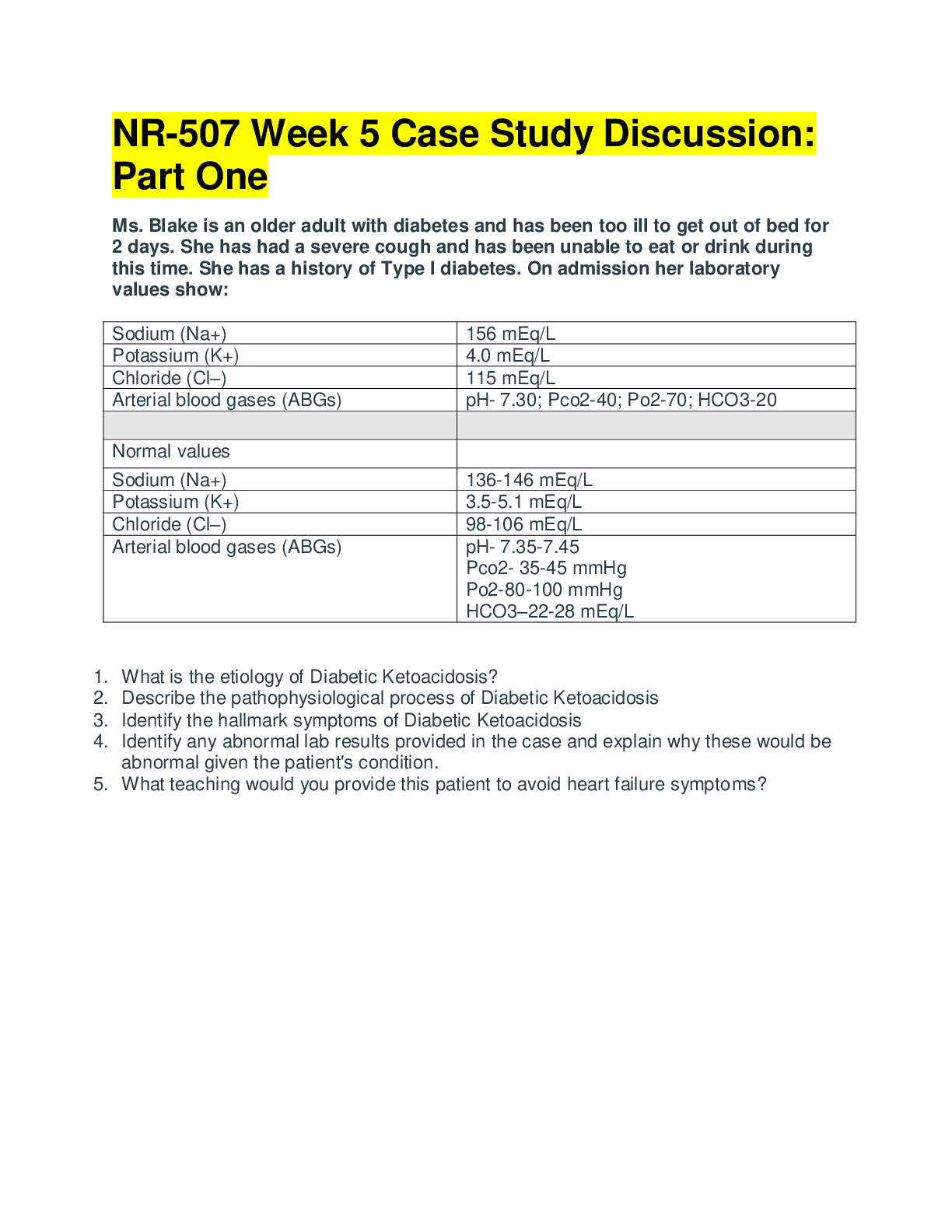
ATI EXAM 2
Norm pregnancy ranges
hct = preg 32-42%
Hgb = 10-14 g/dl
Platelets 150-350k increase 3-5days post
WBC 5-15,00
CHAPTER 20------ATI 23 NEWBORN ASSESSMENT
Expected ranges
Weight---5.5-8.8lb (250
...
ATI EXAM 2
Norm pregnancy ranges
hct = preg 32-42%
Hgb = 10-14 g/dl
Platelets 150-350k increase 3-5days post
WBC 5-15,00
CHAPTER 20------ATI 23 NEWBORN ASSESSMENT
Expected ranges
Weight---5.5-8.8lb (2500-4000g)
Length---45-55cm (18-22in)
Head circum---32-36.8cm(12.6-14.5in)
Chest circum---30-33cm (12-13in)
VITALS
Respiratory rate---do first
o 30-60bpm
o should not have grunting or nasal flaring==resp distress
Heart rate
o 110-160bpm
Blood pressure
o 60-80 systolic and 40-50 diastolic
Temperature
o 36.5-37.5 C (97.7-99.5F)
LAB RANGES
hgb- 14-24
hct—44%-64%
platelets 150-300,000
glucose 40-60
Physiologic response of newborn to birth
Resp function established when umbilical cord is cut
Circulatory change occur with expulsion of fetus and cutting umbilicus
o 3 shunts close-ductus arteriosus, ductus venous, and foramen ovaleo murmur over right and left auricles –latency in foramen ovale
Physical assessment
Apgar scoring---rules out abnormalities
o Completed at 1 min and 5 min
o 0-3 severe distress
o 4-6 mod diff
o 7-10 minimal/no diff adjusting to life
don’t use rectal therm. Can injure rectal mucosa
initial assessment
external –skin color, peeling, birthmarks, foot creases, breast tissue, nasal patency,
meconium staining
chest----point of maximal impulse location, ease of breathing, auscultation for hr/tones,
resp for crackles, wheezes, equality of breath sounds
abdomen---rounded, umbilicus has one vein two arteries AVA
Neuro----muscle tone and reflex reaction(MORO), palpation for presense/size of
fontanels and suture, assess for fullness or bulges
Gestational age
Performed within first 48 hrs
Uses measurements and new ballard scale
Ballard scale---assesses neuromuscular and physical maturity
o Neuro maturity—
Posture
Square window wrist formation
Popliteal angle
Scarf sign---arm over chest
Heel to ear
o Physical maturity
Skin texture
Lanugo
Plantar surface creases
Breast tissue buds
Eyes opening /ear cartilage
Genitalia development
AGA---appropriate for gestational age weight in 10th-90th percentile
SGA---- <10th percentile
LGA-- >90th percentile
LBW---low birth weight <2500 g
IUGR---growth rate does not meet norms
Postmature---after 42 weeks gestation with evidence of placental insufficiencySigns of cold stress—check temp
Moderately cyanotic
Mottled trunk
Active movement in extremities
Physical exam
Posture
o Curled up position, moderate flexion, resistant to extension of extremities
Skin
o Pink or acrocyanotic, no jaundice
o Jaundice may appear on 3rd day and disappear on own
o Texture—soft, dry, smooth, crack in hands and feet may be present.
Desquamation(peeling) may occur few days after with full terms
o Vernix caseosa—protective thick cheasy covering
o Lanugo-fine downy hair amount varies…on pinnae of ears, forehead and
shoulders
o Normal deviations
Milia---small white baby pimples, disappear on own
Mongolian spots—bluish purple spots common on shoulders, back, and
butt present on dark skin babies
Telangiectatic nevi—(stork bites)—flat pink/red marks that blanch easily
on neck, nose, upper eyelids, middle forehead…fade in 2nd year
Nevus flammeus (port wine stain)—capillary angioma purple or red does
not blanch or disappear
Erythema toxicum---pink newborn rash during first 3 weeks anywhere on
body no treatment needed
Head
o 2-3cm > chest circum
o hydrocephalus==head more than 4cm that chest
o microcephaly ==<32cm abnormally small head
o anterior fontanel==5cm and diamond shaped
o posterior fontanel==smaller and triangle
o fontanels should be soft and flat…can bulge with crying
bulging=increased cranial pressure, infection, or hemorrhage
depressed=can mean dehydration
sutures ---palpable, separated and overlapping(molding)
o caput succedaneum- local swelling of soft scalp tissue caused by labor pressure
expected, can be palpated as soft edematous mass, crosses suture line
resolves 3-4 days no treatment
o cephalohematoma—collection of blood on skull bone from birth trauma or
forceps. Does not cross suture line. Egg shaped, bluish discoloration resolves 2-6 wks
eyes
o lacrimal glands are immature minimal or no tears
o subconjunctival hemorrhages can result from pressure during birth
o eyeballs can have random jerky movements
Ears
o Low set ears can mean down syndrome or kidney disorder
o Cartilage should be firm and well formed
o Inspect ears for skin tags
Nose
o Midline, flat and brood with lack of bridge
o No drainage
o Nose breathers don’t open mouth to breath til after 3wks
o Apnea <15seconds is normal due to adjusting to life
o Nasal blockage can = flaring of nares, cyanosis , or asphyxia
Mouth
o Assess strength of sucking
o Lip movements should be symmetrical
o Saliva should be scant…excessive=tracheoesophageal fistula
o Epsteins pearls-small white cysts on gums and hard palates, normal
o Protruding tongue=down syndrome
o Gum and tongue should be pink
Neck
o Short, thick with skin folds, no webbing
o Absence of head control can equal=prematurity or down syndrome
Chest
o Barrel shaped
o Respirations primarily diaphragmatic
o Clavicles intact, absence of retractions
Abdomen
o Umbilical – odorless no intestinal structures exhibited
o Round and dome shaped
o Bowel sounds present 15-20 min after birth
Anogenital
o Anus present, patens, uncovered
o Meconium passes 24-48 hrs after birth
o Female genitalia-labia majora covering labia minora and clitoris, usually
edematous
o Vgainal blood tinged can occur in females from mothers hormones—normal
o Hymenal tag should be present
o Urine passed within 24 hrs…rust color from uric acid in first couple days
Extremities
o Assess for full range on motion with extremities flexedo Bowed legs and flat feet present due medial muscles more developed than
lateral
o No click in abducting hips
o Gluteal folds symmetrical
o No extra digits
Spine
o Straight flat midline easily flexed
REFLEXES
o Sucking/ rooting
Stroking cheek, turns head to suck
Disappears 3-4months can persist to 1 yr
o Palmar grasp
Newborn grabs examiners fingers when touching palm
Lessens 3-4 months
o Plantar grasp
Curling toes down
Birth-8months
o Moro relex
Allow head and trunk to fall back in semisitting position, extends and
abducts arms fingers form a C
Birth-6mnths
o Babinski
Stroke outer edge of foor—toes fan out
Birth-1yr
o Stepping
Hold newborn upright, does stepping movements
Birth-4wks
Senses
o Can focus on objects 8-12 inches away
o Prefer dim lighting
o Mouth most sensitive to touch
o Taste-prefer sweet
o Smell-prefer sweet smells recognize mothers smell
Diagnostics
Assess cord blood at birth for blood type, rh status
Complications
If hypothermic, use skin to skin or radiant warmer
Check temp every hour until stableCHAPTER 21 CARE OF NEWBORN---ATI 24&26
Physical newborn assessments
After birth done every 30min x 2, every 1hr x 2 …then every 8hr
Weight check daily
In first 6-8 hrs of life check for periods of reactivity
o 1st period
alert, exploring activity, sucking sounds
rapid hr ---160-180 lasts for 30 min after birth
can have rapid rr
o period of relative inactivity
60-100 min after birth
quiet begins to rest/sleep
HR and RR decreases
o 2nd period of reactivity
reawakens and responsive
can gag/choke on mucous
2-8hr after birth
Labs
genetic mandated screening--must have been fed for at least 24hrs
PKU testing
Serum bilirubin-before discharge
Respiratory complications
Bradypnea--<30/min
Tachypnea--- >60/min
Abnormal—expiratory grunting, crackles, wheezes
Respiratory distress---nasal flaring, retractions, grunting, gasping, labored breathing
Suction mouth then nasal passage for excess mucous
C-sections more susceptible to fluid remaining in lungs
Is bulb doesn’t work---back blows or chest thrusts can be used
BULB USE
o Compress before insertion to side of mouth
o Avoid center
o Mouth first then nostril
Identification
Newborn should have wrist and ankle band matching mothers record #
Staff must have photo id badge
Must verify with mother each time given
Thermoregulation Monitor temp for hypothermia
o <97.7
o cyanosis
o increased RR
Keeps warm by metabolizing brown fat
Cold stress can increase oxygen demands and use up brown reserves (BAD)
Heat loss occurs by 4 mechanisms
o Conduction- loss heat by contact with cooler surface
Preheat warmer, stethoscope, and scales
o Convection—heat loss from body to cooler air
Do procedures under warmers
Cover head, swaddle in blanket
o Evaporation--- heat loss by surface liquids evaporating
Rub newborn dry in warm sterile blanket immediately after delivery
o Radiation--- loss of heat from body to cooler solid surface that is nearby but not
in contact
Keep newborn away from examining tables and windows
Bathing
Can begin with stabilized temp (97.7F) 36.5C
Sponge bath under warmer 1-2hrs after birth
Wear gloves
Feeding
Breast-Start immediately after birth
Formula-2-4hr after birth , on demand normally 3-4hrs
Breast-6-8wet diapiers or 8-12x/day as demanded
Sleep
Sleep 16-19hr/day
Supine to decrease SIDS
No shared beds
Need for immunizations as a measure to prevent SIDS
Elimination
Monitor/document output
Should void once within 24hrs
6-8x/day after day 4
stool 3-4x/day after meconium pass
breastfed stools=yellow and seedy 3/day--lighter and loser than formula babies
avoid alcohol diaper wipes
cleanse area with water or mild soap after diaper change
apple antibiotic ointment, jelly or zinc oxide per hosp protocol
Infection control
provide individual thermometer, diapers, bathing supplies
don’t mix with other newbornsFamily education
encourage holding newborn
Umbilical cord care
cord clamp stays for 24-48hrs
cleaning with water during initial bath
assess for erythema, edema and drainage at each diaper change
fold diaper down and away
cords fall off in 10-14 days
Complications
Cold stress
hypoxia, acidosis, hypoglycemia
newborns with resp distress=higher risk hypothermia
o monitor for cold stress
o warm slowly over 2-4hr
o correct hypoxia with oxygen
Hypoglycemia
frequent in first few hrs of lide
risks
o mother has DM
o SGA or LGA
o <37wks or >42wks
o monitor these risky babies within first 2hrs
SIGNS
o jitteriness, twitching, weak slow high-pitched cry, irregular resp effort, cyanosis,
lethargy, eye rolling, seizing, blood glucose <40mg/dl heel stick
o breastfeed immediately or give donor milk or formula
o brain damage can result if depeleted of glucose
Hemorrhage
improper cord care or placement of clamp
o ensure clamp is tight, check for blood seepage
o notify provider is bleeding continue
Medications
Erythromycin
EYE care prophylactic
Prevents eye infection through birth canal---opthalmia neonatorum
Side effects-redness, swelling, drainage, blurred vision 24-48hrs
Vitamin K (phytonadione)
Prevents hemorrhagic disorders
Not produce in GI until day 7
Admin 0.5-1mg IM within 1hr after birth
HEP B immunization Informed consent needed
For healthy womens babies---at birth, 1 month, and 6months old
For hep b babies – 12hrs with hep b immunoglobulin, hep B 1mnth, 2mnth, 12mnth
DON’T give with vit K on same thigh
CHAPTER 26 ATI—nursing newborn care
Discharge
48hr after vaginal
72hr after c section
Education
Crying occurs when
o Overfeeding, hungry, overstimulated, wet, cold, tired, hot, bored, or need
burping
Quieting techniques
o Swaddling, close skin contact, pacifier, rhythmic noises,
movement(car,swing,rocking), on stomach while bouncing legs, stimulation, eye
contact
Sleep-wake cycle
o Sleep without feeding through night by 4-5mnths
o Get day/night routine-bathe before bed to soothe, last feeding at 2300
o Use dim lights at night for changing to not fully wake them
Basic holding
o Cradle
o Upright
o Football
o Colic hold—face down on arm face by elbow, quiets fussy baby
Bathing
o 2-3x/week using mild soap-no hexachlorophene
o no immersion until umbilical and circumsicion healed
o groin area washed last
o for males do not push back foreskin on penis to wash
o apply lotion fragrance free immediately after bathing
Health benefits of circumcision
o Easier hygiene
o Decreased risk of UTI
o Decreased risk STIs and HIV
o Decreased risk of penile cancer and cervical cancer for partner
o Contraindications
Bleeding disorders
Parents declined vit k—can be more likely to bleed
Newborns with hypospadias(abnormal urethra positioning) or
epispadias(urethral canal terminates on dorsum of penis)
Post care- Assess for bleeding every 15-30 min during 1st hr and hourly for
next 4-6hr
Fan fold diaper to prevent pressure on area
DO NOT wash off yellow mucous film that may develop at day 2
Complications
Hemorrhage-provide gentle pressure if bleeding persists notify
provider
Cold stress/hypoglycemia
Lack of voiding
Wellness checkups-
examined within 72hrs 2-3days after discharge by a pediatrician
1mnth
2mtnhs
4mths
6mths
9mnth
12mnths
15mnths
18mnths
2yrs, 2.5yrs, 3yrs, 4yrs and every year after
Manifestations of illness to educate parents
temp >100.4 (38C) or < 97.9F (36.6C)
poor feeding
frequent vomiting
decreased urine, or bowels, or diarrhea
labored breathing
jaudince
cyanosis
diff waking
CHAPTER 10 PREGNANCY COMPLICATIONS---ATI 7&9
Chapter 7----bleeding
spontaneous abortion
o terminated before 20wks or wt <500g.
o types-threatened, inevitable, incomplete, complete, and missed
o risks
chromosomal abnormatilies(50%) maternal illness---type 1 DM
advanced maternal age
premature cervical dilation
chronic maternal infection or malnutrition
trauma/injury
anomalies in fetus or placenta
substance use
antiphospholipid syndrome
o Expected findings
Backache/abdominal tenderness
Ruptured membranes
Fever
Signs/symptoms of hermorrhage –hypotension/tachycardia
o Labs
Hgb/hct-if lots of blood loss
Clotting factors
Wbc-inection
Hcg-confirm pregnancy
o Therapeutic procedures
D&C-dilation and curettage—dilate and scrape to remove contencts for
incomplete abortions
D&E-dilation and evacuation—evacuate uterine contents after 16wks
gestation
Prostaglandins and oxytocin—induce contractions to expel products
Causes of bleeding during pregnancy
1st trimester
o spontaneous abortion
o ectopic pregnancy-abrupt unilateral lower quadrant pain with or without vaginal
bleeding
2nd trimester
o gestational trophoblastic disease- uterine size increasing abnormally fast,
abnormal high levels hcg, nausea/increased emesis, dark brown red vaginal
bleeding. No fetus present
3rd trimester
o placenta previa-painless vaginal bleeding
o abruptio placentae-vaginal bleeding, sharp abdominal pain, tender rigid uterus
o Vasa previa- fetal vessels implanted into membranes rather than placenta
Other causes
Recurrent premature dilation of the cervix-painless bleeding with cervical dilation to
fetal expulsion
Preterm labor-pink stained vaginal discharge
Hydatidiform mole-benign proliferation growth of the placental trophoblastNursing care for bleeding
Perform pregnancy test
Observe color, amount of bleeding (pad count)
Avoid vaginal exams
Admit meds/blood products as prescribed
Use lay term miscarriage nor abortion
Provide emotional support and referrals
Medications
Analgesics
Prostaglandin-vaginal suppository
Oxytocin
Antibiotics
RhoD if rh negative
Client education
Notify provider of heavy bright red bleeding, temp, or foul discharge
Refrain from tub baths, sex, or placing things inside vagina for 2wks
Avoid pregnancy for 2mnths
Ectopic pregnancy
Abnormal implantation outside uterine cavity usually in fallopian tubes
2nd most frequent cause of bleeding in early pregnancy
leading cause of infertility---tube rupture
Risks
o STIs
o Tubal surgery
o IUD
o Assisted reproductive technologies
Findings
o Unilateral stabbing pain/tenderness in lower ab quadrant
o Delayed light irregular menses
o Scant, dark red or brown spotting 6-8wks after last menses
o Referred shoulder pain due to blood in peritoneal cavity
o Faintness/dizziness---bleeding in ab cavity
o Signs of hemorrhage—pallor, hypotension, tachycardia
Tests
o Progesterone levels----if elevated rules out
o hCG levels ----if elevated rules out ectopic pregnancy
therapeutic procedures
o transvaginal ultrasound—shows empty uterus
o methotrexate-inhibits cell division—dissolves pregnancy(avoid alcohol and folic
acid—to prevent toxicity) photosensitive
o salpingostomy-salvages tube if not rupturedo laparoscopic salphingectomy- removal of tube if ruptured
Care
o Replace fluids
o Education
o Prepare for surgery
o Obtain hCG/progesterone levels, liver/renal function, CBC and rH type
Gestational trophoblastic disease-
Uterine size increasing abnormally fast, abnormal high levels hcg, nausea/increased
emesis, dark brown red vaginal bleeding
Embryo fails to develop
Molar growths develop two types
o Complete mole
Paternally derived genetic material
No fetus, placenta, or fluid
Hemorrhage in uterine cavity occurs
o Partial mole
Genetic material from paternal and maternal
Abnormal fetal parts, amniotic sac, fetal blood with congenital anomalies
Risks
o Prior molar pregnancy
o Early teens or >40 years old
Findings
o Excessive vomiting due to elevated hCG levels
o Rapid uterine growth due to trophoblastic cells
o Dark bleeding or bright red can be scant or profuse
o Anemia from blood loss
o Clinical findings of preeclampsia
o Higher than expected fundal height
Labs
o Serum level of hCG high with decline after 10-12 wks
Therapeutic procedures
o Ultrasound reveals dense growth but no fetus
o Suction curettage to evacuate mole
o RhoD if needed
o Serum hCG done weekly for 3wks then monthly for 6months-1yr to detect GTD
Nursing care
o Measure fundal height
o Assess GI status and appetite
o Admin meds and chemo meds for malignant cells containing choriocarcinoma
o Advise clients to save clots for evaluationPlacenta previa
Placenta abnormally implants in lowe segment of uterus or over cervical os instead of at
fundus
Results in bleeding at 3rd trimester
Complete or total-cervical os completely covered by attachment
Incomplete/parital –cervical os partially covered
Marginal or low-lying—attached to lower uterine segment but does not reach os
Risks
o Previous placenta previa
o Uterine scarring
o Age >35
o Multifetal pregnancy
o Smoking
Findings
o Painless, bright red bleeding 2nd-3rd trimester
o Uterus soft, relaxed, nontender with normal tone
o Fundal height greater than expected for gest. Age
o Fetus in breech, oblique, or transverse position
o Reassuring FHR
o Decreased urinary output
Labs
o Hgb & hct for blood loss assessment
o CBC/coagulation profile
o Kleihauer-betke test—detects fetal blood in maternal circulation
o Transabdominal or transvaginal ultrasound for placement of placenta
Care
o Assess bleeding & fundal height
o Perform leopold maneuvers
o Refrain from vaginal exam
o Have oxygen available
o Bed rest
o Nothing inserted vaginally
Abruptio placentae
Premature separation of the placenta from the uterus
After 20wks gest (3rd trim)
Leasing cause maternal death
Coagulation defect (DIC) is often associated with abruption
Risks
o Maternal HTN
o Blunt traumao Cocaine use
o Smoking
o Previous abruption
o Premature rupture of membranes
o Multifetal pregnancy
Findings
o Sudden uterine pain with dark red bleeding
o Uterine tenderness
o Contractions with hypertonicity
o Fetal distress
o Clinical findings of hypovolemic shock
Labs
o Hgb and hct decreased
o Clotting defects
o Kleihauer betke test
o Biophysical profile for fetal well being
o Ultrasound for placental placement
Careo Palpate uterus for tenderness and tone
o Assess fhr
o Immediate birth is the management
Need 8-10L o2
Vasa previa
Fetal umbilical vessels implant into fetal membranes rather than placenta
Velamentous insertion of the cord—vessels begin in the branch at the membranes then
course to the placenta
Succenturaite insertion of the cord—placenta divided into 2 or more lobes and not one
mass
Battledore insertion of the cord—marginal insertion, increased risk fetal hemorrhage
Use ultrasound for well being and vessel assessment
CHAPTER 9 ATI—MEDICAL CONDITIONS
Cervical insufficiency(premature cervical dilation)
Expulsion of products of conception
Risks
o Hx of cervical trauma
o In utero exposure to diethylstilbestrol
o Congenital structural defects of uterus or cervix
Findingso Increase in pelvic pressure/urge to push
o Pink stained vaginal discharge/bleeding
o Rupture membranes
o Uterine contractions with expulsion of fetus
Diagnostic procedures
o Ultrasound showing short cervix, presence of funneling, effacement
o Prophylactic cervical cerclage-reinforcement of cervix with heavy ligature to
strengthen and prevent dilation..best if done at 12-14wks
Care
o Assess discharge
o Monitor reports of pressure and contractions
Meds
o Tocolytics inhibit contractions
Discharge instructions
o Bed rest/activity restriction
o Encourage hydration
o Avoid intercourse, tampons, douching
Hyperemesis gravidarum
Excessive nausea/vomiting prolonged past 12wks, 5%wt loss, acetonurio, electrolyte
imbalance, ketosis
At risk for preterm birth or intrauterine growth restriction
Risks
o Age <30
o History migraines
o Obesity
o 1st pregnancy
o multifetal gestation
o gestation trophoblastic disease
o fetus with chromosomal anomaly
o high emotional stress
o hyperthyroid disorder
o GI disorder, diabetes
Findings
o Excessive vomiting for prolonged periods
o Dehydration
o Wt loss
o Increased pulse
o Decreased BP
o Urine ketones present
Tests
o Urinalysis---for ketones and acetones & elevated urine spec gravity
o Chem profile---electrolyte imbalance
o Thyroid testo CBC—hct
Care
o Monitor I&O
o Monitor wt, vitals, assess skin turgor
o NPO 24-48 hrs
Meds
o IV lactated ringers—hydration
o Pyridoxine (VIT b---vitamins as tolerated
o Antiemetics---ondansetron, metoclopramide
o Corticosteroids- treat refractory hyperemesis
Gestational Diabetes
Ideal blood glucose during pregnancy 70-110 mg/dl
Impaired tolerance to glucose during pregnancy recognition
Risks to fetus
o Spontaneous abortion
o Infections
o Hydramnios
o Ketoacidosis
o Hypoglycemia
o Hyperglycemia---excessive fetal growth
Risk factors
o Obesity
o HTN
o Glycosuria
o Age >25
o Family Hx diabetes
o Previous delivery of infant large or stillborn
Findings
o HYPO--Nervousness, headache, weakness, irritability, hunger, blurred vision ,
tingling of mouth./extremities---shaking, clammy skin, shallow respirations, rapid
pulse
o HYPER—polydipsia, polyphagia, polyuria, nausea, ab pain, dry flushed skin, fruity
breath----vomiting & excessive wt gain.
Tests
o Routine urinalysis—check for glucose, ketones
o Glucola screening/1hr glucose tolerance test
@24-48wks gestation 50g oral glucose wait 1hr
don’t fast
positive=130-140 or >
o oral glucose tolerance test
overnight fasting
avoid caffeine, smoking for 12hr prior 100g glucose test at 1,2,and 3 hr following
diagnostics
o biophysical profile for fetal well being
o amniocentesis with alpha fetoprotein
o nonstress test for well being
Meds
o Manage with diet and exercise
o Begin insulin if no change
Education
o Daily kick counts
o Diet and exercise
Gestational HTN
Underlying cause-vasospasms contributing to poor tissue perfusion
Associated with placental abruption, kidney failure, hepatic rupture, preterm birth, and
fetal/maternal death
GH---Begans after wk 20….BP >140/90 no proteinuria, goes to baseline after 6 wks post
Mild preeclampsia---GH with proteinuria 1+ or more, headaches, and edema
Severe preeclampsia—BP>160/110, proteinuria 3+, oliguria, elevated serum creatinine
>1.1, hyperreflexia with clonus, visual disturbances, epigastric/upper quadrant pain,
thrombocytopenia
Eclampsia---severe preeclampsia with seizure/coma activity
o Warnings of convulsions by headache, severe epigastric pain, hyperreflexia, and
hemoconcentrations
HELLP syndrome---GH with hepatic dysfunction
o H=hemolysis—anemia/jaundice
o EL= elevated liver enzymes –ALT and AST, epi pain and N/V
o LP= low platelets <100,000---abnormal bleeding, bleeding gums, petechiae
Risks
<19 yo or >40
1st pregnancy
morbid obesity
multifetal gestation
chronic renal disease
chronic HTN
DM
Rheumatoid arthritis
Lupus
Findings
Severe continuous headache
Nausea
Blurred vision
Flashes of lights/dotsPhysical assessment findings
HYN, proteinuria, facial/hand/ab edema, pitting edema, vomiting, oliguria,
hyperreflexia, scotoma, epi pain, dyspnea, seizures, diminished breath sounds
Abnormal labs
Elevated LDH, AST liver enxymes
Increased creatinine
Increased plasma uric acid
Thrombocytopenia
Decreased hgb
Hyperbilirubinemia
Care
Assess LOC
Pulse ox
Monitor urine output and assess for proteinuria
Daily wt
Encourage lateral positioning
perform daily kick counts
Meds
antihypertensives—(methyldopa, nifedipine, hydralazine, labetalol)
avoid ace inhibitors and angiotension II
Magnesium sulfate for anticonvulsants
o Will initially feel flushed hot and sedated
o Toxicity—absence oof deep tendon reflexes
o Urine <30/hr
o Resp <12
o Decreased LOC
o Cardiac dysrhythmias
o Antidote==calcium gluconate or chloride
Chapter 17 postpartum
BP & PULSE q 15min for first 2hrs after birth
Temp q4hr for first 8hr after birth then q8hr
BUBBLE
RhoD globulin- admin within 72hrs to women neg and infant +
Kleiauer betke test—determines if fetal blood is in mother circulation
FUNDUS
Fundus descends 1cm per day
After 2wks the uterus should lie within the true pelvis and not be palpable Assess q8hr
Care
Admin tocolytics to promote uterine contractions
o Oxytocin& misoprostol (watch hypotension)methylergine, ergovine, and
carboprost(watch HYPERtension)
Early breastfeeding will stimulate oxytocin and prevent hemmorhage
3 stages of lochia
Rubra- bright red, fleshy odor 1-3 days, can contain small clots
Lochia serosa- pinkish brown and serosanguinous consistency 4-10 days
Lochia alba- yellowish creamy white color, fleshy odor last 11days-4-8wks
Amount
Scant- <2.5cm
Light 2.5-10cm
Heavy-one pad within 2hr
Excessive one pad in 15min or less
Care
Can apply ice to the perineum for the frst 24-48 hrs
Sitze bath 2x day
With hazel can help with swelling and hemorrhoids
CHAPTER 17 POSTPARTUM ADAPTATIONS AND NURSING CARE
Uterine involution-return to previous size
o Contraction of muscle fibers
Contraction controls bleeding and shrinks uterus
o Catabolism-
Convert cells into simpler compounds
o Regeneration of uterine epithelium
Outer portion expelled
Leaves the endometrial layer smooth and spongy
Uterine Descent
o Immediately after delivery
Size of a large grapefruit
Palpate between the symphysis pubis and the umbilicus-midline
o 24 Hrs
within 12 the fundus rises to level of umbilicus
o By day 10
Descends by 1cm/finger per day
No longer palpable by day 14. – into pelvic cavityReproductive system
Afterpains—intermittent uterine contractions
o Loss of muscle tone
In multipara this is more painful due to less muscle tone
o Over distention
Primipara may have more pain if uterus was overdistended
o Breast feeding
Causes more pain due to oxytocin release during breast feeding causing
strong uterine contractions
o Use analgesics
o Should become less severe by 3rd day
Cervix
o 1 week = firm and external os 1cm and slit-like
o external os remains permanently slit like and slightly open in nullparous
Vagina
o Mucosa atrophic(thinning) until estrogen production is reestablished
o Vaginal dryness and dyspareunia(sex pain) is likely if breastfeeding-estrogen not
producing
o 6-10 wks for vaginal epithelium to be restored
Perineum----REEDA
o Episiotomy-heals in about 2-3wks
o Lacerations –less discomfort 2-3wks healing
Cardiovascular system
o Increase in cardiac output due to =
Blood from uteroplacental unit returns to central circulation
Decreased pressure from uterus on vessels
Excess extracellular fluid foes into the vascular compartment
Returns to pre-pregnancy levels-6-12wks postpartum
o Excess plasma volume
Diuresis
Diaphoresis
o Coagulation
4-6wks return to pre preg state
may use compression stockings if not ambulating enough
o Blood values
WBC up to 30,000
Hgb/Hct-return to norm 4-6wks after
o GI
Begins to be hungry and thirsty after birth
Constipation is common
Offer stool softeners
Normal pattern resume 8-14days after
o Urinary
Kidneys return to norm 4wks post Increased capacity and decreased muscle tone-little sensation of voiding
Uterine distention can lead to increase bleeding as the uterus is not
contracting
o Musculoskeletal
Diastasis recti
Use gentle exercises to strengthen wall –may take 6wks to return
o Integumentary
Pigmentation reduces or disappears
o Hair
Loss starts at 4-20wks and is regrown by 6 months
o Neuro
Anesthesia/analgesics may cause temporary dizziness/lack of feeling
Prevention of injury is priority
Carefully assess headaches
Headache with blurr vision/photophobia/ab pain—preeclampsia
Severe headaches may be from postdural puncture—lay supine
o Immune-
Administer rubella after birth for nonimmune mothers
Wil need 2nd vaccine in 4-8wks
Avoid pregnancy for 1 month after vaccine
Safe if nursing
Flu-symptoms may occur
Rho(D) immune globe
Admin is mother is (-) and baby is (+)
Negative coombs test—rh factor. Mom has not developed antibodies
against babies (+) blood
Receive issued card
Postpartum Initial assessments
BUBBLET3E
BREASTS
o Size, contour, symmetry, nipple cracks/fissures/flat or inverted/mastitis
UTERUS
o Fundus should be firm midline below umbilicus
o If boggy-support lower segment and massage
o If displaced/high-have pt void
o Soft after massage-express clots, notify, begin oxytocin
BOWEL
o Bowel movement
o Flatulence
o Hemorrhoids
BLADDER
o Void w/in 6-8hrso Have decreased urge
o Assess for distention
o Risk for UTI
o Stress incontinence
o 150ml upon voiding-retention
o 300-400ml- usually empty
LOCHIA---TACO
o Rubra-day 1-3 scant
o Serosa= day 4-10
o Alba= day 10-up to 6wks
o Moderate---rubra with small clots 2nd day
EPISIOTOMY/LACERATION---REEDA
o Redness, ecchymosis, edema, discharge, approximation
THROMBUS
o Assess using homans sign
o Deep tendon relfexes
EMOTIONS
o Baby blues
o S/S= postpartum discomforts, sleep deprivation, anxiety, body image
concern
o Returning to weork
RHOGAM/RUBELLA (if indicated)
Maternal adaptation:phases of role attainment
Taking in phaseo Wants to talk about and labor
o Makes phone calls goes over all details
Taking hold phaseo Becomes more independent
o Assumes responsibility for own care
o Shifts attention to newborns behaviors
o “teachable, reachable, referable”
Letting go phase
o Parents give up previous roles and accept parenting
o At this point can be disappointed in fantasy’s
When to call health provider
Fever==over 100.4
Persistent perineal pain
Breast infection
S/S UTI
Abdominal tenderness
Abnormal change in lochia S/S thrombi
Pelvic fullness or pressure
S/S infection of incision
Postpartum discharge
Hospital length stay
o Vaginal---48hrs
o C-section---72hrs
Preventing discharge
o Mother
o Infant
Resumption of menstruation
Lactating—6months
Non lactating—27-75days after birth, menses resumes 4-6wks
CHAPTER 9 ANTEPARTUM FETAL ASSESSMENT
Biophysical profile includes
Fetal breathing movement
Fetal tone
Amniotic fluid volume
Amniocentesis
Evaluate fetal lung maturity using the (L/S) lecithin/sphingomyelin ratio
Empty bladder before procedure
Supine position, wedge under right hip to displace uterus off vena cava
Identifies fetal genetic defects
Lecithin/sphingomyselin ratio (L/S)---test done to determine fetal lung maturity
Nonstress test uses an acoustic vibration device to awake the fetus
Assesses FHR in relationship to fetal movement
Mom pushes button everytime she feels fetal movements
Contraction stress test indications Decreased fetal movement
Intrauterine growth restriction IUGR
Post-maturity
CHAPTER 18 POSTPARTUM COMPLICATIONS
Postpartum hemorrhage
Loss of >500mL – vaginal delivery
>1000mL c section
decrease in hct >10% since admission
Assess 4 T’S
Tone
Trauma
Tissue
thrombin
risks---
o infection
o prolonged labor
o meds
o uterine inversion
o precipitate labor or delivery or operative delivery
o multiparity
o clotting disorder
o uterine leiomyomas—fibroids
o placenta abnormalities
o C-section
Early hemmorhage
o Uterine atony
o Trauma
o Retained tissue
o Abnormal coagulation
Late
o Subinvolution
o Retained tissue
o Infection
Signss
o Fundus soft or boggy
o Hard to locate fundus
o Firm with massage but then loses toneo High fundus
o Excessive lochia---1pad 15min
o Excessive clots
Meds----uterotonics
o Methylergonovine (HTN)and carboprost(don’t use in asthma,MAD DIARRHEA)
most common
o Oxytocin
o Misoprost—Can be rectal
o Stimulate uterine contractions
Retained placental fragments
preventable through inspection of placenta after delivery
Risks
o Attempts to deliver placenta prior to separation
o Manual removal
o Abnormal implantation
o previous c section
o Uterine leiomyomas
Thromboembolic disorders
o Most common during pregnancy/post
Superficial venous thrombophlebitis
Deep vein thrombosis
Pulmonary embolism
o Primary cause
Venous stasis
Hypercoagulable blood
Injury to vessel
Late postpartum hemorrhage
Failure of uterus to involve
Signs
o Prolonged discharge of lochia
o Excessive uterine bleeding
o Possibly profuse hemorrhage
o Pelvic pain/heaviness
o Backache
o Fatigue
o Uterus larger and softer than norm
Hypovolemic shock
Puerperal infection—infection after childbirth
Endometritis-uterine infection
Wound infection UTI—1-2 days post
o Risks-epidural, catheter, frequent pelvic exams, hx utis, c section
Mastitis—2-4wks post
o Completely empty ech breast at feeding, prevents milk stasis/bacteria growth
Septic pelvic thrombophlebitis---2-4days post
CHAPTER 27 – WOMENS HEALTH//STI’s
Bacterial STIs
o Chlamydia trachomatis
Most common/fastest spreading
Often silent/diff to diagnose
Asymptotic is pregnant women
Often coexist with gonorrhea
Can lead to PID(tubal scarring), infertility or ectopic pregnancy if
untreated **
Yearly screening sexually active women >25
Screen in 1st prenatal and 3rd trimester –if <25 or high risk
Risks---multiple partner & unprotected sex
Findings---
Male= urethral discharge(mucoid,watery), dysuria
Female=dysuria, urinary frequency, spotting/postcoital bleeding
o Mucopurulent endocervical discharge
o Easily induced endocervical bleeding
Lab tests----
Urine culture-male
Endocervical-female
Care----
Take entire prescription
Identify/treat all partners
Pregnant clients retest 3 wks after treatment
Report cases of disease
Meds----
Azithromycin or amoxicillin
o Gonorrhea
Perinatal complications
PROM, preterm birth, chorioamnionitis, neonatal sepsis, IUGR,
maternal post partum sepsis
Can be spread genital-genital-anal-oral-newborn delivery
Typically asymptotic Can lead to PID and infertility
Yearly screening>25, 1st prenatal and 3rd trimester
Risks----multiple partners, unprotected sex
Findings----
Male=dysuria, urethral discharge
Female=dysuria, vaginal bleeding btwn periods, dysmenorrhea,
yellow/green discharge, easily induced endocervical bleeding
Labs----
Urine culture=male
Endocervical=female
Care----
Education
Identify/treat all partners
Erythromycin following delivery for infant
Report disease
Avoid intercourse treat partners simultaneously
Meds-----Ceftriaxone and azithromycin PO
Pelvic inflammatory disease (PID)
o Increased risk for ectopic pregnancies, infertility and chronic pelvic pain
o Risks---
IUD
Douche products
Untreated STIs
o Symptoms---asymptotic or subtle
Pelvic pain, pain, fever, purulent discharge, nausea, anorexia,
irregular vaginal bleeding
Abdominal or adnexal tenderness
o Screening & labs---
Sexual history
Leukocytosis, increased ESR
o Management
Serious may need to go to hospital
Will need IV antibiotics for next 48hrs
Ceftriaxone plus azithromycin or doxycycline
Cefixime plus azithromycin or doxy
Pelvic abscess may require surgical intervention
Educate on how to prevent STDs
Avoid IV drug use//HIV risks
HIV- Human immunodeficiency virus
o Destructs T lymphocyteso Test in 3rd trimester—rapid if in labor and status unknown
o Avoid amniocentesis and episiotomy if (+)
o Don’t administer injections until after first bath
o Risks----
IV drug us
Multiple partners
Hx of STIs
Blood transfusion(rare)
Gay men
o Findings----
Fatigue-flu like findings
Fever
headache
Diarrhea/weight loss
Lymphadenopathy and rash
Anemia
myalgia
o Tests---
Need maternal consent
Antibody screening-enzyme immunoassay
Rapid HIV antibody test—blood or urine
Screen for STIs
Obtain viral load levels and CD4 cell counts throughout pregnancy
o CARE---
Counseling
Use standard precautions
Encourage immunizations
Encourage condoms
Plan for c section at 38ws is viral load >1,000copies/mL
DO NOT breast feed
o Meds----antiretroviral
Nucleoside reverse transcriptase inhibitor
admin at 14wks gestation, throughout pregnancy, and before labor/c
section
admin retrovir to infant at delivery and for 6wks following
o Contraindications for HIV patients---episiotomy, internal fetal monitoring,
forceps----all can cause bleeding
Trichomoniasis
o STI
o Common cause of vaginal infection
o Can lead to PID and infertility
o More likely to have preterm babies and LBW
o Risks--- Multiple partners
Unprotected sex
o Findings—
Penile itching or irritation, dysuria—urethral discharge—male
Yellow-green frothy vaginal disorder with foul odor----women
Dyspareunia (painful sex) and itching-----women
Dysuria
Strawberry spots on cervic, cervix bleeds easily
o Labs//screening---
Whiff test---discharged placed on pH paper
Speculum exam
Pap smear
o Diangnosis---
Whiff + if Ph>4.5
Wet mount saline prep
o Care----avoid alcohol with meds
o Meds---metrodinazole tinidazole—single dose
INFECTIONS----Group B streptococcus
Screening at 35-37 weeks
Associated with poor pregnant outcomes
Effects of STIs
Premature rupture of labor
Premature labor
Dystocia
Miscarriage
Fetal effects- preterm birth
Pneumonia
Systemic infection
Congenital infection
TORCH infection---toxoplasmosis
Contracted by consuming undercooked meats, or handling cat feces
Joint pain, rash, malaise, tender lymph nodes
CHAPTER 22 INFANT FEEDINGNewborns nutrition needs
Breastfed---85-100kcal/kg/daily
Formula---100-110kcal/kg/day
May lose 10% of birth weight
Breast milk composition
Colostrum=="liquid gold”
Transitional milk==like 2% yellowish white
Mature milk
Benefits to breast feeding---infant
Less allergies develop
Immunologic properties
decreased infections
lower incidence of obesity/diabetes/SIDS
meets specific needs of baby
easily digested
unlikely to be contaminated
less likely to over-feed
constipation less likely
Mother benefits
oxytocin releases enhances uterine involution
less blood loss
resumption of ovulation delayed
decrease cancer risk
mom can rest during feeds
burns calories
skin ti skin
convenient(traveling)
cheaper
Formula
cows milk to compare with breast
o reduced protein
o remove sat fats
formula for special needs infants
o soy/protein hydrolysate
Factors influencing choice of feeding
o Support from others
o Cultural influenceso Employment
o Staff knowledge
Normal breastfeeding
Prolactin-activate milk production. Suckling increased prolactin levels
Oxytocin-increases in response to nipple stimulation and causes milk ejection
Nursing care for breastfeeding
Teaching positions
Latching on
Suckling pattern
Removal from breast
Frequency and length
Common concerns
Sleepy
Nipple confusion
Suckling problems- poorly positioned nipple
Infant complications
o Jaundice
o Prematurity –mother should self express milk
o Illness and congenital defectsEngorgement
Breast
o Heat
o Pump/breastfeed
o Pain meds
o Supportive bra
o Cold compress between feedings can help with engorgement
Bottle-feeding
o Cold
o Avoid stimulation
o Pain meds
o Supportive tight fitting bra for first 73hrs
Interventions to assist with breastfeeding
Pumps
Breast milk storage
Shells---for inverted/weird nipples
Shieds
Seek assistance from lactation consultant
CHAPTER 18 POSTPARTUM COMPLICATIONSPostpartum hemorrhage
Loss of >500mL – vaginal delivery
>1000mL c section
decrease in hct >10% since admission
Assess 4 T’S
Tone
Trauma
Tissue
thrombin
risks---
o infection
o prolonged labor
o meds
o uterine inversion
o precipitate labor or delivery or operative delivery
o multiparity
o clothing disorder
o uterine leiomyomas—fibroids
o placenta abnormalities
o C-section
Early hemmorhage
o Uterine atony
o Trauma
o Retained tissue
o Abnormal coagulation
Late
o Subinvolution
o Retained tissue
o Infection
Signss
o Fundus soft or boggy
o Hard to locate fundus
o Firm with massage but then loses tone
o High fundus
o Excessive lochia---1pad 15min
o Excessive clots
Meds----uterotonics
o Methylergonovine (HTN)and carboprost(don’t use in asthma,MAD DIARRHEA)
most common
o Oxytocino Misoprost—Can be rectal
o Stimulate uterine contractions
Retained placental fragments
Reventable through inspection of placenta after delivery
Risks
o Attempts to deliver placenta prior to separation
o Manual removal
o Abnormal implantation
o previous c section
o Uterine leiomyomas
Thromboembolic disorders
o Most common during pregnancy/post
Superficial venous thrombophlebitis
Deep vein thrombosis
Pulmonary embolism
o Primary cause
Venous stasis
Hypercoaguable blood
Injusry to vessel
Late postpartum hemorrhage
Failure of uterus to involve
Signs
o Prolonged discharge of lochia
o Excessive uterine bleeding
o Possibly profuse hemorrhage
o Pelvic pain/heaviness
o Backache
o Fatigue
o Uterus larger and softer than norm
Hypovolemic shock
Peurperal infection—infection after childbirth
Endometritis-uterine infection
Wound infection
UTI—1-2 days post
Mastitis—2-4wks post
Septic pelvic thrombophlebitis---2-4days post
[Show More]


.png)