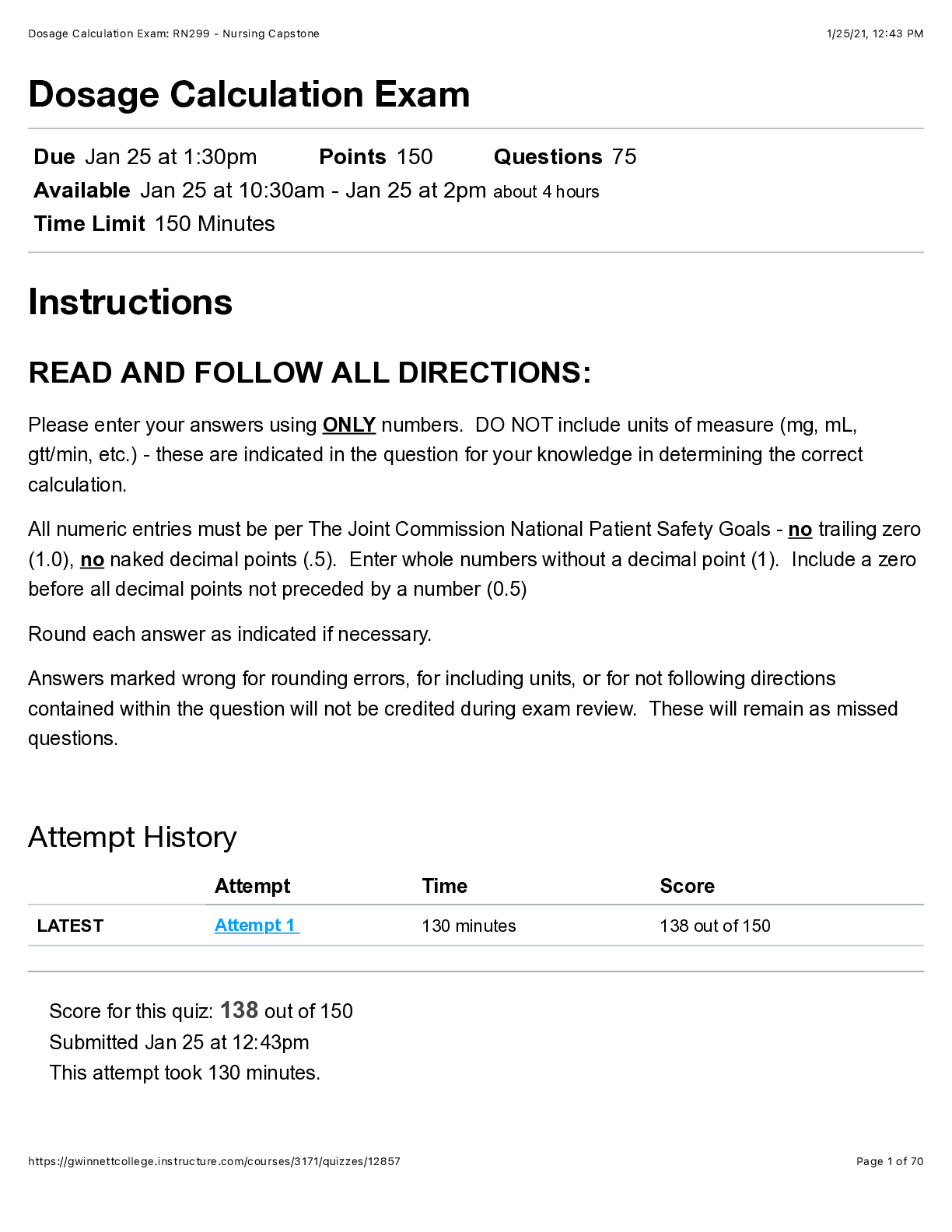
Dosage Calculation Exam: RN299 - Nursing Capstone.
Micro Biology > Class Notes > MICROIMM 2500B Micro MIDTERM 2 NOTES (All)
MICROIMM 2500B Micro MIDTERM 2 NOTES Lecture 1: Introduction to Bacteriology - There are not that many bacteria that are actually pathogenic; most bacteria are beneficial - Prokaryotes: the smalle ... st, simplest and most abundant cells on earth; includes bacteria and archaea - Lack a nucleus and complex organelles - Viruses outnumber the amount of prokaryotes - Bacteria can grow fast - bacteria reproduce by binary fission - 4 stages of growth: lag, log phase, stationary growth, and then death - Some bacteria are very slow at growing and they can cause disease. E.g. Tuberculosis - Bacteria classification by shape - Coccus looks like a sphere - Rods can also be called visills - Spirillium are spiral shaped ones - Bacteria classification by oxygen utilization - Obligate aerobe: require oxygen for growth - Obligate anaerobe: oxygen is toxic for growth - Facultative anaerobe: can use oxygen if present and grow better with it, but can also grow without oxygen - Aerotolerant anaerobe: doesn’t use oxygen but oxygen is not toxic - Microaerophile: grow best with low levels of oxygen - Can have two strains of bacteria that look the same but can have a completely different genome Gram Stain - Two general types of bacteria - Gram positive = purple - Gram negative = pink - Don’t stain for mycoplasma because they don’t stain as a result of weird cell envelopes - Don’t stain for mycoplasma because they don’t have cell walls 1. Put cells onto slide which is slightly hot to make sure that they are there 2. Stain the slide with a crystal violet 3. Put iodine onto the slide as well so that the purple will get into some of the cells 4. Wash the cells on the slide with a pray bottle of ethanol - This causes the purple to come off of the gram negative and the gram positive would get it stuck in their thick cell wall - The cell wall of the gram + is very thick while that of the gram – is very thin 5. Counter stain with safrinin so that the gram negative are pink Gram positive and gram negative cell envelopes - The peptidoglycan is a thick layer on the gram positive- It is the same thing as the cell wall - The gram negative has 2 membranes: an outer membrane and a cytoplasmic membrane - There is still a peptidoglycan structure in between the membranes that is separated by the periplasmic space - Both have a cytoplasmic membrane - Lipopolysaccharide is a part of the gram – - Teichoic acids and lipoteichoic acids are part of gram + Bacterial cell walls (peptidoglycan) - Rigid structure - Prevents osmotic lysis - This structure is unique for bacteria so it can be a target for antibiotics - If you get rid of the cell wall, it will die from exposure to enzymes and blow up - Backbone is an alternating backbone of G and M all the way around the bacterial cell - Between the M, there is a peptide linkage - Gram positive cell wall: can be forty layers or so thick - Crystal violet gets stuck in the meshwork not allowing it to be washed out looks purple - Gram-negative cell wall - Some antibiotics that we use to kill bacteria cannot get across the outer membrane - Thin peptidoglycan in the middle Lipopolysaccharide (Endotoxin) - Endotoxin because it is part of the outer membrane - O-specific polysaccharide (also called O-antigen) - Antigenic and highly variable - At the top it sticks out - Different gram negatives have different O antigens - Core polysaccharide - Lipid A - N-Acetylglucosamine disaccharide - Fatty acid groups - Recognized by the innate immune system septic shock - If there is too much release of LPS, the immune system can be over stimulated, which can cause a cytokine storm can put you in sepsis and shock (hyper inflammatory condition) - Component that is buried in the membrane - Amphipathic Primary Functions of the Cytoplasmic Membrane - Permeability barrier: prevents leakage and functions as a gateway for transport of nutrients into and out of the cell - Protein anchor: site of many proteins involved in transport- Energy conversion: site of generation and use of the proton motive force - Around the membrane it will set up this protein gradient, which by the movement of protons into the cell can make ATP Periplasm - Only in gram negatives - Located between the outer and inner membranes - Contains: hydrolytic enzymes, proteins involved in transport of molecules into and out of the cell Nucleoid - Not the nucleus - No surrounding membrane - Single, circular chromosome in most bacteria - Haploid genomes (one set of chromosomes) Plasmids - Extrachromosomal genetic elements - Usually not required for bacterial growth - Often encode for fitness factors such as antibiotic resistance - Can be transported from bacteria to bacteria - Pieces of DNA that are outside of the chromosome and capable of replication on their own Host-microbe relationships - Commensalism: one benefits without helping or hurting the other - Mutualism: both benefit (the host and the microbe) - Parasitism: one benefits (usually the microbe) at the expense of the other (usually the host) What makes bacterial pathogen successful? - Colonization - Invasion/toxicity - Immune evasion - Transmission - Pathogens produce virulence factors – molecules produces by that pathogen that contribute to disease - Surface: LPS, Flagella, Pili, capsules, surface proteins, and secretion systems - Secreted: exotoxins - Pathogenic organisms are not trying to make you sick; they are just trying to complete their life cycle within a host - Consequence of this makes us sick Flagella - Structure that allows some bacteria to be motile (chemotaxis) - Can be an important virulence factor - Have flagella on the surface of bacteria by spinning the flagella - Spinning counterclockwise allows it to go forward (run) - If it is clockwise, it will tumble and spin towards a random direction -If there is no attractant, it is a random process and they don’t get anywhere (run, tumble, run tumble…) - If there is an attractant, the runs become longer towards the direction of the attractantPili (Fimbriae) - Primarily involved in attachment to: surfaces, host tissue, and other bacteria - Shorter compared to flagella Capsules - Usually made of exo polysaccharides - Attachment of host tissues - Protection from host immune system - Can sometimes be used in vaccines - Effective because the immune system needs to be tricked to respond to sugar - Leads to the formation of biofilms - T cells do not respond to sugars, but these capsules sometimes contain sugars Biofilms - Stages: attachment, microcolony development, biofilm development, and maturation - Bacteria live in these multicellular structures - Complex structures that have water channels so that the nutrients can get in and the waste products can leave - Sometimes they shut down in allowing stuff in and out, which makes it hard to treat because antibiotics need to have active bacteria - Become very resistant to antibodies because they are not growing; they just sit there - Some cells will come off biofilms as single cells and continue on Endospores – virulence factors in a certain context - Highly differentiated cells from within the parent cell - Highly resistant to heat, harsh chemicals, and radiation - A dormant stage of the life cycle - Most common in: soil - Only made by gram positive bacteria - You would have a vegetative cell that goes under stress where it makes a developing spore that will eventually be released - Autoclaves get rid of endospores where as if you just boiled it, it won’t get rid of endospores Exotoxins - Specialized virulence factors that are secreted from bacteria - Part of the outer membrane - Exotoxin is actively secreted out of bacteria and then will float away - Types - Hemolysins: lyse red blood cells - Extracellular enzymes - Superantigens: proteins that function to activate T cells - Like capsules, if the toxin is critical for the disease, we can make a vaccine out of this Some bacteria are intracellular pathogens - Are taken up and survive within phagocytic cells - Some force their own uptake into epithelial cells - Allows bacteria to hide from different components of the immune systemLecture 2: Plague – The Black Death - Bacterial infection - Incubation of 2-6 days, death in 2-4 days - Patients experience sudden onset of fever, chills, headaches, muscle pain, weakness - Painful swellings (buboes) of the lymph nodes in the armpits, legs, neck, and groin - High fever, delirium, mental deterioration, large blackish pustules that burst, vomiting of blood, and bleeding in the lungs The Plague of Justinian (the first pandemic) - Started in the 6th century - Caused by Yersinia pestis - Spread to the Mediterranean, Italy, and Europe - 50% of the population is estimated to have died ~100 million people - Continued in cycles for another 200 years - Gets into rodents and lives in reservoirs Yersinia - Gram-negative rod shaped bacterium - There are 3 species that are pathogenic for human - Y. enterocolitica casues yersiniosis – a rate cause of diarrhea and abdominal pain - Y. pseudotuberculosis – primarily an animal pathogen that can cause tuberculosis-like symptoms in animals, enteritis in humans - Y. pestis – cause of Plague Yersinia pestis - Pestis contagious or infectious epidemic disease - An extraordinarily virulent pathogen - Causes death in 2-4 days by sepsis and/or overwhelming pneumonia with respiratory failure - Not an efficient colonizer of humans; not a human adaptive pathogen The Black Death (the second pandemic) - Caused by Yersinia pestis - Originated in Asia and reached Europe in the late 1340s - Reduced the global population by about 100 million - Killed 1/3 of the total European population - They would put herbs and flowers in the beak so that they would not be able to smell the plague - There would sometimes be crystals in the eyes because they thought that seeing the plague would make you contagious - Many people believed this was due to “God's anger” or "Satan's influence" - Persecution of strangers, minorities, and witches - European social order, family structure, agriculture, the military and the feudal system, were destroyed The Feudal System - Political structure and social structure prevalent in Europe - A few people had everything; most had nothing - Plague provided new opportunities for peasants because positions of authority needed to be filled - Plague would kill all people regardless of position in the feudal system- Opened up opportunities for people to go up and broke the feudal system Did Y. pestis really cause the Black Death? - Extracted nucleic acids from the teeth and they were able to sequence the entire genome of the Y.pestis - The plague of Justinian strain died out and the plague today is made from a new strain - Were able to see if there was an extra virulence factor Mid 19th century (third pandemic) - Started in China and then spread to all continents - >12 million deaths in China and India alone - Reached San Francisco in 1900 – infected rats exchanged fleas with local wildlife – Y pestis is now established in southwestern U.S. Pathogenesis of Yersinia pestis - Organisms live in rodents and are transmitted by fleas - Termed a zoonotic pathogen because it comes from an animal - Y pestis causes blocking in the flea - The flea takes the blood meal - Causes regurgitation of organisms - Survives and grows in innate immune cells - Once it is transferred, Y. pestis is taken up by macrophages but survives in them - Macrophages take the organism into lymph nodes and lymph nodes will swell causing buboes - The cells destroy the macrophages once in lymph nodes and Y. pestis continues to grow extracellularly - Intracellular and extracellular bacteria - Very low infective dose - At the terminal stage, the blood contains high concentrations of bacterial cells Virulence factors of Y. Pestis - Ability to overcome immune defense mechanisms resulting in massive growth in vivo - Major virulence factors include: - LPS (septicemia) - Phospholipase (survival in the flea) - Breaks down phospholipids - Plasminogen activator clot buster (dissemination) -Host protein that breaks clots when converted into a plasmid - Yersiniabactin – iron binding siderophore - Type III secretion (typical for Gram negative intracellular pathogens) - Act as syringes and inject the factors right into host cells through pores - Secrete virulence factors (called 'effectors') directly into host cells across the host cell membrane - Effectors function to ‘poison’ the host cell by targeting host cell signaling pathways Evolution of Yersinia pestis - Y. pestis evolved from y. pseudotuberculosis - Y. pestis acquired new virulence plasmids - All pathogenic Yersinia contain pYV which encodes the type III secretion system- Y. pseudotuberculosis is primary an intestinal pathogen of animals and is found widely in the environment - Y. pestis can infect the flea and is hypervirulent in humans, but does not survive well in the animal intestine Plague - The three major forms of the disease: Bubonic plague, septicemic plague, and pneumonic plague - Bubonic plague - Most common form transmitted by flea bites - Painfully swollen lymph nodes in groin, armpits and neck - Can develop into both septicemic and pneumonic plague - 40-60% mortality if untreated - Septicemic plague - Presence of Y. pestis is systemic (in the blood) - An overwhelming and progressive bacteremia - Bacteria in the blood - Flea’s bites can now pick up Y. pestis to transmit to a new host - Patients experience gangrene and disseminated intravascular coagulation (LPS mediated) - 50-90% mortality if untreated - Clotting disorder in major organs and organ systems - Pneumonic plague - Most dangerous - Transmission via aerosols directly into the lung, or spread to lungs from septicemic plague - Short incubation - Disease can pass directly from person-to-person through coughing (coughing up blood) - 95-100% mortality if untreated, but treatable only within the first 24hrs of symptoms Transmission - Four routes for human disease - Flea-bite (most common) - Inhalation from humans (pneumonic) or animals - Handling infected animals – skin contact, scratch, bite - Ingesting infected meat - Historically rat-borne urban epidemics - Now mostly wildlife associated plague with sporadic outbreaks Diagnosis, Treatment, and Prevention - Culture and identification from bubo aspirate, sputum, blood (post-mortem) may take 4 days - Endemic regions – stains, antigen tests - Non-endemic regions? - Isolation of pneumonic plague patients - Outbreaks – insecticides to kill fleas, treat human cases with appropriate antibiotics, prophylaxis to exposed individuals Plague as a bioterrorism agent: - The centers for disease control and prevention identify plague as a category A organism - Can be easily disseminated or transmitted from person to person - Results in high mortality rates and has the potential for major public health impact- Might cause public panic and social disruption - Y. pestis is easy to grow and can grow in 2 days - Known incidents: - In 1347 the Mongol armies catapulted plague-ridden bodies over the city walls in Caffa, Ukraine - In WWII, Unit 731 of the Japanese Imperial Army infected fleas and released them in China - Larry Wayne Harris, an American "microbiologist", with suspect motives obtained Y. pestis through the mail (American Type Culture Collection) - WHO worst-case scenario - Aerosol release of 50 kg Y. pestis over city of 5 million people (150,000 infected; 36,000 deaths) Modern Plague - Found everywhere expect Australia - Cannot be eradicated because y. pestis is widespread in wildlife rodent reservoirs - Approximately 1500 cases/year globally - 10-15 cases/year in U.S. Lecture 3: Antibiotics and Antibiotic Resistance Antimicrobial agents - Disinfectants: applied to inanimate objects - Antiseptics: sufficiently nontoxic to be applied to living tissues (hand sanitzers) - Antibiotics: produced by bacteria and fungi that are exploited by humans Alexander Fleming (1881-1955) - Discovered penicillin in 1928; produced from penicillium - Colonies of staphylococci couldn’t grow around a contaminating mold Antibiotics - Represent our most effective therapeutic agent against bacterial infections - Availability of antibiotics enables cancer chemotherapy, organ transplantation, invasive surgeries, and treatment of premature infants - Community: outside of healthcare areas and hospitals - Nosocomial: healthcare associated infections - 2 major problems - Diminished interest from pharmaceutical companies to develop new antibiotics - Drug companies don’t want to develop antibiotics due to “resistance” to get a new antibiotic, with clinical trials, formulations etc., is very expensive - Bacterial resistance to antibiotics always happens - 1930s was the golden era of antibiotics How do antibiotics work? - Antibiotics either kill bacteria or stop them from growing - For bacteriostatic antibiotics the immune system must eventually kill the bacteria - When bacteria develop a new resistance method, they tend to go global (spread around the world via human travel) Measuring antibiotic activity - Minimum inhibitory concentration (MIC)- Series of culture tubes with varying concentration of the agent - Check for visible growth - MIC = lowest concentration of agent that inhibits growth - Minimum inhibitory concentration (MIC) - Antibiotic strips - Faster, multiple antibiotics What do antibiotics target? - Antibiotics target essential bacterial components: cell wall synthesis, protein synthesis, DNA/RNA, folate synthesis, and alter the cell membrane - Targets are not present or are different in eukaryotic cells B lactam antibiotics – contains a B lactam ring Example: penicillin - Functions to inhibit cell wall synthesis in bacteria - B lactams bind the bacterial “penicillin-binding proteins” - PBPs are transpeptidases - No peptide cross links = weak cell wall = death - But some bacteria can produce a B lactamase - An enzyme that destroys the ring and thus the antibiotic - These bacteria are resistant to penicillin Example: Methicillin - Chemically modified penicillin - Can’t be cleaved by B lactamases - But some bacteria can produce a different PBP encoded by mec - This doesn’t bind methicillin or other B lactams - Penicillin can still kill the bacteria Bacteria cell wall synthesis - When the cell wall is being synthesized transpeptidase helps link and strengthen the cell wall - Methicillin makes sure B lactamase can’t destroy penicillin Vancomycin - A glycopeptide antibiotic - Inhibits cell wall synthesis in gram positives - Often a drug of last resort - Vancomycin binds the peptide linkage at terminal D-Ala-D-Ala residues and inhibits transpeptidation - Resistance genes change these to D-Ala-D-Lac and vancomycin can no longer bind - The van genes encode resistance Protein synthesis inhibitors - Many antibiotics target bacterial ribosomes and block translation - Function is to block translation Folic acid synthesis inhibitors - Ex. Trimethoprim and sulfonamides - Folic acid is a vitamin B9 for humans - Bacteria need folic acid for thymidine synthesis - But bacteria cannot absorb folic acid so they must synthesize their own- Inhibition of folic acid synthesis blocks DNA replication DNA/RNA synthesis inhibitors - Fluoroquinolones: interfere with DNA gyrase needed for supercoiling of DNA - Rifampicin: inhibits bacterial RNA polymerase Cell membrane alteration - Polymyxin B: used for Gram negatives - Bind to LPD - Hydrophobic tail inserts and disrupts outer and inner membranes Selection for antibiotic resistance - The more we use antibiotics, the more we select for resistant bacteria - If you put an antibiotic in, the few that were resistant to it by chance will undergo natural selection and produce only resistant bacteria The bacteria that are affected by the antibiotics may not be as fit Bacterial strategies for antibiotic resistance - Prevention of antibiotic entry: gram-negative outer membrane and mycobacteria cell wall - Antibiotic modification: B lactamase - Efflux of antibiotic: actively pump out the antibiotic - Alteration of antibiotic target: PBPs, Ribosome modifications - Bypassing the antibiotic action: using environmental folic acid - A lot of drug resistant mechanisms are genetically encoded by genes - Can pick up a gene and become resistant overnight Antibiotic resistance genes - Many mechanisms of antibiotic resistance are genetically encoded (e.g. mec, β lactamase, efflux pumps) - Can produce very high levels of antibiotic resistance - Often encoded on mobile genetic elements (e.g. plasmids) allowing for horizontal gene transfer "superbugs" - Acquired resistance to all the normal antibiotics - Bacteria get the genes from mobile genetic elements Horizontal gene transfer - Rather than alter gene function through mutations, new genes are acquired from another source - Transformation: the bacteria picks up free-floating DNA - There are some bacteria that have complex systems that can do this - Transduction: bacteria can become infected with viruses known as bacteriophages - Conjugation: there are plasmids and they form channels that allows the plasmids to move DNA - Everything in the end can be drug resistant Overuse/misuse of antibiotics? - Empiric use = when a physician would treat someone in a blind fashion - May not know what the bacteria is, but still give them some antibiotic - Ideal way is to see what the bacteria is resistant to and then treat it- Increased use of Broad spectrum agents = not specified for the specific bacteria (allows bacteria to gain general resistance more easily … which is bad) - Pediatric use for viral infections: if you give a kid an antibiotic for no reason… when it could have cleared up on its own - Patients who do not complete course: how long to take an antibiotic…. If you stop taking it after you “feel better” the bacteria may not be completely dead and can mutate and spread especially with chronic - Antibiotics in animal feeds = growth promoters – very bad The pathogen: Enterococci - Gram-positive cocci - Normal colonizers of the intestinal tracts in mammals - An important “nosocomial” pathogen known for drug resistance - 2 main pathogenic species - E. faecalis (more virulent but less drug resistant) - E. faecium (less virulent but more drug resistant) - Responsible for: - Urinary tract infections, surgical infections/wounds, endocarditis - VRE – vancomycin resistant enterococci - first reported in 1989 (E. faecium) – no longer just “colonizers” - VRE is now globally disseminated - Resistance due to the van genes The pathogen: Klebsiella pneumonia - Gram negative - An important cause of nosocomial pneumonia - Produces a capsule and is commonly resistant to multiple antibiotics - First documented source of "NDM-1" - New Delhi Metallo-beta-lactamase-1 also known as a carbapenemase - Carbapenems are -lactamase resistant β lactams with broad-spectrum activity - NDM-1 is now widespread in other Gram negatives = CRE (carbapenem resistant Enterobacteriaceae) Clostridia - Gram-positive, rod shaped, endospore-formers - Strict anaerobes, vegetative cells killed by oxygen - Generally found in soil and intestinal tracts of animals - Can be dominant for a really long time - Responsible for several unrelated diseases - >80 species - Important human pathogens - Clostridium difficile - pseudomembranous colitis - Clostridium tetani - tetanus - Clostridium botulinum - botulism - Clostridium perfringens – food-borne illness and gas gangrene - Can cause life-threatening diseases mediated by exotoxins The pathogen: Clostridium difficile - Can exist as- Asymptomatic carrier state in the large intestine - Cause of mild to moderate diarrhea - Cause of life-threatening pseudomembranous colitis - Often found in nursing homes and hospital environments - A nosocomial pathogen - Endospores can be very difficult to eradicate from the environment - Cultured from floor, bed pans, toilets, hands and clothing of medical personnel - Mode of transmission is through the spore: fecal-oral route - Cause of pseudomembranous colitis, also called antibiotic-associated diarrhea The disease: pseudomembranous colitis - Most symptomatic patients have recently received an antimicrobial agent - The most important risk factor - An inflammatory condition of the large intestine - Offensive smelling diarrhea, abdominal pain, fever, nausea, dehydration - Symptoms may occur 1-2 days after antibiotics or several weeks after the antibiotic is discontinued - Endoscopy can show characteristic yellow lesions - Antibiotics are used to cure infections, but they also kill the normal microbiota - After the antibiotic is stopped, spores germinate, overgrowth of C. difficile occurs with production of toxins - C. difficile does not itself invade, but the toxins damage the intestinal lining of the large intestine The pathogen: Clostridium difficile - Produces A-B toxins called the large clostridial cytotoxins - The A domain denotes the active portion of the toxin that carries the enzymatic activity - The B domain denotes the portion of the toxin molecule responsible for binding and uptake by the host cell - Will stick receptor on host cell - “A” domain functions to inactivate key regulatory proteins of host cells causes deregulation of multiple cell processes including cytoskeletal rearrangements, cell death and inflammation -The epithelial cells peel off Diagnosis and Treatment - History (antibiotic use), symptoms and laboratory tests to confirm C. difficile - Endoscopy and toxin detection assays - Discontinue inciting antibiotic if still being used - Fluids - Antibiotics more specific for “C. diff” – oral vancomycin or I.V. metronidazole - Avoid antidiarrheal agents – would cause decreased toxin clearance Fecal microbiota transplantation - FMT is the idea that you take someone else’s intestinal microbiota and transplant it into the patient that has the disease - Stopped the trial because it worked so well - After 1 infusion, 81% of the patients were cured Lecture 4: Mycobacteria – Tuberculosis and LeprosyMycobacteria - M. Tuberculosis - Causative agent of Tuberculosis in humans - Humans are the only known reservoir - Often called TB for tubercle bacilli - M. bovis - Causes tuberculosis in cows, rarely in humans - Humans can be infected by the consumption of unpasteurized milk leading to extrapulmonary tuberculosis - M. avium - Can cause a tuberculosis-like illness in humans, particularly in AIDS patients - M. leprae - Causative agent of Leprosy in humans Disease of poverty - TB infects 1/3 of the world total population right now - TB is contagious and is airborne The pathogen: Mycobacterium tuberculosis - An obligate human pathogen - An intercellular pathogen (lives within macrophages) - Slow generation time of >15 hours - Mycobacteria have an unusual cell envelope with high concentration of mycolic acid waxy - This unusual envelope is associated with resistance to - Many antibiotics - Killing by acidic and alkaline compounds - Osmotic lysis via complement deposition - Lethal oxidative stress promoting survival inside of macrophages - Impermeability to stains and dyes because the cell envelope is very hydrophobic - Gram-positive acid-fast stain - Acid-fast stain - Stained with carbol-fuchsin dye with slow heating (to melt the wax) - Red stain - Washed with EtOH and HCl - Counter stained with methylene blue - Acid-fast organisms appear red whereas non-acid fast organisms appear blue Spread and Progression of tuberculosis - Stage 1: Transmission - Transmission is from inhalation of droplets from an infected host, usually by coughing or sneezing - Small diameter droplets can stay airborne for extended periods of time - Stage 2: spread - Begins 7-21 days after initial exposure - Phagocytosis of TB cells by lung (alveolar) macrophages - TB inhibits the fusion of the lysosome on the phagosome and can multiply in macrophages - Macrophages will lyse and release TB cells to infect more macrophages - A key virulence property M. tuberculosis is the ability to survive within the host macrophage- Stage 3 - Infected macrophages can form granulomas - TB granulomas are tubercles of immune cells that try to destroy invading pathogens (typically formed by macrophages) - The granuloma represents a balance between the pathogen and the host latent infection - Granuloma: something the system is trying to get rid of but it can’t - TB sits in the granuloma and doesn’t spread but it is not killed either - There are macrophages in the middle of the granuloma that aren’t interacting with T cells causing the bacteria to grow - T cell activated macrophages can kill TB - Activated T cells can secrete cytokines (INF-gamma) to activate the macrophages - Macrophages at the center of the granuloma remain harder to activate by T cells - Chronic inflammation cause “cheese-like” necrosis caseous necrosis - Stage 4 - Some macrophages remain inactivated and infected - The tubercle grows - Erosion of the granuloma into the airway provides the route of transmission - Bacterium is released - Denaturation of the host immunity can result in life threatening infection active tuberculosis - Can be due to a lack of food or old age - The caseous center can liquefy leading to cavitation (when the granuloma explodes because it is very big) - The very large granuloma will explode Tuberculosis - 75% of active tuberculosis is pulmonary - Progressive, irreversible lung destruction can occur, and the bacteria may enter the bloodstream It is thought that a single inhaled bacterium can infect - 25% of active tuberculosis is extra pulmonary - More likely to occur in immunocompromised people - Can infect: bone, joints, liver, spleen, GI tract, and brain - Systemic spread, called miliary tuberculosis, is almost always fatal - When the organism has escaped the lungs and it continues to infect the rest of the body - Only about 10% of TB infected people develop active disease - Symptoms often non-specific - A prolonged (> 2 weeks) cough with thick and possibly blood in mucus - Fever, chills, night sweats - Fatigue and weakness - Chest pain and shortness of breath - Loss of appetite and weight loss “consumption” - Pallor, meaning pastiness or pale skin “the white death” - Extra pulmonary TB can vary widely depending on where TB has spread Testing and diagnosis - Tuberculin test (PPD = purified protein derivative from M. tuberculosis) - Injecting this in - A positive result is a red and swollen circle at 48h- A person is considered infected if they convert from negative to positive on a TB skin test - A negative result could mean: latent or active TB, BCG vaccine, or previously infected - A positive test would likely mean a careful history check and chest x-ray - X-ray: typical upper lobe “shadowing” = lesions - Calcified granulomas may be seen on an X-ray - Staining of sputum for acid fast bacilli and culturing - More complex immunological techniques - Usually when people get infections, it is in their upper lungs -TB is an aerobic organism and it’s usually in the upper area of the lung because it wants oxygen - The lower part of the lung doesn’t always get oxygen because that would require deep breaths that we don’t always do Treatment - Active TB will kill 2 out of 3 people if untreated - Six months of antibiotics for the short treatment - Slow growth means long treatments - Generally multiple types of antibiotics are used - Rifampin (inhibits RNA polymerase) - Isoniazid (inhibits mycolic acid synthesis) Drug resistant TB - Multi-drug resistant TB (MDR-TB) - Defined as being resistant to the two most effective first-line therapeutic drugs, isoniazid and rifampin - Extensively-drug resistant TB (XDR-TB) - Also resistant to the most effective second-line therapeutic drugs used commonly to treat MDR-TB - XDR-TB has been found in all regions of the world - These strains can be virtually untreatable BCG - “Bacille Calmette-Guérin” - A living vaccine prepared from attenuated M. bovis - BCG shares antigenicity with TB - Controversial due to variable efficacy (~80% or much less) for pulmonary TB - Effective against miliary TB - Vaccinated people can give a false positive for the tuberculin test - Vaccination leaves large scars - Recommended for people with high risk to exposure - Lab stain loses a lot of its virulence properties - Because it is a live vaccine and it is used across the world, they might not be the same strain - Some will be more aggressive than others; people believe that it does not work Tuberculosis and HIV/AIDS - Individuals infected with HIV are ~30-times more likely to develop tuberculosis - At least one third of the persons living with HIV infection are co-infected with TB - TB is a leading killer of HIV-positive people causing one fourth of all HIV-related deaths -The HIV virus goes after the T cells and these cells are needed for TB- People with HIV are more susceptible to TB because they lack T cells - Once granuloma is present, your immune system doesn’t have a chance to get rid of the bacteria on its own - You’re considered infected with TB when it’s in your macrophages and it doesn’t go away The disease: Leprosy - A chronic disease caused by Mycobacterium leprae - Also called Hansen’s disease - Very slow progression – incubation period of ~5 years - Can cause permanent damage to skin, nerves, limbs, and eyes - Very rare in developed countries - ~ 2 million people are permanently disabled by leprosy, mainly in tropical developing countries (this may be a low estimate) - Lesions in tuberculosis are “hidden” - Lesions in leprosy are “visible” - BUT, leprosy is much less infectious that TB - It is very unlikely that you will get leprosy if you come in contact with a person who has the disease The pathogen: Mycobacterium leprae - M. leprae shares some features with M. tuberculosis - “Gram positive” acid fast, rod shaped, aerobic, waxy cell envelope (mycolic acid) - Cannot be cultivated in vitro (less well-studied than M. tuberculosis) - Can grow in the foot pads of mice (low numbers) - Causes systemic infection in the armadillo (1010 organisms per gram of infected tissue) - M. leprae infects macrophages of skin and Schwann cells in nerves The disease: leprosy - Two major forms: Tuberculoid and Lepromatous - Most people that are exposed to mycobacteria will be immune to it and will not develop any disease - Better immunity and better cell mediated immune response - People that are exposed to it will just kill the organism resulting in no problem - Tuberculoid is a mild case of leprosy - Lepromatous is the serious form - Small subset of people that this infects Tuberculoid leprosy - Cell-mediated immunity present - Macrophage can contain the bacteria - Light colored lesions with anesthetic areas - Loss of touch sensation - Sometimes loss of hair and pigmentation - Patients become tuberculin positive (activate T cell-mediated responses) - Bacterial cells are generally not recoverable from lesions - Tuberculoid leprosy can be self-limiting - Most infections are self-limiting: you are able to clear the virus Lepromatous leprosy- Cell-mediated immune responses are absent - Macrophages are not activated - M. leprae survives and multiplies in macrophages and Schwann cells - Schwann cells provide myelin insulation to peripheral nerves -Schwann cells are cells that surround peripheral nerves and they provide insulation so that action potential can travel down - Due to nerve damage and loss of sensation leads to inadvertent traumatic lesions on the face and extremities - Can cause loss of eyebrows, thickening and enlarged nares, ears and cheeks “lion like” appearance - Lesions can become secondarily infected, eventually resulting in bone resorption, disfigurements and mutilation Spread and progression of leprosy - Transmission is not well understood - Probably close (direct) contact for extended periods of time – inhaled droplets? - Most exposed individuals do not develop disease – host genetics likely plays an important role Treatment - Leprosy is highly treatable with antibiotics - Multiple drugs are used (6 months to 1 year) - Dapsone (1940s) – resistance developed in 1960s - Multidrug therapy (MDT) (1980s) – dapsone, rifampin, clofazimine - Patients no longer transmit the disease after one dose of MDT - Can be eradicated if the incidence is low enough Lecture 5: Bacterial Meningitis - Problem with meningococcal disease is that it occurs in outbreaks, and the first person that has it doesn’t know they have it making them more in danger Meninges - The membranes that envelope the central nervous system (brain and spinal cord) - Three layers of the meninges going from dura mater, arachnoid mater and pia mater going from outside in - Cerebral spinal fluid is between the arachnoid and pia mater - Exists as a cushion for your brain - Arachnoid mater functions as a shock absorber Meningitis - An infection of the meninges - Meningitis is usually due to viral or bacterial infection - Bacterial meningitis can be rapid and life threatening - Viral meningitis is generally less severe and usually resolves without specific treatment The Blood Brain Barrier - A protective cellular structure that restricts passage of chemicals, toxins, and microorganisms from the blood to the CNS and also protects your CNS from the peripheral immune system - The cells that surround the blood are like the skin- The white blood cells are not found in the central nervous system normally - BBB is specialized cells within your blood vessels that make a tight layer - Endothelial cells are stitched together by structures called "tight junctions" - Astrocytes and pericytes provide support for other cells of the CNS including the BBB - Microglia cells are the "tissue macrophages" of the CNS - T cells, b cells, NK cells, monocytes, neutrophils aren’t found in CNS because they can’t get across BBB The disease: bacterial meningitis 1. Nasopharyngeal colonization 2. Invasion into blood 3. Multiplication in blood 4. Crossing of the blood brain barrier (BBB) 5. Invasion of the meninges 6. Production of proimfammatory cytokines/chemokines 7. Recruitment of leukocytes into CNS 8. Edema, increased cranial pressure 9. Inflammation 10. Neuronal damage - You have an organism that is colonizing - Usually nasopharyngeal - At some point they can invade epithelial and get into blood system - They are capable of multiplying in the blood - They have mechanisms that prevent the killing of them in the blood - Cross BBB and invade into meninges (in CNS) -CNS can probably kill a few cells but can’t kill a lot - Proinflammatory, which makes cytokines/chemokines that call leukocytes to get into meninges - This causes more inflammation, more cells in the CNS - This causes a lot of swelling that results in neural damage Traversing the BBB - Transcellular traversal mechanism - Invades into endothelial cells and goes out the other side - Most of the major meningitis pathogens do this - Pericellular traversal mechanism - Bacteria push themselves through the junctions - Example: Lyme disease - Trojan-horse mechanism - Bacteria have an intercellular life cycle that causes a leukocyte to bring it into the cell - Example: macrophage bringing the bacteria into the cell The disease: bacterial meningitis - A very rare but very dangerous disease that can kill in days - Early signs may be non-specific - In an outbreak, the first people to develop disease are the most likely to die - If an outbreak is known to be occurring, people are more wary of initial symptoms - Mortality rate has remained high (10-25%) - Survivors may have irreversible damage - Brain damage, blindness, hearing loss, and learning disabilitiesClinical symptoms in children and adults - High fever, severe headache, stiff neck, confusion, vomiting or nausea, seizures, sleepiness or difficulty waking up, photophobia, sensitivity to light, and skin rash in cases of meningococcal meningitis Clinical symptoms in infants - Can be subtle, variable, and non-specific - Fever, constant crying, excessive sleepiness or irritability, poor feeding, inability to maintain eye contact, a bulge in the soft spot on top of a baby's head (fontanel), stiffness in the baby's body and neck, and skin rash in cases of meningococcal meningitis Risk factors - Lack of vaccination - Young age (infants) - Living in a community setting - Immunocompromised individuals due to disease or chemotherapy - Cranial surgery Diagnosis - History and symptoms - Blood tests for inflammatory markers, culture - Lumbar puncture (spinal tap) - Lumbar puncture is major diagnosis treatment - Stick needle into spinal chord and take out cerebral spinal fluid - If its cloudy it means things are growing it - Gram staining the CSF gives a lot of information very early on as to what bacteria is there - Presence of white cells like neutrophils meaning that there are neutrophils that have gone through and t cells indicate virus -Low glucose levels in CSF which indicates either hyperglycemia or bacterial/ viral infections like meningitis or TB - Imaging (CT or MRI) - Organism can get cultures if it’s in blood system Physical signs - Nucal rigidity: inability to flex the head forward - Brudzinski’s sign: severe neck stiffness causes a patient’s knees to flex when the neck is flexed - Kernig’s sign: severe stiffness of the hamstrings causes an inability to straighten the leg when the hip is flexed to 90 degrees - If these signs are absent it does not mean much, but if they are present, it means the person has the disease Treatment - Must be sought immediately - Intravenous antibiotics (prior to culture analysis) - Is very complex - They would do this blind by using their knowledge - Corticosteroids (dexamethasone) to reduce swelling in the meninges- Supportive therapies The disease: bacterial meningitis - Almost all known bacterial pathogens have the potential to cause meningitis, but relatively few account for most cases - Major causes of bacterial meningitis - Neisseria meningitidis - Streptococcus pneumoniae - (Haemophilus influenzae) - Listeria monocytogenes - In infants (0 - 2 months): - Streptococcus agalactiae (Group B Streptococcus) - Escherichia coli K1 - These diverse pathogens (except Listeria) produce a capsule as a major virulence factor Capsule - A loose, relatively unstructured network of polymers that cover the surface of some bacteria - Most are composed of polysaccharides - Main role in meningitis is to protect bacteria from the complement system - Complement: innate immune system serum proteins like C3b - Encapsulated bacteria are less likely to be opsonized by the complement system - More likely to survive in the blood - Capsule blocks the complement system from binding to C3b preventing the bacteria from being opsonized Capsules as vaccines - An effective host response against capsules is the generation of antibodies from B cells that can recognize the capsule - Antibodies that recognize the capsule promote opsonization and phagocytosis - Capsules can therefore be used as antibitoics - Problem is bacterial capsules are made of polysaccharides which means that the capsules are t cell independent pathogens - T cells don’t respond to sugar, they only respond to peptides - As a result of this you don’t get isotype switching and memory responses - You can vaccinate people but it’d be a short term, non-memory response - Polysaccharide vaccines do not provide long-term memory because they are T cell-independent - Conjugate vaccine: polysaccharide conjugated to protein carrier - This vaccine will be T cell-dependent - This tricks the immune system by allowing the B cell to bring T cells in as a result of the protein on the sugar The pathogen Neisseria meningitidis - "meningococcus" - Gram-negative, diplococcus - A human specific pathogen - Colonizes the nose and throat – asymptomatic carriage is common - Produces a polysaccharide capsule - Antigenic variants (i.e. serotypes)- A, B, C, W135 and Y - A leading cause of bacterial meningitis and also meningococcemia - termed invasive meningococcal disease - This infection is highly contagious and may cause local epidemics in college dormitories, boarding schools and on military bases - The antibodies that recognize 1 capsule will not be able to recognize the other capsules - Different strains can produce different capsules - Antigenically different so they make different sugars Meningococcal disease - Meningitis occurs after bacteria enter the bloodstream and cross the BBB - Endotoxin (LPS) can lead to septic shock - Disseminated intravascular coagulation - Widespread blood clotting - Ischemia (loss of blood flow) - Clotting factors are used up which leads to small skin bleeds purpuric rash - Rash does not fade under pressure ("glass test”) - Cytokine driven type response - Organisms have high amounts in blood - They have LPS, which can cause septic shock - If you push a glass on the rash, the rash would stay there verses the normal rash where you can force blood out - Get clots forming in small vessels - As clot gets thicker and thicker, there will be no blood being passed through - It’s the using up of all the clotting factors that causes bleeds in other places Vaccines for Neisseria meningitidis - Menactra (Sanofi Pasteur)/Menveo (Novartis) – quadrivalent conjugate capsule vaccine from 4 serotypes of meningococcus (serogroup A, C, Y, W-135) - Serogroup B most common for invasive disease in Canada but the capsule is poorly immunogenic - Serogroup B is poorly immunogenic and not used in the combination of serogroups in the conjugate capsule vaccinations - Can mimic host tissue - Some people have tried to make vaccinations with this but it got complicated - No capsule vaccination used for serogroup b - Bexsero (Novartis) – contains 4 recombinant protein antigens – now licensed (as of 2014) for use in Canada The African Meningitis Belt - The highest burden of the disease in the world - Mostly caused serogroup A - Herd immunity wipes this thing out The pathogen: Streptococcus pneumoniae - "Pneumococcus" - Gram-positive cocci, grows in chains - Commonly resides asymptomatically in the nasopharynx - Causes pneumonia, ear infections, sinusitis and many other diseases- The leading cause of bacterial meningitis in infants and young children - Produces a polysaccharide capsule - Many different serotypes exist - A major global pathogen with > 700,000 deaths per year globally Vaccine for Streptococcus pneumonaie - A pneumococcal vaccine has been licensed for use in Canada for children - Prevnar 13 (Pfizer) - A capsule vaccine from the 13 most prevalent serotypes of pneumococcus - Use of the vaccine is associated with decreasing rates of invasive pneumococcal disease in Canada and elsewhere - They are going to have to put more serotypes into the vaccine - Have thirteen serotypes because there is a race to have the most common capsules in the vaccines to prevent the ones that aren’t in the combination from becoming resistant The pathogen: Haemophilus influenza type b - "Hib" - Gram negative, coccobacillus, produces a polysaccharide capsule - Primarily causes meningitis in children under 5 - When it occurs, it tends to follow an upper respiratory infection, ear infection or sinusitis - Bib conjugate vaccine available as part of the routine childhood immunization schedules has reduced 99% of invasive Hib disease to low levels (<1 per 100,000) - Before the 1990s, H. influenzae type b (Hib) was the leading cause of bacterial meningitis The pathogen: Listeria monocytogenes - Gram-positive rod shaped - Not you typical meningitis pathogen - A foodborne pathogen - Listeriosis can range from gastroenteritis bacteremia meningitis - High rates of mortality in immunocompromised individuals including neonates and the fetus - Able to grow at 4°C (a psychrotroph) – important for a food-borne pathogen (soft cheeses often implicated) - If the milk used to make the cheese has not been pasteurized, it can contain the pathogen - Listeria invades intestinal epithelial cells and replicates within the cytosol (actin-based motility and cellto-cell spread) - Listeria causes ~ 11% of meningitis cases - Not flagella - This is the one that is associated with pregnant women who aren’t supposed to eat stinky cheeses because listeria will be in those foods and this is very dangerous for the unborn fetus - Psychrotroph is cold tolerant and grow at refrigerator - Listeria is ingested and it invades intestinal epithelial cells and replicates in cytosol - Pushes from one host cell to another cell - Listeria gets into host cells into phagosome - Makes membrane active compounds - Has neat protein that polymerizes the host actin in the cell - Not flagella- Allows the pushing of the cell around - The listeria can eventually push into another cell even by hiding itself from your immune system - Can infect blood and then cross the placenta to infect the fetus The pathogen: Streptococcus agalactiae - "Group B Streptococcus" GBS - Gram positive cocci, grows in chains - Produces a capsule - Many women carry S. agalactiae in the urogenital tract - GBS can be passed from the mother to infant during labour - Women are usually tested for GBS at ~36 weeks - Women who are positive may be treated with antibiotics during labour to prevent infection of the newborn - Group B can be passed to the infant The pathogen: Escherichia coli K1 - E. coli expressing the K1 antigen (capsule) is a leading cause of infant meningitis Lecture 6: Staphylococci Staphylococci - "Staphyle" – Greek for Bunch of Grapes - Gram-positive, coccus shaped - Coagulase Positive Staphylococci - Staphylococcus aureus - "Aureus" = Latin for gold - Coagulase Negative Staphylococci - Staphylococcus epidermidis - Staphylococcus saprophyticus - Many other coagulase negative species - Important causes of biofilm-associated infections - When the cells divide, they divide in all planes this is why they look like grapes The pathogen: Staphylococcus epidermidis - Coagulase negative - Not as dangerous as S. aureus -A great skin colonizer - Resistant to a number of antibiotics - Produces a capsule (surface polysaccharide) - S. epidermidis is known for forming biofilms - Major problem for implanted devices - Indwelling catheters and medical prostheses - Coagulase positive - An effective colonizer of humans that doesn’t usually cause problems - Anterior nares (nostril) and skin- If we swabbed everyone's nostrils in the class, there are a third that carry it all the time, a third carry it intermittently, and a third never carry it - No reason why some people carry it why some people don’t - Carriers are usually healthy - Carriers of S. aureus are healthy, asymptomatic people - Colonization leads to greater risk of infection, but prognosis is also generally better - If you get an infection, your prognosis is probably going to better than someone who doesn’t carry it around - This is because you develop immunity to it (surface factors, virulence factors) Colonization - Skin and mucous membranes, nose (~30% of people are persistently colonized) - Spread person-person by direct or indirect contact - Fomites (inanimate objects capable of transmitting an infectious disease) e.g. towels, razors, bandages - Resistant to high salt (skin) - S. aureus surface proteins bind host proteins using adhesions (e.g. fibronectin, collagen and elastin binding proteins) - 30% will sometimes carry it, and another 30% will never carry it The pathogen: Staphylococcus aureus - A leading cause of hospital-acquired (nosocomial) infections - Generally an extracellular pathogen - A “pyogenic” or pus-producing infection - The "Hallmark" of S. aureus infection is the abscess - Heat, redness, swelling, and pain - A collection of dead neutrophils (pus) due to infection - Abscesses can occur in any organ but are most frequent on the skin - Can cause major complications if the organisms spread from the abscess - Abscesses don't typically heal on their own – require drainage and maybe antibiotics - Capable of causing a very wide range of infections - An escape organism because it develops resistance against antibiotics very easily - Has many virulence factors Staphylococcus aureus virulence factors - Expression of virulence factors is regulated - Surface virulence factors expressed during exponential growth - Secreted virulence factors (Exotoxins) expressed during stationary phase - Generally, surface virulence factors are for colonization purposes, while secreted virulence factors are for invasion and spread - Expresses surface proteins during exponential growth - Will adhere to tissues - Secreted ones mostly doing damage Immune evasion mechanisms - Resistant to antibody mediated phagocytosis- Protein A - S. aureus surface protein - Binds the Fc portion of IgG upside down - Antibodies are bound in the incorrect orientation to be recognized by phagocyte Fcreceptor - Toxins that kills leukocytes - S. aureus can make a number of cytolytic toxins that kill white blood cells - Often called “hemolysins” because they can lyse red blood cells - Actual targets are mostly white blood cells - E.g. a-toxin and leukocidins - Helps to protect S. aureus in abscesses and for spreading Diseases due to direct effect of organism - Skin lesions, deep abscesses, and systemic infections Skin lesions - Impetigo – superficial skin infection usually in young children - The non-bullous form has pimple-like lesions with pus (also caused by strep pyogens) - The bullous form has painless, fluid filled blisters - Only staph casues this - Stye – infection of the eye sebaceous glands - Often will drain on its own, warm compress - Do not lance - Furuncle (boil) - Infection of hair follicle - Warm compress to drain - Carbuncles (infection of several hair follicles) - Coalescing furuncles Deep abscesses - Not superficial but still localized – has a "focus" of infection - E.g. cellulitis, liver, lung, kidney, tooth etc. - Wound or surgical infections - Symptoms may not be obvious and may be more "constitutional" (whole body) e.g. fever, chills, malaise etc. - Deep abscesses can become systemicSystemic infections - Often no single "focus" of infection - E.g. bacteremia/septicemia, pneumonia, osteomyelitis, endocarditis - Very dangerous, often difficult to treat - Osteomyelitis - Infection of bone or bone marrow - S. aureus is the most common cause - Can come from: - Hematogenous spread (blood stream) or local infection (cellulitis) - Fractures - Joint replacement - Can be very difficult to treat and may require open surgery, i.v. Antibiotics - Infective Endocarditis - Infection of the heart valves - Typically occurs on damaged or prosthetic heart valves and with i.v. drug users - The lesion is called the "vegetation" - Bacteria can grow to large numbers and "seed" causing strokes and pulmonary embolisms - Fatigue, fever, heart murmurs, splinter hemorrhages - ~25% are S. aureus but can be aggressive - Everyone will die from the disease if there are no antibiotics Toxic mediated diseases - Infection often localizes, but effects are systemic - E.g. toxic shock syndrome, staphylococcal scalded skin syndrome, and food poisoning Toxic Shock Syndrome TSS - First formally described as a systemic illness in 7 children associated with non-invasive staphylococcus aureus infection - Acute onset of fever, hypertension, rash, multiple-organ dysfunction, desquamation - Caused by both Staphylococcus aureus and Streptococcus pyogenes - Staphylococcal TSS has menstrual and non-menstrual forms (<5% mortality) - Streptococcal TSS occurs in association with invasive streptococcal disease ('flesh-eating' disease) (>40% mortality) - Hypotension: low blood pressure resulting in shock Menstrual TSS - High absorbency tampons were identified as a major risk factor and were withdrawn from the market - Bacteria changed their response to the environment and started making toxic versions - Skin peeling off desquamation TSS - Caused by superantigens (Secreted toxins) - Function to over activate large numbers of T cells and cause a systemic inflammatory response - Produces a cytokine storm - Eventually results in vascular leakage leading to shock and organ failure - TSS toxin-1 is responsible for the menstrual form - Staphylococcal enterotoxins are also called superantigensStaphylococcal scalded skin syndrome - Caused by exfolitative toxin (specific proteases) - Proteases that destroy host proteins that hold cells together in the superficial layers of the skin - Primarily affects neonates (newborn less than 4 weeks old) - Causes skin peeling, but the mucus membrane does not shed - Heals in 1-2 weeks Staphylococcal foodborne illness - Staphylococcal enterotoxins cause staph food poisoning – proteins also function as Superantigens - The toxin is performed in food – does not require the ingestion of viable staphylococci - 1 ug is sufficient to induce projectile vomiting - Mechanism remains uncharacterized Methicillin-resistant Staphylococcus aureus - MRSA is a superbug - Resistance to multiple antibiotics and B lactam antibiotics - Early penicillin resistance due to S. aureus B-lactams - Methicillin is a modified penicillin that is insensitive to B-lactams - Methicillin resistance encoded by the “mec” region - encodes a “penicillin binding protein” called PBP2a - B-lactam antibiotics bind “Normal” PBP, but these antibiotics can’t bind PBP2a - Typically associated with hospitals - Patients generally have co-morbidity - CA-MRSA strains – lack of exposure to health care setting - CA-MRSA are hypervirulent, but still susceptible to a number of other antibiotics - May cause necrotizing pneumonia - Most common cause of skin and soft tissue infections Lecture 7: Lyme disease Lyme Disease (Lyme Borreliosis) - A prototype emerging infectious disease - A multisystemic disorder - Commonly presents as skin lesion (erythema migrans) - If untreated, can lead to arthritis, carditis, and nervous system manifestations - Most common vector-borne disease in North America - Vector borne transmitted by something else - Can sometimes cause a bulls eye rash - First recognized in 1975 in rural communities surrounding Lyme, Connecticut - Epidemic of polyarthritis, mostly in children - Most were misdiagnosed with rheumatoid arthritis - Rheumatoid arthritis isn’t an epidemic because it is autoimmune - Many were noted to have a bulls eye rash prior to development of symptoms - Rash was associated with a tick bite - A 'spirochete' was isolated from the ticks, and subsequently from skin, blood and cerebral spinal fluid of patients Borrelia burgdorferi Borrelia burgdorferi- Gram-negative spirochete - Thin (~0.5 µm) and long (>10 µm), spiral shaped - Lyme Borrelia are widely found throughout temperate zones in the Northern hemisphere - B. burgdorferi is the major cause in North America - Other species can cause Lyme Disease – collectively called B. burgdorferi sensu lato - B. burgdorferi are spread by the bite of ‘hard’ ticks (Ixodes species) = vector borne disease Reservoir for Borrelia birgdorferi - Transmitted to different mammalian hosts through ticks - Is only found in their vertebrate or arthropod hosts - White footed mice are the major reservoir - Called a deer tick ticks will bite deer but deer are not the reservoir, mouse are - Mice are infected and larva come around and larva come around and get a blood meal - Tick has a blood meal can molt from a larva into a nymph - It then takes another blood meal, which will infect an animal Ixodes Tick (black legged or deer tick) - Hard bodied ticks - In North America, B. burgdorferi is transmitted primarily by lxodes scapularis and lxodes pacifica - Other species transmit in Europe and Asia Lxodes life cycle - 3 stages: larva nymph adult - Ticks require blood meals between stages - No adult to egg transmission – ticks must acquire B. burgdorferi - Mice, squirrels, and birds carry this - Majority of human infections come from nymphs - Disease doesn’t start fro the larvae because there is no transmission form the adult to the egg - They need to be infected from a mouse, they aren’t born with it - Nymphs are the ones that most likely transmit the disease -The nymphs are so much smaller so they are harder to see -Adults can transmit but nymphs are harder to see Lyme disease transmission - Ticks do not fly or jump - Ticks sit on grasses/shrubs and wait for a host to pass by - Bites often occur in hard to see areas - Dogs and cats can get lyme disease - No evidence of direct person to person transmission - Move to hard to see areas that are moist like armpits, back of knees, and hairlines - Need the vector to get in - Ticks insert a feeding tube with barbs that secretes a local anesthetic - Transmission is not thought to occur during the first 24 hr. following a bite - Transmission increases >24 hours - Nymphs normally transmit the disease - Ticks suck blood slowly for several days - Ticks appear grey when engorgedTick removal - Use fine tipped tweezers - Grasp the tick as close to the skin as possible - Steadily pull upwards - Thoroughly wash the area and keep the tick - Do not squish the tick body - Do not burn the tick off - Do not apply petroleum jelly - Can submit the tick for testing - Grasp the tick as close to the barb as possible The pathogen: Borrelia burgdorferi - Following initial infection, B. burgdorferi must cause disseminated and persistent infection to propagate through its life cycle - Hematogenous dissemination is a central event in the development of Lyme Borreliosis - For the tick to transmit the disease, it needs to pick up new organisms in the blood - Needs to become a systemic organism to continue its life cycles - You don’t get a rash all the time - At some point, the bacteria can spread from your skin to your blood vessels where they’ll spread - They need to then get out of the blood and get into tissue - Compounds in tick saliva are thought to inhibit DC function on multiple levels - Decreased phagocytosis - Decreased maturation - Decreased inflammatory mediators - Decreased antigen presentation - The pathogen contains periplasmic flagella called axial filaments - Flagella is in the periplasmic space since these bacteria are gram-negative - Axial filaments wrap around cells to produce cork-screw shapes - Rotation of the axial filament causes the bacteria to move in a corkscrew like manner - Promotes movement through extracellular matrix of host tissue and invasion of vasculature - Contain an unusual outer membrane - No LPS - Many surface expressed lipoproteins that can act as adhesions - Escape from the vasculature requires adhesion to sloe down the pathogen - Repetitive mobility is required to invade the endothelium - When is pops out of the vasculature it is disseminated - Flagella is very important for this to important - Has an unusual genetic structure - Linear chromosome - Multiple plasmids – some linear and some circular - Plasmids are required for infection but are variable from strain to strain - Limited metabolic capability so it needs to live inside of a host Early localized stage - Most common symptom is erythema migrans – 'Bulls-eye rash' (~25% of patients do not have a rash) - Occurs ~1-2 weeks after tick bite - Groin, axilla, waist, back, legs, (head and neck in children) - Rash will expand and if untreated can reach >12 inches diameter- Flu-like symptoms including fever, chills, fatigue, body aches Early disseminated stage (days to weeks) - Occurs in untreated patients - Multiple rashes would indicate dissemination of B. burgdorferi - Pain and swelling of large joints - Heart palpitations – interference with heart electrical signals - Meningitis – severe headaches and neck stiffness - Bell's (facial) palsy – loss of muscle tone on one or both sides of the face Traversing the BBB - Lyme disease gets through the BBB through the paracellular traversal mechanism Late Disseminated Stage (months to years) - Can cause serious long-term disability - Response to antibiotics takes longer - Muscle pain - Arthritis - Severe pain and swelling in large joints - ~5% of patients can develop neurological problems - Shooting pains - Numbness - Tingling in hands and feet - Memory Post-treatment Lyme disease syndrome - 10-20% experience symptoms following treatment with antibiotics - Cause is unknown - Lingering symptoms including - Fatigue, muscle and joint pain, cognitive defects, sleep disturbances - May involve an autoimmune response or possibly persistent infection - Most patients recover after a number of months - Long-term antibiotics are not thought to help - People in medical biology don’t think it’s a persistent infection so there is no point of ling-term antibiotics Lyme disease in Canada? - Ticks will latch onto birds and move north - The warmer climate causes a less harsh winter allowing them to continue their life cycle without dying - Reported numbers for the disease are massively underestimated Prevention - Avoid wooded areas endemic with Lyme disease - Stay on paths, avoid low lying brush and long grass - Wear long pants and long-sleeved shirts - Light coloured clothing - So you can spot the ticks and remove them - Repellants containing DEET- Check for ticks and remove them Diagnosis - Erythema migrans and other 'typical' symptoms - Tick bite or reason to suspect tick exposure - Anti-B. burgdorferi antibody tests (no 'Gold-standard') - Detect antibodies to a laboratory strain of B. burgdorferi - False negatives often due to early testing (no antibody response yet) and genetic diversity of B. burgdorferi - Sensitivity is somewhat controversial not that good - Antibody tests are controversial because tests are based on lab strain so if you’ve had clinical strain you might get false negatives - Submission of tick for testing (if you have it) to the National Microbiology Laboratory Treatment - If bitten by a black-legged tick, watch for a rash (30 days) and be aware of symptoms - Patients when diagnosed early will recover following antibiotic treatment - 2 - 4 week course of an antibiotic - Without treatment can lead to joint, heart, and nervous system problems - ~10-20% of patients, typically with a late diagnosis, have post-treatment Lyme disease syndrome Chronic Lyme disease - Very controversial - Some think this is due to chronic infection by B, burgdorferi - Can be diagnosed without evidence of prior lyme disease - Persistent symptoms include: fatigue, headaches, sleep disturbances, cognitive dysfunction and other neurological problems - Long-term antimicrobial therapy is not helpful – demonstrated by 4 clinical trials - Controversial as to if chronic lyme disease to exist or not - Medical establishment don’t believe that this has happened One of the big problems is that you can be diagnosed with it without being diagnosed with it - The fact that the antimicrobial therapy didn’t help is the best evidence that it doesn’t exist - Most common in children (5-9 years old), and in women - Case definition may have been too narrow - Many symptoms in "chronic Lyme disease" not properly recognized - Commercial tests probably not sensitive enough for B. burgdorferi - Treatment may be too restrictive, too short Lyme Disease Vaccine? - LYMErix – based on an outer membrane protein - Human trial (11,000 adults) showed it to be 75% effective - ‘Should be considered’ for those in high risk areas (not ’recommended’) - Claims (and lawsuits) that the vaccine caused arthritis – no evidence - Pulled from the market in 2002 due to ‘lack of demand’ – only now approved for dogs - Some people that got the vaccine got arthritis but the same number of people with the placebo got arthritis too Lecture 8: StreptococciStreptococci - Gram-positive, Coccus shaped, grows in chains - Non-motile, non-endospore forming - Initially classified by their pattern of hemolysis on blood agar - Step grows in chains where as staph grows in clusters - Alpha-hemolytic - S. pneumoniae (pneumococcus) - viridans group including: - S. viridans - endocarditis - S. mutans – tooth decay - S. thermophilus – dairy foods - Beta-hemolytic -S. pyogenes (Group A Streptococcus) - S. agalactiae (Group B Streptococcus) - S. equi (Group C Streptococcus) - Gamma-hemolytic - Enterococcus species (Group D Streptococcus) - Lactococcus lactis (Group N Streptococcus) - "Lancefield Classification" - Classified on the basis of surface carbohydrate antigens The pathogen: Steptococcus pyogens - A common human specific pathogen - An extracellular pathogen - Pyo = pus - Historically a major cause of mortality due to scarlet fever, puerperal sepsis, and wound infections in soldiers - Today a common cause of pharyngitis and impetigo - Also causes severe invasive streptococcal disease and the streptococcal toxic shock syndrome ("flesheating” disease) - An important cause of "post infection sequelae" including acute rheumatic fever - When you develop a disease even when the bacteria is gone - In general its life cycle is extracellular causes a lot of inflammation -Usually younger kids carry it in asymptomatically -These group of kids can carry the organism in their throat for over two years without symptoms -This shows that asymptomatic carriage is the bacteria’s preferred place - Flesh eating infection can allow you to go head to head with Ebola -Can be autoimmune diseases that is initiated by the bacteria -Very strong neutrophil response leads to the formation of pus - Produces an arsenal of virulence factors - A master at hiding from the immune system - Armed to cause severe damage - The virulence factors can be used to hide from hosts immune system or can be used to cause a lot of damage - Proteases that destroy molecuels in chemotaxis - Can also break up antibodies-Dnase that destroys DNA - Modify cell surface to inhibit antimicrobial peptides - M protein is the hallmark virulence factor M protein - An anti-phagocytic cell surface expressed protein - Binds “Factor H” of the complement system - Factor H is a complement regulatory protein that protects self cells from C3b deposition - >100 M protein serotypes - Hypervariable N-terminus – basis for M protein serotypes - E.g. M1, M3 typically cause pharyngitis and invasive disease - E.g. M18 typically cause acute rheumatic fever - However, if you have antibodies to a particular M protein serotype you will opsonize and kill these bacteria Factor h is a host protein part of your complement system (shuts it down and protects cells) - Factor h binds to m protein, which allows the cell to be protected from c3b - You can make antibodies to m protein, which will allow you to opsonize it - Different streps have different m proteins (serotypes) - Different serotypes cause different infections - Blocks phagocytosis of the bacteria S. pyogenes makes 2 hemolysins - Streptolysins (O and S) - streptolysin S produces β-hemolysis - streptolysin O is “O2-sensitive” – can be seen under anaerobic conditions - Hyaluronic acid capsule - A polysaccharide - Hyaluronic acid is a major component of host tissues – bacteria “look like self” - Can also block opsonization through C3b (typical of other capsules) - On blood agar plate you get hemolysins around the colonies - Presence of oxygen inactivates streptolysins wont be seen - Bacteria make a capsule that looks like itself - Makes a capsule where some strains are very capsulated or some are not so much - Made of hyaluronic acid -This is a problem because this is also a component of our extracellular matrix - We can’t make a vaccine against this because it is the same as our tissue - This also makes the bacteria look like tissue too which means that we wont have an immune response to it Superantigens - Secreted exotoxins - Streptococcal pyrogenic exotoxins (Spe’s) - Function as potent activators of T cells and can result in a cytokine storm disease known as the toxic shock syndrome - NOT emetic like the staphylococcal enterotoxins (SE's)- You’ll develop an immune response to the antibodies of the toxin The disease: Pharyngitis (strep throat) - Most common in school aged children and teenagers - Fever and severe sore throat - Typically absence of cough - Swollen cervical lymph nodes - Tonsillar exudate (pus) and skin rash - Is it strep or viral??? - Diagnosed by a rapid strep test - Positive test = strep throat antibiotics - Negative test throat culture - Treated with antibiotics - β-lactams (no documented resistance!!!!) - Erythromycin (resistant strain exist) - Untreated pharyngitis can lead to a number of complications including acute rheumatic fever - It is very specific so when it is positive, you will have strep -If it’s negative, it’s less specific so they’ll have to figure it out more -Not a single strain anywhere that is resistant to b lactam antibiotics -Been using penicillin for the organism for a very long time -Can use erythromycin but there is resistance to erythromycin -If you’re allergic to penicillin -If you have untreated strep throat, the inflammation will go away and you will recover in two weeks - The problem with this is that it can cause acute rheumatic fever The disease: Impetigo - Most common among children - Also caused by S. aureus - A superficial skin infection - Red sores that forms crusts, normally on the face - Highly contagious through direct contact The disease: scarlet fever - Rash that develops typically during strep throat - 5-15 years of age - High fever, “strawberry tongue” - Red tongue - Rash – small red bumps - Normally on the chest and stomach - Can look like sunburn - Rough sandpaper - Lasts 2-7 days - Toxin mediated - caused by the “scarlet fever toxins” - Same toxins as streptococcal pyrogenic exotoxins - Toxins are superantigens The disease: Rheumatic fever - "Post infection” sequelae- Occurs 2-3 weeks after infection (e.g. strep throat or scarlet fever) - Typically occurs in children 5-15 years of age - A form of autoimmunity caused by antibody cross-reactivity with the M protein - Acute rheumatic fever the initial inflammation can cause painful swollen joints - Rheumatic heart disease damaged heart valves - Can lead to congestive heart failure - Patients are at increased risk for infective endocarditis by other pathogens - Rare in developed counties since 1960s but endemic in many developing countries - Doesn’t happen during infection but after the infection is gone - This is an autoimmune disease - Probably cross reactive to M protein -If you keep having acute rheumatic fever over and over again without antibiotics, you can get rheumatic heart disease - Rheumatic heart disease can be chronic and permanent because heart valves don’t usually get better -Some people do not have access to antibiotics and these people can develop this disease every few months -Causes rheumatic heart disease The disease: Invasive streptococcal disease - Rare in developed countries but very serious - Defined as isolation of S. pyogens from a normally sterile site - Blood isolation bacteremia - If soft tissue involved necrotizing fasciitis - If muscle involved necrotizing myositis - Streptococcal toxic shock syndrome Risk factors for invasive streptococcal disease - Tissue injury (penetrating and nonpenetrating) - Prior use of nonsteroidal antiinflammatory agents - Chicken pox in children (58-fold increased risk) - Postpartum - Lack of immunity to superantigens and M protein - MHC class II haplotypes (ie. superantigen receptors) Treatment - Antibiotics - Supportive therapy - Debridement/amputation - Intravenous immunoglobulin (IVIG) - Neutralize superantigen activity - Opsonization of S. pyogenes -Bacteria can get inside the injured tissue -Children with chicken pox are 58 times more likely to get this - Because chicken pox causes lesions on skins to allow the bacteria to get in and it suppresses the immune system -If you don’t have immunity to superantigens and the m protein you are at increased risk of getting flesh-eating bacteria -Depending on what MHC class II you have too -If you have MHC class II molecules that can bind to t cells better for this disease, you are more susceptible-IVIG is antigens from people that will be given to you -The chicken pox vaccine prevents the risk for this disease -MHC class II are receptors for the superantigens -In humans these are extremely polymorphic molecules -If the superantigen can bind well it will drive a hyper inflammatory disease - IVIG pool of antibodies from many donors -If you are exposed to new antigen, it will be processed and exposed to t cell where -.01 t cells will be activated to new antigen - Superantigen isn’t actually processed by APC -Binds directly to T cell receptor forcing unconventional contacts between t cell -Forces a lot of t cells to be activated -Superantigens bind to the B chain of the TCR and the MHC class II molecule on the APC -This can push the immune system into a hyper inflammatory stage that can lead to the toxic shock syndrome Mobile genetic elements and superantigens in S. pyogens - Almost all serotypes have a very similar core chromosome - All color-coated things are different viruses that have entered into the organism -Adds DNA to organism -Triangles are mobile genetic elements -Point is that strep is very similar but difference in it is driven by all mobile genetic elements - Believe that the mobile elements is what causes the disease - Encodes for 6 different superantigens - Most potent known activator t cells - Why does strep need superantigens causing your adaptive immune system to turn on because there is no benefit to a pathogen that causes toxic shock syndrome to kill the host (because they will have no host to grow in)? Mouse models of S. pyogenes nasopharyngeal infection - S. pyogenes is a human specific pathogen - Went from 1 million bacteria to 100 in two days - Mice are not infected (they can clear out the bacteria) and so they are not good models - Superantigens do not bind to mouse MHC class II - What would happen in transgenic mice that express human MHC class II (human leukocyte antigens DR4/DQ8)? - Would cause a while lot more bacteria coming back from human genes - This is likely because of the superantigens because they can bind to human MHC class II molecules over the mouse ones Superanitgens are critical for nasopharyngeal infection in HLA-B6 mice -Very left is wild type -If you knock out speA, infection drops way down -Deleting all other superantigen, you see variation in the model -They can still infect really well -Delta strain can’t infect at all -SpeA toxin is driving infection In mice -Infect the mice with all the different strains that were deleted-Most of the deletions do not have much of an affect on infection -If you delete the SpeA, the infections go down a lot -The SpeA superantigen drives the - If you delete superantigens on right panel, you see not so many strep in the lymphatic tissue - Think the superantigens drive it all and that it is an inflammation driven infection - Strep in the nose of the mice inactivating t cells but it is opposite of what wed think would happen T cell depletion in HLA-B6 mice - Taken T cells out - Wild type infected mice with normal t cells on left -cd 4 depletion doesn’t cause many infection drops -cd 8 drops a lot - Not sure why cd 8 happens over cd 4 - Antigens activate cd 4 and cd 8’s equally -The Strep needs to make superantigens to cause infections -It is using the T cells to promote its own infection -In a way we have imunocompromised the mice by removing the T cells, but the strep cannot develop anymore - Superantigens as vaccines - One toxin that drives the infection phenotype - Why not use this as a vaccine - Mutated a single amino acid to know where speA binds to MHC class II - 2 is a t cell specific one -Mutant toxin is dramatically impaired - Hundred to thousand times less active to the other one - Use this toxin as vaccine - Think that supernantigen should be used in vaccines for strep because think that without the use of superantigens, it wont be able to colonize - Epitopes on M protein that are similar to epitopes on our proteins with cardiac myosin - Antibodies to that epitope can bind to our own tissue -There was a single amino acid mutation that affected the ability of the superantigen to bind to the MHC class II molecule -The mutant protein is actually a 100-1000x less functional than the wild type -Use that protein as a vaccine -If you vaccinate the mice with the SpeA superantigen, strep cannot infect the mice [Show More]
Last updated: 3 years ago
Preview 1 out of 37 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Can't find what you want? Try our AI powered Search
Connected school, study & course
About the document
Uploaded On
May 15, 2021
Number of pages
37
Written in
All
This document has been written for:
Uploaded
May 15, 2021
Downloads
0
Views
154
Scholarfriends.com Online Platform by Browsegrades Inc. 651N South Broad St, Middletown DE. United States.
We're available through e-mail, Twitter, and live chat.
FAQ
Questions? Leave a message!
Copyright © Scholarfriends · High quality services·