Nutrition > STUDY GUIDE > Nutrition 110 Midterm Study Guide (VERIFIED) Questions and Answers elaborations | 100% correct (All)
Nutrition 110 Midterm Study Guide (VERIFIED) Questions and Answers elaborations | 100% correct
Document Content and Description Below
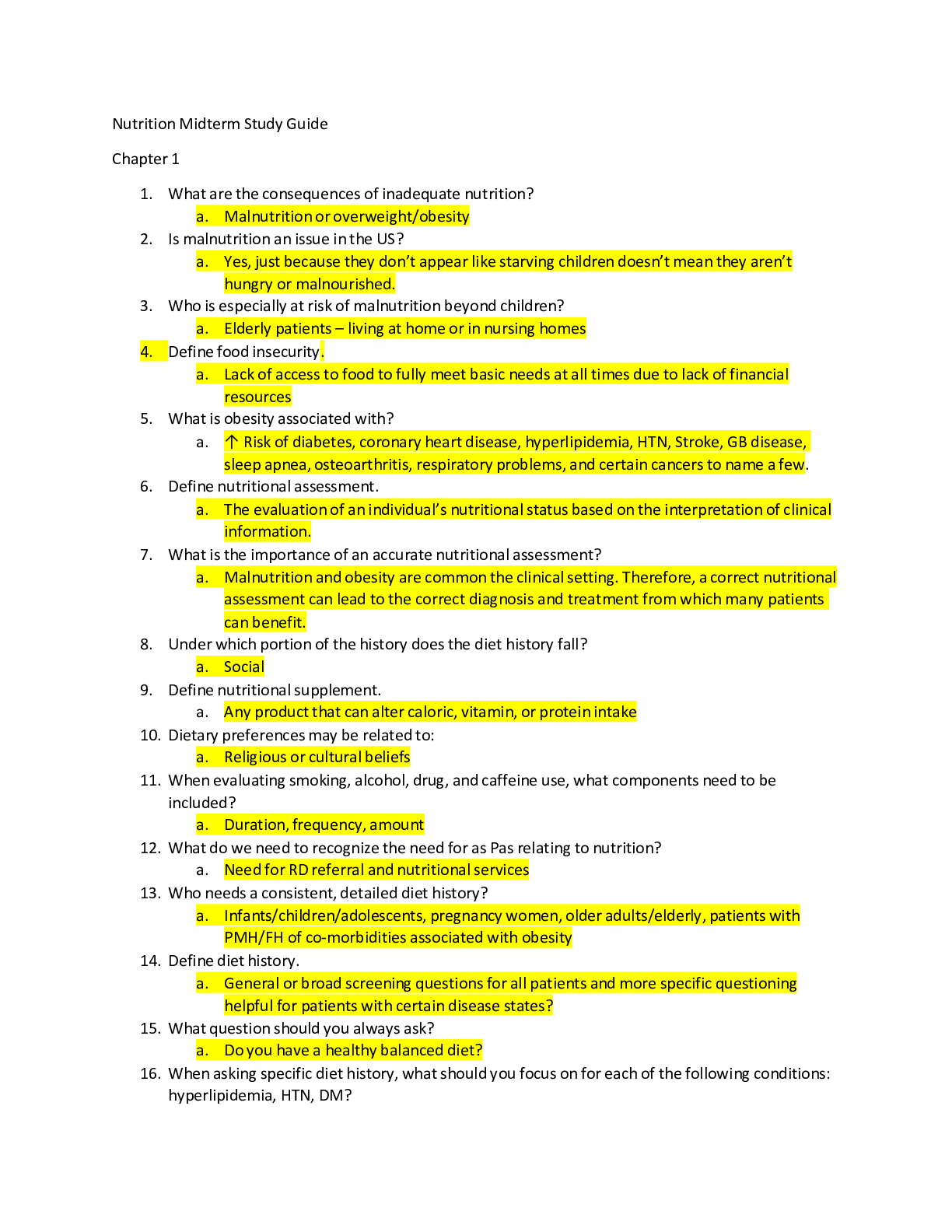
Nutrition Midterm Study Guide Chapter 1 1. What are the consequences of inadequate nutrition? a. Malnutrition or overweight/obesity 2. Is malnutrition an issue in the US? a. Yes, just because they ... don’t appear like starving children doesn’t mean they aren’t hungry or malnourished. 3. Who is especially at risk of malnutrition beyond children? a. Elderly patients – living at home or in nursing homes 4. Define food insecurity. a. Lack of access to food to fully meet basic needs at all times due to lack of financial resources 5. What is obesity associated with? a. ↑ Risk of diabetes, coronary heart disease, hyperlipidemia, HTN, Stroke, GB disease, sleep apnea, osteoarthritis, respiratory problems, and certain cancers to name a few. 6. Define nutritional assessment. a. The evaluation of an individual’s nutritional status based on the interpretation of clinical information. 7. What is the importance of an accurate nutritional assessment? a. Malnutrition and obesity are common the clinical setting. Therefore, a correct nutritional assessment can lead to the correct diagnosis and treatment from which many patients can benefit. 8. Under which portion of the history does the diet history fall? a. Social 9. Define nutritional supplement. a. Any product that can alter caloric, vitamin, or protein intake 10. Dietary preferences may be related to: a. Religious or cultural beliefs 11. When evaluating smoking, alcohol, drug, and caffeine use, what components need to be included? a. Duration, frequency, amount 12. What do we need to recognize the need for as Pas relating to nutrition? a. Need for RD referral and nutritional services 13. Who needs a consistent, detailed diet history? a. Infants/children/adolescents, pregnancy women, older adults/elderly, patients with PMH/FH of co-morbidities associated with obesity 14. Define diet history. a. General or broad screening questions for all patients and more specific questioning helpful for patients with certain disease states? 15. What question should you always ask? a. Do you have a healthy balanced diet? 16. When asking specific diet history, what should you focus on for each of the following conditions: hyperlipidemia, HTN, DM? a. Fats b. Salts c. Carbohydrates 17. Name the different questioning methods and tools available. Which as retrospective and which are prospective? a. Retrospective - 24-hour recall, unusual intake/diet history, food frequency questionnaire, b. Prospective - 3-day food record 18. What are the cons of the 24-hour recall? a. Patients may overestimate or underestimate if generalizing based on one day; relies on patient recollection 19. What is the pro to the usual intake/diet history? a. Approach provides more information about usual intake patterns, reflects longer term habits with better accuracy 20. What is the con to the usual intake/diet history method? a. Patients may only report what they know or think to be healthy 21. What is the food frequency questionnaire used for? a. Determine trends in patients’ usual consumption of specific foods; geared toward whatever condition the patient has; evaluates current intake of specific foods 22. Which method is the most accurate? a. 3-day food record 23. What is the con to the 3-day food record? a. Difficult for some patients to keep written logs 24. How do you calculate BMI? a. Weight (kg)/height (m^2) b. ((weight (lbs.))/(height (in^2)))*703 25. What is considered a normal BMI? a. 18.5-24.9 kg/m^2 26. How is energy expressed? a. Kilocalories 27. Based on 1 gram, how many kcals do you get from: protein, carbohydrate, fat, or alcohol? a. Protein – 4 b. Carbohydrate – 4 c. Fat – 9 d. Alcohol – 7 28. What equation estimates energy requirements? a. Mifflin-St. Jeor Equation 29. What is the Mifflin – St. Jeor Equation a. (10*weight in kg)+(6.25*height in cm) – (5*age in years); +5 for males; -161 for females 30. When is waist circumference helpful? a. In patients with a BMI <35 31. Why is waist circumference important? a. Independent risk factor for diabetes, dyslipidemia, HTN, CV disease 32. What are the waist circumference values? a. >102cm (40in) male b. >88cm (35in) female 33. How do you calculate percent weight change? a. ((Usual weigh-current weight)/(usual weight))*100 34. Nutrition oriented aspects of the physical exam focus where? a. Skin, hair, eyes, mouth, nails, extremities, abdomen, skeletal muscle, fat stores 35. What skin PE findings are associated with nutritional implications? a. Rashes, dermatitis, bruising, petechia, purpura, changes in pigmentation, pressure ulcers, paleness, pallor, thickening, dryness 36. What hair PE findings are associated with nutritional implications? a. Dyspigmentation, easy pluckability, alopecia 37. What head PE findings are associated with nutritional implications? a. Temporal muscle washing, delayed closure of fontanelle 38. What eye PE findings are associated with nutritional implications? a. Night blindness, xerosis, bitot spots, corneal vascularization, keratomalacia, photophobia, blurring, conjunctival inflammation, macular degeneration 39. What mouth PE findings are associated with nutritional implications? a. Angular stomatitis, bleeding gums, cheilosis, fissuring, scarlet, raw tongue, nasolabial seborrhea, dental caries, hypogeusia, glossitis, papillary atrophy/smooth tongue 40. What neck PE findings are associated with nutritional implications? a. Goiter, parotid enlargement 41. What thoracic PE findings are associated with nutritional implications? a. Rickets rosary, thoracic rachitic rosary 42. What abdominal PE findings are associated with nutritional implications? a. Abdominal obesity, diarrhea, hepatomegaly/ascites 43. What cardiac PE findings are associated with nutritional implications? a. Heart failure 44. What genital/urinary PE findings are associated with nutritional implications? a. Delayed puberty, hypogonadism 45. What extremity/musculoskeletal PE findings are associated with nutritional implications? a. Ataxia, bone ache, joint pain, bone tenderness, kyphosis, edema, hyporeflexia, growth retardation, failure to thrive, muscle wasting and weakness, tenderness of long bones, squaring of shoulders – loss of deltoid 46. What nail PE findings are associated with nutritional implications? a. Transverse lines, spooning of nails 47. What neurological PE findings are associated with nutritional implications? a. Dementia, delirium, disorientation, loss of reflexes, wrist drop, foot drop, ophthalmoplegia, peripheral neuropathy, tetany, carpopedal spas 48. Why should a nutritional assessment always be included in the H&P? a. Children – evaluate growth and development; children and adults – assess for nutrient excess/deficiency Chapter 2 1. What does RDA stand for? a. Recommended daily allowance 2. What does DRI stand for? a. Dietary reference intake 3. What does EAR stand for? a. Estimated average requirement 4. What does AI stand for? a. Adequate intake 5. What does TUL stand for? a. Tolerable upper intake limit 6. What are vitamins needed for? a. Normal growth, development, and metabolism 7. What is the best source of vitamins? a. Balanced diet 8. When do you need vitamin supplementation? a. When you’re sick 9. Where are RDA set for vitamins? a. 2SD above the mean requirement to cover the needs of practically all healthy people 10. What does the DRI focus on? a. Prevention of chronic diseases 11. What specific values does DRI look at? a. EAR, AI, TUL 12. When is EAR most helpful? a. Assessing nutrient intake of a population 13. What is adequate intake? a. Approximation of the average nutrient intake by a healthy population without increase risk 14. Define tolerable upper intake level. a. Maximum level of daily nutrient intake that is unlikely to pose risk of adverse health effects to almost all individuals 15. Which vitamins are fat soluble? a. Vit A, D, E, and K 16. Why are fat soluble vitamins dangerous? a. Can reach toxic levels if you get too much because they’re stored in the body 17. What are some of the function of vitamin A? a. Eye – maintenance of mucous membranes, cornea, and conjunctiva; night vision and perception of color in bright light b. Skin – production of keratin, normal skin integrity, and growth of skin/tissue, mucous membranes c. Reproductive- functioning of testicles and ovaries and development of embryo d. Act as antioxidant 18. What are three types of vitamin A? Where are they found? a. Retinoic acid b. Retinol – preformed vit A found in animal sources c. Carotenoids – pro vitamin A converted to retinol in body, plant source 19. What is the most active form of Vit A? a. Retinol 20. What is one of the most common deficiencies? a. Vitamin A 21. What causes Vitamin A deficiencies? a. Primary – inadequate intake b. Secondary – poor absorption 22. What clinical problems can be caused by Vit A deficiencies? a. Perifollicular hyperkeratosis b. Night blindness c. Xeropthalmia d. Impairment of the immune system 23. What is the TUL for vitamin A? a. Chronic excess >30mg/d b. Acute dose >150mg 24. What are the symptoms of Vit A poisoning? a. Carotenosis b. Bone and skin changes, liver abnormalities, HA/N, vertigo, blurred vision, lack of muscles coordination, moderate levels affect bone health, increased risk for osteoporosis c. Birth defects to developing embryo 25. What are the two forms of vitamin D? a. D2 and D3 26. What are the functions of vitamin D? a. Intestinal absorption, regulation of, and maintenance of blood calcium and phosphorus b. Immunity, neuromuscular function, blood pressure regulation, insulin production, reduction of inflammation 27. What two things are coupled closely? a. Vit D and Calcium 28. What can cause Vit D deficiency? a. Impaired availability, impaired metabolism, groups at increased risk 29. What are the clinical signs of Vit D deficiency? a. Ricketts and osteomalacia 30. What is the main problem with Vit D toxicity? a. Leads to increased Ca which can cause soft tissue calcification 31. What can too much Vit D cause? a. Children – retarded growth, rounding of skull, mental retardation, death, b. Kidney stones, N, HA, weakness, anorexia, frequent urination, weight loss, irregular heartbeat, weak bones/muscles 32. What is the composition of vitamin E? a. Alcoholic compounds 33. What are the functions of Vit E? a. Antioxidant activity b. Protection of cell membrane from oxidative damage c. Inhibition of cell proliferation, platelet aggregation, monocyte adhesion d. Assists in maintenance of fertility 34. When is the only time a vitamin deficiency occurs? a. Patients who can’t absorb fat 35. What are the clinical signs of vit E deficiency? a. Neurologic dysfunction 36. What is the TUL of Vit E? a. 1000 mg/day 37. What can vit E toxicity result in? a. Interfere with vit K formation and functioning of clotting factors – hemorrhage 38. When is vit E avoided? a. Pre/post op, patients taking coumadin 39. Who is especially susceptible to Vit E toxicity? a. Premature infants 40. How is vit K obtained? a. Diet and produced in intestinal bacteria 41. What is vit K’s function? a. Cofactor for enzyme process in the proteins involved in clotting the blood as well as bone mineralization b. Required for activity of factors 42. What are the clinical signs of deficient Vit k? a. Impaired coagulation 43. When can a vit K deficiency occur? a. Patients with fat malabsorption, prolonged antibiotics 44. What are infants given regarding Vit K and why? a. Injection b. At birth – intestinal tract lack bacteria until at least one week, liver unable to produce adequate levels of coagulation factors c. Prevent hemorrhagic disease of the newborn 45. What can too much vit K causes? a. Will just get rid of it in stool b. Mega doses – allergic reactions and jaundice in newborn 46. What is the TUL for vit K? a. There isn’t one. 47. What is the least stable vitamin? a. Vitamin C 48. What is Vitamin C also known as? a. Ascorbic acid 49. What are the functions of vitamin C? a. Formation of collagen, strengthening of bones and blood vessels b. Anchoring teeth into gums c. Forming substance necessary for body growth, tissue repair, wound healing d. Synthesis of neurotransmitters e. Antioxidant activity 50. Who is at risk of vit C deficiency? a. Individuals without access to fresh citrus fruits or juices, severe burns, fractures, pneumonia, rheumatic fever, post-op, heavy alcoholics and smokers 51. Why does alcohol cause Vit C deficiency? a. Decreases absorption 52. What are the clinical signs of Vit C deficiency? a. Scurvy 53. What is the TUL for vitamin C? a. 2000mg/day 54. Why can vitamin C cause problems? a. Metabolized to oxalic acid 55. What are the clinical signs of Vit C toxicity? a. D/N, stomach cramps, kidney stones, iron overload 56. What is another name for vitamin B1? a. Thiamine 57. When is absorption of Vitamin B1 reduced? a. Alcohol and folate deficiency 58. What are the functions of Vitamin B1? a. Essential part of enzymes that play key role in production of energy from carbohydrate and protein 59. Why is Vitamin B1 deficiency rare in the US? a. Grain products are fortified 60. What is a vitamin B1 deficiency known as? a. BeriBeri 61. Why may vitamin B1 be deficient in alcoholics? a. Significant decrease thiamine absorption and interferes with metabolism? 62. What is advanced vitamin B1 deficiency characterize by? a. Neurological and CV changes 63. When is thiamine given to alcoholics promptly? a. Showing signs of acute mental status change 64. What are the two forms of BeriBeri? a. Dry and wet 65. What are the symptoms of dry BeriBeri? a. Painful tender muscles, foot drop, numbness, burning, tingling, confusion, emaciation, inability to speak, wrist drop, great weakness 66. What are the symptoms of wet BeriBeri? a. Right heart failure, edema 67. What is another name for vit B2? a. riboflavin 68. What are the functions of riboflavin (vit B2) a. Normal growth and development b. Breakdown of glucose to yield energy in all cells c. Facilitation of glycogen production and digestion of fats d. Synthesis of niacin from tryptophan e. Maintenance of normal mucous membranes f. Protection of nervous system, skin, and eyes g. Metabolism of Vit K, Folate and pyridoxine 69. When does Vit B2 deficiency occur? What is it a result of? a. In conjunction with deficiencies of other water soluble vitamins b. Inadequate intake, lack of absorption, poor utilization, increased secretion 70. What are the clinical signs of Vit b2 deficiency? a. Mouth – inflammation of oral mucosa/tongue, cheilitis, stomatitis, glossitis b. Skin – seborrheic dermatitis c. Eyes – blood short, itchy, water, sensitive to light d. Blood – normocytic anemia 71. What is the TUL for Vit B2? a. There is none. 72. What are the two forms of B3? a. Nicotinic acid b. Nicotinamide 73. What are the functions of vit B3? a. Normal enzyme production of over 200 reactions in the body with energy production 74. Why is a Vit B3 deficiency rare in US? a. Protein rich diets 75. When can a Vit B3 deficiency occur? a. Contributed by Vit B6 deficiency b. Alcoholics – decreased absorption 76. What are the signs of a Bit B3 deficiency? a. Fatigue, loss of appetite, GI disturbance, anxiety, depression, irritability, weakness 77. What a severe deficiency of Vit B3 called and what are the symptoms? a. Pellagra – diarrhea, rough skin, pigmented rash in sun exposed skin, inflammation of mucous membranes and mouth – magenta tongue, dementia, and if untreated death 78. What is the TUL for Vit B3 and what can passing this cause? a. 35mg/day b. Increased LFT c. Increased bowel sounds 79. What do excessive levels of Vit B3 cause? a. N/V, metabolic acidosis, EKG abnormalities 80. What are pharmacologic doses of Vit B3 used for? a. Treat cholesterol 81. What is vitamin B7 also known as? a. Biotin 82. What is the function of Vitamin B7? a. Plays a role in glucose synthesis 83. What is the toxic level of Vitamin B7? a. There is none. 84. What are the symptoms of a vitamin B7 deficiency? a. Inflammation of the skin, hair loss, muscle pain, increased skin sensitivity, loss of appetite/N, metal problems, increased cholesterol, decreased hemoglobin 85. What is Vit B6 also known as? a. Pyridoxine 86. What are the functions of Vitamin B6? a. Various reactions including AA b. Synthesis of serotonin, dopamine, NE and histamine c. Heme synthesis d. Conversion to niacin e. Breakdown of glycogen f. Conversion of homocysteine 87. When can a Vitamin B6 deficiency occur? a. Side effect of medications 88. What are the signs of a VitB6 deficiency? a. Cheilosis, glossitis, pellagra like dermatitis, depression, confusion, EEG abnormalities 89. What is the TUL for Vit B6? a. 100mg/day 90. What is the mega dose for Vit B6? a. 500mg/day 91. What does a megadose of Vit B6 causes? a. Photosensitivity, polyneuropathy, failure of muscular coordination, and sensory nerve damage 92. Where does Vit B12 come from? a. Animal products and fermented foods, produced a bacterial fermentation 93. What does VitB12 require for absorption? a. Intrinsic factor and stomach acid 94. What are the functions of VitB12? a. Cell replication and neurological function b. Required for folic acid supplementation 95. What is a Vit B12 deficiency called? a. Pernicious anemia 96. What patients are at risk for VitB12 deficiency? a. Vegetarians, vegans, those without intrinsic factor 97. What is the TUL for VitB12? a. There isn’t one. 98. What are the S&S of VitB12 deficiency? a. Megaloblastic anemia, nerve damage, swollen painful red tongue, long term and untreated causes irreversible damage to peripheral nerves and spinal cord causing ataxia, loss of vibratory sense, dementia 99. What are the sources of folate? a. Plant or animal sources 100. What are the functions of folate? a. Synthesis of DNA/RNA, cell division, growth and development, synthesis of heme for foundation of blood vessels 101. What has folic acid supplementation in early pregnancy has been shown to? a. Prevent neural tube defects 102. What can cause a folate deficiency? a. Suboptimal dietary intake of folate, inadequate absorption, inadequate utilization, increased demands, increase losses 103. What is a common cause of folate deficiency? a. Alcoholics 104. What does a lack of folate result in? a. Affects cell division resulting in abnormalities in RBC formation 105. What are the symptoms of folate deficiency? a. Macrocytosis, weakness/fatigue, irritability, HA, palpitations, SOB 106. What is the TUL for folate? a. 1mg/day 107. Why is there a TUL for folate? a. Excessive consumption of folic acid may mask VitB12 deficiency allowing neurological sxs to progress even though the anemia with this deficiency resolves 108. What are the functions of VitB5? a. Convert food to usable energy b. Make and break down fats c. Make cholesterol, steroid hormones, NT, and hgb d. Help the liver break down certain drugs and toxins 109. What is the TUL for Vit B5? a. There is none 110. Where is calcium found? a. Bones and teeth 111. What is calcium’s absorption regulated by? a. Vitamin D 112. What are the functions of Calcium? a. Bone mineralization b. Maintenance of cell membrane permeability c. Muscle contraction d. Blood clotting e. Nerve impulse conduction 113. What are the signs of toxic calcium levels? a. Dehydration b. Lethargy c. Nausea and vomiting (N/V) d. Anorexia e. Possible death 114. What is the TUL for calcium? a. 250mg/day 115. What are the signs of calcium deficiency? a. Irritability, pins & needles in hands & feet (paresthesia), muscle cramps and twitching + possible seizures b. In long run osteoporosis, fractures, loss of height c. Rickets (mainly vitamin D) 116. What are the functions of magnesium? a. Competes with Ca for same absorption sites b. Absorb enhanced by vit D c. Found in bone/muscle/ intra and extra cellular fluid d. 1% found in blood 117. What are the clinical signs of Magnesium deficiency? a. Fatigue, lethargy, weakness, poor appetite, impaired speech, anemia, irregular heartbeat, tremors, failure to thrive b. Advanced – rapid heart rate, cardiac fibrillation, convulsions 118. What are clinical signs of Magnesium toxicity? a. Diarrhea, changes in mental status, muscle weakness, nausea, low BP, difficulty breathing, irregular heartbeat 119. What are the functions of Magnesium? a. 100s of ATP requiring rxns b. Transmitting neural impulses eliciting muscle contractions c. Component of bones & teeth d. Protein synthesis / cell replication e. Suppressing PTH secretion 120. What is the TUL for Magnesium? a. 350mg/day 121. What is the most abundant mineral in our body? a. Calcium 122. What is the second most abundant mineral? a. Phosphorus 123. Where is phosphorus located? a. Present in bones & teeth, phospholipid proteins, carbs, enzymes, DNA, & ATP 124. What are the functions of phosphorus? a. Normal construction of bones & teeth b. DNA & RNA synthesis c. Energy synthesis (ATP/ ADP) d. Metabolism of protein, fat, carbs e. Maintenance of body normal PH f. Normal cell membrane structure 125. What are the clinical signs of phosphorus toxicity? a. Seen in patients with renal failure, precipitates metastatic calcification b. ↑ levels assoc with ↑ risk of CVD + mortality 126. What are the signs of phosphorus deficiency? a. Weakness, anorexia, bone pain, proximal muscle myopathy b. Prolonged rickets/ osteomalacia 127. When is phosphorus deficiency seen? a. Alcoholics and with ketoacidosis 128. What is the result of hypercalcemia? a. Death 129. What are the functions of iron? a. Synthesis of hemoglobin & myoglobin b. Synthesis of cytochrome protein c. Metabolic reactions d. Electron transport e. Drug detoxification 130. What indicates toxic fe levels? a. deposition of iron in tissues/cells b. Hereditary hemochromatosis causes increased absorption of iron = bronze pigmentation in skin, damaged liver and pancreas tissue, and may cause diabetes c. Tissue damage results 131. What causes Fe deficiency? a. Very prevalent worldwide b. Caused by blood loss, decreased oral intake, or diet low in bioavailable iron 132. What are the signs of iron deficiency? a. Signs: weakness, fatigue, poor work performance, adverse pregnancy outcomes, developmental delays, cognitive impairment b. Microcytic anemia c. Poor capillary bed refill d. Pale mucosa e. Soft, concave & brittle nails f. Infants / children low IQ, learning & behavior problems g. Fatigue h. Feelings of faintness i. Cold/abnormal sensation in extremities j. Dyspnea (SOB ?) k. ↑ susceptibility to infections 133. What is the TUL for Fe? a. 45mg/day 134. Where is zinc found in our body? a. Prostate b. Skin c. Brain d. Liver e. Pancreas f. Bone g. Blood 135. What are the functions of zinc? a. Co-factor for enzymes in carb, fat, protein metabolism b. Cell division, growth, repair- all life stages-esp during fetal growth c. Synthesis of DNA/ RNA/ gene regulation d. Normal immune FXN- wound healing e. Sexual maturation, fertility, reproduction f. Maintenance of normal taste and smell 136. What indicates a zinc deficiency? a. Poor appetite b. Changes in taste perception c. Anosmia (loss of smell) d. Hair loss e. Skin problems f. Poor wound healing g. Impaired immunity h. Growth retardation i. Corneal edema / opacification 137. What indicates zinc toxicity? a. Rare b. Causes: diarrhea, nausea, vomiting c. Can impair copper status d. Depress immune function e. High doses assoc with Urinary Tract Infections 138. What are the functions of copper? a. Production of skin, hair, eye pigmentation b. Synthesis of connective tissue c. Protection of cells from oxidative damage d. Maintenance of myelin sheath surrounding nerves e. Functioning of nervous system f. Promotion of Fe metabolism 139. What is Wilson’s disease? a. genetic syndrome b. Copper deposition in brain, kidney, cornea, & liver with decreased blood Copper levels 140. What are indications of copper deficiency? a. Anemia b. Connective tissue damage c. Lung damage d. Excessive bleeding 141. What are indications of copper toxicity? a. Nausea/ vomiting b. Diarrhea c. Anemia d. Anuria e. Death in extreme cases 142. What are the functions of sodium? a. Regulates hydration and cell membrane potentials (with Chloride) b. Predominant extracellular cation 143. What indicates Na deficiency? a. HA, N/V, muscle cramps, fainting, fatigue, & death 144. What can cause Na deficiency? a. Can occur with prolonged vomiting, diarrhea, excessive or persistent sweating 145. What indicates Na toxicity? a. Symptoms: vomiting, diarrhea, excess sweating, mental status changes due to cerebral edema, seizures, and death 146. What causes Na toxicity? a. Dehydration 147. What is low serum sodium called? High serum sodium? a. Hyponatremia, Hypernatremia 148. What are the functions of Selenium? a. Protects cells from free radicals b. Normal fxn of immune system & thyroid c. Antioxidant properties 149. When is selenium deficiency seen? a. Seen in patients on Total Parenteral Nutrition (TPN) as only source of nutrition b. Signs of deficiency seen only in counties where content in the soil is low and intake of selenium in domestic animals is rare 150. What are the signs of selenium deficiency? a. Children develop enlarged heart and poor cardiac function 151. What is the TUL for Selenium? a. 400ug 152. What are the symptoms of selenium toxicity? a. Symptoms: GI upset, joint pain, hair loss, nail discoloration, and fatigue b. Acute toxicity respiratory distress, acute Myocardial Infarction, renal failure 153. When has selenium toxicity been seen? a. Manufacturer error 154. What is the function of fluoride? a. Increase tooth mineralization & bone density b. Reduce risk & prevalence of dental caries c. Promote enamel remineralization 155. Where is fluoride found? a. Found in varying concentrations in water and soil b. Public water- fluoride added 156. What is toxicity by fluoride called and what are the symptoms? a. Fluorosis b. Mild – chalky white spots c. Severe – brown spots d. Highly resistant to dental cavities 157. What are the functions of iodine? a. Essential for humans as component of thyroid hormones 158. Where is iodine stored in the body? a. 40% body’s iodine stored in thyroid gland 159. What does an iodine deficiency cause? What are the symptoms? a. Causes a decrease in thyroid hormones goiter b. Symptoms: lethargy, dry skin, thick lips, enlarged tongue, reduced muscle and skeletal growth, mental retardation 160. What do toxic levels of iodine cause? a. Excessive dietary intake inhibition of thyroid hormone synthesis b. When blood levels too high, iodine absorption is low- so you can see Goiter 161. What is the TUL for iodine? a. 1100 ug/day 162. What are the functions of chromium? a. Hypothesized to potentiate the action of insulin b. “identified as glucose tolerance factor” 163. What do deficient levels of chromium causes? a. No deficiency defined. 164. What do toxic levels of chromium causes? a. There isn’t a toxic level. 165. What is the main source of chromium? a. Drinking beer out of a can Chapter 3 1. What is considered to be normal weight gain in pregnancy? a. 20-30lbs 2. What changes need made in the diet for pregnancy? a. Increased folic acid and iron, increased caloric intake by 300cal/day, increased need for water 3. When is the ideal time to start counseling regarding pregnancy? a. Pre-pregnancy, when you hear a couple is trying to conceive 4. What nutritional assessments need included in pregnancy? a. Clinical, dietary, and lab components 5. What is severe N/V in pregnancy called? a. Hyperemesis gravidarum 6. What trimester is the most important regarding weight gain? a. 2nd 7. Where is weight gain in the mother occurring? a. Increase in tissue, blood volume, breast mass, uterine size, and feto-placental growth 8. Weight gain in the first half of the pregnancy most reflects while changes in the 2nd half reflect . a. Changes in the mother, continued maternal and fetal growth 9. What does rapid weight at >32 weeks indicates? a. Edema 10. What is the recommended weight gain for underweight, normal weight, overweight, and obese patients? a. Underweight – 28-40 lbs. b. Normal weight – 25-35 lbs. c. Overweight – 15-25 lbs. d. Obese – 15lbs. 11. What are overweight and obese patients at risk of? a. Gestational diabetes and HTN, thromboembolic evens, pre-eclampsia, macrosomia, and risk of C-section 12. What does a rapid excessive weight gain indicate? a. Fluid retention/development of pre-eclampsia 13. What does a slow excessive weight gain indicate? a. Fat deposition 14. What weight gain is recommended for an adolescent pregnancy? a. 28-40 lbs. 15. What do you need to be screening for in pregnancy? a. Anemia, gestational diabetes, urinary screening (from DM, renal disease, and increased protein indicating pre-eclampsia) 16. Routine vitamin and mineral supplementation for women reporting appropriate dietary intake and demonstrating adequate weigh gain without edema is still recommended. True or false? a. False 17. What food needs eliminated in pregnancy and why? a. Fish - heavy metals 18. How do the caloric needs change in each semester? a. 1st – none b. 2nd – additional 340kcal/day c. 3rd – additional 452kcal/day 19. When does the neural tube develop? a. 18-26 days of pregnancy 20. How do protein needs change? a. 46g/day to 71g/day in all three semesters 21. What is the total maternal energy requirement for full term pregnancy? a. 80,000 calories 22. What is the RDA of folic acid for pregnancy women? a. 600ug 23. What are the recommendations regarding hydration during pregnancy? a. At least 64 oz of water/day 24. What are the recommendations regarding caffeine during pregnancy? a. No more than 200mg/day 25. What is a known teratogen to the baby? a. Alcohol 26. Cigarette smoking is known to cause? a. Low neonatal weight 27. Why can heavy metals do to the fetus? a. Neurotoxic effects 28. What are some common nutrition related problems in pregnancy? a. N/V/C b. Heartburn and indigestion 29. When do you screen for GDM? a. 24-28 weeks 30. How do you screen for gestational diabetes? a. Glucose clearance tests 31. Following what surgery may there be nutritional defects in pregnancy? a. Bariatric surgery 32. With what vitamins/minerals are there high nutritional needs? a. Iron, B12, folate, vitD, calcium 33. How long should a woman delay pregnancy following gastric bypass surgery? a. 12-18 mos. 34. When does body prep for lactation? a. During pregnancy 35. What are the two roles of the mammary glands? a. Provide nourishment and transfer antibodies 36. What are three stages of lactation? a. Mammogenesis: mammary growth and development b. Lactogenesis: initiation of milk secretin c. Galactopoiesis: maintenance of established milk secretion 37. What hormone is necessary for milk production? a. Prolactin 38. What maintains milk production? a. Usage of milk by the infant 39. What will improve milk supply? a. Positive thoughts 40. What is released during nipple stimulation, the expectation of nursing or the sound of a baby crying? a. Oxytocin 41. What one thing is lacking in natural breast milk? a. Vitamin D 42. What will negatively affect breast milk production? a. Restricting caloric intake 43. What are the three types of breast milk? Describe. a. Colostrum – first yellowish milk produced at the end of pregnancy and first few days after delivery b. Foremilk – from front of breast, more water based c. Hindmilk – from back of breast, more fat based 44. When are the concentration of antibodies highest in breast milk? a. First week 45. What helps provide immunity for the infant? a. Lactobacillus bifidus b. Lysozyme c. Lactoferrin d. Interferons 46. Studies have proven the decreased incidence of what in relation to breast feeding? a. Allergies, bacterial and viral infections, severe diarrhea, necrotizing entercolitis, TB, neonatal meningitis 47. What are some of the advantages for the mother regarding breast feeding? a. Economical b. Helps contract the uterus c. Promotes mother infant bonding d. Maternal GI motility enhanced e. Ovulatory cycles delayed f. Protect against female cancers 48. What are some of the disadvantages for the mother? a. Inconvenient, tiring, if had a c-section = pain, decreased bone mineral content, your partner can’t help 49. What are some of the advantages for the infant? a. Ideal food b. Decreased incidence of many diseases c. Promotes infant mother bonding d. Improved cognitive development and intelligence 50. What are the AAP recommendations regarding breast feeding? a. Exclusive breast milk for first 6mos. b. Breast milk + introduction of solid foods for 6mos-12mos. c. After 1 yr, breast milk continued if mutually desired 51. What does the WHO recommend regarding breast feeding? a. Same as AAP but continue breast feeing up to 2 yrs. 52. What is contraindicated in breast feeding? a. Street drug use, alcohol abuse, leukemia type 1, breast cancer, active herpes simplex of breast, active TB, galatosemia in infant, mother taking chemo or radiation 53. When does in infant have trouble with breast feeding? a. Premature, ill, weakness, clef palate, choanal atresia, PKU 54. How much must a mother increase food intake for breast feeding? a. 500kcal/day 55. What can cause low milk supply? a. Failure to empty breasts b. Emotional problems c. Medical complications d. Complementary formula or food e. Illness f. Pregnancy 56. How can you tell if the baby isn’t getting enough milk? a. Weigh infant before and after feeding or weight wet diapers b. How many wet diapers is baby making per day? 57. How can you trick your body into making more milk? a. Pumping 58. What pathogen is mastitis caused by? a. Staph aureus 59. Why is breast milk called liquid gold? a. So many uses have been discovered Chapter 4 1. Define infancy, toddler, preschooler, middle childhood, pre-adolescence, and adolescence. a. Infancy – birth to 12mos. b. Toddler – 1-3yo c. Preschooler – 3-5yo d. Middle childhood – 5-10yo e. Pre-adolescence – 9-11, 10-12 f. Adolescence – 11/12 – 21 2. What are the nutritional assessments for this age group? a. Anthropometric data b. Biochemical data c. Clinical/physical observations d. Diet History + PMH 3. What anthropometric data assessment do we use? a. Growth charts 4. Define growth chart. a. combined growth patterns of breast and formula fed infants in all racial and ethnic groups 5. When assessing a child’s growth, what should we be looking at? a. Patterns 6. What is the cornerstone of pediatric nutritional assessment? a. Growth and development 7. What does the growth pattern depict? a. Nutritional status 8. When does a newborns weight double? a. By 4-6 mos 9. When does a newborn’s weight triple? a. By 1 year 10. Typically, there is a weight and length increase how often in infants? a. Monthly 11. Describe the growth of toddlers. a. gain ~ 6 lbs (2.7 kg) per year b. grow ~4.8 in (12.2 cm) per year 12. Describe the growth of preschoolers. a. gain ~4.4 lbs (2 kg) per year b. grow ~2.75 in (7 cm) per year 13. Describe the grow of school age children. a. gain ~ 7 lbs (3-3.5 kg) per year b. grow ~2.5 in (6 cm) per year 14. When is the linear growth velocity at it’s greatest? a. 9.5-14.5 years female b. 10.5-17.5 years male 15. Females increase in mass while males increase in mass. a. Fat, muscle 16. What percentiles are considered to be within normal limits? a. 10th-90th 17. What is under the 5th percentile defined as? a. Underweight 18. What is between the 85th-95th percentile defined as? a. At risk for overweight 19. What is above the 90th percentile defined as? a. Overweight 20. BMI is more predictive of? a. Body fat 21. When does BMI reach its lowest? a. 4-6yo 22. What may reflect an increase in body fat? a. An annual increase of four units in the BMI 23. What is considered to be a normal BMI? a. Greater than the 5th and less than the 85th percentile 24. What is the goal in looking at BMI? a. Strive for BMI for age in normal range, not a specific BMI value 25. What lab test is an indication of poor nutritional status? a. Hypoalbuminemia 26. What is commonly used as an assessment of nutritional status and protein status? a. Albumin 27. When should a fasting glucose be done? a. Overweight plus 2 other risk factors 28. When do you begin screening high risk children for lipids? a. 2yo 29. Who has an increased risk for iron deficiency and why? a. Overweight and obese children – eating a lot of calories but not a lot of iron 30. When do the proteins needs, comparing males and females, change? a. Around age 14-18 31. Energy needs / kg of body weight are highest when? a. Infant 32. Energy requirements are based on? a. LBM, activity level, illness, growth patterns 33. Define the recommended carbohydrate requirements. a. Same as those for adults 34. Most of an infant’s energy should come from? a. Fat 35. What is the potential problem with low fat diets? a. Have low vitamin and mineral content 36. What is the recommendation for those 12mos+ regarding VitD? a. Obtain via food sources and sun exposure 37. What do we need to supply to breast fed infants and infants no consuming 1 Liter fortified formula/day? a. 400 IU VitD 38. What can the result of too much fluoride be? a. Tooth discoloration 39. When is a fluoride supplement needed? When is it not? a. If water consumed by nursing mother is not fluoridated, if water consumed by nursing mother is fluoridated 40. Who needs iron supplementation as an infant? a. Full term until 4mos. b. Preterm 41. What are the AAP recommendations regarding breast feeding? a. Exclusive breast feeding for the first six months and continue to 1yr with addition of solid foods 42. How often should an infant be breast fed? a. First few weeks, 8-12 times/day, every 2-3 hours, 10-15 minutes/breast 43. What determines the adequacy of milk volume? a. Growth rate and health status 44. Why is it better to breast feed than formula? a. Nutrients are more bioavailable in breast milk than formula 45. What is special about formulas? a. They’re modeled after breast milk 46. When is it okay to give cow’s milk? a. At 1 year of age 47. What types of milk are given at what ages? a. Breast milk/formula – birth to 12mos. b. Whole cow’s milk 1-2 yo c. Reduced fat cow’s milk 2-5yo 48. Why should you continue with Whole cow’s milk until 2yo? a. Mimics breast milk 49. When do you start weaning to a cup? Finish weaning? a. 6-8mos, 12-24mos 50. How much juice should an infant/child be allowed? a. 4oz 51. When can solid foods be introduced? (2 options) a. 6mos b. When they can hold their head up 52. How should solid foods be introduced? a. 1 at a time; no more than every 2-3 days 53. How many times do new foods have to be introduced for a child to be accepting? a. 5-10 times 54. What foods will an infant start with (in order)? a. Iron fortified baby cereal b. Fruits c. Vegetables d. Protein e. Fat 55. When should intake not be limited? a. Before 2 yo 56. When can juice be offered? a. 6mos 57. What foods should be omitted from an infant’s diet? a. Concentrated sweets b. Products with sugar alcohols (sorbitol) that may cause diarrhea c. Canned vegetables contain too much sodium. d. There is a botulism risk with honey and corn syrup. e. Choking hazards from hot dogs, cherries, gum, hard or gel-like candies, marshmallows, nuts, peanut butter, popcorn, raw celery, whole beans, and whole grapes 58. What are the eight most common food allergies? a. Peanuts b. Eggs c. Tree nuts (walnuts or cashews) d. Milk e. Shellfish f. Fish g. Wheat h. Soy 59. Define: adverse reaction, food hypersensitivity, food anaphylaxis, food intolerance. a. Adverse reaction – clinically abnormal response b. Food hypersensitivity – immunological response c. Food anaphylaxis – classic allergic response d. Food intolerance – general term describing abnormal physiological response 60. What is child malnutrition a result of? a. A poor or sub-optimal diet b. Inadequate or excessive caloric intake c. Specific nutrients may be inadequate or unbalanced 61. What is the effect of missing meals and why? a. Missing meals, especially breakfast, affects behavior and academic performance. b. Low blood glucose, smaller glycogen stores 62. Is there evidence that sugar causes hyperactivity? a. No 63. What are the genetic and environmental factors for childhood obesity? a. Parental obesity – need to act as role models b. Poor diet c. Physical inactivity 64. Compared to their normal weight peers, obese children: a. Diminished academic achievement b. Lower household incomes c. Higher rates of household poverty 65. Describe adolescent energy needs. a. Much lower per kg than infants and children 66. What do adolescent boys need? Girls? a. Boys – increases kcal/protein b. Girls – increase protein/Fe 67. When do adolescents have increased energy/nutrient needs? a. Growth spurts 68. What are some common lifestyle issues associated with nutrition and adolescence? a. Tendency to skip meals b. Insufficient funds and opportunities to purchase food outside the home or school c. Increased consumption of “junk food” and sweetened beverages (esp males) d. Tendency to diet e. Changes in physical activity f. Exploration of dietary restrictions and fad diets 69. What are the s/s of eating disorders? a. Dysfunctional eating habits b. Body image misperception c. Rapid wt loss 70. What are the consequences of adolescent obesity? a. Stop growing at a shorter height b. Greater bone and muscle mass to support weight, thus “stocky” appearance c. Abnormal blood lipid profile d. Increases the risk for high blood pressure, type 2 diabetes, and respiratory disease e. Psychological Development - Emotional and social problems/Stereotypes and discrimination Chapter 5 1. Who accounts for much of the population right now? a. Older adults 2. Define early adulthood, midlife, and later adulthood. a. Early adulthood: 20/22-39 b. Midlife: 40-64 c. Older adults: 65+ 3. What provides the greatest income for the older adults? a. Social security 4. Why are health care resources greater in the older adults? a. Multiple chronic problems 5. How do the physiological changes of older adults affect pharmacology? a. Change in drug metabolism 6. What causes older adults to not want to eat? a. Change in taste and smell 7. What four chronic diseases cost most deaths? a. Heart disease, cancer, stroke, and diabetes 8. What are the top three chronic conditions seen in older adults? a. HTN, hypercholesteremia, arthritis 9. How do chronic conditions and nutrition relate? a. Put them at risk for poor nutritional status 10. What role does epigenetics play? a. We know we are prone to different diseases but there are things we can do to prevent it 11. % of adults have at least one chronic condition; % have 2+ chronic conditions. a. 80, 65 12. What are the eight things that can contribute to poor nutritional status in older adults? a. Chronic conditions b. Oral health problems c. Cognitive and emotional impairment d. Isolation e. Alcohol and drug abuse f. Socioeconomic status g. Functional status h. Polypharmacy 13. How does oral health problems contribute to their nutritional status? a. Poor teeth = go for soft fattier foods easier to chew, not getting protein 14. How does isolation contribute to their nutritional status? a. Don’t feel safe out with the general public because they are embarrassed of their impairments 15. What is considered risky alcohol use? a. 7drinks/week or >3 drinks/day 16. How does socioeconomic status affect nutrition? a. Stigma with welfare so they don’t reach out for help; taught to work for what you get 17. What ADL’s have a direct effect on nutritional status? a. Eating, walking 18. What IADL’s have a direct effect on nutritional status? a. Shopping, food preparation 19. How many older adults take a least 1 prescription medication? a. 89% 20. How many older adults take 4+ meds/day a. 60-70% 21. What are two examples of screening tools used for older adults? a. DETERMINE b. SNAQ 22. What is the minimum calories an older adult needs? a. 1200kcal/day 23. Define lean body mass. a. Total body weight – body fat weight 24. Adults use a range of kcal/kg/day. a. 20-35 25. A majority of protein should be from? a. High biological value protein 26. We need to make sure older adults are aware of what type of proteins? a. Complementary 27. What older adults need more protein? a. Ill/compromised medical status 28. Why can getting enough protein be a problem for older adults? a. Expense, loss of appetite, difficulty chewing 29. What is the RDA minimum for carbs for older adults? a. 130g/day 30. 50% of kcal from carbs for older adults should come from? a. Complex carbs 31. What are the fiber recommendations? a. 25-35g/day 32. Which fats should we recommend? Which should be avoided? a. Recommend – mono and poly unsaturated fats b. Avoid – saturated fats 33. What is the RDA for fat for older adults? a. <30% of total kcals 34. What percent of your total kcals should trans-fats be? a. <1% 35. What is the most common diagnosis for hospitalization? a. Dehydration 36. Why are older adults lacking adequate fluids? a. Decreased cue for thirst b. Fear of incontinence c. Forgetfulness d. Limited mobility e. Problems holding a cup or glass f. Difficulty swallowing 37. What is the recommended amount of free fluid? a. 30cc/kg/day 38. What is the recommended daily allowance of calcium? a. 1000-1200 mg/day 39. What is the TUL for calcium? a. 2000mg/day 40. Why are older adults at an increased risk for vit D deficiency? a. Less sun exposure b. Less efficient conversion of cholesterol to vit D c. Typically consume less vitamin D containing foods/fluids 41. What supplement should be considered for older adults? a. B12 42. Why is B6 beneficial for older adults? a. Reduces homocysteine levels (high = arterial damage and blood clots) 43. For what reason may older adults have decreased Fe? a. Antacids and low stomach acid secretion decrease absorption 44. When is a general multivitamin recommended for older adults? a. If intake it less than 1200kcal/day 45. What juice is commonly known for interacting with drugs? a. Grapefruit [Show More]
Last updated: 2 years ago
Preview 1 out of 26 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$15.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jan 10, 2023
Number of pages
26
Written in
All
Additional information
This document has been written for:
Uploaded
Jan 10, 2023
Downloads
0
Views
77