*NURSING > SHADOW HEALTH > Nasogastric Intubation Skills & Reasoning Jim Sanderson, 65 years old (All)
Nasogastric Intubation Skills & Reasoning Jim Sanderson, 65 years old
Document Content and Description Below
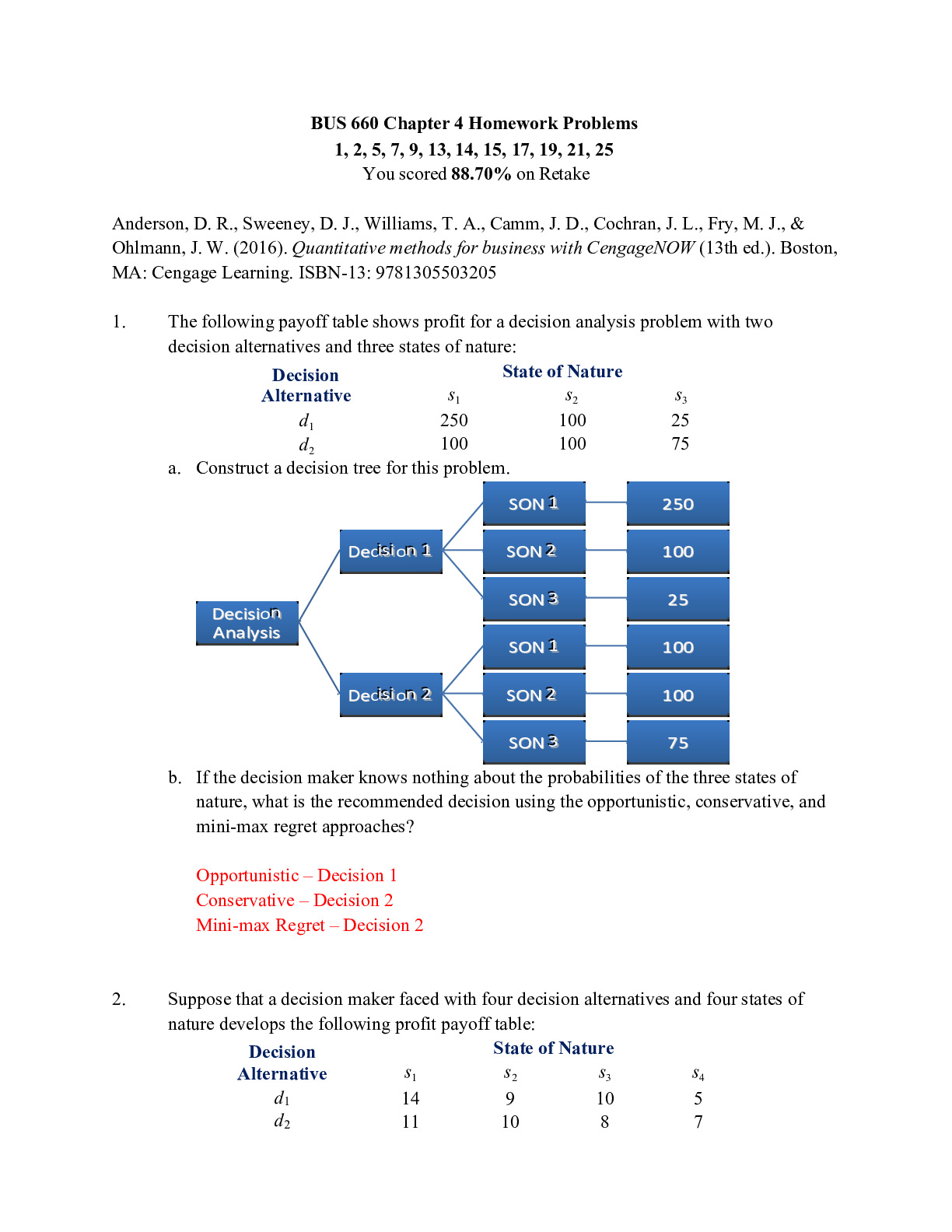
Nasogastric Intubation Skills & Reasoning Jim Sanderson, 65 years old Nasogastric Intubation Skills & Reasoning Jim Sanderson, 65 years old Primary Concept Elimination Interrelated Concepts (I... n order of emphasis) Clinical Judgment Patient Education Communication Collaboration NCLEX Client Need Categories Percentage of Items from Each Category/Subcategory Covered in Case Study Safe and Effective Care Environment Management of Care 17-23% Safety and Infection Control 9-15% Health Promotion and Maintenance 6-12% Psychosocial Integrity 6-12% Physiological Integrity Basic Care and Comfort 6-12% Pharmacological and Parenteral Therapies 12-18% Reduction of Risk Potential 9-15% Physiological Adaptation 11-17% Copyright © 2019 Keith Rischer, d/b/a KeithRN.com. All Rights reserved. This study source was downloaded by 100000826504961 from CourseHero.com on 06-20-2022 06:11:53 GMT -05:00 https://www.coursehero.com/file/72163737/clincals-day-5-jim-sanderson-1026docx/History of Present Problem: Jim Sanderson is a 65-year-old male who is admitted for acute lower abdominal pain which was the result of a ruptured appendix. He had an open appendectomy and is now post-operative day three. He refuses to use the incentive spirometer or get up in the chair and requires encouragement to get out of bed and ambulate on the unit. His appetite is poor, and he eats a small portion of his meals but tolerates and drinks fluids readily. He has had 2200 mL intake to 1800 mL urine output the past 24 hours. He denies nausea and has not had a bowel movement since surgery despite receiving milk of magnesia and senna tabs daily. His abdomen is obese, rounded, firm and tender to palpation with hypoactive bowel sounds. His incision site in his RLQ has no drainage; swelling and mild erythema along the edge of the incision. Current Complaint: Jim puts on his call light. When you arrive, he states he feels nauseated. He has an order for ondansetron 4 mg IV every 4 hours PRN for nausea, and this is administered. Thirty minutes later he puts his call light on again, stating that his nausea has gotten worse. While in the room, he begins to wretch and has a small bile green emesis. What data from the story and current complaint do you NOTICE as RELEVANT and why is it clinically significant? (Reduction of Risk Potential/Health Promotion and Maintenance) RELEVANT Data-Present Problem: Clinical Significance: Lower abdominal pain resulting from ruptured appendix- pt underwent appendectomy. Post op day 3. Noncompliant- will not use incentive spirometer or get up in the chair. Poor appetite. No bowel movement for 3 days. Tender abdomen. incision swelling and mild erythema. After appendectomy it can hurt to breath in deeply or push out air which is likely why pt is unwilling to use incentive spirometer or get up in the chair. Peristalsis does not usually occur until about 3 days after so this is normal and pt should receive an enema. RELEVANT Data-Current Complaint: Clinical Significance: Pt feels nauseated. 30 min after pt receives ondansetron he states nausea has gotten worse Ondansetron is ordered to treat pt nausea. Nursing Assessment Begins: Current VS: Most Recent VS: Current WILDA: T: 99.2 F/37.3 C (oral) T: 99.4 F/37.4 C (oral) Words: ache/cramp P: 92 (reg) P: 74 (reg) Intensity: 5/10 R: 24 (reg) R: 18 (reg) Location: generalized abdomen BP: 168/88 BP: 142/80 Duration: ongoing-started last hour O2 sat: 93% room air O2 sat: 98% room air Aggravate: movement Alleviate: rest Current Assessment: GENERAL APPEARANCE: Patient’s body and facial expression appears tense, uncomfortable RESP: Breath sounds clear with equal aeration bilaterally, diminished in the bases bilaterally, nonlabored respiratory effort CARDIAC: Skin color is pink, warm & dry, no edema, heart sounds strong, regular with no abnormal beats, pulses 3+, equal with palpation at radial/pedal/post-tibial landmarks NEURO: Alert & oriented to person, place, time, and situation (x4) GI: Abdomen firm-tender to palpation, distended, with rare, high pitched tympanic bowel sounds GU: Voiding without difficulty, urine clear/yellow SKIN: Skin integrity intact, abdomen incision edges intact with mild erythema along edges, staples intact This study source was downloaded by 100000826504961 from CourseHero.com on 06-20-2022 06:11:53 GMT -05:00 https://www.coursehero.com/file/72163737/clincals-day-5-jim-sanderson-1026docx/What clinical data do you NOTICE that is RELEVANT and why is it clinically significant? (Reduction of Risk Potential/Health Promotion and Maintenance) RELEVANT VS Data: Clinical Significance: TREND: Improve/Worsening/Stable: T: 99.2 F/37.3 C (oral) P: 92 (reg) R: 24 (reg) BP: 168/88 O2 sat: 93% room air temp is improving compared to most recent. Pulse is normal. Normal RR is 12-16- tachypnea could be a sign of illness or stress due to current situation. Bp still high due to pain level. At risk for heart attack or stroke. Tachypnea likely the cause for low o2 sat stable Worsening Worsening Worsening worsening RELEVANT Assessment Data: Clinical Significance: General Resp Gi Skin This is a sign he is in pain could possibly be complication from post op Diminished breath sounds are low could mean air or fluid in lungs. Post op comp or obstruction/constipation. Normal but monitor 1. What additional clinical data you need to collect to identify the primary problem to guide your plan of care? (Management of Care) 2. INTERPRETING relevant clinical data, what is the primary problem? What primary health related concept(s) does this problem represent? (Management of Care/Physiologic Adaptation) Problem: Pathophysiology of Problem in OWN Words: Primary Concept(s): Bowel obstruction causing nausea Constipation can lead to stomach distention and bloating. This triggers an increase of bacteria in our colon which prompts nausea. Constipation can also cause loss of appetite which explains why pt is not eating. Constipation no peristalsis due to surgery 3. What nursing priority(ies) will guide your plan of care that determines how you decide to RESPOND? (Management of Care) Nursing PRIORITY: Relieve constipation PRIORITY Nursing Interventions: Rationale: Expected Outcome: Take account of a possible laxative and enema use, type, and frequency. Request abdominal CT. One of the main reasons for enema treatment is to relieve constipation. Generally, doctors recommend other treatments, such as stool softeners or suppositories, first. But for very hard or dry stool that doesn't pass with other approaches, enemas are beneficial. Relieve constipation I can assume that this could be due to his constipation since constipation can cause nausea. Also the pt took his medication on an empty stomach. Request an abdominal CT This study source was downloaded by 100000826504961 from CourseHero.com on 06-20-2022 06:11:53 GMT -05:00 https://www.coursehero.com/file/72163737/clincals-day-5-jim-sanderson-1026docx/4. What will you communicate with the primary care provider to concisely and accurately report the current problem? Situation: I am calling about Jim Sanderson a 65 yomale the patients problem I am calling about is neausea. I have just assessed the patient personally. Vital signs are T: 99.2 F/ oral, P: 92, R: 24 (reg), and BP: 168/88. I am concerned about the respiration rate and blood pressure. Background: He is post op day 3 after an appendectomy after his appendix burst. No bowel movement and refuses to ambulate Assessment: patient is nauseous and has been administered zofran but no signs of improvement. The patient seems to be worsening. The patient is alert and oriented x4. The skin is warm and dry. The patient is not on oxygen. The patient oximeter reads 93%. His pain level is 5/10. Recommendation: I recommend, we need to continue to monitor the patients vitals, I also suggest npo due to his nausea so I recommend a NG tube and to increase his fluids and an xray to check for obstruction. Medical Management: Rationale for Treatment & Expected Outcomes Care Provider Orders: Rationale: Expected Outcome: Insert NGT to LIS NPO-may have ice chips This prevents the tube from adhering to the gut wall. The purpose of the NGT is to carry food and medicine to the stomach through the nose. NPO to prevent pt from vomiting or becoming more nauseous. Pt will no longer feel nauseated and wont vomit. In response to your concise and well organized SBAR, the primary care provider agrees with your concern and orders an abdominal CT that confirms dilated proximal small intestinal loops suggestive of paralytic ileus with no evidence of gas in the large intestine. You receive the following orders: Insert nasogastric tube [NGT] Connect NGT to LIS [low intermittent suction] NPO [nothing by mouth] except small amount of ice chips PRN [as needed] This study source was downloaded by 100000826504961 from CourseHero.com on 06-20-2022 06:11:53 GMT -05:00 https://www.coursehero.com/file/72163737/clincals-day-5-jim-sanderson-1026docx/Procedural Safety Principles 1. What supplies does the nurse need to gather to perform this skill? 2. Review nasogastric tube insertion and summarize essential steps and knowledge that the nurse will use in this scenario to safely place the tube. (Management of Care) What does the Nurse Need to KNOW to Be Safe in Practice: How will you measure the correct length to insert? Measure and mark tube by going from the nose to the tip of the ear lobe then done to the tip of the xiphoid process. Depending on facility policy we may have to add to our estimate. How will you validate that the tube is correctly placed? check for color and ph and a chest xray How many people will you need to assist you with insertion and what will their role be? Just myself and help from the pt when possible. But have another nurse in the room just in case. What other safety concerns are present? Pt may gag but this is normal. The NGT can go into the lungs causing the pt to aspirate 3. What will you communicate to the patient to educate them about the need for nasogastric tube insertion and what to expect? (Health Promotion and Maintenance) Evaluation: NGT, lubricant and guaze, emesis basin, tissues, ph testing strips, dressing, water for the patient, local anesthetic spray for t is requested. You NGT will administer food and meds directly into the stomach through your nose. This is temporary and will be removed as soon as the doctor sees improvement. After the NG tube has been placed, 800 mL of green bile drainage from the stomach is removed over the next 15 minutes. Jim states that the nausea is improved and appears to be more comfortable. This study source was downloaded by 100000826504961 from CourseHero.com on 06-20-2022 06:11:54 GMT -05:00 https://www.coursehero.com/file/72163737/clincals-day-5-jim-sanderson-1026docx/1. What data do you NOTICE as RELEVANT and why is it clinically significant? (Reduction of Risk Potential/Health Promotion and Maintenance) RELEVANT Data: Clinical Significance: 800 mL of bile was removed from the stomach over the next 15 minutes. Pt seems more comfortable and states nausea has improved. Pt was experiencing bile reflux due to bile being in his stomach this happens when the fluid from the liver aka bile is backed up and goes into the stomach. Due to this he was experiencing nausea to excrete the waste from his body. 2. Has the status improved or not as expected to this point? Does your nursing priority or plan of care need to be modified in any way after this evaluation assessment? (Management of Care, Physiological Adaptation) Evaluation of Current Status: Modifications to Current Plan of Care: After inserting the NGT 800mL of bile was removed from the pt stomach- since then the pt has verbally advised us that his nausea has improved and is more comfortable. At this moment the plan of care does not need to be modified since we are seeing progress. We will continue to monitor. 3. Based on your current evaluation, what are your CURRENT nursing priorities and plan of care? (Management of Care) CURRENT Nursing PRIORITY: Maintain fluid balance PRIORITY Nursing Interventions: Rationale: Expected Outcome: Maintain fluid balance Sufficient hydration has shown to reduce risk of nausea. No nausea and continue monitoring incision. Use Reflection to THINK Like a Nurse What did I learn from this scenario? How can I use what has been learned from this scenario to improve patient care in the future? What Did You Learn? How to Use to Improve Future Patient Care: I learned to think outside the box and not only focus on . I did not think the issue would be paralytic ileus but after thinking it through it finally made sense to me. This will help me improve pt care in the future because I am now away that this is something very possible after pt has surgery. This study source was downloaded by 100000826504961 from CourseHero.com on 06-20-2022 06:11:54 GMT -05:00 https://www.coursehero.com/file/72163737/clincals-day-5-jim-sanderson-1026docx/Nursing Plan of Care (please refer to rubric when completing this form) Patient Initials: Objective Cluster Data (for this problem) Subjective Cluster Data (for this problem) T: 99.2 F/37.3 C (oral) Words: ache/cramp P: 92 (reg) Intensity: 5/10 R: 24 (reg) Location: generalized abdomen BP: 168/88 Duration: ongoing-started last hour Aggravate: movement Alleviate: rest Nursing Problem (Diagnosis) #1: nausea related to vomiting as evidence by vomiting green bile. Goals (List one short term and one long term goal) STG: improve nausea STG Interventions (List 3, with rationales & citation) 1. Maintain fluid balance in patients at risk; sufficient hydration shows to reduce the risk of nausea. 2. Keep rooms well-ventilated. If possible, assist the patient to go outside to get some fresh air; A well-ventilated room or having a fan close by promotes easier breathing. 3. Educate the patient to take prescribed medications as ordered. Following the prescribed schedule for medications reduces episodes of nausea. LTG: Patient’s electrolyte levels will remain within normal range throughout hospital stay. LTG Interventions (List 3, with rationales & citation) 1. The nurse will measure the patient’s urinary output every 2 hours.-The nurse will measure the patient’s intake and output every 12 hours 2. The nurse will assess patients pain rating every 4 hours 3. The nurse will assess the patient energy level every shift. Evaluation: (State if goals were met/not met and why; If goal should continue/discontinue or be revised) STG: goal was met once we administered the NGT. LTG: the goal was met and we are continuing to monitor. This study source was downloaded by 100000826504961 from CourseHero.com on 06-20-2022 06:11:54 GMT -05:00Patient Initials: Objective Cluster Data (for this problem) Subjective Cluster Data (for this problem) T: 99.2 F/37.3 C (oral) Words: ache/cramp P: 92 (reg) Intensity: 5/10 R: 24 (reg) Location: generalized abdomen BP: 168/88 Duration: ongoing-started last hour Aggravate: movement Alleviate: rest Nursing Problem (Diagnosis) #2: acute pain related to tissue trauma related too appendectomy incision. Goals (List one short term and one long term goal) STG: manage incision pain STG Interventions (List 3, with rationales & citation) 1. Determine the client’s perception of pain. provides an opportunity for the client to express in their own words how they view the pain and the situation to gain an understanding of what the pain means to the client. 2. Investigate signs and symptoms related to pain. Bringing attention to associated signs and symptoms may help the nurse in evaluating the pain. 3. determine the factors that alleviate pain LTG: educate pt on long term post op care LTG Interventions (List 3, with rationales & citation) 1. Produce relaxation such as deep breathing, peaceful imaging, etc. relaxation techniques help reduce skeletal muscle tension. 2. demonstrate and practice relaxation techniques. Provides and opportunity for the nurse to evaluate pt knowledge. 3. evaluate and document his response to relaxation therapy. Evaluation: (State if goals were met/not met and why; If goal should continue/discontinue or be revised) STG: the goal has been met. Paint nausea is much better and pain level is low. LTG: n/a [Show More]
Last updated: 2 years ago
Preview 1 out of 9 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Nov 08, 2022
Number of pages
9
Written in
Additional information
This document has been written for:
Uploaded
Nov 08, 2022
Downloads
0
Views
139