*NURSING > SHADOW HEALTH > ETOH Withdrawal or Delirium? Next Gen SKINNY Reasoning Case Study Stanley Harris, 90 years old (All)
ETOH Withdrawal or Delirium? Next Gen SKINNY Reasoning Case Study Stanley Harris, 90 years old
Document Content and Description Below
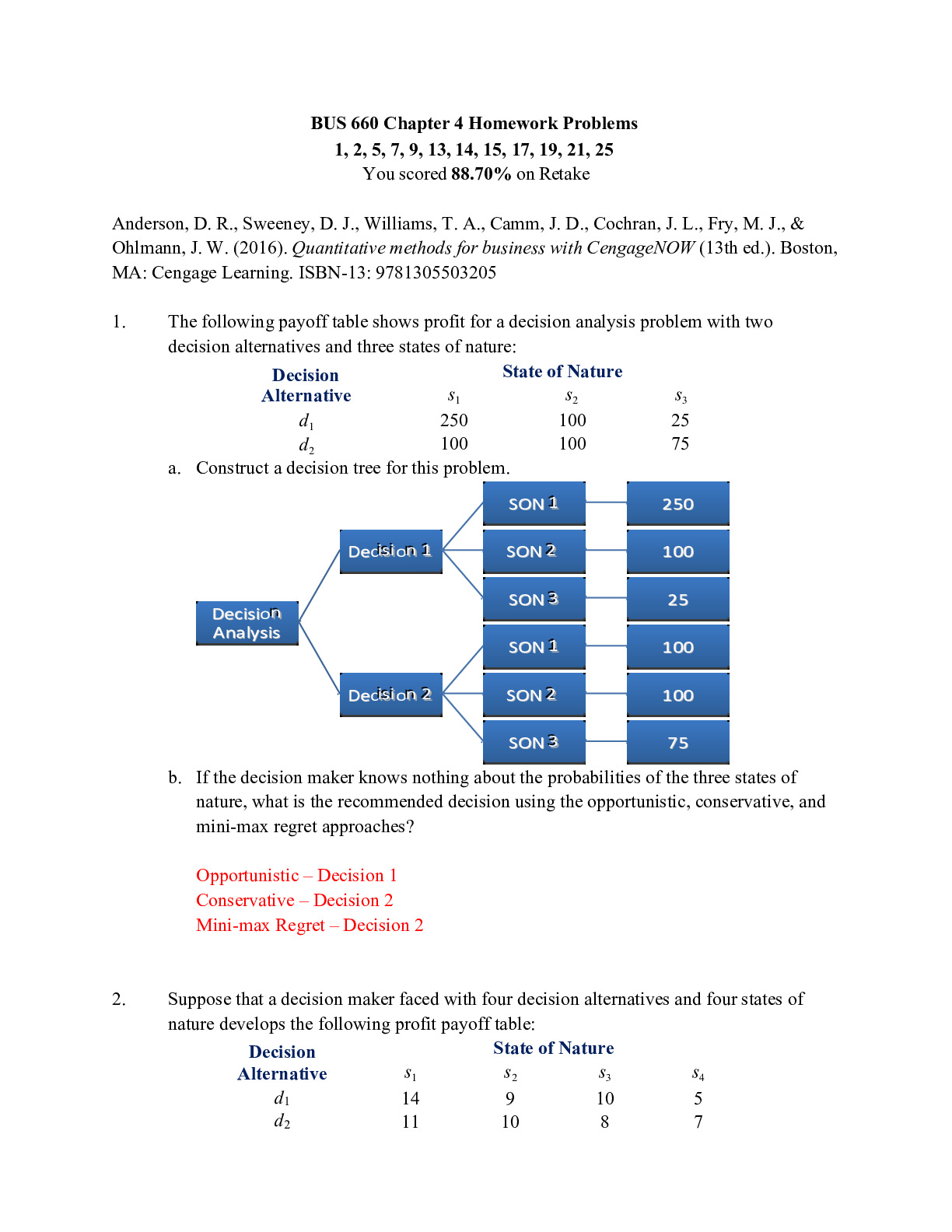
ETOH Withdrawal or Delirium? Next Gen SKINNY Reasoning Case Study Stanley Harris, 90 years old © 2020 KeithRN LLC. All rights reserved. No part of this case study may be reproduced, stored in retr... ieval system or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior written permission of KeithRN ETOH Withdrawal or Delirium? Next Gen SKINNY Reasoning Case Study Stanley Harris, 90 years old Primary Concept Intracranial Regulation Interrelated Concepts (In order of emphasis) • Clinical judgment NCLEX Client Need Categories Covered in Case Study NCSBN Clinical Judgment Model Covered in Case Study Safe and Effective Care Environment Step 1: Recognize Cues ✓ • Management of Care ✓ Step 2: Analyze Cues ✓ • Safety and Infection Control Step 3: Prioritize Hypotheses ✓ Health Promotion and Maintenance Step 4: Generate Solutions ✓ Psychosocial Integrity Step 5: Take Action ✓ Physiological Integrity Step 6: Evaluate Outcomes ✓ • Basic Care and Comfort • Pharmacological and Parenteral Therapies • Reduction of Risk Potential ✓ • Physiological Adaptation© 2020 KeithRN LLC. All rights reserved. No part of this case study may be reproduced, stored in retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior written permission of KeithRN Present Problem: You are the nurse taking care of Stanley Harris, a 90-year-old was admitted yesterday evening for syncope after falling at home where he lives alone. His head CT was negative for an intracranial hemorrhage and no other injuries were sustained. He is admitted for dehydration and electrolyte imbalances of potassium 3.3 and magnesium of 1.4 on admission. The day shift nurse reports that Mr. Harris received a liter of Lactated Ringer’s over her eight-hour shift and is alert and oriented x4. Upon your initial assessment on the evening shift, Mr. Harris is extremely pleasant. He correctly states that he is in the hospital because he fell and correctly states the date. He seems to be a little forgetful –unable to recall that you were the same nurse who admitted him yesterday until you remind him. As you are leaving the room, the patient’s daughter approaches you and says, “You know, every time my dad gets hospitalized he gets agitated and confused after a night or two. I just wanted to warn you in case he gets out of hand later tonight.” Around 8 PM, the nursing assistant notifies you that Mr. Harris is trying to pull out his peripheral IV catheter and keeps climbing out of bed. You go in to assess him and notice that he is confused, sweaty, and trembling. He is difficult to redirect and keeps saying, “Why won’t you people let me have something to drink?” even though he has ice water available at the bedside. When you ask him where he is, he states that he is in his garage. He is not able to tell you the year or why he is in the hospital. 1. What data from the present problem is RELEVANT and must be NOTICED as clinically significant by the nurse? (NCSBN: Step 1 Recognize cues/NCLEX: Reduction of Risk Potential) RELEVANT Data from Present Problem: Clinical Significance: Current VS: P-Q-R-S-T Pain Assessment: T: 97.5 F/36.4 C (oral) Provoking/Palliative: P: 114 (regular) Quality: Denies R: 20 (regular) Region/Radiation: BP: 140/93 Severity: O2 sat: 97% room air (RA) Timing: 2. What VS data is RELEVANT and must be NOTICED as clinically significant by the nurse? (NCSBN: Step 1 Recognize cues/NCLEX: Reduction of Risk Potential) RELEVANT Data from Present Problem: Clinical Significance: Recognizing a potential problem, you promptly collect a full set of VS:© 2020 KeithRN LLC. All rights reserved. No part of this case study may be reproduced, stored in retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior written permission of KeithRN Additional Information: Since you were the nurse that admitted this patient, you did a brief assessment of the patient’s social history last night. You recall that during this assessment, you inquired about alcohol use and the patient reported to you that he usually “has a nightcap or two” every single day. He denied street drug use. He denied tobacco use. Past medical history includes Afib, BPH, and coronary artery disease with stent placement in 2012. His medication list includes carvedilol, apixaban, tamsulosin, and vitamin D. He occasionally takes acetaminophen or ibuprofen for chronic lower back pain but currently denies pain. 3. What data is RELEVANT and must be NOTICED as clinically significant by the nurse? (NCSBN: Step 1 Recognize cues/NCLEX: Reduction of Risk Potential) RELEVANT Data from Additional Info: Clinical Significance: 4. Interpreting clinical data collected, what problems are possible? Which problem is priority? Why? (NCSBN: Step 2: Analyze cues/Step 3: Prioritize hypotheses/NCLEX: Management of Care) Problems: Priority Problem: Rationale: 5. What nursing priority will guide how the nurse RESPONDS to formulate a plan of care? (NCSBN: Step 4 Generate solutions/Step 5: Take action/NCLEX: Management of Care) Nursing PRIORITY: Nursing Interventions: Expected Outcome:© 2020 KeithRN LLC. All rights reserved. No part of this case study may be reproduced, stored in retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior written permission of KeithRN Situation: Name/age: BRIEF summary of primary problem: Background: Primary problem/diagnosis: RELEVANT past medical history: RELEVANT background data: Assessment: Vital signs: RELEVANT body system nursing assessment data: RELEVANT lab values: How have you advanced the plan of care? Patient response? INTERPRETATION of current clinical status (stable/unstable/worsening): Recommendation: Suggestions to advance plan of care: Use SBAR to communicate your concern to the primary care provider: The primary care provider agrees with your recommendation to implement an alcohol withdrawal protocol using diazepam. Based on his most recent MINDS assessment, you administer diazepam 10 mg PO. You continue to closely assess Mr. Harris and two hours later you collect the following assessment data:© 2020 KeithRN LLC. All rights reserved. No part of this case study may be reproduced, stored in retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior written permission of KeithRN 6. After implementing the plan of care, EVALUATE your patient by INTERPRETING relevant clinical data to determine if patient status is improving, declining, or reflects no change. (NCSBN: Step 6 Evaluate outcomes/NCLEX: Management of Care) Assessment Finding: Improving: Declining: No Change: Is less agitated and appears to be resting comfortably in bed. [Show More]
Last updated: 2 years ago
Preview 1 out of 5 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Nov 08, 2022
Number of pages
5
Written in
Additional information
This document has been written for:
Uploaded
Nov 08, 2022
Downloads
0
Views
97