*NURSING > Solutions Guide > Health Assessment objectives NURS 3020 (All)
Health Assessment objectives NURS 3020
Document Content and Description Below
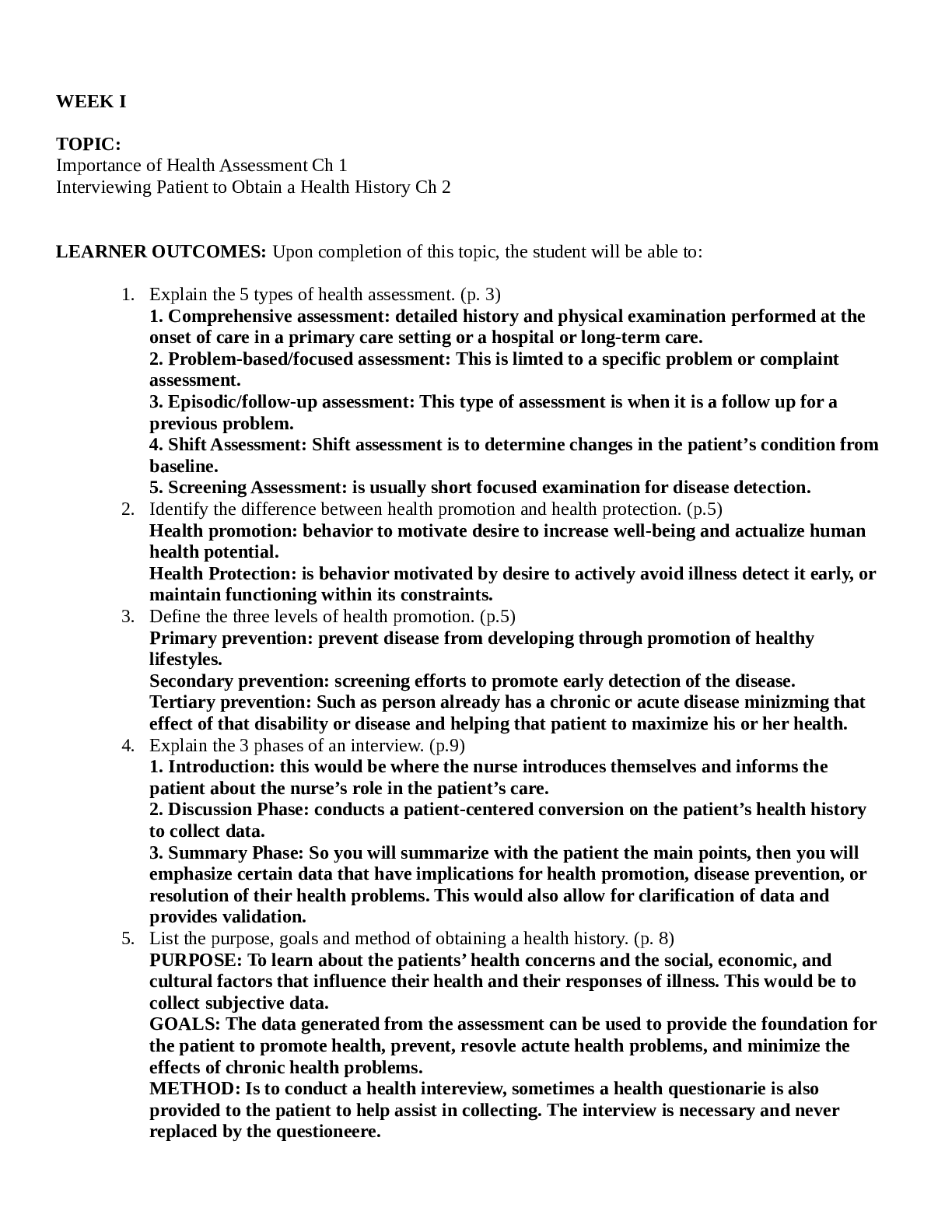
LEARNER OUTCOMES: Upon completion of this topic, the student will be able to: 1. Explain the 5 types of health assessment. (p. 3) 1. Comprehensive assessment: detailed history and physical examinati ... on performed at the onset of care in a primary care setting or a hospital or long-term care. 2. Problem-based/focused assessment: This is limted to a specific problem or complaint assessment. 3. Episodic/follow-up assessment: This type of assessment is when it is a follow up for a previous problem. 4. Shift Assessment: Shift assessment is to determine changes in the patient’s condition from baseline. 5. Screening Assessment: is usually short focused examination for disease detection. 2. Identify the difference between health promotion and health protection. (p.5) Health promotion: behavior to motivate desire to increase well-being and actualize human health potential. Health Protection: is behavior motivated by desire to actively avoid illness detect it early, or maintain functioning within its constraints. 3. Define the three levels of health promotion. (p.5) Primary prevention: prevent disease from developing through promotion of healthy lifestyles. Secondary prevention: screening efforts to promote early detection of the disease. Tertiary prevention: Such as person already has a chronic or acute disease minizming that effect of that disability or disease and helping that patient to maximize his or her health. 4. Explain the 3 phases of an interview. (p.9) 1. Introduction: this would be where the nurse introduces themselves and informs the patient about the nurse’s role in the patient’s care. 2. Discussion Phase: conducts a patient-centered conversion on the patient’s health history to collect data. 3. Summary Phase: So you will summarize with the patient the main points, then you will emphasize certain data that have implications for health promotion, disease prevention, or resolution of their health problems. This would also allow for clarification of data and provides validation. 5. List the purpose, goals and method of obtaining a health history. (p. 8) PURPOSE: To learn about the patients’ health concerns and the social, economic, and cultural factors that influence their health and their responses of illness. This would be to collect subjective data. GOALS: The data generated from the assessment can be used to provide the foundation for the patient to promote health, prevent, resovle actute health problems, and minimize the effects of chronic health problems. METHOD: Is to conduct a health intereview, sometimes a health questionarie is also provided to the patient to help assist in collecting. The interview is necessary and never replaced by the questioneere. 6. Identify the factors that affect the physical setting in an interview. PRIVACY: patient should have privacy when conducting interview PHYSICALLLY COMFORTORBALE: They should remain in street clothes during the intrewiew, during the examination they can change into a gown. NO DISTRACTIONS: try to minimize interruption or distractions during an interview. 7. Describe 4 attributes for professional behavior of the nurse during an interview. 1. First impression is the nurses appearance. 2. Nurses interpersonal skills they must have a professional demeanor but warm tone 3. Nurses should also be active listerners, need to understand the patient’s point of view. 4. Nonverbal behavior, try to avoid extreme gestures or reactions. 8. Identify appropriate uses of communication techniques and open and closed-ended questions to elicit information during the history and physical examination. (p. 10-11) Questions should be clearly spoken and understood by the patient. So have questions that are adapted to the patients developmental level, knowledge, and understanding. Ask one question at a time, wait till they reply before asking another question. If something the patients states is confusing then the nurse may ask for clarification. So if a nurse needs to talk about sensitive or personal issues the nurse needs to address the patient and state that they will ask personal or sensitive questions. Begin interviews with open-ended questions. OPEN ENDED QUESTIONS: this allow for free-flowing open responses CLOSE ENDED QUESTIONS: These are more direct and precise questions, that only require one or two words to respond to. DIRECTIVE QUESTIONS: are questions that lead patients to focus on one set of thoughts. 9. Demonstrate the use of open and closed ended questions. (p. 11) OPEN ENDED QUESTION: Such as the onset of symptom a patient can describe it in more than one to two words. The open-ended question should not be too broad, and focus on the patient’s health. CLOSED ENDED QUESTIONS: These can provide options such as saying to patient that it sharp, dull or aching type of pain. These are used in combination with open-ended questions. 10. Identify and explain the use of techniques for enhancing data collection. (p.11) Active Listening: This is listening with a purpose to the patient, also notcing their nonverbal cues. Facilitation: These are pharses the nurse use to allow the patient to continue talking. Such as “go on” Clarification: This are statements made by the nurse to get information on conflicting, vague or unclear statements made by the patient. Restatement: This is where the nurse repeats what the patient said in order for the nurse to get a confirmation. Reflection: This where the nurse would ask a question to get clarification on a pharase or sentence the patient stated: P: “I didn’t feel well this moring” N: “You didn’t feel well?” P: “I was dizzy this morinng” Confrontation: This is used when there is inconsistences that are noted between what the patient reports and the observation and other data about the patient. You would use pharase such as “I am confused, you said this, but the report shows you gain weight” Need to have confusing tone with patient. Interpretation: This where the nurse shares with the patient all the subjective data the patient provided to the nurse. SO that the patient can confirm, deny, or improve (revise) the information. Summary: This is just condenses the data obtained during the interveiew, good for patients who ramble. 11. Describe techniques that diminish data collection. (p. 12) Using Medical Terminology: So using medical terminology or acronyms with the patient can interfere with communication process. Expressing Value Judgments: These are ways that nurse tries to state their values such as telling a patient that they don’t wear protection during intercose. Interrupting the Patient: You must allow the patient to finish their sentences, do not become impatient and finish their sentences. Nurses need to give the patient time to allow them the opportunity to finish their thoughts. Being Authoritarian or Paternalistic: Nurses who say I know what is best for you, or do what I say would make the patient igonore the nurse advice or disreagard it. Using “Why” Questions: Using the why question may seem threating and put patients in the defensive mode. Instead say questions w/o why, such as I noticed that you or I’m curious about the reason. 12. Define 3 types of awkward moments and how to manage them during a health history interview. (p.12) Answering personal questions: Just give a brief, direct answer. It could be useful especially experiences such as parental experiences could enhance the relationship with the patient. Silence: Some patients need silence, such as some issues can be so painful that silence is necessary. Nurses should become comfortable with silence it can be useful. Displays of Emotion: Crying is natural emotion, do not say “Don’t Cry” that is not a therapeutic response. Saying responses as “Take all the time you need to express your feeling”, May need to postpone the questioning until the patient is ready. When patient is angry, then need to discuss with the patient such as stating “You seem angry, can you tell me the reason why you are feeling that way?” If they are angry with someone else then try to discuss with that person about why they are angry with them. If they are angry with a nurse, try to encourage them to discuss their feeling. Acknoledwege their feelings, and if appropriate apologize to them. If they are still angry the nurse another nurse may need to come in. 13. Identify variables in the process of obtaining a health history that impact on the content of information received. (environment, verbal and non-verbal skills). (p. 13-13) Mangaing the Overly Talkative Patient: The nurse would tactifully redirect the converstation, use of close-ended questions can help redirect the conversation. Others in the Room: If the adult or adolscene patient is able to speak for themselves, then they should be interviwed directly and in private. If others are in the room, the nurse must have patient’s approval for the others to be present during the interview. If someone keeps answering for the patient, the nurse can ask that person to allow the patient themselves to answer if not, the nurse can ask that person to leave the room until the end of the interview. Language Barrier: Have a translator over a patient’s family member as they may alter the meaning of what your saying to the patient. Must also have time when using a interpator. Cultural Differences: Patient-centered care is provided when the nurse develops culturally competence to identify cultural factors that may influence patients beliefs about health and illness. Cultural competence is when the nurse is able to communicate between and among culture of origin. They must interact with each individual as unique individuals. 14. Determine key data to be obtained in each of the following components of a health history: (p. 14- 17) a. Biographic data: Name, Gender, Address, telephone #, email address, Birth date, Birthplace, Race/ethnicity, Religion, Marital status, occupation, contact person, and source of data, b. Reason for Seeking Health Care: called chief complaint or presenting problem is brief statement of why the patient is seeking care, this is written in direct quotes. c. History of present illness: So the nurse ask them and writes as is, but the nurse needs more details hence using a symptom anaylsis which is systematic way to collect data about the history and status of symptoms. Using OLD CARTS to gather history of illness. d. Present health status: Health conditions, medications, allergies. e. Past Health History: Childhood illness, Surgeries, Hospitaliz [Show More]
Last updated: 3 years ago
Preview 1 out of 50 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$8.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
May 05, 2021
Number of pages
50
Written in
All
Additional information
This document has been written for:
Uploaded
May 05, 2021
Downloads
0
Views
179



 V1-V2.png)