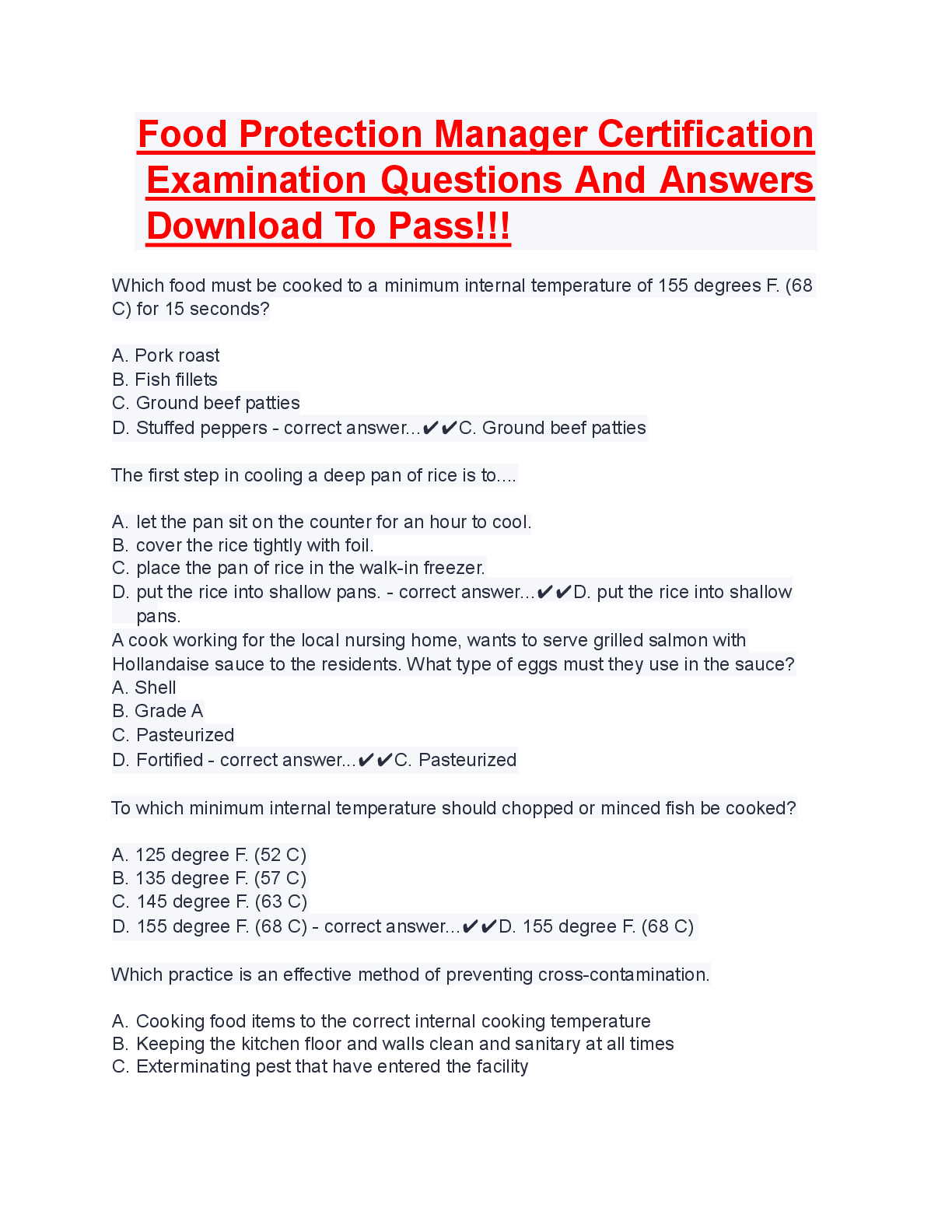
MULTIPLE CHOICE
1. Data generated by the laboratory is directly influenced by:
a. the quality of the specimen and its condition when received.
b. the physician’s decision to do the test.
c. quality control perform
...
MULTIPLE CHOICE
1. Data generated by the laboratory is directly influenced by:
a. the quality of the specimen and its condition when received.
b. the physician’s decision to do the test.
c. quality control performed on a monthly basis.
d. the air quality in the laboratory.
A
The old adage of garbage in–garbage out applies here. High-quality specimens result in high-quality laboratory results. Even though the laboratory professional does not usually perform the preanalytic process of collecting microbiology specimens, it directly affects the outcome.
REF: 112 OBJ: Level 1: Recall
2. To assist hospital personnel in collecting the highest quality specimen, the laboratory should:
a. post the microbiology laboratory’s phone numbers in each section so personnel can call with questions and problems.
b. develop a well-written handbook and make it available at every patient care unit.
c. allow personnel to go to the floor and collect all specimens.
d. severely reprimand staff for not collecting specimens properly.
B
The laboratory should establish policies for specimen management, and these must be distributed to all users and clients of microbiology laboratory services. A well-written handbook should be available at every patient care unit specifying the policies for specimen collection and transport, and test ordering. Training and education, such as in-services by the microbiology technologist, should be provided to the individuals collecting the specimens.
REF: 112 OBJ: Level 1: Recall
3. The goal of the specimen collector when collecting specimens for culture should be to:
a. make sure the specimen gets to the laboratory.
b. avoid hurting the patient when collecting the specimen.
c. maintain the viability of the living organisms at the site with minimal contamination.
d. get the specimen quickly to get the doctor off the collector’s back.
C
The specimens to be analyzed in the microbiology laboratory are likely to contain living organisms and the goal of the specimen collector must be to maintain the viability of these organisms with minimal contamination. That means the specimen needs to be delivered to the laboratory quickly so that the organisms do not die, taking your time when collecting the specimen to make sure you get a good one, and collecting the best specimen you can—even if it means inconveniencing the patient for just a little bit.
REF: 112 OBJ: Level 1: Recall
4. All the following principles of specimen collection are fundamental to ensuring appropriate specimen management except:
a. collect the appropriate quantity of specimen.
b. label the specimen accurately with the specific anatomic site and the patient information.
c. select the correct anatomic site to collect the specimen.
d. it is acceptable to delay transport of the specimen to the laboratory if it is in transport media.
D
The following principles of specimen collection are fundamental to ensuring appropriate specimen management: if possible, collect the specimen in the acute phase of the infection and before antibiotics are administered; select the correct anatomic site to collect the specimen; collect the specimen using the proper technique and supplies with minimal contamination from normal flora; collect the appropriate quantity of specimen; package the specimen in a container designed to maintain the viability of the organisms and avoid hazards due to leakage; label the specimen accurately with the specific anatomic site and the patient information; and transport the specimen to the laboratory promptly or make provisions to store the specimen in an environment that will not degrade the suspected organism(s).
REF: 112 OBJ: Level 1: Recall
5. Why does a fecal sample for culture need to be collected in a leak-proof, nonsterile container?
a. Fecal samples can be runny and if the specimen leaks, this can present a biohazard.
b. Many types of bacteria call the intestinal tract home; the specimen cannot become contaminated.
c. Leak-proof containers are always sterile, so the container will be leak-proof, as well as sterile.
d. Because DNA probes can determine resident flora from pathogenic bacteria.
B
There are many types of bacteria in a normal, healthy colon. With so many bacteria as normal flora, the risk of contamination is slight with a stool specimen. Stool specimens are evaluated for specific pathogens rather than identifying all bacteria present.
REF: 112 OBJ: Level 2: Interpretation
6. Swabs are appropriate for specimens collected from all the following sites except:
a. upper respiratory tract.
b. external ear.
c. urine.
d. genital tract.
C
In general, swabs are not recommended for urine collection because they do not provide sufficient quantity, are easily contaminated, and can become dried out, leading to a loss of organisms. Swabs are appropriate for specimens from the upper respiratory tract, external ear, eye, and genital tract. Swab collection systems are available that provide transport media and protect the specimen from drying. Urine cultures are always spread on a plate using a calibrated loop so that the technician can estimate the number of organisms present in the urine specimen.
REF: 112 OBJ: Level 2: Interpretation
7. How should specimen collection instructions be given to the patient to ensure collection of a good specimen for culture?
a. Verbally
b. Verbally, in many different languages
c. Verbally and written in English
d. Written, using simple language (in several languages) and pictures to help the patient understand the procedure as it is verbally explained
D
It is best to give the patient as much information as possible to collect the specimen. It is always good to read the procedure to the patient and show pictures to ensure they understand the procedure. This needs to be done in more than one language, because sometimes the patient does not speak English well and may not understand the procedure.
REF: 112 OBJ: Level 1: Recall
8. Why is a clean-catch midstream urine used for a urine culture as opposed to a clean-catch urine?
a. The first portion of the urine flow washes contaminants from the urethra and the next portion of urine is more representative of the bladder.
b. The name was changed, but the procedure remains the same and the entire amount of urine from the bladder is cultured.
c. No urine is free from contamination, so just wipe the external genitalia and void into the cup.
d. Catheterized specimens are also called clean-catch midstream urine specimen.
A
Instructions for urine collection must include an explanation of the clean-catch midstream urine specimen. A first morning specimen is preferred because it provides a more concentrated sample. The patient collects this specimen following cleansing of external genitalia to reduce the presence of indigenous flora. Patients are asked to void without collecting the first portion of the urine and instead to collect the middle portion. The first portion of the urine flow washes contaminants from the urethra and the midstream portion is more representative of the bladder. Personnel collecting catheterized specimens should also use this technique to eliminate organisms carried up the urethra during catheterization.
REF: 114 OBJ: Level 2: Interpretation
9. Sputum specimens are often collected for the diagnosis of:
a. acute pharyngitis.
b. bacterial pneumonia.
c. meningitis.
d. diverticulitis.
B
Many types of bacterial pneumonia produce purulent material that is coughed up as sputum. This specimen may contain the pathologic agents producing the disease. Unfortunately, lower respiratory tract specimens are among the most difficult specimens to collect adequately because they are contaminated with oropharyngeal flora.
REF: 114 OBJ: Level 2: Interpretation
10. The best way to minimize the amount of upper respiratory flora in a sputum specimen is to follow which of these procedures?
a. Cough up the specimen and when the specimen gets to the laboratory, digest it with enzymes that will kill the normal flora.
b. When plating the specimen, ensure that the swab goes deep into the sample to get only bacteria present in the lower lung.
c. Have the patient rinse the mouth with water and expectorate with the aid of a really deep cough directly into a sterile container.
d. Have a respiratory technician decontaminate a patient’s mouth and throat before the specimen is collected.
C
Rinsing the mouth will clean out most of the normal flora. A deep cough should gather as much purulent material as possible from the lower lung area. Using enzymes to digest the specimen will kill all bacteria in it, not just the normal flora. Sometimes the sputum is so thick that it is not possible to probe into the middle of the specimen to avoid any outer contaminating flora. It is not practical to have a respiratory technician disinfect a patient’s mouth and throat before collecting a sputum specimen.
REF: 114 OBJ: Level 2: Interpretation
11. The specimen of choice for detecting gastrointestinal pathogens is:
a. a urine specimen.
b. vomit.
c. a swab of the anal area with no feces on it.
d. a stool specimen.
D
A stool specimen contains samples of the gastrointestinal tract, and any pathogens that may be there can be passed out by the body. Urine specimens are good for diagnosing urinary tract infections. Vomit is not a good specimen because most gastrointestinal infections occur in the intestines and vomit comes from the stomach. A swab of the anal area with no feces on it will not reveal gastrointestinal pathogens. The most likely isolates from a swab of this type is skin flora.
REF: 114 OBJ: Level 1: Recall
12. Proper identification of each specimen includes a label firmly attached to the container with all the following information except:
a. diagnosis.
b. name.
c. identification number.
d. date.
A
Proper identification of each specimen includes a label firmly attached to the container with the following information: name, identification number, room number, physician, culture site, date of collection, and time of collection.
REF: 114 OBJ: Level 1: Recall
13. To perform a quality laboratory analysis, the laboratory needs specific information regarding the patient and the specimen. What can be a critical weak link in the specimen management process?
a. Poor specimen collection techniques
b. Incomplete information on the requisition
c. Poor-quality hospital information system
d. Poor-quality laboratory information system
B
To perform a quality laboratory analysis, the laboratory needs specific information regarding the patient and the specimen. All that the laboratory knows about the patient is learned from the requisition form. The less information that is provided, the more difficult it is for the laboratory to provide good patient care. Incomplete information on the requisition is often a weak link in the specimen management process. Complete and thorough requisitions can often lead the microbiology technologist to suspect certain pathogens based on the diagnosis or patient history. This will allow them to use specific media or make certain adjustments to the incubation to maximize recovery of the pathogen.
REF: 114 OBJ: Level 1: Recall
14. The requisition form should provide all the following information except:
a. patient name or identification number.
b. patient age and gender.
c. patient home address.
d. specific anatomic site.
C
Patient address is not needed on the requisition. The requisition form should contain the following information: patient name and identification number, patient age and gender, patient room number or location, physician name and address, specific anatomic site, date and hour of specimen collection, clinical diagnosis or relevant patient history, antimicrobial agents (if the patient is receiving), and name of individual transcribing orders.
REF: 114 OBJ: Level 1: Recall
15. If a test is not considered appropriate for the specimen, which of the following should happen?
a. Discipline the ward clerk for ordering the wrong test.
b. Discipline the nurse for ordering the wrong test.
c. Hold a training session to teach hospital staff about correctly ordering tests.
d. The laboratory needs to communicate with the physician to determine exactly what needs to be done.
D
The laboratory needs to communicate with the physician to find out what needs to be done. Disciplining the ward clerk and the nurse is not a solution to this problem. They do not know what are and what are not appropriate tests for each specimen. Because each situation is different, there is no need for a staff training session.
REF: 115 OBJ: Level 1: Recall
16. All specimens must be transported in:
a. leak-proof secondary containers.
b. syringes with needles attached.
c. a tube of broth.
d. a latex glove.
A
It is imperative that specimens collected for microbiology do not pose a safety hazard to those who handle them. Leaking containers and specimens with needles attached present the greatest hazards. All specimens must be transported in leak-proof secondary containers. A tube of broth and a latex glove are not leak-proof secondary containers.
REF: 115 OBJ: Level 1: Recall
17. A safe method of transporting aspirated wound material would be in a(n):
a. leak-proof bag.
b. tube of broth.
c. anaerobic transport system.
d. plastic container.
C
Transporting personnel should refuse to transport specimens without the protection of a secondary container. Refusing to accept syringes with needles attached is also appropriate. The aspirated material could also be transferred to another sterile container with a tight lid or to an anaerobic transport container.
REF: 115 OBJ: Level 2: Interpretation
18. What is the primary goal in the transportation of specimens to the laboratory?
a. To get the specimen to the laboratory by the end of the day
b. To maintain the specimen as near its original state as possible with minimal deterioration
c. To place the specimen in formalin and then transport it to the laboratory
d. To allow the specimen to sit, as long as it is delivered to the laboratory within 2 to 3 days after collection
B
The primary goal in the transportation of specimens to the laboratory is to maintain the specimen as near its original state as possible with minimal deterioration and to prevent risk to the specimen handler. Pathogens deteriorate rapidly if there is no food or the right environmental conditions. Formalin will kill most pathogens, so you do not want to place the specimen in formalin. Specimens should be transported to the laboratory ideally within 30 minutes of collection and preferably within 2 hours.
REF: 115 OBJ: Level 1: Recall
19. If transport of the specimen is delayed, the specimen can be maintained by all of the following except:
a. preservatives.
b. transport or holding medium.
c. saltwater.
d. anticoagulants.
C
Pathogens should be stored according to the best conditions to keep them viable. These include use of preservatives, anticoagulants, transport or holding medium, and even culture media. Organisms that are not cold sensitive can also be placed in the refrigerator to prevent degradation of the specimen.
REF: 115 OBJ: Level 1: Recall
20. A night technician is working in microbiology when a cerebrospinal fluid (CSF) specimen comes in. Almost simultaneously, the technician is called to the emergency department to draw blood on seriously injured car crash victims. How would the technician store the CSF until time permits to work on the CSF specimen?
a. Put the specimen in the refrigerator where it is good for 4 hours at 4° C.
b. Leave the specimen on the shelf where it is good for 6 hours at room temperature.
c. Pour the specimen into a tube of broth.
d. Place the specimen in a 35° C incubator for 6 hours.
D
Because CSF specimens are usually home to fastidious pathogens, creating an environment closest to that in the body will preserve the organisms the longest. So placing the specimen in a 35° C incubator for 6 hours will allow for maximum organism recovery. Leaving the tube in a refrigerator or at room temperature will cause the fragile organisms to die. CSF is always cultured according to protocol, and the entire specimen is never poured into a tube of broth to preserve it.
REF: 115 OBJ: Level 3: Synthesis
21. Two types of specimens can use preservatives to maintain them until they can be delivered to the laboratory. They are:
a. urine and stool.
b. urine and vaginal secretions.
c. stool and throat cultures.
d. pus from a wound and vaginal secretions.
A
The preservatives are designed to maintain the bacterial population in the urine at room temperature for 24 hours and thus are useful for collection of urine specimens at distant locations. Stool specimens for bacterial culture and ova and parasites can be added to a vial containing preservatives to maintain the organisms until they can be transported to the laboratory. Vaginal secretions, throat cultures, and pus from a wound can be placed in a vial containing transport media to maintain the viability of the organisms.
REF: 115 OBJ: Level 1: Recall
22. Specimens such as blood, bone marrow, and synovium are mixed with anticoagulants right after collection. Why should this occur?
a. Anticoagulants often dissolve part of the bacteria’s cell wall and congeal many bacteria into groups.
b. Organisms become bound up in the clotted material and are difficult to isolate.
c. It ensures the specimen will work when using an automated spreader device.
d. It kills off the normal flora and only leaves the pathogens in the specimen.
B
When a specimen clots, many of the pathogens are trapped inside the clotted blood. This makes it more difficult to determine the cause of the infection. Anticoagulants do not dissolve bacterial cell walls, but they do have a certain degree of antimicrobial properties. Very small amounts must always be used to ensure that this compound does not kill any bacteria present in the specimen.
REF: 116 OBJ: Level 2: Interpretation
23. The purpose of transport media is to:
a. make sure the microorganisms can multiply and live as though they were still in the host.
b. keep the swab moist so that the microorganisms do not dry out.
c. ensure the preservation of microorganisms in the specimen.
d. take the place of plating a routine culture with the specimen.
C
The purpose of transport media is to maintain the viability of the bacteria in the specimen. These materials do not want to promote multiplication because the metabolic by-products (i.e., acids) may build up and kill the bacteria. These media do keep the swab moist, but this is not their purpose. Also, the use of transport media is to do just that—ensure viable organisms during transport. They will never take the place of a routine culture.
REF: 116 OBJ: Level 1: Recall
24. In certain instances, it is desirable for specimens to be inoculated directly onto culture media. Specimens for this pathogen can be placed onto a commercial transport system called a JEMBEC system. What pathogen is this?
a. Bordetella pertussis
b. Clostridium difficile
c. Francisella tularensis
d. Neisseria gonorrhoeae
D
The JEMBEC system was developed specifically for transporting culture media inoculated with specimens for N. gonorrhoeae (GC) cultures. This method of transport increases the yield of organisms recovered from cultures. This system consists of a media selective for Neisseria spp., a Ziploc plastic bag, and a tablet. The tablet is added to the proper spot, a couple drops of water are added to the table, then the cover is placed on the media. The entire plate is inserted into the plastic bag and sealed so that an atmosphere high in carbon dioxide can be generated.
REF: 116 OBJ: Level 1: Recall
25. The shipment of clinical specimens and cultures of microorganisms is governed by a complex set of national and international guidelines issued by The Department of:
a. Transportation and the U.S. Postal Service.
b. Agriculture and the United Parcel Service.
c. Energy and Federal Express.
d. Defense and Homeland Security.
A
The Department of Transportation prescribes regulations for the safe transportation of hazardous material in commerce to ensure public safety and minimize risks in transportation. The regulations specify the way potentially infectious substances must be packaged to prevent leaks or spills, and how the packages must be labeled to caution handlers and other parties about their hazardous content. The U.S. Postal Service reinforces these transportation regulations.
REF: 116 OBJ: Level 1: Recall
26. How does the Department of Transportation (DOT) define an infectious substance?
a. Any substance capable of transmitting disease
b. A material known to contain or is suspected of containing a pathogen that causes disease in humans or animals
c. Any substance that can cause disease in animals
d. A bacterium, virus, prion, or virion
B
The DOT defines an infectious substance as material known to contain or is suspected of containing a pathogen that causes disease in humans or animals. An infectious substance is assigned to a risk group with a number from 1 (low risk) to 4 (high risk). The substance must be capable of transmitting disease to human or animals. It can be bacterial spores that are not considered a bacterium, virus, prion, or virion.
REF: 116 OBJ: Level 1: Recall
27. A technician receives a package from a supplier of quality control microorganisms. The package has a small watertight vial in a larger watertight tube. The larger tube has some bubble wrap around it, but the larger tube is just placed in the fiberboard box. All of the following was right with this packaging except the:
a. microorganisms are placed in a small watertight vial.
b. small vial is placed in a larger watertight tube.
c. primary receptacle was placed into the secondary container with no absorbent material.
d. outer container is made of fiberboard.
C
Patient specimens or culture isolates must be triple packaged before being shipped. The material is placed into a primary receptacle that must be watertight. Absorbent material is placed around the primary receptacle and it is then placed into a secondary container that is also watertight. The secondary package is sealed and placed into a sturdy outer container constructed of fiberboard.
REF: 116 OBJ: Level 2: Interpretation
28. All of the four levels represent a possible scheme for prioritizing the handling of specimens, except level:
a. 1: critical.
b. 2: unprotected.
c. 3: quantitation required.
d. 4: anticoagulated.
D
Level 4: specimens that are arriving in transport media. Level 1: critical because the specimens represent a potential life-threatening illness and are from an invasive source. Level 2: unprotected; may quickly degrade or have overgrowth of contaminating flora. Level 3: requires quantitation, and a delay in processing may adversely affect the accuracy of quantitation.
REF: 117 OBJ: Level 1: Recall
29. Types of specimens that can be batch processed include all the following except:
a. specimens for Neisseria gonorrhoeae (GC) cultures.
b. specimens for acid-fast bacillus (AFB) cultures.
c. stool specimens for ova and parasite tests that are collected in preservatives.
d. specimens for viral culture collected in viral transport media.
A
Specimens for GC cultures involve a very fastidious and fragile organism—Neisseria gonorrhoeae—and these cultures must be processed immediately so as to preserve the bacteria present in the specimen. All other specimens mentioned can be batch processed.
REF: 118 OBJ: Level 1: Recall
30. All of the following are examples of suboptimal specimens that must be rejected except the:
a. information on the requisition does not match the information on the specimen label.
b. specimen is for a Neisseria gonorrhoeae (GC) culture and submitted in a JEMBEC system.
c. specimen container is leaking when received in the laboratory.
d. specimen is received in a fixative solution such as formalin.
B
The specimen for a GC culture that is submitted in a JEMBEC system is the correct way to submit that specimen for culture. The rest options are grounds for rejecting the specimen.
REF: 118 OBJ: Level 1: Recall
31. The technician in the laboratory has received a specimen that is rejected. The technician calls the physician and tells the physician the specimen is unacceptable and the reason why. The physician insists that the culture needs to be performed on this unacceptable culture. What should the technician do?
a. Have the laboratory manager call the physician and tell him that a new specimen needs to be resubmitted because the laboratory will not perform a culture on this specimen.
b. Throw the specimen away and request a new one from the physician.
c. Plate the culture, but include a comment explaining the potentially compromised test results.
d. Discard both the specimen and the requisition, and pretend that the specimen was never received in the laboratory.
C
Physicians can be very insistent that laboratory tests be performed on suboptimal or unacceptable specimens. The best thing for the laboratory technician to do is to perform the requested test, include a comment that the specimen was suboptimal or unacceptable, and bring this matter to the pathologist. The pathologist will usually speak to the physician about the matter and take care of the problem.
REF: 118 OBJ: Level 3: Synthesis
32. Notations from the macroscopic (gross) examination of a specimen should include all the following except:
a. swab or aspirate.
b. stool consistency.
c. blood or mucus present.
d. the type of container in which the specimen was collected.
D
The gross appearance of the specimen may provide useful information to both the microbiologist and the physician. The physical characteristics of the specimen should be documented so that if different technologists work on the sample, they will all know the results of the gross examination. This gross examination also allows the processor to determine the adequacy of the specimen and the need for special processing. The type of the container in which the specimen was received has nothing to do with the macroscopic/physical/gross appearance of the specimen.
REF: 118 OBJ: Level 1: Recall
33. The direct microscopic examination is a useful tool for all the following reasons, except it can:
a. tell the physician what type of normal flora is present on the smear and if it is anaerobic or aerobic.
b. be used to determine the quality of the specimen.
c. give the microbiology technologist and the physician an indication of the infectious process involved.
d. dictate the need for nonroutine or additional testing.
A
A direct microscopic examination can inform a physician if bacteria are present, but it cannot tell the physician if the bacteria are normal flora, nor if they are anaerobic or aerobic. The microscopic examination will show formed elements such as epithelial cells, white blood cells, red blood cells, bacteria, and fungus, but it only shows shapes.
REF: 118 OBJ: Level 1: Recall
34. Direct microscopic examinations are not recommended for all the following specimen sources except:
a. throat specimens.
b. urethral discharge from a male.
c. nasopharyngeal specimens.
d. vaginal specimens.
B
A direct microscopic examination from the urethral discharge from a male can be diagnostic for Neisseria gonorrhoeae. This is because the male urethra is considered sterile, so any bacteria, especially intracellular bacteria, would be considered pathogenic. At all the other sites listed, there is much normal flora and the shapes of some of the normal flora can resemble the shapes of pathogenic organisms.
REF: 118 OBJ: Level 1: Recall
35. Nonselective media supports the:
a. grouping of microbes based on different characteristics demonstrated in the media.
b. growth of one type or group of microbes, but not another.
c. growth of most nonfastidious microbes.
d. growth of fastidious microbes through the addition of certain growth enhancers.
C
Nonselective media support the growth of most nonfastidious microbes. Selective media support the growth of one type or group of microbes, but not another. Differential media allow grouping of microbes based on different characteristics demonstrated on that medium. Enriched media contain growth enhancers that are added to nonselective agar to allow fastidious organisms to flourish.
REF: 119 OBJ: Level 1: Recall
36. Selective media:
a. allow the growth of fastidious microbes through the addition of certain growth enhancers.
b. support the grouping of microbes based on different characteristics demonstrated in the media.
c. support the growth of most nonfastidious microbes.
d. support the growth of one type or group of microbes, but not another.
D
Selective media support the growth of one type or group of microbes, but not another. Nonselective media support the growth of most nonfastidious microbes. Differential media allow grouping of microbes based on different characteristics demonstrated on that medium. Enriched media contain growth enhancers that are added to nonselective agar to allow fastidious organisms to flourish.
REF: 119 OBJ: Level 1: Recall
37. Differential media:
a. support the grouping of microbes based on different characteristics demonstrated in the media.
b. allow the growth of fastidious microbes through the addition of certain growth enhancers.
c. support the growth of most nonfastidious microbes.
d. support the growth of one type or group of microbes, but not another.
A
Differential media allow grouping of microbes based on different characteristics demonstrated on that medium. Nonselective media support the growth of most nonfastidious microbes. Selective media support the growth of one type or group of microbes, but not another. Enriched media contain growth enhancers that are added to nonselective agar to allow fastidious organisms to flourish.
REF: 119 OBJ: Level 1: Recall
38. Enriched media:
a. support the grouping of microbes based on different characteristics demonstrated in the media.
b. allow the growth of fastidious microbes through the addition of certain growth enhancers.
c. support the growth of most nonfastidious microbes.
d. support the growth of one type or group of microbes, but not another.
B
Enriched media contain growth enhancers that are added to nonselective agar to allow fastidious organisms to flourish. Nonselective media support the growth of most nonfastidious microbes. Selective media support the growth of one type or group of microbes, but not another. Differential media allow grouping of microbes based on different characteristics demonstrated on that medium.
REF: 119 OBJ: Level 1: Recall
39. An enrichment broth is:
a. a broth that has growth enhancers to allow fastidious organisms to flourish.
b. used as a supplement to agar plates to detect small numbers of most aerobes, anaerobes, and microaerophiles.
c. a liquid medium designed to encourage the growth of small numbers of a particular organism while suppressing other flora.
d. a broth that allows the grouping of microbes based on different characteristics demonstrated in the medium.
C
An enrichment broth is a liquid medium designed to encourage the growth of small numbers of a particular organism while suppressing other flora. Enrichment broths are incubated for a certain period and then must be subcultured to isolate the particular organism. Broth media can be used as a supplement to agar plates to detect small numbers of most aerobes, anaerobes, and microaerophiles.
REF: 119 OBJ: Level 1: Recall
40. How is culture media selected for specimen plating?
a. Determine the supplemental agar needed, as well as the broth media.
b. Always include nonselective media and differential media to help save a day of reading the culture on the bench.
c. Use only broth for the initial inoculation and subculture to plates after 24 hours of incubation.
d. The selection of media to inoculate is based on the type of specimen submitted for culture and the organisms likely to be involved in the infectious process.
D
The selection of media to inoculate is based on the type of specimen submitted for culture and the organisms likely to be involved in the infectious process. Specimens in which fastidious pathogens are more likely involved require media with appropriate nutrients to aid in their recovery. Specimens that are collected from a site containing normal flora will require types of media to diminish the normal flora while allowing the pathogens to be detected.
REF: 119 OBJ: Level 2: Interpretation
41. Routine primary plating media include all the following items except:
a. special biochemical media.
b. nonselective agar plate.
c. selective and differential medium for enteric gram-negative bacilli for most routine bacterial cultures.
d. broth medium used as a supplement.
A
Special biochemical media are used to identify the pathogen once it has been isolated from the primary culture. The other choices are correct for routine primary plating media.
REF: 119 OBJ: Level 1: Recall
42. What method is used to concentrate specimens to increase recovery of pathogens in the microbiology laboratory?
a. Homogenization
b. Centrifugation
c. Mixing
d. Anticoagulation
B
Using a centrifuge can help the microbiology technologist concentrate pathogenic organisms at the bottom of the tube in liquid specimens. This is usually performed when the specimen volume is large. Homogenization is used to release pathogens that may be trapped in a tissue. Mixing a specimen will spread out the pathogenic organisms as opposed to concentrating them.
REF: 119 OBJ: Level 1: Recall
43. What technique is used to isolate bacterial colonies when inoculating organisms onto an agar plate?
a. Homogenization
b. Centrifugation
c. Isolation streaking
d. Culture streaking
C
Isolation streaking is a special way of streaking or spreading out a specimen so that it covers all the plate. It allows for individual colonies to be spread apart from the large group of colonies, making it easier to isolate and identify pathogens. Homogenization and centrifugation are performed during specimen processing, not actually applying the specimen to the microbiologic media. Culture streaking is a general term that represents many ways of spreading a specimen over the surface of an agar plate.
REF: 119 OBJ: Level 1: Recall
44. When using the isolation streaking technique, the greatest concentration of organisms (if present) will be in which quadrant?
a. Fourth
b. Third
c. Second
d. First
D
The specimen is applied by rolling the swab or placing a drop of liquid specimen onto a small area at the edge of the plate. The inoculating loop is sterilized and allowed to cool thoroughly before streaking the agar. The cooled loop is passed back and forth through the inoculum in the first quadrant several times. The first quadrant should be at least one quarter of the plate, and the streak lines should be close together. The plate is turned one-quarter turn, and quadrant two is streaked by passing the loop through the edge of the first quadrant a few times and then streaking the rest of the area. The plate is turned one-quarter turn again, and the loop is passed through the edge of quadrant two a few times and into the rest of the third quadrant. Finally, passing the loop over the final area of the agar streaks the fourth quadrant.
REF: 119 OBJ: Level 2: Interpretation
45. When using the isolation streaking technique, the most isolated forms of the organism should be in which quadrant?
a. Fourth
b. Third
c. Second
d. First
A
The specimen is applied by rolling the swab or placing a drop of liquid specimen onto a small area at the edge of the plate. The inoculating loop is sterilized and allowed to cool thoroughly before streaking the agar. The cooled loop is passed back and forth through the inoculum in the first quadrant several times. The first quadrant should be at least one quarter of the plate, and the streak lines should be close together. The plate is turned one-quarter turn, and quadrant two is streaked by passing the loop through the edge of the first quadrant a few times and then streaking the rest of the area. The plate is turned one-quarter turn again, and the loop is passed through the edge of quadrant two a few times and into the rest of the third quadrant. Finally, passing the loop over the final area of the agar, streaks the fourth quadrant.
REF: 120 OBJ: Level 2: Interpretation
46. If a 0.001 mL quantitative loop is used to inoculate plate media for a urine culture, each colony of growth represents how many organisms per milliliter in the original sample?
a. 1 organism
b. 10 organisms
c. 100 organisms
d. 1000 organisms
B
0.001 mL of urine streaked onto a plate will give colony counts in multiples of 103. Therefore, each colony of growth represents 1000 organisms or colony-forming units per milliliter in the original sample.
REF: 121 OBJ: Level 2: Interpretation
47. Most bacterial cultures are incubated at what temperature range?
a. 25° to 27° C
b. 30° to 40° C
c. 35° to 37° C
d. 40° to 42° C
C
Most pathogenic bacteria grow at body temperature—35° to 37° C. Room temperature (25° to 27° C) allows pathogens to grow very slowly or it may kill the organism. The range 30° to 40° C includes body temperature, but the lower temperatures may inhibit growth and the higher temperatures may kill the organism. Most human pathogens do not grow at 40° to 42° C.
REF: 121 OBJ: Level 1: Recall
48. Aerobes are bacteria that grow in:
a. low oxygen tension.
b. high carbon dioxide concentrations.
c. high nitrogen concentrations.
d. ambient air.
D
Aerobes are bacteria that grow in ambient air. Capnophiles are bacteria that grow in increased carbon dioxide concentrations. Microaerophiles grow with reduced oxygen and increased carbon dioxide. Anaerobes grow when no or very little oxygen is present.
REF: 121 OBJ: Level 1: Recall
49. Microaerophiles are bacteria that grow:
a. in low oxygen concentrations.
b. in high carbon dioxide concentrations.
c. in reduced oxygen concentrations but increased carbon dioxide concentrations.
d. where little or no oxygen is present.
C
Aerobes are bacteria that grow in ambient air. Capnophiles are bacteria that grow in increased carbon dioxide concentrations. Microaerophiles grow with reduced oxygen and increased carbon dioxide. Anaerobes grow when no or very little oxygen is present.
REF: 121 OBJ: Level 1: Recall
50. Capnophiles are bacteria that grow:
a. in increased carbon dioxide concentrations.
b. in low oxygen concentrations.
c. in reduced oxygen concentrations but increased carbon dioxide concentrations.
d. where little or no oxygen is present.
A
Aerobes are bacteria that grow in ambient air. Capnophiles are bacteria that grow in increased carbon dioxide concentrations. Microaerophiles grow with reduced oxygen and increased carbon dioxide. Anaerobes grow when no or very little oxygen is present.
REF: 121 OBJ: Level 1: Recall
51. Anaerobes are bacteria that grow:
a. in increased carbon dioxide concentrations.
b. in low oxygen concentrations.
c. in reduced oxygen concentrations but increased carbon dioxide concentrations.
d. where little or no oxygen is present.
D
Aerobes are bacteria that grow in ambient air. Capnophiles are bacteria that grow in increased carbon dioxide concentrations. Microaerophiles grow with reduced oxygen and increased carbon dioxide. Anaerobes grow when no or very little oxygen is present.
REF: 121 OBJ: Level 1: Recall
52. Cultures for anaerobes and broth cultures may be incubated for:
a. 5 to 7 days.
b. 48 to 72 hours.
c. 7 to 9 days.
d. 12 to 24 hours.
A
Most routine bacterial cultures are held for 48 to 72 hours. Cultures for anaerobes and broth cultures may be held for 5 to 7 days. Unusual organisms may require special medium or conditions beyond the routine.
REF: 121 OBJ: Level 1: Recall
53. All of the following are questions that the microbiology technologist will ask while reading and interpreting the growth of cultures except:
a. What is the source of the culture?
b. How long has this culture been incubated?
c. Does this source have normal flora, or is it a sterile source?
d. What are the most likely pathogens in this specimen?
B
The microbiology technologist examines the culture media and uses considerable skill and judgment in the interpretation. The following questions are asked as each specimen is examined:
1. What is the specimen source?
2. Does this source have normal flora, or is it a sterile source?
3. If there is normal flora, what bacteria are found and what do these colonies look like?
4. What are the most likely pathogens in this specimen?
5. What is the colonial morphology of these pathogens?
6. Which media are demonstrating growth and what is the purpose of the media?
REF: 121 OBJ: Level 1: Recall
54. What work practice have microbiologists incorporated to keep laboratory testing cost-effective while providing optimum patient care?
a. Using definitive identification for the standard of quality patient care
b. Always identifying organisms to the maximum extent
c. Limited identification procedures
d. Limited antimicrobial susceptibility procedures
C
A challenging issue confronting microbiology technologists is the extent of the identification required. The microbiology technologist can ultimately save the patient money by providing an accurate diagnosis in a timely fashion using a cost-effective strategy. Although definitive identification is the standard for quality patient care, microbiologists have incorporated limited identification procedures into their daily practice.
REF: 123 OBJ: Level 1: Recall
55. When plating a nonroutine culture on primary culture media, the technician should ask all the following questions except:
a. What anaerobic bacteria will be present in this specimen?
b. Is the specimen likely to contain low numbers or high numbers of organisms?
c. Are the organisms to be found in this specimen likely to be fastidious or nonfastidious?
d. Are any normal flora presently associated with the specimen?
A
All the other questions are general appropriate questions to ask, whereas a is not. Other questions to be asked include:
1. If the number of organisms is extremely low, is it important to enhance them?
2. Does the specimen contain any preservative or growth inhibitors that must be counteracted?
3. What is a reasonable amount to culture?
REF: 123 OBJ: Level 2: Interpretation
56. Nonroutine specimens can include all the following specimen types except:
a. vein grafts.
b. syringe needles.
c. water samples.
d. multiple-lumen catheters.
B
Syringe needles are not cultured. All the choices except syringe needles are examples of nonroutine specimens.
REF: 123 OBJ: Level 1: Recall
57. To help the microbiologist report microbiology results to the physician in a timely fashion to ensure the appropriate treatment, the technician may use the _____ report.
a. antibiogram
b. infection control summary
c. preliminary
d. final
C
Preliminary reports allow the physician to check to make sure the pathogen is the suspected pathogen and change the treatment, if necessary. Final reports are issued only after all the work on a culture has been completed. Antibiograms and infection control summaries are used by infection control practitioners to track infections and infecting bugs in the hospital.
REF: 123 OBJ: Level 1: Recall
[Show More]















.png)
.png)
.png)