Discussion Board Week 8
Liberty University
Reviewing this week’s discussion prompt and then engaging in the topic was a eye opener and a
tragedy. According to Nwosu (2015), medical errors are a common cause of mortali
...
Discussion Board Week 8
Liberty University
Reviewing this week’s discussion prompt and then engaging in the topic was a eye opener and a
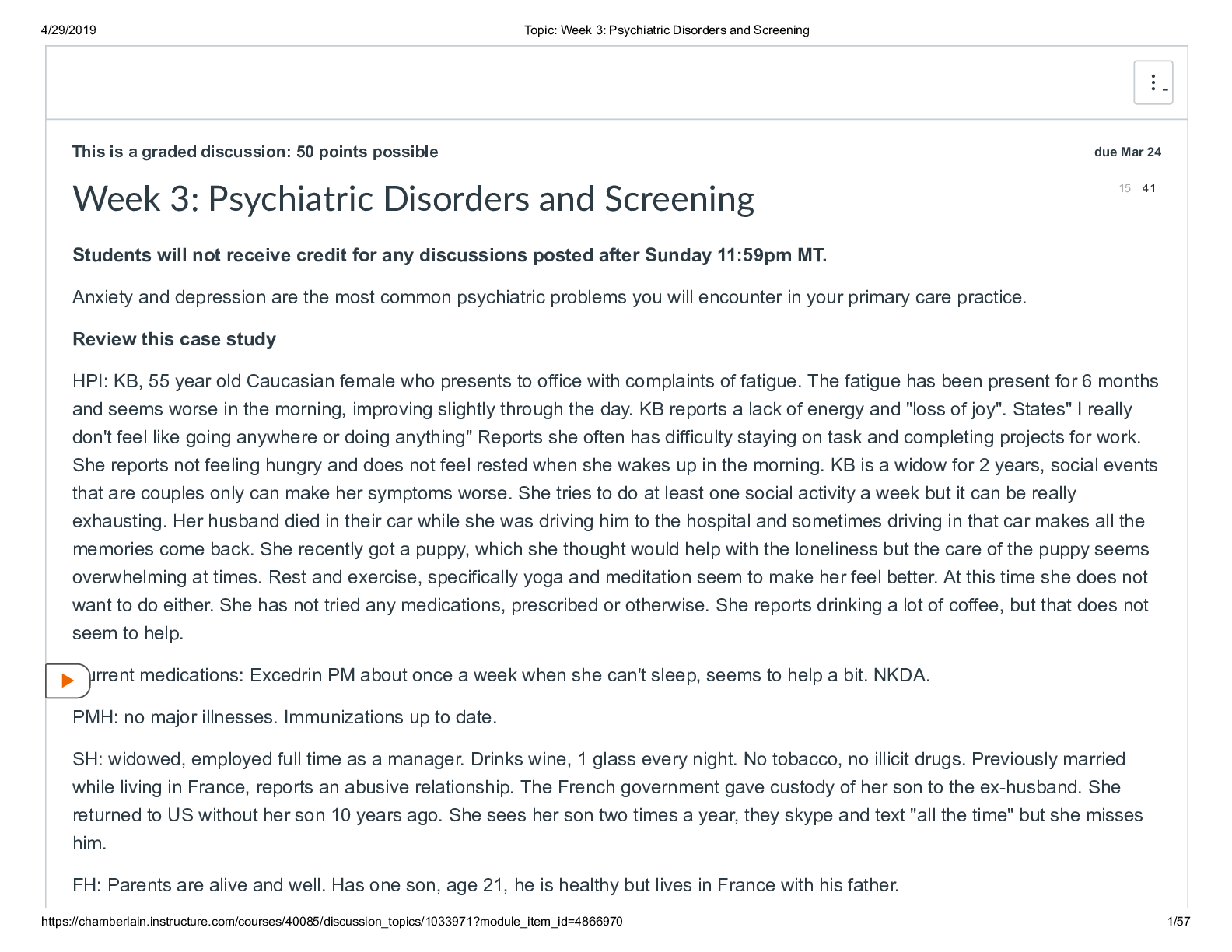
tragedy. According to Nwosu (2015), medical errors are a common cause of mortality and morbidity
among patients” (p.4). However, after reviewing both cases, it is evident that these errors do happen and
with all the academic training and knowledge of the providers the may happen again. The question then
becomes, how do the physician and the surgical staff mitigate these erroneous wrong-site surgeries or
mistakes. Ojeda (2015) in research spoke about accuracy as an important factor for registration and
identification of the correct patient. According to a research by the Institute of Medicine in 2000 “To err
is human: building a safer health system” which was later quoted in several journals recently, highlighted
the fact that in health care, building a safer system means designing processes of care to ensure that
patients are safe from accidental injury. When agreement has been reached to pursue a course of
medical treatment, patients should have the assurance that it will proceed correctly and safely so they
have the best chance possible of achieving the desired outcome.
The article also highlighted that of the two cases, the patients involved and the procedures that
ensued in the lower extremities was not reported as incident officially to the hospital administration,
which in retrospect may be an in-action caused by denial and shame, consequently no audit or root
cause analysis was instituted (Nwosu, 2015). Surprisingly, within the USA itself, research has shown that
it is a small number of these wrong-site surgery that do get traction to litigation in the courts. In fact,
according to Ojeda (2015), only 2% of these orthopedic malpractice claims in the USA get an award from
successful litigation.
The Institute of Medicine has identified that up to 98,000 patients die each year as a result of
poor decision-making in healthcare (Panesar et al., 2016). Decision-making is essential to nursing
practice (Panesar et al., 2016). Decision-making in acute care nursing practice is a complex process.
Nurses must consider numerous, potentially competing factors when making decisions to meet patient
and family needs. This process is further complicated by the fact that nurses may care for five or more
patients in an acute care environment (Ragusa et al., 2015). Research identifies other factors associated
with decision-making challenges for acute care nurses. For instance, critical care nurses can make
decisions every 30 seconds. Nurse decision-making in acute care is highly demanding. Improved
understanding of decision-making research in this environment may help to guide future efforts to
support nursing practice (Nibbelink, 2018).
Incorrect or missing data in electronic health records is one of the top 10 patient safety concerns
identified in a recent Institute report (Ragusa et al., 2015). Inaccurate registration information can harm
patients in a few ways, test results might be sent to the incorrect physician, the wrong patient’s
information might be added to another patient’s account, Incorrect dosages can be given if outdated
weights in registration systems are shared with pharmacy systems. Also, registration accuracy is “a very
significant issue in terms of patient safety. In a recent survey of states conducted by the Joint
Commission on Accreditation of Healthcare Organizations (JCAHO), it was found that at least one-third of
states have some form of adverse event reporting system. The committee also believes that voluntary
reporting systems play a valuable role in encouraging improvements in patient safety and are a
complement to mandatory reporting systems (Rajasekar, 2015).
[Show More]



.png)
.png)

.png)