Pharmacology > STUDY GUIDE > NURSING 238 Pharm Exam 3 study guide . Chapter 26: ATI PG. 151 Ch 20 on ATI (All)
NURSING 238 Pharm Exam 3 study guide . Chapter 26: ATI PG. 151 Ch 20 on ATI
Document Content and Description Below
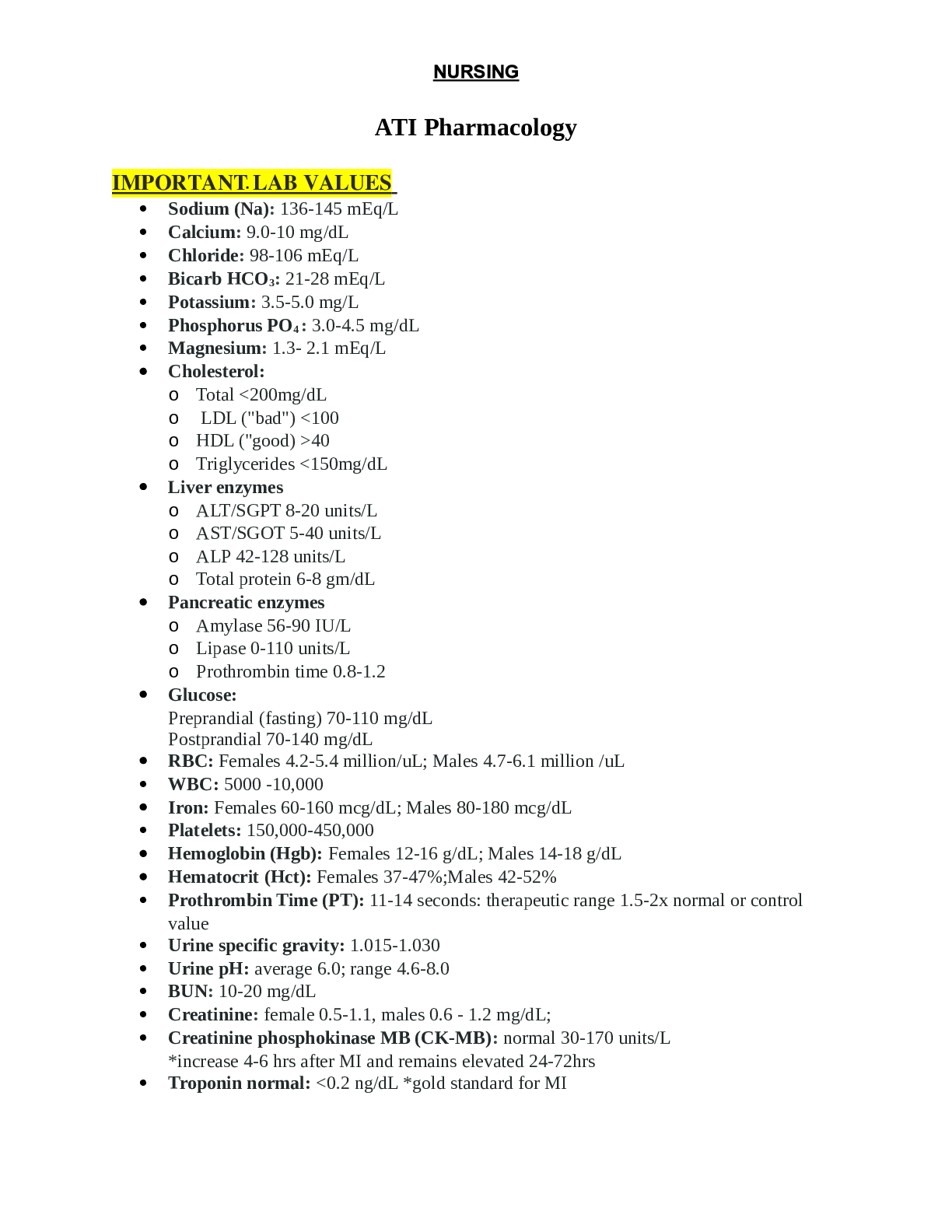
Pharmacology Study Guide Exam 3 NURSING 238 Exam 3 study guide Pharm. Chapter 26: ATI PG. 151 Ch 20 on ATI Drugs that control Hypertension Mechanism of action of different classifications o... Indication of usage o Adverse effects o Education/Teaching/nursing interventions Angiotensin‑ converting enzyme inhibitors SELECT PROTOTYPE MEDICATION: Captopril Mechanism of action: Angiotensinconverting enzyme (ACE) inhibitors reduce production of angiotensin II by blocking the conversion of angiotensin I to angiotensin II and increasing levels of bradykinin, Leading to the following: Vasodilation (mostly arteriole) Excretion of sodium and water, and retention of potassium by actions in the kidneys Reduction in pathological changes in the blood vessels and heart that result from the presence of angiotensin II and aldosterone. Indication of usage: Hypertension Heart failure Myocardial infarction (to decrease mortality and to decrease risk of heart failure and left ventricular dysfunction) Diabetic and nondiabetic nephropathy For clients at high risk for a cardiovascular event, ramipril is used to prevent MI, stroke, or death. Adverse effects: First‑ dose orthostatic hypotension NURSING CONSIDERATIONS If the client is already taking a diuretic, stop the medication temporarily for 2 to 3 days prior to the startPharmacology Study Guide Exam 3 of an ACE inhibitor. Taking another type of antihypertensive medication increases the hypotensive effects of an ACE inhibitor. Start treatment with a low dosage of the medication. Monitor blood pressure for 2 hr after initiation of treatment. Instruct clients to change positions slowly and to lie down if feeling dizzy, lightheaded, or faint. Cough Related to inhibition of kinase II (alternative name for ACE), which results in increase in bradykinin CLIENT EDUCATION: Inform clients of the possibility of experiencing a dry cough and to notify the provider. Discontinue the medication. Hyperkalemia NURSING CONSIDERATIONS Monitor potassium levels to maintain a level within the expected reference range of 3.5 to 5 mEq/L. Advise clients to avoid the use of salt substitutes containing potassium. Monitor for manifestations of hyperkalemia, such as numbness and tingling and paresthesia in hands and feet. Rash and dysgeusia (altered taste) Primarily with captopril NURSING CONSIDERATIONS Clients should inform the provider if these effects occur. Adverse effects will stop with discontinuation of the medication. Angioedema Swelling of the tongue and oral pharynx NURSING CONSIDERATIONS Treat severe effects with subcutaneous injection of epinephrine. Discontinue medication. Neutropenia Rare but serious complication of captopril NURSING CONSIDERATIONS Monitor WBC counts every 2 weeks for 3 months, then periodically. This condition is reversible when detected early.Pharmacology Study Guide Exam 3 Inform clients to notify the provider at the first indications of infection (fever, sore throat). Discontinue medication. Education/Teaching/Nursing Intervention: Administer ACE inhibitors orally except enalaprilat, which is the only ACE inhibitor for IV use. Advise clients that the medication is prescribed as a single formulation or in combination with hydrochlorothiazide (a thiazide diuretic). Advise clients that blood pressure is monitored after the first dose for at least 2 hr to detect hypotension. Instruct clients to take captopril and moexipril at least 1 hr before meals. Other ACE inhibitors are taken with or without food. Advise clients to notify the provider if cough, rash, dysgeusia (altered taste), or indications of infection occur. Advise client to rise slowly from sitting. Advise client to avoid activities that require alertness until effects are known. Advise clients to report if pregnancy is suspected. Angiotensin II receptor blockers SELECT PROTOTYPE MEDICATION: Losartan Mechanism of action: EXPECTED PHARMACOLOGICAL ACTION: These medications block the action of angiotensin II in the body. This results in the following. Vasodilation (arterioles and veins) Excretion of sodium and water (by decreasing release of aldosterone) Indication of usage: THERAPEUTIC USES Hypertension Heart failure (valsartan and candesartan) Stroke prevention (losartan) Delay progression of diabetic nephropathy (irbesartan and losartan) Protect against MI, stroke, and death from cardiac causes in individuals unable to tolerate ACE inhibitors (telmisartan) Reduce mortality following an acute myocardial infarction (valsartan)Pharmacology Study Guide Exam 3 Slow the development of diabetic retinopathy (losartan) COMPLICATIONS The major difference between angiotensin II receptor blockers (ARBs) and ACE inhibitors is that cough and hyperkalemia are not adverse effects of ARBs. Adverse effects: Angioedema NURSING CONSIDERATIONS Advise clients to observe for manifestations (skin wheals, swelling of tongue and pharynx) and to notify provider immediately. Treat severe effects with subcutaneous injection of epinephrine. Discontinue medication. Fetal injury CLIENT EDUCATION Advise women of risk during the second and third trimester of pregnancy. Advise women of childbearing age to use contraception while on this medication. Hypotension NURSING CONSIDERATIONS: Monitor blood pressure. Advise clients to rise slowly from a sitting position. Dizziness, lightheadedness: CLIENT EDUCATION: Instruct clients to avoid activities that require alertness until effects are known. Education/Teaching/Nursing Intervention: Administer medications by oral route. Advise clients that medication is prescribed as a single formulation or in combination with hydrochlorothiazide. Take ARBs with or without food. Advise clients who have heart failure to monitor weight and edema. Aldosterone antagonists Mechanism of action: SELECT PROTOTYPE MEDICATION: Eplerenone OTHER MEDICATION: Spironolactone EXPECTED PHARMACOLOGICAL ACTION: Aldosterone antagonists reduce blood volume by blocking aldosterone receptors in the kidney, thus promoting excretion of sodium and water and retention of potassium. Indication of usage: THERAPEUTIC USES: Hypertension Heart failurePharmacology Study Guide Exam 3 Adverse effects: Hyperkalemia, hyponatremia NURSING CONSIDERATIONS Monitor serum potassium and sodium levels periodically. Advise client not to use potassium supplements or salt substitutes containing potassium. Advise client to monitor and report manifestations of hyperkalemia, such as paresthesia and tingling of hands and feet. Flu-like manifestations Fatigue, headache, diarrhea, abdominal pain, cough CLIENT EDUCATION: Advise client to report severe manifestations to provider. Gynecomastia Enlargement and tenderness of male breast tissue CLIENT EDUCATION: Advise the client to report severe manifestations to the provider. Dizziness, fatigue CLIENT EDUCATION: Avoid activities that require alertness until reaction is known. Education/Teaching/Nursing Intervention: Administer orally with or without food. Do not administer with potassium supplements. Direct renin inhibitors SELECT PROTOTYPE MEDICATION: Aliskiren Mechanism of action: Binds with renin to inhibit production of angiotensin I, thus decreasing production of both angiotensin II and aldosterone. Indication of usage: Relieves hypertension when used alone or with another antihypertensive medication. Adverse effects: Angioedema, rash, and cough Angioedema is swelling of the pharynx, tongue, glottis CLIENT EDUCATION: Teach client to monitor for rash and angioedema. Stop medication and notify provider, or call 911 for severe manifestations. Hyperkalemia NURSING CONSIDERATIONS Monitor serum potassium periodically during treatment. Advise client not to use potassium supplements or salt substitutes containing potassium. Advise client to monitor and report manifestations of hyperkalemia, such as paresthesia and tingling of hands and feet.Pharmacology Study Guide Exam 3 Diarrhea Dose‑ related Seen most often in females and older adult clients NURSING CONSIDERATIONS Teach client to notify provider for severe diarrhea. Monitor for dehydration, especially in older adults. Hypotension NURSING CONSIDERATIONS Monitor blood pressure. Advise clients to rise slowly from sitting. Advise clients to avoid activities that require alertness until effects are known. Education/Teaching/Nursing Intervention High‑ fat meals interfere with absorption. Instruct clients to take at the same time daily away from foods high in fat. Available alone or in combination tablets with a variety of other antihypertensives (e.g., hydrochlorothiazide, a diuretic; valsartan, an ARB). Calcium channel blockers Mechanism of action: SELECT PROTOTYPE MEDICATIONS Nifedipine Verapamil Diltiazem OTHER MEDICATIONS Amlodipine Felodipine Nicardipine Nifedipine Blocking of calcium channels in blood vessels leads to vasodilation of vascular smooth muscle (peripheral arterioles) and arteries/arterioles of the heart. Nifedipine acts primarily on arterioles. Veins are not significantly affected. Verapamil, diltiazem Blocking of calcium channels in blood vessels leads to vasodilation of peripheral arterioles and arteries/ arterioles of the heart. Blocking of calcium channels in the myocardium, SA node, and AV node leads to a decreased force of contraction, decreased heart rate, and slowing of the rate of conduction through the AV node. These medications act on arterioles and the heart at therapeutic doses. Veins are not significantly affected.Pharmacology Study Guide Exam 3 Indication of usage: Adverse effects: NIFEDIPINE Reflex tachycardia NURSING CONSIDERATIONS: Monitor clients for an increased heart rate. Administer a beta‑ blocker (metoprolol) to counteract tachycardia. Acute toxicity NURSING CONSIDERATIONS: With excessive doses, the heart, in addition to blood vessels, is affected. Monitor vital signs and ECG. Provide gastric lavage and cathartic if indicated. Administer medications (norepinephrine, calcium, isoproterenol, lidocaine, and IV fluids). Have equipment for cardioversion and cardiac pacer available. Orthostatic hypotension and peripheral edema NURSING CONSIDERATIONS: Monitor blood pressure, edema, and daily weight. Instruct clients to observe for swelling in the lower extremities, and notify the provider if it occurs. A diuretic can be prescribed to control edema. Instruct clients about the manifestations of postural hypotension (lightheadedness, dizziness). If these occur, advise clients to sit or lie down. Can be minimized by getting up slowly. VERAPAMIL, DILTIAZEM Orthostatic hypotension and peripheral edema NURSING CONSIDERATIONS: Monitor blood pressure, edema, and daily weight. Instruct clients to observe for swelling in the lower extremities, and notify the provider ifPharmacology Study Guide Exam 3 it occurs. A diuretic can be prescribed to control edema. Instruct clients about the manifestations of postural hypotension (lightheadedness, dizziness). If these occur, advise clients to sit or lie down. Can be minimized by getting up slowly. Constipation (primarily verapamil) CLIENT EDUCATION: Advise clients to increase intake of high fiber food and oral fluids, if not restricted. Suppression of cardiac function Bradycardia, heart failure NURSING CONSIDERATIONS: Monitor ECG, pulse rate, and rhythm. Advise clients to observe for suppression of cardiac function (slow pulse, activity intolerance), and to notify provider if these occur. Discontinue medication if needed. Dysrhythmias QRS complex is widened and QT interval is prolonged. NURSING CONSIDERATIONS: Monitor vital signs and ECG. Acute toxicity Resulting in hypotension, bradycardia, AV block, and ventricular tachydysrhythmias NURSING CONSIDERATIONS: Monitor vital signs and ECG. Gastric lavage and cathartic can be indicated. Administer medications (norepinephrine, calcium, isoproterenol, lidocaine, and IV fluids). Have equipment for cardioversion and cardiac pacer available. Education/Teaching/Nursing Intervention Pregnancy Risk Category C. Nifedipine is contraindicated in clients who are in cardiogenic shock. Use nifedipine with caution in clients who have acute MI, unstable angina, aortic stenosis, hypotension, sick sinus syndrome, and second‑ or third‑ degree AV block. Verapamil is contraindicated in clients who have hypotension, heart block, digoxin toxicity, severe heart failure, and during lactation. Use cautiously in older adults and clients who have kidney or liver disorders, mild to moderate heart failure, or GERD. Alpha adrenergic blockers (sympatholytics) Mechanism of action: SELECT PROTOTYPE MEDICATION: PrazosinPharmacology Study Guide Exam 3 OTHER MEDICATIONS: Doxazosin Terazosin EXPECTED PHARMACOLOGICAL ACTION Selective alpha1 blockade results in the following. Venous and arterial dilation Smooth muscle relaxation of the prostatic capsule and bladder neck Indication of usage: Primary hypertension. Doxazosin and terazosin are used to decrease manifestations of benign prostatic hyperplasia (BPH), which include urgency, frequency, and dysuria. Adverse effects: First‑ dose orthostatic hypotension NURSING CONSIDERATIONS Start treatment with low dosage of medication. First dose often is given at night. Monitor blood pressure for 2 to 6 hr after initiation of treatment. Instruct clients to avoid activities requiring mental alertness for the first 12 to 24 hr. Instruct clients to change positions slowly and to lie down if feeling dizzy, lightheaded, or faint. Education/Teaching/Nursing Intervention Instruct clients that the medication can be taken with food. Recommend that clients take the initial dose at bedtime to decrease “first‑ dose” hypotensive effect. Advise client about safety measures to minimize effects of orthostatic hypotension/dizziness. Centrally acting- alpha2 agonists Mechanism of action: SELECT PROTOTYPE MEDICATION: Clonidine OTHER MEDICATIONS: Guanfacine Methyldopa These medications act within the CNS to decrease sympathetic outflow resulting in decreased stimulation of the adrenergic receptors (both alpha and beta receptors) of the heart and peripheral vascular system. Decrease in sympathetic outflow to the myocardium results in bradycardia and decreased cardiac output (CO).Pharmacology Study Guide Exam 3 Decrease in sympathetic outflow to the peripheral vasculature results in vasodilation, which leads to decreased blood pressure. Indication of usage: Primary hypertension (administered alone, with a diuretic, or with another antihypertensive agent) Severe cancer pain (administered parenterally by epidural infusion) INVESTIGATIONAL USE Migraine headache Flushing from menopause Management of ADHD and Tourette syndrome Management of withdrawal from alcohol, tobacco, and opioids Adverse effects: Drowsiness and sedation NURSING CONSIDERATIONS Drowsiness will diminish as use of medication continues. Advise clients to avoid activities that require mental alertness until manifestations subside. Education/Teaching/Nursing Intervention: Dry mouth CLIENT EDUCATION Advise clients to be compliant with medication regimen. Reassure clients that dry mouth usually resolves in 2 to 4 weeks. Encourage clients to chew gum or suck on hard candy, and to take small amounts of water or ice chips. Rebound hypertension if abruptly discontinued NURSING CONSIDERATIONS: Advise clients not to discontinue treatment without consulting the provider. Discontinue clonidine gradually over 2 to 4 days. Education/Teaching/Nursing Intervention: Administer medication by oral, epidural, and transdermal routes. Medication is usually administered twice a day in divided doses. Take larger dose at bedtime to decrease the occurrence of daytime sleepiness. Transdermal patches are applied every seven days. Advise clients to apply patch on hairless, intact skin on torso or upper arm. Beta adrenergic blockers (sympatholytics) Mechanism of action: SELECT PROTOTYPE MEDICATIONSPharmacology Study Guide Exam 3 Cardioselective: Beta1 (affects only the heart) Metoprolol Atenolol Esmolol Nonselective: Beta1 and beta2 (affecting both the heart and lungs) Propranolol Nadolol Alpha and beta blockers Carvedilol Labetalol In cardiac conditions, the primary effects of beta‑ adrenergic blockers are a result of beta1‑ adrenergic blockade in the myocardium and in the electrical conduction system of the heart. Decreased heart rate (negative chronotropic [rate] action). Decreased myocardial contractility (negative inotropic [force] action); decreases cardiac output. Decreased rate of conduction through the AV node (negative dromotropic action). Alpha blockade adds vasodilation in medications such as carvedilol and labetalol. Reduces release of renin which decreases angiotensin II and causes vasodilation and promotes excretion of sodium and water. Indication of usage: Primary hypertension (exact mechanism unknown: long‑ term use causes reduction in peripheral vascular resistance). Angina, tachydysrhythmias, heart failure, and myocardial infarction. Suppresses reflex tachycardia due to vasodilators. Other uses can include treatment of hyperthyroidism, migraine headache, pheochromocytoma, and glaucoma Adverse effects: BETA1 BLOCKADE: METOPROLOL, PROPRANOLOL Bradycardia NURSING CONSIDERATIONS Monitor pulse. If below 50/min, hold medication and notify the provider. Use cautiously in clients who have diabetes mellitus. This medication can mask tachycardia, an early manifestation of low blood glucose. Advise clients to monitor blood glucose to detect hypoglycemia. Decreased cardiac output NURSING CONSIDERATIONSPharmacology Study Guide Exam 3 Use cautiously with clients who have heart failure. Doses are started very low and titrated to the desired level. Advise clients to observe for manifestations of worsening heart failure (shortness of breath, edema, weight gain, fatigue). Notify the provider if manifestations occur. AV block NURSING CONSIDERATIONS: Obtain a baseline ECG and monitor. Orthostatic hypotension CLIENT EDUCATION Advise clients to sit or lie down if experiencing dizziness or faintness. Advise clients to avoid sudden changes of position and rise slowly. Rebound myocardium excitation NURSING CONSIDERATIONS: The myocardium becomes sensitized to catecholamines with long‑ term use of beta‑ blockers. Advise clients not to stop taking beta‑ blockers abruptly, but to follow the provider’s instructions. Discontinue use of beta‑ blockers over 1 to 2 weeks. BETA2 BLOCKADE: PROPRANOLOL Bronchoconstriction NURSING CONSIDERATIONS Avoid in clients who have asthma. Clients who have asthma should receive a beta1 selective agent. Glycogenolysis is inhibited NURSING CONSIDERATIONS Clients who have diabetes mellitus rely on the breakdown of glycogen into glucose to manage low blood glucose (can happen with insulin overdose). In addition, a decreased heart rate can further mask manifestations of impending low blood glucose level. Clients who have diabetes mellitus receive a beta1 selective agent. Education/Teaching/Nursing Intervention Administer medications orally, usually once or twice a day. Atenolol, metoprolol, labetalol, and propranolol can be administered by the IV route.Pharmacology Study Guide Exam 3 Advise clients not to discontinue medication without consulting the provider. Advise clients to avoid sudden changes in position to prevent occurrence of orthostatic hypotension. Instruct clients not to crush or chew extended‑ release tablets. Teach clients to self‑ monitor heart rate and blood pressure at home on a daily basis. Take with food to increase absorption. Medications for hypertensive crisis Mechanism of action: SELECT PROTOTYPE MEDICATION: Nitroprusside (centrally‑ acting vasodilator) OTHER MEDICATIONS Nitroglycerin (vasodilator) Nicardipine (calcium channel blocker) Clevidipine (calcium channel blocker) Enalaprilat (ACE inhibitor) Esmolol (beta blocker) EXPECTED PHARMACOLOGICAL ACTION: Direct vasodilation of arteries and veins resulting in rapid reduction of blood pressure (decreased preload and afterload). Indication of usage: Hypertensive crisis Adverse effects: Excessive hypotension NURSING CONSIDERATIONS Administer medication slowly because rapid administration will cause blood pressure to go down rapidly. Monitor blood pressure and ECG continuously. Keep client supine during administration. Cyanide poisoning/thiocyanate toxicity Headache and drowsiness, and can lead to cardiac arrest Nitroprusside only NURSING CONSIDERATIONS Clients who have liver dysfunction are at increased risk. Risk of cyanide poisoning is reduced by administering medication for no longer than 3 days, and at a rate of 5 mcg/kg/min or less. Avoid prolonged use of nitroprusside. Manifestations include weakness, disorientation and delirium. Administer thiosulfate to reverse effects.Pharmacology Study Guide Exam 3 Monitor plasma levels if used for more than 3 days. Level should be maintained at less than 10 mg/dL. Discontinue medication if cyanide toxicity occurs. Education/Teaching/Nursing Intervention: Prepare medication by adding to diluent for IV infusion. Note color of solution. Solution can be light brown in color. Discard solution of any other color. Protect IV container and tubing from light. Discard medication after 24 hr. Monitor vital signs and ECG continuously. Chapter 27: ATI PG.163 Ch 21 Drugs for heart failure Mechanism of action of different classifications o Indication of usage o Adverse effects o Education/Teaching/nursing interventions Mechanism of action: Indication of usage: Adverse effects: Education/Teaching/Nursing Intervention Cardiac Glycosides and Heart Failure Mechanism of action: SELECT PROTOTYPE MEDICATION: Digoxin EXPECTED PHARMACOLOGICAL ACTION Positive inotropic effect: increased force of myocardial contraction Increased force and efficiency of myocardial contraction improves the heart’s effectiveness as a pump, improving stroke volume and cardiac output. Negative chronotropic effect: decreased heart rate At therapeutic levels, digoxin slows the rate of sinoatrial (SA) node depolarization and the rate of impulses through the conduction system of the heart. A decreased heart rate gives the ventricles more time to fill with blood coming from the atria, which leads to increased SV and increased CO. Indication of usage: As a second‑ line medicationPharmacology Study Guide Exam 3 Treatment of heart failure Dysrhythmias (atrial fibrillation) Can reduce manifestations, but does not prolong life Adverse effects: Education/Teaching/Nursing Intervention Adverse effects: Dysrhythmias, cardiotoxicity Dysrhythmias caused by interfering with the electrical conduction in the myocardium). Cardiotoxicity leading to bradycardia NURSING CONSIDERATIONS Conditions that increase the risk of developing digoxin‑ induced dysrhythmias include hypokalemia, increased serum digoxin levels, and heart disease. Older adult clients are particularly at risk. Monitor serum levels of K+ to maintain a level between 3.5 to 5.0 mEq/L. Instruct clients to report manifestations of hypokalemia (nausea/vomiting, general weakness). Potassium supplements are prescribed if clients are concurrently taking a diuretic. Teach clients to consume high‑ potassium foods (green leafy vegetables, bananas, potatoes). Monitor digoxin level. Therapeutic serum levels can vary, but usually range from 0.5 to 0.8 ng/mL. Dosages should be based on serum levels and client response to medication. Teach clients to monitor pulse rate, and recognize and report changes, such as irregular rate with early or extra beats. GI effects Include anorexia (usually the first manifestation of toxicity), nausea, vomiting, and abdominal pain. CLIENT EDUCATION: Teach clients to monitor for these effects and report to the provider if they occur. CNS effects Include fatigue, weakness, vision changes(diplopia, blurred vision, yellow‑ green or white halos around objects). CLIENT EDUCATION: Teach clients to monitor for these effects and report to the provider if they occur Education/Teaching/Nursing Intervention. Education/Teaching/Nursing Intervention Advise clients to take the medication as prescribed. If a dose is missed, the next dose should not be doubled. Check pulse rate and rhythm before administration of digoxin and record. Notify the provider if heart rate is less than 60/min in an adult, less than 70/min in children, and less than 90/min in infants.Pharmacology Study Guide Exam 3 Administer digoxin at the same time daily. Monitor digoxin levels periodically during treatment and maintain therapeutic levels between 0.5 and 0.8 ng/mL to prevent digoxin toxicity. Avoid taking OTC medications to prevent adverse effects and medication interactions. Instruct clients to observe for manifestations of hypokalemia, such as muscle weakness, and to notify the provider if they occur. Instruct clients to observe for indications of digoxin toxicity (fatigue, weakness, vision changes, GI effects), and to notify the provider if they occur. If administering IV digoxin, infuse over at least 5 min, (10 to 15 min in clients who have pulmonary edema) and monitor client for dysrhythmias. Adrenergic agonists Mechanism of action: SELECT PROTOTYPE MEDICATION: Catecholamines Epinephrine Dopamine Dobutamine Isoproterenol Norepinephrine OTHER MEDICATIONS Albuterol Ephedrine SITE/RESPONSE Alpha1 receptors Activation of receptors in arterioles of skin, viscera and mucous membranes, and veins leads to vasoconstriction. Mydriasis (dilation of pupil) Beta1 receptors Heart stimulation leads to increased heart rate, increased myocardial contractility, and increased rate of conduction through the AV node. Activation of receptors in the kidney lead to the release of renin. Beta2 receptors Activation of receptors in the arterioles of the heart, lungs, and skeletal muscles leads to vasodilation. Bronchial stimulation leads to bronchodilation. Activation of receptors in uterine smooth muscle causes relaxation.Pharmacology Study Guide Exam 3 Activation of receptors in the liver cause glycogenolysis. Skeletal muscle receptor activation leads to muscle contraction. Dopamine receptors Activation of receptors in the kidney cause the renal bloodvessels to dilate. MEDICATIONS: Epinephrine Alpha1 receptors PHARMACOLOGICAL ACTION: Vasoconstriction THERAPEUTIC USE o Slows absorption of local anesthetics o Manages superficial bleeding o Decreased congestion of nasal mucosa o Increased blood pressure Beta1 receptors PHARMACOLOGICAL ACTION o Increased heart rate o Increased myocardial contractility o Increased rate of conduction through the AV node o Increased cardiac output o Improved tissue perfusion THERAPEUTIC USE: Treatment of AV block, heart failure, shock, and cardiac arrest Beta2 receptors o PHARMACOLOGICAL ACTION: Bronchodilation THERAPEUTIC USE: Asthma Dopamine Low dose: Beta1 o PHARMACOLOGICAL ACTION: Renal blood vessel dilation THERAPEUTIC USE o Shock o Heart failure o Acute kidney injury Moderate dose: Beta1 PHARMACOLOGICAL ACTION o Renal blood vessel dilation o Increased heart rate o Increased myocardial contractility o Increased rate of conduction through the AV node THERAPEUTIC USE o Shock o Heart failurePharmacology Study Guide Exam 3 High dose: Beta1, alpha1 PHARMACOLOGICAL ACTION o Renal blood vessel constriction o Increased heart rate o Increased myocardial contractility o Increased rate of conduction through the AV node o Vasoconstriction THERAPEUTIC USE o Shock o Heart failure Dobutamine Beta1 PHARMACOLOGICAL ACTION o Increased heart rate o Increased myocardial contractility and cardiac output o Increased rate of conduction through the AV node THERAPEUTIC USE: Heart failure Adverse effects: EPINEPHRINE Vasoconstriction Hypertensive crisis due to activation of alpha1 receptors in the heart. NURSING CONSIDERATIONS: Provide for continuous cardiac and blood pressure monitoring. Report changes in vital signs to the provider. Cardiac complications Dysrhythmias due to activation of beta1 receptors in the heart. Beta1 receptor activation also increases the workload of the heart and increases oxygen demand, leading to the development of angina. NURSING CONSIDERATIONS: Provide for continuous cardiac monitoring. Monitor clients closely for dysrhythmias, change in heart rate, and chest pain. Notify the provider of dysrhythmias, increased heart rate, and chest pain. Treat per protocol. DOPAMINEPharmacology Study Guide Exam 3 Cardiac complications Beta1 receptor activation in the heart can cause dysrhythmias. Beta1 receptor activation also increases the workload of the heart and increases oxygen demand, leading to development of angina. NURSING CONSIDERATIONS Provide for continuous cardiac monitoring. Monitor clients closely for dysrhythmias, change in heart rate, and chest pain. Notify the provider of dysrhythmias, increased heart rate, and chest pain. Treat per protocol. Necrosis Can occur from extravasation of high doses of dopamine NURSING CONSIDERATIONS: Monitor IV site carefully. Infuse through central IV line if possible. Discontinue infusion at first indication of irritation. If extravasation occurs, administer phentolamine, an alpha blocker to counteract alpha mediated vasoconstriction. DOBUTAMINE Increased heart rate NURSING CONSIDERATIONS Provide continuous cardiac monitoring. Report changes in vital signs to the provider. Education/Teaching/Nursing Intervention These medications must be administered IV by continuous infusion. Use an IV pump to control infusion. Dosage is titrated based on blood pressure response. Stop the infusion of dopamine at first evidence of infiltration. Extravasation can be treated with local injection of an alpha‑ adrenergic blocking agent, such as phentolamine. Assess/monitor for chest pain. Notify the provider if chest pain occurs. Monitor urine output frequently for indications of decreased kidney perfusion. Monitor ECG continuously, and notify provider of indications of tachycardia or dysrhythmias. Monitor perfusion to extremities. Monitor cardiac output, pulmonary capillary wedge pressure, central venous pressure. [Show More]
Last updated: 2 years ago
Preview 1 out of 19 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$12.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Mar 18, 2021
Number of pages
19
Written in
Additional information
This document has been written for:
Uploaded
Mar 18, 2021
Downloads
0
Views
59