*NURSING > QUESTIONS & ANSWERS > NURS 4403 (SOLVED MCQ)Chapter 43: Hematologic and Immunologic Dysfunction MULTIPLE CHOICE (All)
NURS 4403 (SOLVED MCQ)Chapter 43: Hematologic and Immunologic Dysfunction MULTIPLE CHOICE
Document Content and Description Below
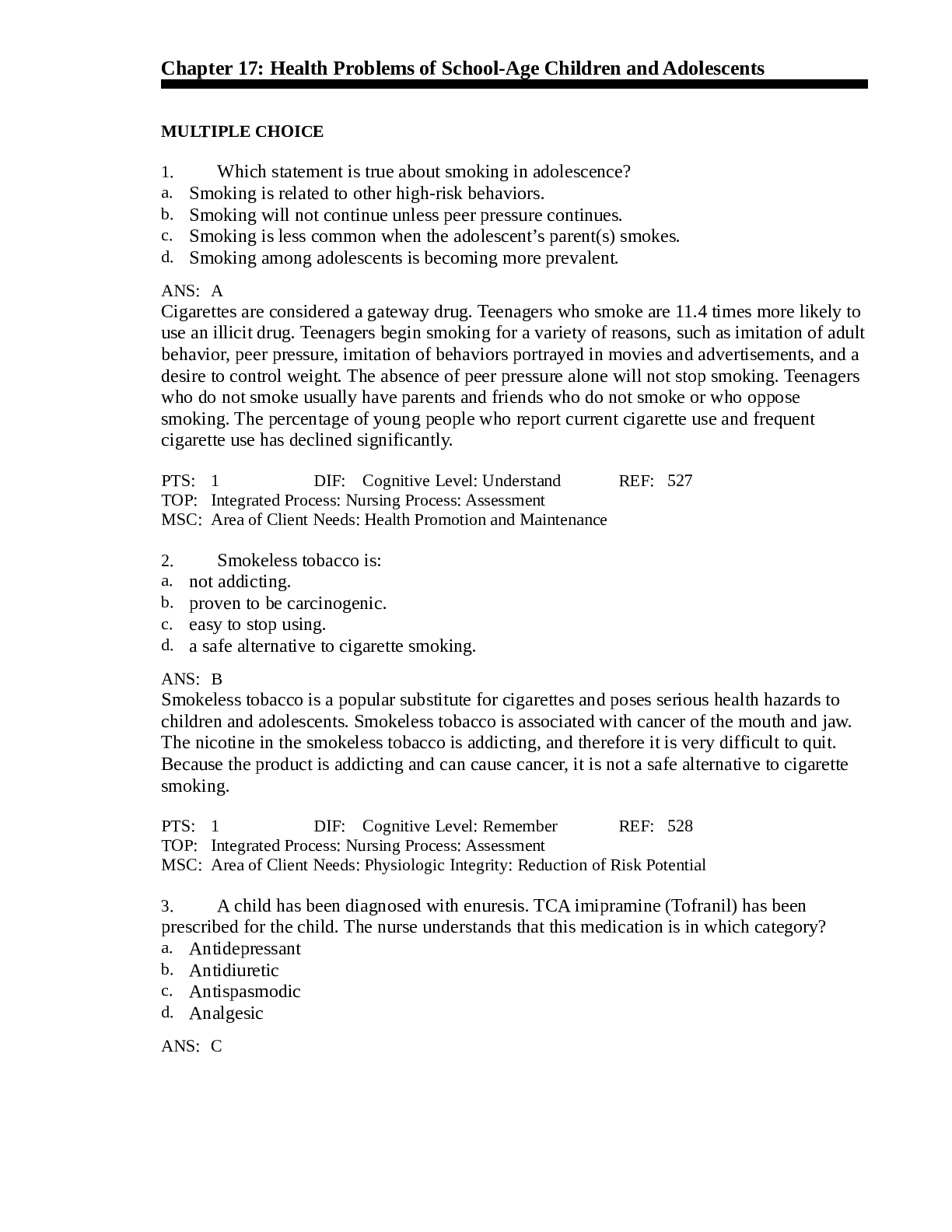
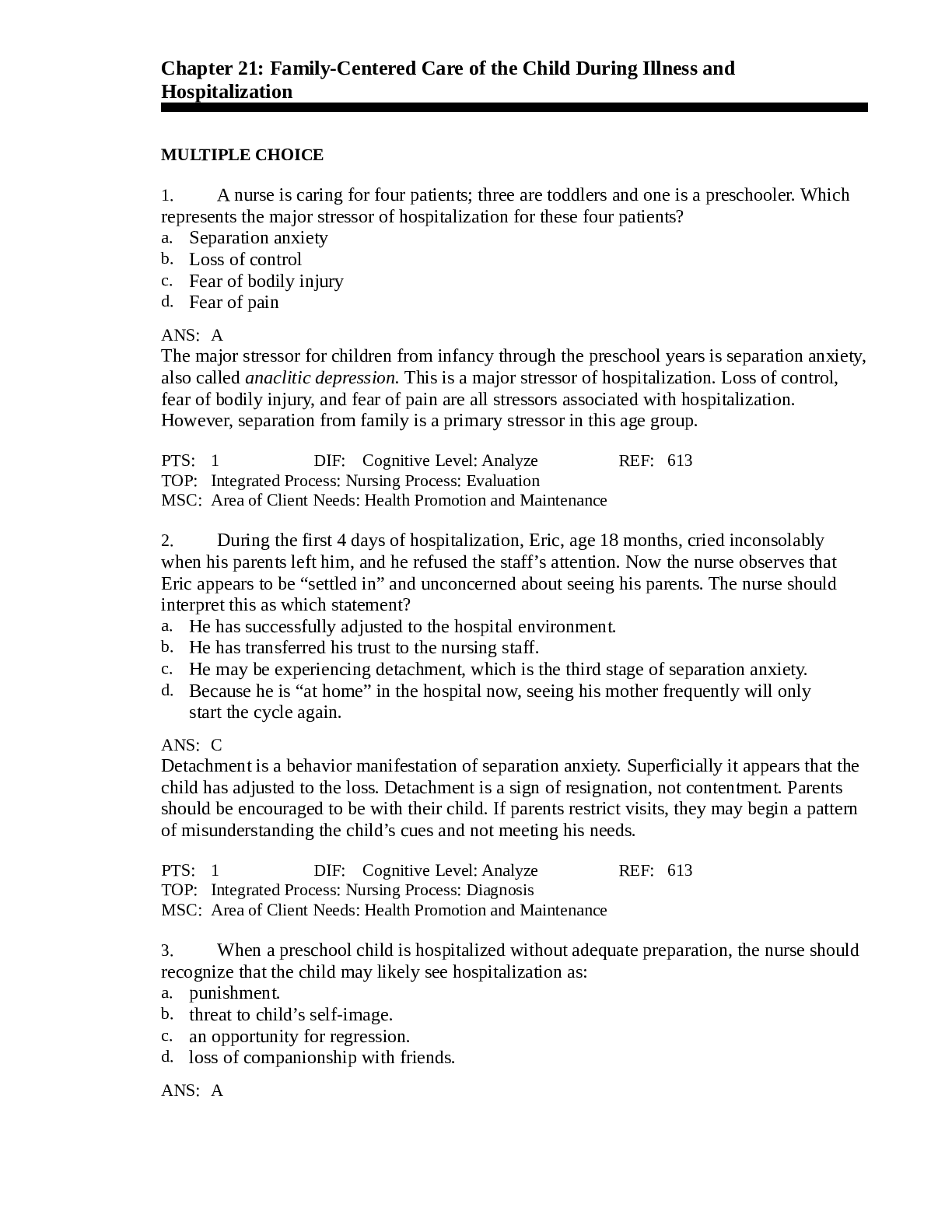
NURS 4403 Chapter 43: Hematologic and Immunologic Dysfunction MULTIPLE CHOICE 1. An accurate description of anemia is: a. Increased blood viscosity. b. Depressed hematopoietic system. Presence of a ... bnormal hemoglobin. c. d. Decreased oxygen-carrying capacity of blood. ANS: D Anemia is a condition in which the number of red blood cells or hemoglobin concentration is reduced below the normal values for age. This results in a decreased oxygen-carrying capacity of blood. Increased blood viscosity is usually a function of too many cells or of dehydration, not of anemia. A depressed hematopoietic system or abnormal hemoglobin can contribute to anemia, but the definition depends on the deceased oxygen-carrying capacity of the blood. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1362 OBJ: Nursing Process: Assessment MSC: Client Needs: Physiologic Integrity 2. Several blood tests are ordered for a preschool child with severe anemia. She is crying and upset because she remembers the venipuncture done at the clinic 2 days ago. The nurse should explain that: a. Venipuncture discomfort is very brief. b. Only one venipuncture will be needed. c. Topical application of local anesthetic can eliminate venipuncture pain. d. Most blood tests on children require only a finger puncture because a small amount of blood is needed. ANS: C Preschool children are very concerned about both pain and the loss of blood. When preparing the child for venipuncture, a topical anesthetic will be used to eliminate any pain. This is a very traumatic experience for preschool children. They are concerned about their bodily integrity. A local anesthetic should be used, and a bandage should be applied to maintain bodily integrity. A promise that only one venipuncture will be needed should not be made in case multiple attempts are required. Both finger punctures and venipunctures are traumatic for children. Both require preparation. PTS: 1 DIF: Cognitive Level: Application REF: 1365 OBJ: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 3. The most appropriate nursing diagnosis for a child with anemia is: a. Activity Intolerance related to generalized weakness. b. Decreased Cardiac Output related to abnormal hemoglobin. Risk for Injury related to depressed sensorium. c. d. Risk for Injury related to dehydration and abnormal hemoglobin. ANS: AThe basic pathology in anemia is the decreased oxygen-carrying capacity of the blood. The nurse must assess the child’s activity level (response to the physiologic state). The nursing diagnosis would reflect the activity intolerance. In generalized anemia no abnormal hemoglobin may be present. Only at a level of very severe anemia does cardiac output become altered. No decreased sensorium exists until profound anemia occurs. Dehydration and abnormal hemoglobin are not usually part of anemia. PTS: 1 DIF: Cognitive Level: Analysis REF: 1365 OBJ: Nursing Process: Diagnosis MSC: Client Needs: Physiologic Integrity 4. Which statement best explains why iron deficiency anemia is common during toddlerhood? a. Milk is a poor source of iron. b. Iron cannot be stored during fetal development. c. Fetal iron stores are depleted by age 1 month. d. Dietary iron cannot be started until age 12 months. ANS: A Children between the ages of 12 and 36 months are at risk for anemia because cow’s milk is a major component of their diet, and it is a poor source of iron. Iron is stored during fetal development, but the amount stored depends on maternal iron stores. Fetal iron stores are usually depleted by age 5 to 6 months. Dietary iron can be introduced by breastfeeding, iron- fortified formula, and cereals during the first 12 months of life. PTS: 1 DIF: Cognitive Level: Analysis REF: 1365 OBJ: Nursing Process: Assessment MSC: Client Needs: Physiologic Integrity 5. When teaching the mother of a 9-month-old infant about administering liquid iron preparations, the nurse should include that: a. They should be given with meals. b. They should be stopped immediately if nausea and vomiting occur. c. Adequate dosage will turn the stools a tarry green color. d. Preparation should be allowed to mix with saliva and bathe the teeth before swallowing. ANS: C The nurse should prepare the mother for the anticipated change in the child’s stools. If the iron dose is adequate, the stools will become a tarry green color. The lack of the color change may indicate insufficient iron. The iron should be given in two divided doses between meals, when the presence of free hydrochloric acid is greatest. Iron is absorbed best in an acidic environment. Vomiting and diarrhea may occur with iron administration. If these occur, the iron should be given with meals, and the dosage reduced and gradually increased as the child develops tolerance. Liquid preparations of iron stain the teeth. They should be administered through a straw, and the mouth rinsed after administration. PTS: 1 DIF: Cognitive Level: Analysis REF: 1366 OBJ: Nursing Process: Implementation MSC: Client Needs: Physiologic Integrity 6. Iron dextran is ordered for a young child with severe iron deficiency anemia. Nursing considerations include: a. Administering with meals. b. Administering between meals.c. Injecting deeply into a large muscle. d. Massaging injection site for 5 minutes after administration of drug. ANS: C Iron dextran is a parenteral form of iron. When administered intramuscularly, it must be injected into a large muscle using the Z-track method. Iron dextran is for intramuscular or intravenous administration; it is not taken orally. The site should not be massaged to prevent leakage, potential irritation, and staining of the skin. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1366 OBJ: Nursing Process: Implementation MSC: Client Needs: Physiologic Integrity 7. The nurse is recommending how to prevent iron deficiency anemia in a healthy, term, breastfed infant. What should she or he suggest? Iron (ferrous sulfate) drops after age 1 month. a. b. c. d. Iron-fortified commercial formula can be used by ages 4 to 6 months. Iron-fortified infant cereal can be introduced at age 2 months. Iron-fortified infant cereal can be introduced at approximately 6 months of age. ANS: D Breast milk supplies inadequate iron for growth and development after age 5 months. Supplementation is necessary at this time. Iron supplementation or the introduction of solid foods in a breastfed baby is not indicated. Introducing iron-fortified infant cereal at 2 months should be done only if the mother is choosing to discontinue breastfeeding. PTS: 1 DIF: Cognitive Level: Application REF: 1366 OBJ: Nursing Process: Implementation MSC: Client Needs: Physiologic Integrity 8. A condition in which the normal adult hemoglobin is partly or completely replaced by abnormal hemoglobin is: a. Aplastic anemia. c. Thalassemia major. b. Sickle cell anemia. d. Iron deficiency anemia. ANS: B Sickle cell anemia is one of a group of diseases collectively called hemoglobinopathies, in which normal adult hemoglobin is replaced by abnormal hemoglobin. Aplastic anemia is a lack of cellular elements being produced. Hemophilia refers to a group of bleeding disorders in which there is deficiency of one of the factors necessary for coagulation. Iron deficiency anemia affects size and depth of color of hemoglobin and does not involve abnormal hemoglobin. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1367 OBJ: Nursing Process: Assessment MSC: Client Needs: Physiologic Integrity 9. Which statement most accurately describes the pathologic changes of sickle cell anemia? a. Sickle-shaped cells carry excess oxygen. b. Sickle-shaped cells decrease blood viscosity. Increased red blood cell destruction occurs. c. d. Decreased red blood cell destruction occurs. ANS: CThe clinical features of sickle cell anemia are primarily the result of increased red blood cell destruction and obstruction caused by the sickle-shaped red blood cells. Sickled red cells have decreased oxygen-carrying capacity and transform into the sickle shape in conditions of low oxygen tension. When the sickle cells change shape, they increase the viscosity in the area where they are involved in the microcirculation. PTS: 1 DIF: Cognitive Level: Application REF: 1364 OBJ: Nursing Process: Diagnosis MSC: Client Needs: Physiologic Integrity 10. Which clinical manifestation should the nurse expect when a child with sickle cell anemia experiences an acute vaso-occlusive crisis? Circulatory collapse a. b. Cardiomegaly, systolic murmurs c. Hepatomegaly, intrahepatic cholestasis d. Painful swelling of hands and feet, painful joints ANS: D A vaso-occlusive crisis is characterized by severe pain in the area of involvement. If in the extremities, painful swelling of the hands and feet is seen; if in the abdomen, severe pain resembles that of acute surgical abdomen; and if in the head, stroke and visual disturbances occur. Circulatory collapse results from sequestration crises. Cardiomegaly, systolic murmurs, hepatomegaly, and intrahepatic cholestasis result from chronic vaso-occlusive phenomena. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1369 OBJ: Nursing Process: Diagnosis MSC: Client Needs: Physiologic Integrity 11. A school-age child is admitted in vaso-occlusive sickle cell crisis. The child’s care should include: a. Correction of acidosis. b. Adequate hydration and pain management. Pain management and administration of heparin. c. d. Adequate oxygenation and replacement of factor VIII. ANS: B The management of crises includes adequate hydration, minimizing energy expenditures, pain management, electrolyte replacement, and blood component therapy if indicated. The acidosis will be corrected as the crisis is treated. Heparin and factor VIII are not indicated in the treatment of vaso-occlusive sickle cell crisis. Oxygen may prevent further sickling, but it is not effective in reversing sickling because it cannot reach the clogged blood vessels. PTS: 1 DIF: Cognitive Level: Analysis REF: 1369 OBJ: Nursing Process: Implementation MSC: Client Needs: Physiologic Integrity 12. The parents of a child hospitalized with sickle cell anemia tell the nurse that they are concerned about narcotic analgesics causing addiction. The nurse should explain that narcotic analgesics: a. Are often ordered but not usually needed. b. Rarely cause addiction because they are medically indicated. c. Are given as a last resort because of the threat of addiction. d. Are used only if other measures such as ice packs are ineffective. ANS: BThe pain of sickle cell anemia is best treated by a multidisciplinary approach. Mild-to- moderate pain can be controlled by ibuprofen and acetaminophen. When narcotics are indicated, they are titrated to effect and given around the clock. Patient-controlled analgesia reinforces the patient’s role and responsibility in managing the pain and provides flexibility in dealing with pain. Few if any patients who receive opioids for severe pain become behaviorally addicted to the drug. Narcotics are often used because of the severe nature of the pain of vaso-occlusive crisis. Ice is contraindicated because of its vasoconstrictive effects. PTS: 1 DIF: Cognitive Level: Application REF: 1371 OBJ: Nursing Process: Implementation MSC: Client Needs: Physiologic Integrity 13. Which statement best describes -thalassemia major (Cooley’s anemia)? a. All formed elements of the blood are depressed. b. c. d. Inadequate numbers of red blood cells are present. Increased incidence occurs in families of Mediterranean extraction. Increased incidence occurs in persons of West African descent. ANS: C Individuals who live near the Mediterranean Sea and their descendants have the highest incidence of thalassemia. An overproduction of red cells occurs. Although numerous, the red cells are relatively unstable. Sickle cell disease is common in blacks of West African descent. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1373 OBJ: Nursing Process: Assessment MSC: Client Needs: Physiologic Integrity 14. Chelation therapy is begun on a child with -thalassemia major. The purpose of this therapy is to: a. Treat the disease. b. Eliminate excess iron. c. Decrease the risk of hypoxia. d. Manage nausea and vomiting. ANS: B A complication of the frequent blood transfusions in thalassemia is iron overload. Chelation therapy with deferoxamine (an iron-chelating agent) is given with oral supplements of vitamin C to increase iron excretion. Chelation therapy treats the side effects of disease management. Decreasing the risk of hypoxia and managing nausea and vomiting are not the purposes of chelation therapy. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1374 OBJ: Nursing Process: Implementation MSC: Client Needs: Physiologic Integrity 15. In which condition are all the formed elements of the blood simultaneously depressed? a. Aplastic anemia b. Sickle cell anemia c. Thalassemia major d. Iron deficiency anemia ANS: A Aplastic anemia refers to a bone marrow–failure condition in which the formed elements of the blood are simultaneously depressed. Sickle cell anemia is a hemoglobinopathy in which normal adult hemoglobin is partly or completely replaced by abnormal sickle hemoglobin. Thalassemia major is a group of blood disorders characterized by deficiency in the production rate of specific hemoglobin globin chains. Iron deficiency anemia results in a decreased amount of circulating red cells.PTS: 1 DIF: Cognitive Level: Comprehension REF: 1374 OBJ: Nursing Process: Assessment MSC: Client Needs: Physiologic Integrity 16. A possible cause of acquired aplastic anemia in children is: a. Drugs. b. Injury. c. Deficient diet. d. Congenital defect. ANS: A Drugs such as chemotherapeutic agents and several antibiotics such as chloramphenicol can cause aplastic anemia. Fanconi syndrome is a primary form of the disorder, which is congenital/present-at-birth and not acquired after birth. Injury, deficient diet, and congenital defect are not causative agents in acquired aplastic anemia. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1374 OBJ: Nursing Process: Assessment MSC: Client Needs: Physiologic Integrity 17. As related to inherited disorders, which statement is descriptive of most cases of hemophilia? a. Autosomal dominant disorder causing deficiency in a factor involved in the blood- clotting reaction b. X-linked recessive inherited disorder causing deficiency of platelets and prolonged bleeding c. X-linked recessive inherited disorder in which a blood-clotting factor is deficient d. Y-linked recessive inherited disorder in which the red blood cells become moon shaped ANS: C The inheritance pattern in 80% of all of the cases of hemophilia is X-linked recessive. The two most common forms of the disorder are factor VIII deficiency (hemophilia A or classic hemophilia), and factor IX deficiency (hemophilia B or Christmas disease). The disorder involves coagulation factors, not platelets. The disorder does not involve red cells or the Y chromosome. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1375 OBJ: Nursing Process: Diagnosis MSC: Client Needs: Physiologic Integrity 18. An acquired hemorrhagic disorder that is characterized by excessive destruction of platelets is: a. Aplastic anemia. b. Thalassemia major. c. Disseminated intravascular coagulation. d. Idiopathic thrombocytopenic purpura. ANS: D Idiopathic thrombocytopenic purpura is an acquired hemorrhagic disorder characterized by an excessive destruction of platelets, discolorations caused by petechiae beneath the skin, and a normal bone marrow. Aplastic anemia refers to a bone marrow failure condition in which the formed elements of the blood are simultaneously depressed. Thalassemia major is a group of blood disorders characterized by deficiency in the production rate of specific hemoglobin globin chains. Disseminated intravascular coagulation is characterized by diffuse fibrin deposition in the microvasculature, consumption of coagulation factors, and endogenous generation of thrombin and plasma.PTS: 1 DIF: Cognitive Level: Comprehension REF: 1379 OBJ: Nursing Process: Assessment MSC: Client Needs: Physiologic Integrity 19. What is most descriptive of the pathophysiology of leukemia? a. Increased blood viscosity occurs. b. Thrombocytopenia (excessive destruction of platelets) occurs. c. Unrestricted proliferation of immature white blood cells (WBCs) occurs. d. The first stage of the coagulation process is abnormally stimulated. ANS: C Leukemia is a group of malignant disorders of the bone marrow and the lymphatic system. It is defined as an unrestricted proliferation of immature WBCs in the blood-forming tissues of the body. Increased blood viscosity may occur secondary to the increased number of WBCs. Thrombocytopenia may occur secondary to the overproduction of WBCs in the bone marrow. The coagulation process is unaffected by leukemia. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1380 OBJ: Nursing Process: Diagnosis MSC: Client Needs: Physiologic Integrity 20. A boy with leukemia screams whenever he needs to be turned or moved. The most probable cause of this pain is: a. Edema. b. c. Petechial hemorrhages. Bone involvement. d. Changes within the muscles. ANS: B The invasion of the bone marrow with leukemic cells gradually causes a weakening of the bone and a tendency toward fractures. As leukemic cells invade the periosteum, increasing pressure causes severe pain. Edema, petechial hemorrhages, and muscular changes would not cause severe pain. PTS: 1 DIF: Cognitive Level: Analysis OBJ: Nursing Process: Planning REF: 1380 MSC: Client Needs: Physiologic Integrity 21. Myelosuppression associated with chemotherapeutic agents or some malignancies such as leukemia can cause bleeding tendencies because of a/an: a. Decrease in leukocytes. b. c. Vitamin C deficiency. Increase in lymphocytes. d. Decrease in blood platelets. ANS: D The decrease in blood platelets secondary to the myelosuppression of chemotherapy can cause an increase in bleeding. The child and family should be alerted to avoid risk of injury. Decrease in leukocytes, increase in lymphocytes, and vitamin C deficiency would not affect bleeding tendencies. PTS: 1 DIF: Cognitive Level: Application OBJ: Nursing Process: Planning REF: 1381 MSC: Client Needs: Physiologic Integrity 22. A child with leukemia is receiving triple intrathecal chemotherapy consisting of methotrexate, cytarabine, and hydrocortisone. The purpose of this is to prevent: a. b. Infection. Brain tumor. c. Drug side effects.d. Central nervous system (CNS) disease. ANS: D For certain children, CNS prophylactic therapy is indicated. This drug regimen is used to prevent CNS leukemia. This regimen does not prevent infection or drug side effects. If the child has a brain tumor in addition to leukemia, additional therapy would be indicated. PTS: 1 DIF: Cognitive Level: Application OBJ: Nursing Process: Planning REF: 1381 MSC: Client Needs: Physiologic Integrity 23. A young boy will receive a bone marrow transplant (BMT). This is possible because one of his older siblings is a histocompatible donor. This type of BMT is termed: a. Syngeneic. b. Allogeneic. c. Monoclonal. d. Autologous. ANS: B Allogeneic transplants are from another individual. Because he and his sibling are histocompatible, the bone marrow transplantation can be done. Syngeneic marrow is from an identical twin. There is no such thing as a monoclonal bone marrow transplant. Autologous refers to the individual’s own marrow. PTS: 1 DIF: Cognitive Level: Analysis OBJ: Nursing Process: Planning REF: 1389 MSC: Client Needs: Physiologic Integrity 24. A school-age child with leukemia experienced severe nausea and vomiting when receiving chemotherapy for the first time. The most appropriate nursing action to prevent or minimize these reactions with subsequent treatments is to: a. Encourage drinking large amounts of favorite fluids. b. Encourage child to take nothing by mouth (remain NPO) until nausea and vomiting subside. c. Administer an antiemetic before chemotherapy begins. d. Administer an antiemetic as soon as child has nausea. ANS: C The most beneficial regimen to minimize nausea and vomiting associated with chemotherapy is to administer the antiemetic before the chemotherapy is begun. The goal is to prevent anticipatory symptoms. Drinking fluids will add to the discomfort of the nausea and vomiting. Encouraging the child to remain NPO will help with this episode, but the child will have the discomfort and be at risk for dehydration. Administering an antiemetic after the child has nausea does not avoid anticipatory nausea. PTS: 1 DIF: Cognitive Level: Application REF: 1382 OBJ: Nursing Process: Implementation MSC: Client Needs: Physiologic Integrity 25. The nurse is preparing a child for possible alopecia from chemotherapy. Which suggestion should be included in the teaching? a. Explaining to the child that hair usually regrows in 1 year. b. Advising the child to expose the head to sunlight to minimize alopecia. c. Explaining to the child that wearing a hat or scarf is preferable to wearing a wig. d. Explaining to the child that, when hair regrows, it may have a slightly different color or texture.ANS: D Alopecia is a side effect of certain chemotherapeutic agents. When the hair regrows, it may be of different color or texture. The hair usually grows back within 3 to 6 months after the cessation of treatment. The head should be protected from sunlight to avoid sunburn. Children should choose the head covering that they prefer. PTS: 1 DIF: Cognitive Level: Application REF: 1383 OBJ: Nursing Process: Implementation MSC: Client Needs: Physiologic Integrity 26. A common clinical manifestation of Hodgkin’s disease is: a. Petechiae. b. c. Bone and joint pain. Painful, enlarged lymph nodes. d. Enlarged, firm, nontender lymph nodes. ANS: D Asymptomatic, enlarged, cervical or supraclavicular lymphadenopathy is the most common presentation of Hodgkin’s disease. Petechiae are usually associated with leukemia. Bone and joint pain are not likely in Hodgkin’s disease. The enlarged nodes are rarely painful. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1385 OBJ: Nursing Process: Assessment MSC: Client Needs: Physiologic Integrity 27. Which condition is caused by a virus that primarily infects a specific subset of T lymphocytes, the CD4+ T-cells? a. Wiskott-Aldrich syndrome b. Idiopathic thrombocytopenic purpura (ITP) c. Acquired immunodeficiency syndrome (AIDS) d. Severe combined immunodeficiency disease ANS: C AIDS is caused by the human immunodeficiency virus, which primarily attacks the CD4+ Tcells. Wiskott-Aldrich syndrome, ITP, and severe combined immunodeficiency disease are not viral illnesses. PTS: 1 DIF: Cognitive Level: Application REF: 1386 OBJ: Nursing Process: Assessment MSC: Client Needs: Physiologic Integrity 28. A young child with human immunodeficiency virus is [Show More]
Last updated: 3 years ago
Preview 1 out of 18 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$13.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Sep 08, 2021
Number of pages
18
Written in
All
Additional information
This document has been written for:
Uploaded
Sep 08, 2021
Downloads
0
Views
124

.png)





.png)