swanson, K. M. (1991). Empirical development of a middle range theory of caring. Nursing Research, 40(3), 161–166. Vallerand, A.H., Sanoski, C.A., & Deglin, J.H. (2014) Davis’s drug guide for nurses. (14th ed.). Philadelphia, PA: F.A. [Show More]
Last updated: 2 years ago
Preview 1 out of 15 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Nov 08, 2022
Number of pages
15
Written in
Additional information
This document has been written for:
Uploaded
Nov 08, 2022
Downloads
0
Views
280