*NURSING > SHADOW HEALTH > NUR 211 NUR211 CVA Case Study. Unfolding Reasoning Cerebral Vascular Accident (CVA) John Gates, 59 y (All)
NUR 211 NUR211 CVA Case Study. Unfolding Reasoning Cerebral Vascular Accident (CVA) John Gates, 59 years old
Document Content and Description Below
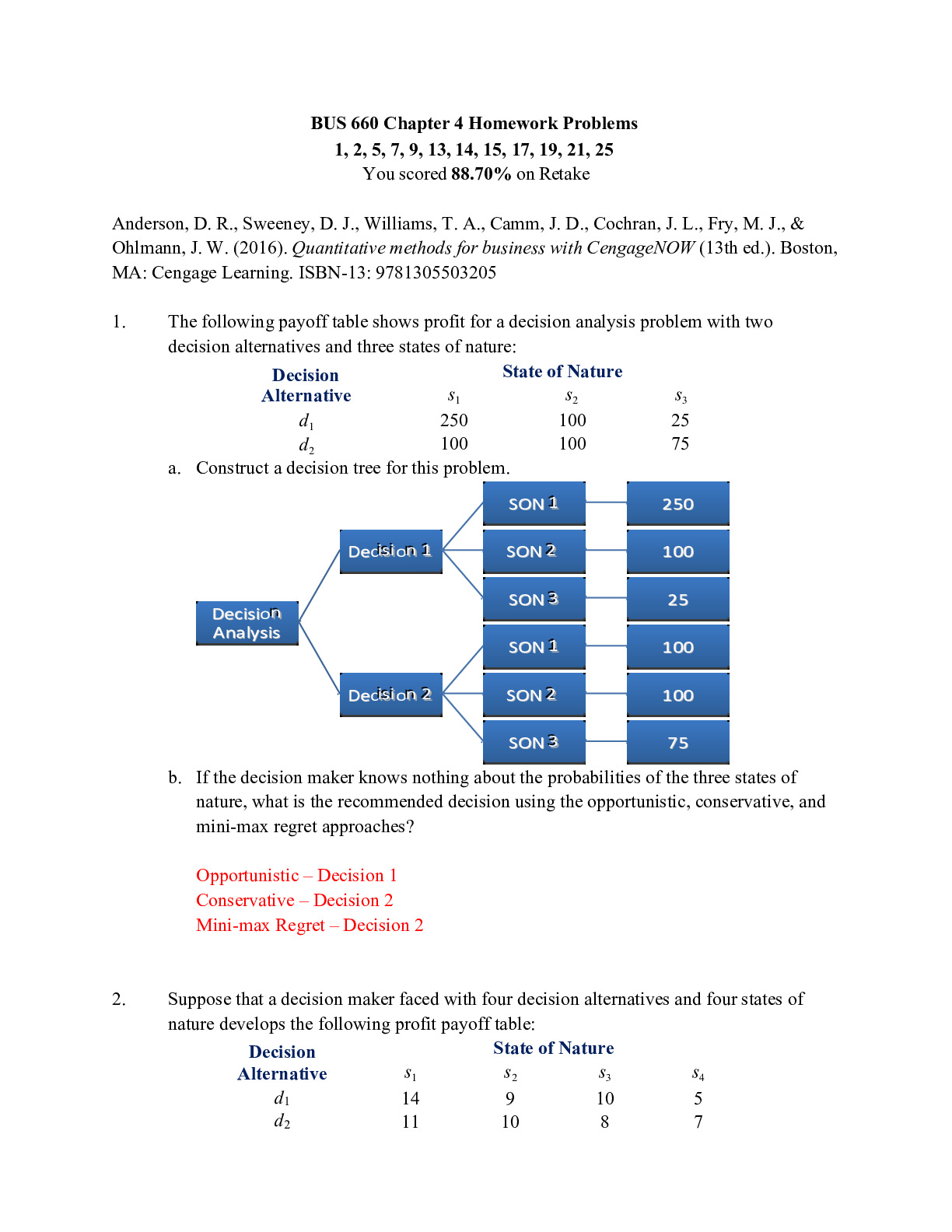
NUR 211 NUR211 CVA Case Study. Unfolding Reasoning Cerebral Vascular Accident (CVA) John Gates, 59 years old Cerebral Vascular Accident (CVA) John Gates, 59 years old Primary Concept Perfusion ... Interrelated Concepts (In order of emphasis) 1. Stress 2. Coping 3. Clinical Judgment 4. Patient Education 5. Communication 6. Collaboration © 2016 Keith Rischer/www.KeithRN.comUNFOLDING Clinical Reasoning Case Study: STUDENT Cerebral Vascular Accident (CVA) History of Present Problem: John Gates is a 59-year-old male with a history of diabetes type II and hypertension who was at work when he had sudden onset of right-sided weakness, right facial droop, and difficulty speaking. He was transported to the emergency department (ED) where these symptoms continue to persist. It has been one hour from the onset of his neurologic symptoms when he presents to the ED. You are the nurse responsible for his care. Personal/Social History: John lives with his wife in their own home in a small rural community. He owns a hardware store where he remains active and involved in the day-to-day operations. His wife insists on being by his side and talking to John despite John’s frustration in not being able to answer her questions. His wife reports that the past week he has been complaining of episodes where his heart felt as if it was beating irregularly and fast but then resolved. His wife also states that he has been complaining of pain in his right foot the past week. John has been trying to quit smoking the past month and has been using a nicotine patch. His wife reports that he does not regularly check his blood glucose and eats what he wants. He is 6 feet tall and weighs 250 pounds (113.6 kg/BMI of 33.9). What data from the histories are RELEVANT and has clinical significance to the nurse? RELEVANT Data from Present Problem: Clinical Significance: Hx of diabetes type II and hypertension Sudden onset of right-sided weakness, facial droop, and difficulty speaking 1 hour from the onset of neuro symptoms Hypertension is the leading cause for stroke and diabetes leads to vascular changes in the body, both of these conditions increases the patient’s risk for stroke These symptoms are some of the common symptoms for stroke, these deficits can correlate with the areas of the brain that the stroke occurred in If this is an ischemic stroke, tPA can be administered within 3 hours of the symptoms of stroke to increase the chances of recovery RELEVANT Data from Social History: Clinical Significance: Frustration in not being able to answer wife’s questions Episodes of irregular rapid heartbeat Pain in his right foot Trying to quit smoking --- using a nicotine patch Does not regularly check blood glucose and eats what he wants BMI of 33.9 Frustration is normal for those in situation when they are having difficulty speaking, it is important to try and communicate with the patient in other way and talk to the doctor for a referral for a speech therapist to collaborate in the patients care The patient is experiencing periods arrythmias, which can increase the patient’s risk for stroke due to the change in blood flow which can form clots Most likely caused diabetic neuropathy due to damage to the small nerve endings in the foot, due to his uncontrolled diabetes Cigarette smoking doubles the patient’s risk for ischemic stroke and increases the patient’s risk for cerebral hemorrhage Self-testing blood glucose is an important tool for managing diabetes and preventing complications. Since the patient is not regularly monitoring his blood glucose and eats what he wants, his diabetes my be uncontrolled and can further increase his risk for stroke Being overweight increases the patient’s risk for stroke Patient Care Begins:Current VS: P-Q-R-S-T Pain Assessment (5th VS): T: 99.2 F/37.3 C (oral) Provoking/Palliative: Unable P: 118 (irregular) Quality: R: 20 (regular) Region/Radiation: BP: 198/94 Severity: O2 sat: 99% room air Timing: RELEVANT VS data: Clinical Significance: Pulse 118 (irregular) BP 198/94 Tachycardia -- can disrupt normal heart function and lead to serious complications including heart failure and stroke The patient has a Hx of HTN, this places patient at an increased risk for heart attacks and strokes. High BP may be caused by a decrease in blood flow to the heartCurrent Assessment: GENERAL APPEARANCE: Appears anxious–he is aware and appears to be concerned about changes in neuro status RESP: Breath sounds clear with equal aeration bilaterally, nonlabored respiratory effort CARDIAC: Pink, warm & dry, no edema, heart sounds irregular–S1S2, telemetry rhythm is atrial fibrillation, pulses strong, equal with palpation at radial/pedal/post-tibial landmarks NEURO: Is anxious, restless, and agitated, speech is currently slurred and difficult to understand, facial droop present on right side, pupils equal and reactive to light (PEARL), both right upper extremity (RUE) and right lower extremity (RLE) notably weak (3/5) in comparison to left, which is strong (5/5), right pronator drift present, unable to hold right arm up, right visual deficit cut present GI: Abdomen soft/non-tender, bowel sounds audible per auscultation in all 4 quadrants Able to swallow saliva GU: Voiding without difficulty, 700 mL urine clear/yellow, SKIN: Skin integrity appears intact, right foot not assessed at this time What assessment data is RELEVANT that must be recognized as clinically significant to the nurse? RELEVANT assessment data: Clinical Significance: General: Appears anxious Cardiac: heart sounds irregular–S1S2, telemetry rhythm is atrial fibrillation Neuro: restless, agitated, slurred speech, right sided weakness and facial droop Anxiety can cause panic attacks which can physical symptoms that include heart palpitations, chest pain, and shortness of breath. Anxiety can increase BP. An irregular heartbeat can interrupt the normal flow of blood, increasing the patient’s risk for blood clots and stroke. During A. fib the AV node is not firing correctly with can lead to pooling of blood, that can then from into a clot that is pumped in to circulation The slurred speech, right sided weakness, and facial droop are all neurological symptoms consistent with signs of stroke. Cardiac Telemetry Strip: Interpretation: Atrial Fibrillation with RVR Clinical Significance: An irregular heartbeat can interrupt the normal flow of blood, increasing the patient’s risk for blood clots and stroke. During A. fib the AV node is not firing correctly with can lead to pooling of blood, that can then from into a clot that is pumped in to circulation. Radiology Reports: Head CT What diagnostic results are RELEVANT and must be interpreted as clinically significant by the nurse? RELEVANT Results: Clinical Significance: No abnormalities noted, Because the patient has such a high risk for stroke the CT was performed to identify if there wasno mass, no bleed, no shift present any hemorrhage, tumors, aneurysm, ischemia, edema, tissue necrosis, or shift in intracranial content. This is used to distinguish the type of stroke that occurred. Head CT is normalLab Results: Complete Blood Count (CBC) Current: High/Low/WNL? Previous: WBC (4.5-11.0 mm 3) 6.8 WNL 7.9 Hgb (12-16 g/dL) 14.8 WNL 16.1 Platelets(150-450x 103/µl) 228 WNL 201 Neutrophil % (42-72) 71 WNL 79 What lab results are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: WBC 6.8 Hgb 14.8 Platelets 228 Neutrophil 71 Always relevant based on its correlation to the presence of inflammation or infection -- A WBC count can detect hidden infections within your body and alert doctors to undiagnosed medical conditions Always relevant to determine anemia or acute/chronic blood loss A platelet count may be used to screen for or diagnose various diseases and conditions that can cause problems with blood clot formation. Could be used to rule out a bleeding disorder, bone marrow disease, or excessive clotting disorder Always relevant based on its correlation to the presence of inflammation or infection --- A high neutrophil count it can mean that the patient has an infection or is under a lot of stress. It can also be a symptom of more serious conditions. Neutrophils are the first responder to any bacterial infection within several hours or when the inflammatory response is activated Stable Stable but decreasing Stable but increasing Improving Basic Metabolic Panel (BMP) Current: High/Low/WNL? Previous: Sodium (135-145 mEq/L) 133 Low 139 Potassium (3.5-5.0 mEq/L) 4.1 WNL 4.5 Glucose (70-110 mg/dL) 222 High 128 Creatinine (0.6-1.2 mg/dL) 1.5 High 1.1 Coag PT/INR (0.9-1.1 nmol/L) 1.1 WNL n/aWhat lab results are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: Sodium 133 Potassium 4.1 Glucose 222 Creatinine 1.5 PT/INR 1.1 It helps maintain normal blood pressure, supports the work of nerves and muscles, and regulates fluid balance. If your sodium blood levels are too high or too low, it may mean that there is problem with the kidneys, dehydration, or another medical condition. This needs to be assessed closely because hyponatremia can also influence and contribute to cerebral edema Essential to normal cardiac electrical conduction --- if too high or low can cause changes to rhythm that can be lifer-threatening Relevant to history of DM --- this is expected and will need sliding scale to cover. Research shows that high glucose levels decrease the body’s ability to reperfuse the infarcted area. If there is adequate blood flow to the affected area, there’s a good chance those neurologic deficits can be reversed. The National Stroke Association recommend blood glucose levels be <140. Gold standard for kidney function and adequacy of renal perfusion PT evaluates the ability to clot and INR ensures that the results from a PT test are the same from one lab test to another. Can be used to monitor the effects of warfarin, assess for liver failure, and evaluate clotting factor deficiencies and for vitamin K deficiency or severe malnutrition. Worsening Stable Worsening Worsening WNL --- no trend can be established yet Lab Planning: Creating a Plan of Care with a PRIORITY Lab: Lab: Normal Value: Why Relevant? Nursing Assessments/Interventions Required: Creatinine Value: 1.5 0.6-1.2 mg/dL RED FLAG: >7.4 mg/dL Creatinine is the gold standard for kidney function and adequacy of renal perfusion. Any increase in serum creatinine can be used as a marker to identify patients with renal dysfunction, as it indicates a diminished ability of the kidneys to filter creatinine. Assess the patient frequently for signs of skin breakdown, patients with high creatine levels often complain of itching skin. The nurse should also turn the patient every 2 hours. As creatinine and BUN levels continue to rise, the patient is likely to experience fatigue, muscle weakness and nausea and vomiting. The person may have decreased mental awareness, including drowsiness and confusion. The nurse should assess the cognitive and physical capabilities of any patient with an increased creatinine and BUN to ensure safe care. Assess I&Os closely Restrict fluid Assess for signs of fluid retention/edema Perform daily weightsClinical Reasoning Begins… 1. What is the primary problem your patient is most likely presenting? Ischemic Stroke Embolic 2. What is the underlying cause/pathophysiology of this primary problem? (Relate initial manifestations to the pathophysiology of the primary problem) Pathophysiology of Primary Problem: Rationale for Manifestations: Ischemic stroke results from blockage and/or stenosis of a cerebral artery, decreasing or stopping blood flow. This decrease or stop in blood flow ultimately causes a brain infraction. Embolic stroke occurs when a blood clot traveling through cerebral blood vessels becomes lodged in vessels that are too narrow for it to pass through. After the clot is lodged into a cerebral blood vessel that is too narrow for it, the area of the brain supplied by the blocked vessel becomes ischemic and causes a sudden onset of symptoms. The symptoms experienced by the patient correlates to the area in the brain the blockage is affecting. Collaborative Care: Medical Management Care Provider Orders: Rationale: Expected Outcome: Establish peripheral IV 12 lead EKG stat Labetalol 10-20 mg IV prn every 15 minutes to keep SBP 160-180 CT head stat Cardiac monitor continuous NPO A patent line is important for administration of IV drugs and emergency drug As a non-invasive yet most valuable diagnostic tool, the 12-lead EKG records the heart's electrical activity as waveforms. When interpreted accurately, an EKG can detect and monitor a host of heart conditions - from arrhythmias to coronary heart disease to electrolyte imbalance. Labetalol is a beta blocker that will work to lower BP by inhibiting beta stimulation as well as alpha 1, which will cause arterial vasodilation Need to rule out hemorrhagic vs. embolic CVA to confirm that is embolic and no other contraindications can receive tPA Assess AFib closely as can go into RVR (any amount >100) at any time which lowers blood pressure and decreases cardiac output as a result Dysphagia is very common post-stroke and puts the patient at risk for aspiration. Mr. Gates is presenting with facial droop and difficulty speaking which are signs of possible dysphagia due to muscle weakness of the mouth and throat. After priorities are addressed and the patient is more stable, a speech therapy consult may be initiated for a swallow evaluation. A barium swallow study identifies abnormal movement of food/fluid, anatomic structures, and various food consistencies to determine patient’s swallowing potential and ensure safety. IV established and patent, so nurse is able to give IV medications and emergency drugs as needed The healthcare team will be able to see and interpret the electrical activity the patient is experiencing and gain more knowledge on the patient’s condition SBP maintained in 160- 180 range No signs of hemorrhage so that tPA can be administer to have neurons HR remains <100 No aspirationAlteplase IV dose per pharmacy (if CT negative for bleed) Thrombolytic therapy is the gold standard of medical management and can give us the best hoped for outcome if done in a timely manner. Mechanism is to bind fibrin and convert plasminogen to plasmin, which stimulates dissolving of the clot. Tolerates therapy with no adverse reactions including massive cerebral hemorrhage or other lesser bleeding complicationsPRIORITY Setting: Which Orders Do You Implement First and Why? Care Provider Orders: Order of Priority: Rationale: 1.Establish peripheral IV 2.Labetalol 10-20 mg IV prn every 15" to keep SBP 160-180 3.CT head stat 4.Cardiac monitor continuous 5.Alteplase IV (if CT negative for bleed) 1. CT head stat 2. Establish peripheral IV 3. Alteplase IV (if CT negative for bleed) 4. Labetalol 10-20 mg IV prn every 15” to keep SBP 160-180 5. Cardiac monitor continuous 1. The CT is used to rule out or identify a hemorrhagic source of neuro changes, so tPA can be considered to save neurons and minimize lifelong deficits 2. Alteplase is a thrombolytic medication, used to treat acute ST elevation myocardial infarction, pulmonary embolism associated with low blood pressure, acute ischemic stroke, and blocked central venous access devices. It is given by injection into a vein or artery. 3. This must be administered ASAP if the CT is negative for bleed, time saves neurons, 4. Lowering the patient BP is a high priority in this case 5. The patient is at an increased risk for dysrhythmias with an acute neuro event. This is important but the other orders hold a higher priority. Medication Dosage Calculation: Medication/Dose: Mechanism of Action: Volume/time frame to Safely Administer: Nursing Assessment/Considerations: Labetalol 20 mg IV push (5 mg/mL vial) Blocks stimulation of beta 1- adrenergic receptors. Does not usually affect beta2 receptor sites. Decrease the BP and HR 4 mL/ 2 minutes IV push IV Push: Volume every 15 sec? 0.5 mL/15 sec Obtain BP and HR before administering ---- hold if SBP <90, HR <60 Change position slowly Contraindicated in worsening CHF, bradycardia, or heart block Use is cation for those with diabetes or liver disease Medication Dosage Calculation: Medication/Dose: Mechanism of Action: Amount to Safely Administer: Nursing Assessment/Considerations: Alteplase 0.9 mg/kg IV over 60 minutes not to exceed 90 mg Alteplase binds to fibrin in a thrombus and converts the entrapped plasminogen to plasmin. Plasmin in turn degrades the fibrin matrix of the thrombus, thereby exerting its thrombolytic action. It also produces limited conversion of plasminogen in the absence of fibrin. Weight: 113.6 kg Amount to administer: 90 mg --- the patient requires 102.24 but this would be an overdose contraindicated in active bleeding monitor closely for signs of bleeding (petechiae) o q 15 min X1hr o q 15-30 min X 8 hr use caution with patient who have had recent surgery may cause intracranial hemorrhage monitor for anaphylaxis use caution with uncontrolled hypertension assess neuro status during therapyCollaborative Care: Nursing 3. What nursing priority(ies) will guide your plan of care? (if more than one-list in order of PRIORITY) Continue to monitor and treat elevated BP to maximize cerebral perfusion o Ineffective tissue perfusion o Acute confusion o Risk for falls 4. What interventions will you initiate based on this priority? Nursing Priority: Nursing Interventions: Rationale: Expected Outcome: Acute confusion/ ineffective tissue perfusion Ineffective tissue perfusion Ineffective tissue perfusion Perform frequent neuro check– usually every 15–30" in the acute phase or per MD orders to trend for any changes Frequent monitoring of BP of at least every 15minutes Continuous monitoring of cardiac rhythm. Afib can accelerate into the 130–150’s readily. Anticipate this possibility Status can change quickly, must assess for any subtle changes that could reflect a complication! Goal is to keep SBP 160–180. Do not want too high or too low to optimize cerebral perfusion May need to slow HR if develops rapid rate and drops BP No change in neuro status SBP in range of 160180 HR remains <100 5. What body system(s) will you assess most thoroughly based on the primary/priority concern? Nervous System 6. What is the worst possible/most likely complication to anticipate? Knowing that this patient is having a large CVA and is at risk for: o increasing ICP o further deterioration in neuro status that could include seizures, respiratory arrest or declining level of consciousness (LOC) 7. What nursing assessments will identify this complication EARLY if it develops? The nurse should be performing frequent neuro assessments, and keep an eye on the trends o Subtle neuro findings can be extremely significant in the clinical setting o Monitor vital signs for changes o Monitor the patient LOC 8. What nursing interventions will you initiate if this complication develops? Rapid response for intubation in case of respiratory arrest Meds to treat ICP and its complications, such as seizures 9. What psychosocial needs will this patient and/or family likely have that will need to be addressed? Emotional support Spiritual support Knowledge deficit10. How can the nurse address these psychosocial needs? Emotional support o Be present and available to the patient Actively listen to what the patient has to say Spiritual support o Ask open-ended questions to assess. o Examples: What thing do you believe in that give meaning to life? Are you involved/ connected with a faith community? Has your current health problem affected your spiritual beliefs? What can I do to support your spiritual beliefs/practices? Knowledge and education about what is taking place and what the care priorities will be in the days ahead. The nurse can integrate patient/family education naturally while providing care by simply explaining at their level everything that the nurse/physician has ordered and WHY it needs to be done. This is why it is essential for the nurse to know and DEEPLY understand the rationale for both the physician and nursing plan of care; so, it can be readily taught and explained to the patient/family at a level they can understand Evaluation: 1 Hour Later…Alteplase has just completed and the following clinical data is collected: Current VS: Most Recent: T: 99.0 F/37.2 C (oral) T: 99.2 F/37.3 C (oral) P: 74 (regular) P: 118 (irregular) R: 16 (regular) R: 20 (regular) BP: 178/86 BP: 198/94 O2 sat: 96% room air O2 sat: 99% room air Current Assessment: GENERAL APPEARANCE: Resting comfortably, appears in no acute distress RESP: Breath sounds clear with equal aeration bilaterally, nonlabored respiratory effort CARDIAC: Pink, warm & dry, no edema, heart sounds regular with no abnormal beats, pulses strong, equal with palpation at radial/pedal/post-tibial landmarks NEURO: Right facial droop no longer present, speech is not as slurred, weakness persists in both RUE and RLE but is stronger (4/5) than before tPA started GI: Abdomen soft/non-tender, bowel sounds audible per auscultation in all 4 quadrants GU: Voiding without difficulty, urine clear/yellow SKIN: Right heel has 1x1 cm stage II pressure ulcer with redness of the entire heel that is blanchable, no drainage noted 1. What clinical data is RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT VS Data: Clinical Significance: Pulse 74 (regular) BP 178/86 HR is now regular. Check the monitor because this patient may have gone back into sinus rhythm. BP is essentially where it needs to be, but the nurse should continue to watch monitor what goes down can also come back up.RELEVANT Assessment Data: Clinical Significance: Neuro: Right facial droop no longer present, speech is not as slurred, weakness persists in both RUE and RLE but is stronger (4/5) than before tPA started Skin: Right heel has 1x1 cm stage II pressure ulcer with redness of the entire heel that is blanchable, no drainage noted The sudden improvement in these key neurologic assessments are reflecting that perfusion and blood flow is being restored to the brain and therefore the improvement in the patient’s status This finding confirms the suspicion that of impaired skin integrity. Blanchable redness is clinically significant because it represents blood flow that is NOT impaired to the site Cardiac Telemetry Strip: Interpretation: Normal Sinus Clinical Significance: Spontaneously converted but needs to be continually monitored as this patient can switch back and forth and will still likely need anti-coagulation 1. Has the status improved or not as expected to this point? The patient’s status has improved 2. Does your nursing priority or plan of care need to be modified in any way after this evaluation assessment? The nursing priorities identified earlier are still relevant, continue to assess neurologic status closely and treat elevated BP to maximize cerebral perfusion. But because there has now been an improvement in status, must closely assess this TREND to ensure that it continues in the right direction! 3. Based on your current evaluation, what are your nursing priorities and plan of care? Transfer out of the ED. o This patient will require ICU level of close monitoring and assessment o Until he is transferred out of the ED, continue to do frequent neuro assessment every 15" as well as VS/rhythm monitoring and assessment. There is still a chance that he may develop a hemorrhagic brain bleed as a result of the TPA and therefore continues to need assessments.Effective and concise handoffs are essential to excellent care and if not done well can adversely impact the care of this patient. You have done an excellent job to this point, now finish strong and give the following SBAR report to the ICU nurse who will be caring for this patient: Situation: Name/age: John Gates, 59 years old BRIEF summary of primary problem: 59-year-old male who was at work when he had sudden onset of right-sided weakness, right facial droop, and difficulty speaking (dysarthric speech). He was transported to the ED where these symptoms persisted. CT confirmed embolic CVA with NO bleed. Initial neuro assessment: Confused to place and why he is in the hospital. Is notably anxious, restless, and agitated. Speech is currently slurred–difficult to understand. Facial droop on right side present, PEARL, both RUE and RLE notably weak in comparison to left, which is strong. Background: Primary problem/diagnosis: Embolic Stroke, New onset of atrial fib-initial rate in the 110’s, BP 198/94 RELEVANT past medical history: Hx of DM-II and HTN Assessment: Vital signs: T: 99.0 F oral P: 74 (regular) R: 16 (regular) BP: 178/86 O2 Sat: 96% room air RELEVANT body system nursing assessment data: Current neuro assessment has shown significant improvement with the following findings: right facial droop no longer present, speech is not as slurred, weakness persists in both RUE and RLE but is stronger than before TPA started. BP has responded to labetalol and is currently and is 178/86. Right heel has 1x1 cm stage II pressure ulcer with redness of the entire heel that is blanchable, no drainage noted How have you advanced the plan of care? Received TPA 1 hour ago --- weakness persists in both RUE and RLE but is stronger than before TPA started. BP has responded to labetalol and is currently and is 178/86. The patient is stable now and has converted to a NSR ---- it is still important to monitor the patient closely for any changes in condition Patient response: Converted to NSR spontaneously 30" ago–rate in the 70’sINTERPRETATION of current clinical status (stable/unstable/worsening): Stable Recommendation: Suggestions to advance plan of care: Since the patient is currently stable, continue to closely assess neuro status for any changes as well as rhythm changes Education Priorities/Discharge Planning 1. What educational/discharge priorities will be needed to develop a teaching plan for this patient and/or family? Strict control of blood glucose to prevent further progression of atherosclerotic changes o Reinforce diet, medications Strict control of hypertension to prevent possible neurologic events o Reinforce diet–low sodium as well as importance and role of medications o Medication education to control A. fib and help prevent neurologic event (Ex: anticoagulants, diltiazem, beta blockers) 2. How can the nurse assess the effectiveness of patient and/or family teaching and discharge instructions? After any education has been completed with the patient or family, one of the more effective strategies to assess effectiveness of teaching is to have them restate the essence or most important points of the teaching after it has been taught and then later in the shift to ensure retention. Caring and the “Art” of Nursing 1. What is the patient likely experiencing/feeling right now in this situation? The patient is likely aware of the seriousness of the current change in status and is likely fearful and anxious. 2. What can you do to engage yourself with this patient’s experience and show that he matters to you as a person? Provide comfort for the patient Anticipating the patients’ needs Preserve the patient’s dignity Informing and explaining what is going on to the patient ----- Knowledge is power from a patient’s perspective, and when the nurse provides this information it can decrease anxiety and fear and make a real difference in her well-being.Med Cards Labetalol Drug Class: antihypertensives, beta blockers Therapeutic Action: Blocks stimulation of beta1 and beta2 -adrenergic receptor sites. Decreases BP Indications: Hypertension Dosages: P.O.----- 100 mg twice daily initially, may increase by 100 mg twice daily every 2-3 days as needed (usual range 400-800 mg/day in 2-3 divided doses): IV ----- 20 mg (0.25 mg/kg) initially, additional doses of 40-80 mg may be given every 10 min as needed (not to exceed 300 mg total dose) or 2 mg/min infusion (range 50-300 mg total dose required). Pharmacokinetics: Route O Onset Peak Duration P.O. 20 min- 2hr 1 1-4 hr 8-12 hr IV 2-5 min 5 min 16-18 hr o Half-life: 3-8 hr Contraindications: Decompensated HF, pulmonary edema, cardiogenic shock, bradycardia or heart block. Use with caution: Renal or hepatic impairment, pulmonary disease (including asthma), diabetes mellitus (may mask signs of hypoglycemia), thyrotoxicosis (may mask symptoms), and patients with a history of severe allergic reactions Adverse Effects: fatigue, weakness, anxiety, depression, dizziness, drowsiness, insomnia, memory loss, mental status changes, nightmares, arrhythmias, bradycardia, CHF, orthostatic hypotension, itching, rash, blurred vision, dry eyes, intraoperative floppy iris syndrome, nasal stuffiness, hyperglycemia, hypoglycemia, constipation, diarrhea, nausea, pulmonary edema, bronchospasm, wheezing. Nursing Considerations: o Monitor BP and pulse frequently during dose adjustment and periodically during therapy. Assess for orthostatic hypotension when assisting patient up from supine position. o Check frequency of refills to determine compliance. o Patients receiving labetalol IV must be supine during and for 3 hr after administration. Vital signs should be monitored every 5-15 min during and for several hrs after administration. o Monitor intake and output ratios and daily weight. Assess patient routinely for evidence of fluid overload (peripheral edema, dyspnea, rales/crackles, fatigue, weight gain, jugular venous distention). o Monitor patients receiving beta blockers for signs of overdose (bradycardia, severe dizziness or fainting, severe drowsiness, dyspnea, bluish fingernails or palms, seizures). Relevant labs: may increase BUN, serum lipoprotein, potassium, triglyceride, uric acid levels, ANA titers, blood glucose levels, serum alkaline phosphatase, LDH, AST, and ALT levels. Client Teaching: o Instruct patient to take medication as directed, at the same time each day, even if feeling well; do not skip or double up on missed doses. Take missed doses as soon as possible up to 8 hr before next dose. Abrupt withdrawal may precipitate life-threatening arrhythmias, hypertension, or myocardial ischemia. o Teach patient and family how to check pulse and BP. Instruct them to check pulse daily and BP biweekly. Advise patient to hold dose and contact health care professional if pulse is <50 bpm or BP changes significantly. o Advise patients to make position changes slowly to minimize orthostatic hypotension, especially during initiation of therapy or when dose is increased. Patients with diabetes should closely monitor blood glucose, especially if weakness, malaise, irritability, or fatigue occurs. Medication may mask tachycardia and increased BP as signs of hypoglycemia, but dizziness and sweating may still occur. o Advise patient to notify health care professional if slow pulse, difficulty breathing, wheezing, cold hands and feet, dizziness, light-headedness, confusion, depression, rash, fever, sore throat, unusual bleeding, or bruising occurs.Alteplase (t-PA) Drug Class: thrombolytics, plasminogen activators Therapeutic Action: Directly converts plasminogen to plasmin, which then degrades clot-bound fibrin. Lysis of thrombi. Indications: Acute myocardial infarction (MI), acute ischemic stroke, pulmonary embolism (PE), occluded central venous access devices. Dosages: 0.9 mg/kg (not to exceed 90 mg), given as an infusion over 1 hr, with 10% of the dose given as a bolus over the 1st min. Pharmacokinetics: Route O Onset Peak Duration IV 30 min 60 min unknown o Half-life: 35 min Contraindications: Active internal bleeding, history of cerebrovascular accident (for MI and PE only), recent (within 3 mo) intracranial or intraspinal injury or trauma, severe uncontrolled hypertension (systolic BP >185 mmHg or diastolic BP >110 mmHg ), evidence or suspicion of intracranial hemorrhage on pretreatment evaluation, recent (within 3 mo) stroke, history of intracranial hemorrhage, seizure at the onset of stroke, current use of oral anticoagulants or an INR >1.7 or a prothrombin time >15 sec, administration of heparin 48 hr before the onset of stroke with an elevated aPTT at presentation, platelet count <100,000/mm3, hypersensitivity Use with caution: Recent (within 10 days) major surgery, trauma, GI or GU bleeding, cerebrovascular disease, systolic BP ≥175 mmHg and/or diastolic BP ≥110 mmHg, high likelihood of left heart thrombus, hemostatic defects, severe hepatic impairment, previous puncture of a non-compressible vessel, severe neurological deficit (NIHSS >22) at presentation Adverse Effects: intracranial hemorrhage, epistaxis, gingival bleeding, bronchospasm, hemoptysis, reperfusion arrhythmias, hypotension, recurrent ischemia/ thrombosis, GI bleeding, nausea, retroperitoneal bleeding, vomiting, GU tract bleeding, ecchymoses, flushing, urticaria, hemorrhage at injection site, phlebitis at injection site, musculoskeletal pain, allergic reaction, and fever Nursing Considerations: o Monitor vital signs, including temperature, continuously for myocardial infarction and at least every 4 hr during therapy for other indications. Do not use lower extremities to monitor BP. Notify health care professional if systolic BP >180 mm Hg or diastolic BP >110 mm Hg. o Assess patient carefully for bleeding every 15 min during the 1st hr of therapy, every 15-30 min during the next 8 hr, and at least every 4 hr for the duration of therapy. Internal bleeding may occur (decreased neurologic status; abdominal pain with coffee-grounds emesis or black, tarry stools; hematuria; joint pain). If uncontrolled bleeding occurs, stop medication and notify health care professional immediately. o Assess patient for hypersensitivity reaction (rash, dyspnea, fever, changes in facial color, swelling around the eyes, wheezing). If these occur, inform health care professional promptly. Keep epinephrine, an antihistamine, and resuscitation equipment close by in the event of an anaphylactic reaction. o Assess neurologic status throughout therapy. Altered sensorium or neurologic changes may be indicative of intracranial bleeding. [Show More]
Last updated: 2 years ago
Preview 1 out of 18 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Nov 08, 2022
Number of pages
18
Written in
Additional information
This document has been written for:
Uploaded
Nov 08, 2022
Downloads
0
Views
83