*NURSING > SHADOW HEALTH > ETOH Withdrawal/Pneumonia UNFOLDING Reasoning Case Study Elena Acosta, 54 years old (All)
ETOH Withdrawal/Pneumonia UNFOLDING Reasoning Case Study Elena Acosta, 54 years old
Document Content and Description Below
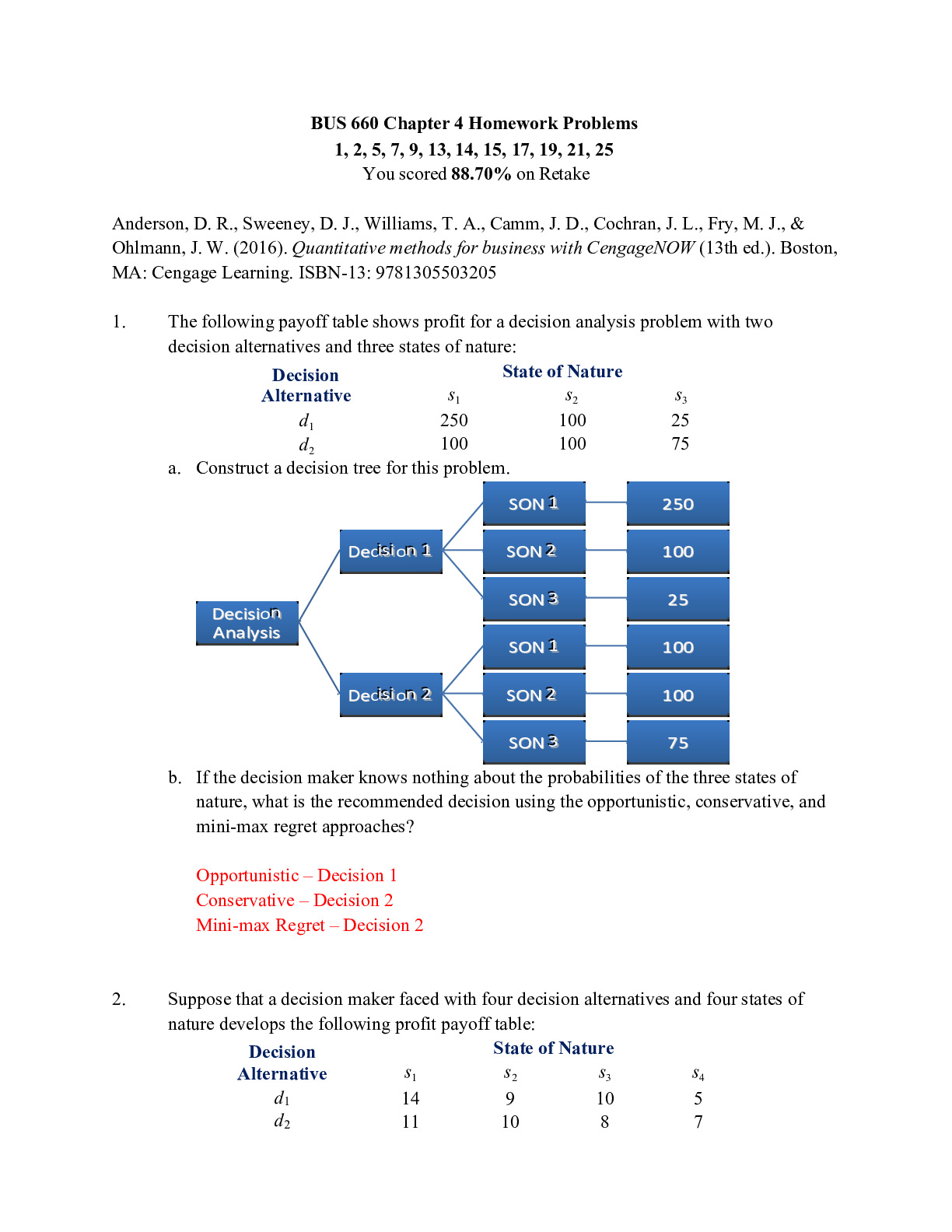
ETOH Withdrawal/Pneumonia UNFOLDING Reasoning Case Study Elena Acosta, 54 years old ETOH Withdrawal/Pneumonia UNFOLDING Reasoning Case Study Elena Acosta, 54 years old Primary Concept Addictio... n Interrelated Concepts (In order of emphasis) • Infection • Intracranial Regulation • Patient Education • Communication • Collaboration NCLEX Client Need Categories Percentage of Items from Each Category/Subcategory Covered in Case Study Safe and Effective Care Environment • Management of Care 17-23% ✓ • Safety and Infection Control 9-15% ✓ Health Promotion and Maintenance 6-12% ✓ Psychosocial Integrity 6-12% ✓ Physiological Integrity • Basic Care and Comfort 6-12% ✓ • Pharmacological and Parenteral Therapies 12-18% ✓ Copyright © 2019 Keith Rischer, d/b/a KeithRN.com. All Rights reserved.• Reduction of Risk Potential 9-15% ✓ • Physiological Adaptation 11-17% ✓ Copyright © 2019 Keith Rischer, d/b/a KeithRN.com. All Rights reserved.History of Present Problem: Elena Acosta is a 54-yr. old Hispanic woman with hypertension managed with hydrochlorothiazide. She is 63” (160.2 cm) and weighs 175 pounds (79.3 kg-BMI 31.0). She felt “crummy” and weaker the last 24 hours and called 911 when she began to have mid-sternal chest pain that increased with coughing and developed a harsh productive cough with green phlegm with difculty breathing. Initial lab results: WBC 14.5, neutrophils 92%, Hgb 12.9, potassium 3.5, creatinine 1.1, total bili 0.9, ALT 42, chestx-ray revealed RLL infltrate consistent with pneumonia, blood and sputum cultures collected and pending. Smell of ETOH present on her breath. Blood alcohol level 0.04, urine drug screen negative. She is admitted to the medical unitwith a diagnosis of pneumonia. You are the nurse responsible for her care. Personal/Social History: Ms. Acosta works in a mid-level management position for a corporate fnance company. She describes her job as quite stressful. She drinks 4-5 cups of coffee every day and to least 1-2 alcoholic drinks most days. She states that she shouldn’t smoke and has cut down to about ½ a pack per day. She reports drinking more and sleeping poorly following her father’s death over a year ago. She takes alprazolam as needed for sleep or when she feels more anxious. She is hesitant to be admitted because she has a high deductible insurance plan and doesn’t know how she will be able to affordit. What data from the histories are RELEVANT and have clinical significance to the nurse? (Reduction of Risk Potential) RELEVANT Data from Present Problem: Clinical Signifcance: RELEVANT Data from Social History: Clinical Signifcance: Patient Care Begins: Initial Assessment Medical Unit Current VS: P-Q-R-S-T Pain Assessment: T: 101.2 F/38.4 C (oral) Provoking/Palliative: nothing P: 96 (regular) Quality: ache R: 28 (regular) Region/Radiation: Denies chest pain currently/Headache-global BP: 138/88 Severity: 5/10 O2 sat: 92% room air Timing: constant What VS data are RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Health Promotion and Maintenance) RELEVANT VS Data: Clinical Signifcance:Current Assessment: GENERAL SURVEY: Looks older than stated age, alert, oriented, pleasant, in no acute distress, calm, bodyrelaxed, no grimacing, appears to be resting comfortably. NEUROLOGICAL: Alert & oriented to person, place, and situation (x3), knew year, but wrong day of week,feels fatigued with chills, weak, no focal defcits HEENT: Head normocephalic with symmetry of all facial features. PERRLA, sclera white bilaterally, conjunctival sac pink bilaterally. Lips, tongue, and oral mucosa pink and moist. RESPIRATORY: Breath sounds bibasilar crackles posteriorly, diminished aeration R>L bases, nonlabored respiratory effort on room air, productive cough with moderate amount thick yellow/brown tinged sputum CARDIAC: Pink, warm & dry, no edema, heart sounds regular, pulses strong, equal with palpation atradial/pedal/post-tibial landmarks, brisk cap refll. Heart tones audible and regular, S1 andS2 noted over A-P-E-T-M cardiac landmarks with no abnormal beats or murmurs. No JVD noted at 30-45 degrees. ABDOMEN: Abdomen round, soft, and nontender. BS + in all 4 quadrants GU: Voiding without difculty, urine clear/yellow INTEGUMENTARY: Skin warm, dry, intact, normal color for ethnicity. No clubbing of nails, cap refll <3 seconds, Hair soft-distribution normal for age and gender. Skin integrity intact, skin turgor elastic, no tenting present. What assessment data is RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Health Promotion & Maintenance) RELEVANT Assessment Data: Clinical Signifcance: Clinical Reasoning Begins… 1. Interpreting relevant clinical data, what is the primary problem? What primary health related concepts does this primary problem represent? (Management of Care/Physiologic Adaptation) Problem: Pathophysiology of Problem in OWN Words: Primary Concept:2. Collaborative Care: Medical Management (Pharmacologic and Parenteral Therapies) Care Provider Orders: Rationale: Expected Outcome: Supplemental O2 per nasal cannula at 2 L/min. for O2 sat <93 % VS every 4 hours and as needed Levofloxacin 500 mg IV in Sodium chloride 0.9% solution to infuse over 60 minutes Hydrochlorothiazide 50 mg PO daily Acetaminophen 325-650 mg PO every 4 hr PRN pain/temp >101; not to exceed 4000 mg/day Collaborative Care: Nursing 3. What nursing priority (ies) will guide your plan of care? (Management of Care) Nursing PRIORITY: PRIORITY Nursing Interventions: Rationale: Expected Outcome: 4. What body system(s) will you assess most thoroughly based on the primary/priority concern? (Reduction of Risk Potential/Physiologic Adaptation) PRIORITY Body System: PRIORITY Nursing Assessments:5. What is the worst possible/most likely complication(s) to anticipate based on the primary problem of this patient? (Reduction of Risk Potential/Physiologic Adaptation) Worst Possible/Most Likely Complication to Anticipate: Nursing Interventions to PREVENT this Complication: Assessments to Identify Problem EARLY: Nursing Interventions to Rescue: Unfolding: Eight Hours After Admission… What data from ongoing assessment are RELEVANT and have clinical significance to the nurse? (Reduction of Risk Potential) RELEVANT Assessment Data: Clinical Signifcance: 1. Recognizing relevant clinical cues, the nurse uses the CAGE questionnaire screening tool that her institution utilizes to screen for a drinking problem that could increase the risk of developing ETOH withdrawal. 2. The nurse asks the following clarifying questions (CAGE): a. Have you ever felt you needed to Cut down on your drinking? b. Have people Annoyed you by criticizing your drinking? c. Have you ever felt Guilty about drinking? d. Have you ever felt you needed a drink first thing in the morning (Eye-opener) to steady your nerves or to get rid of a hangover? Despite frequent coughing, Ms. Acosta is able to sleep intermittently. Sputum culture is positive for Streptococcus pneumoniae. To complete the admission assessment, the nurse addresses her ETOH drinking pattern and history. She admits to drinking a lot more lately due to the increased responsibilities of her job. She needs a drink in the morning to “calm herself down”, especially when she hasn’t been able to sleep. Admits to drinking more heavily since her father died a year ago. She doesn’t think she has a problem with drinking, just too much stress. She became so overwhelmed by the constant coughing and chest pain that she had a “drink or two” to “steady her nerves” before coming to the hospital ED. Denies use of alprazolam past week.What responses from the CAGE assessment are RELEVANT and have clinical significance to the nurse? (Reduction of Risk Potential) RELEVANT Data: Clinical Signifcance: Have you ever felt you needed to Cut down on yourdrinking? “I have been drinking more in the past year since my father died. Yeah, I wonder if I should cut back since it’s been a year since he died.” Have people Annoyed you by criticizing your drinking? “Since I live alone nobody knows except me about my drinking except me.” Have you ever felt Guilty about drinking? “I don’t feel guilty about my drinking because I need something to help me and it’s working for me.” Have you ever felt you needed a drink frst thing in the morning (Eye-opener) to steady your nerves or to get rid ofa hangover? “I need a drink in the morning to calm myself down and study my nerves.” Unfolding: Day #2 at 0100… Current VS: 4 Hours Ago: Current PQRST: T: 99.0 F/37.2 C T: 98.6 F/37.0 C Provoking/Palliative: Bright lights make pain worse P: 110 (reg) P: 98 (reg) Quality: Throbbing like an elastic band around my head R: 20 (reg) R: 20 (reg) Region/Radiation: headache BP: 154/92 BP: 136/84 Severity: 7/10 O2 sat: 95% RA O2 sat: 94% RA Timing: Constant What VS data are RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Health Promotion and Maintenance) RELEVANT VS Data: Clinical Signifcance: The nurse fnds Ms. Acosta fully awake. Reports she was starting to feel better because she was able to rest and eat a little food. Now she feels worse again, but in a “different way”. The nurse completes a focused respiratory assessment and general health assessment. Review the following reported signs and symptoms.Current Assessment: GENERAL SURVEY: Dressed in hospital gown; appears uncomfortable; restless; constantly repositioning self in bed NEUROLOGICAL: Alert & oriented to person, and place, did not know where she was or the day of the week; moderate hand tremors when asked to extend both arms HEENT: Head normocephalic with symmetry of all facial features. PERRLA, sclera white bilaterally, conjunctival sac pink bilaterally. Lips, tongue, and oral mucosa pink and moist. RESPIRATORY: Breath sounds clear with equal aeration on inspiration and expiration in all lobes anteriorly, posteriorly, and laterally, nonlabored respiratory effort; O2 sat: 95% on room air or oxygen? CARDIAC: Pink, warm & dry, no edema, heart sounds regular, pulses strong, equal with palpation at radial/pedal/post-tibial landmarks, brisk cap refll. Heart tones audible and regular, S1 and S2 noted over A-P-E-T-M cardiac landmarks with no abnormal beats or murmurs. No JVD noted at 30-45 degrees. ABDOMEN: Abdomen round, soft, and nontender. BS + in all 4 quadrants, no appetite, upset stomach with nausea; no vomiting GU: Voiding without difculty, urine clear/yellow INTEGUMENTARY: Forehead moist, skin warm, and intact, normal color for ethnicity. No clubbing of nails, cap refll <3 seconds, Hair soft-distribution normal for age and gender. Skinintegrity intact, skin turgor elastic, no tenting present Mental Status Examination (MSE): APPEARANCE: Moderately overweight woman; Looks fatigued and anxious. Less willing to answer assessment questions currently “Just leave me alone, please”. Disheveled appearance. Reports currently having difculty sleeping MOTOR BEHAVIOR: Moderate hand tremor when asked to extend arm twitching, reports feeling shaky inside, frequent repositioning noticed SPEECH: Normal rate and rhythm; occasionally slow to respond MOOD/AFFECT: c/o fatigue and mild depression; intense anxiety; 7 out of a possible 10; irritable and tearful at times THOUGHT PROCESS: Linear and logical THOUGHT CONTENT: Preoccupied with physical symptoms; no evidence of delusions PERCEPTION: Denies hallucinations; reports being bothered by bright lights and noise of the unit INSIGHT/JUDGMENT: Difcult to assess at this time; continues to recognize need for hospitalization for symptoms of pneumonia; seems to understand drinking as a coping strategy for increased stress and not a problem by itself COGNITION: Generally oriented but date is off by 2 days SUICIDAL/HOMICIDAL: Denies suicide, homicide or self-harm ideation What clinical data are RELEVANT that must be recognized as clinically significant? (Reduction of Risk Potential/Health Promotion and Maintenance) RELEVANT Assessment Data: Clinical Signifcance: RELEVANT MSE Assessment Data: Clinical Signifcance:Has the status improved or not as expected to this point? Does your nursing priority or plan of care need to be modified in any way after this evaluation assessment? (Management of Care, Physiological Adaptation) Evaluation of Current Status: Modifcations to Current Plan of Care: Clinical Reasoning Continues… Interpreting relevant clinical data, what is the “new” primary problem? What primary health related concepts does this primary problem represent? (Management of Care/Physiologic Adaptation) Problem: Pathophysiology of Problem in OWN Words: Primary Concept: Based on your current evaluation, what are your CURRENT nursing priorities and plan of care? (Management of Care) CURRENT Nursing PRIORITY: PRIORITY Nursing Interventions: Rationale: Expected Outcome: You have done an excellent job identifying the following: o Need to clarify/expand upon initial assessment information o Recognize potential for life-threatening complications o Recognize need to intervene in an emergent wayNow fnish strong and give the following SBAR report to the health care provider to communicate this change of status. (Management of Care) Situation: Name/age: BRIEF summary of primary problem: Day of admission/post-op #: Background: Primary problem/diagnosis: RELEVANT past medical history: . RELEVANT background data: Assessment: Most recent vital signs: RELEVANT body system nursing assessment data: RELEVANT psychosocial assessment data: How have you advanced the plan of care? RELEVANT lab values: TREND of any abnormal clinical data (stableincreasing/decreasing): Patient response: INTERPRETATION of current clinical status (stable/unstable/worsening): Recommendation: Suggestions to advance the plan of care: In response to the assessment and recommendations of thenurse, the primary care provider orders the following:Collaborative Care: Medical Management (Pharmacologic and Parenteral Therapies) 5. What psychosocial/holistic care PRIORITIES need to be addressed for this patient? (Psychosocial Integrity/Basic Care and Comfort) Psychosocial PRIORITIES: PRIORITY Nursing Interventions: Rationale: Expected Outcome: CARE/COMFORT: Caring/compassion as a nurse Physical comfort measures EMOTIONAL (How to develop a therapeutic relationship): Discuss the following principles needed as conditions essential for a therapeutic relationship: • Rapport • Trust • Respect • Genuineness • Empathy Care Provider Orders: Rationale: Expected Outcome: Lorazepam 2 mg now. Lorazepam 1 mg by mouth (PO) every 4 hours x 2 days. Lorazepam 1 mg PO q 1 hr. for breakthrough withdrawal symptoms (elevated CIWA scores). Hold and notify provider for sedation prior todose. Max dose of 12 mg per 24 hours. Thiamine 1100 mg PO/IV/IM Q8H/TID x 3 days, then 100 mg. PO daily Folic acid 1 mg daily PO Multivitamins 1 tab daily by mouth CIWA scale every 4 hours with VS every 4 hours and PRN as clinically indicated Seizure precautions Fall risk precautions Referral to substance use disorder clinicalSPIRITUAL: • F-Faith or beliefs: • I-Importance and influence • C-Community: • A-Address: CULTURAL Considerations (IF APPLICABLE) Education Priorities/Discharge Planning What educational/discharge priorities will be needed to develop a teaching plan for this patient and/or family? (Health Promotion and Maintenance) Education PRIORITY: PRIORITY Topics to Teach: Rationale: Caring and the “Art” of Nursing What is the patient likely experiencing/feeling right now in this situation? What can you do to engage yourself with this patient’s experience, and show that he/she matters to you as a person? (Psychosocial Integrity) What Patient is Experiencing: How to Engage: [Show More]
Last updated: 2 years ago
Preview 1 out of 14 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Nov 08, 2022
Number of pages
14
Written in
Additional information
This document has been written for:
Uploaded
Nov 08, 2022
Downloads
0
Views
122