*NURSING > SHADOW HEALTH > Sepsis/Septic Shock UNFOLDING Reasoning Case Study STUDENT Jack Holmes, 72 years old (All)
Sepsis/Septic Shock UNFOLDING Reasoning Case Study STUDENT Jack Holmes, 72 years old
Document Content and Description Below
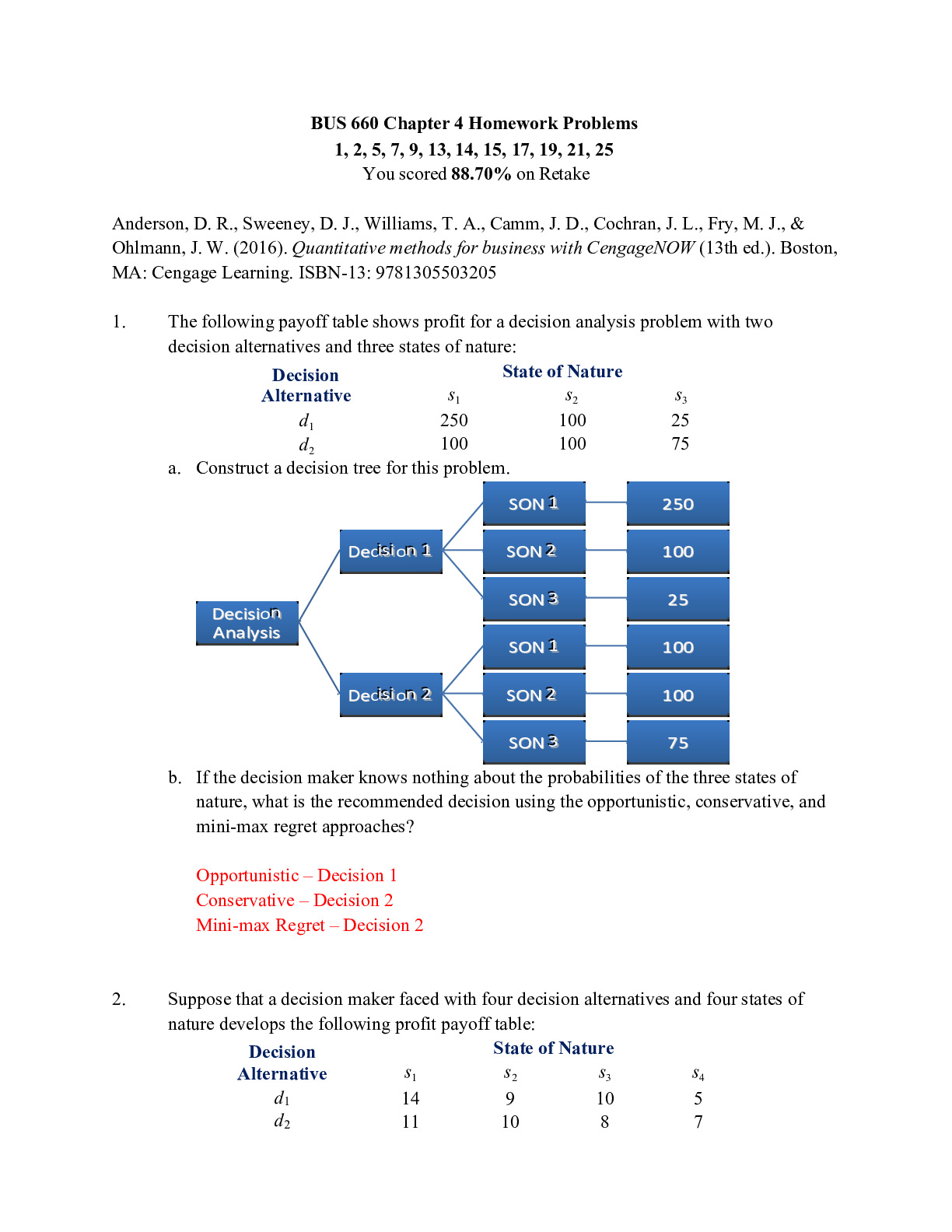
Sepsis/Septic Shock UNFOLDING Reasoning Case Study STUDENT Jack Holmes, 72 years old Copyright © 2018 Keith Rischer, d/b/a KeithRN. All Rights reserved. Sepsis/Septic Shock UNFOLDING Reasoning C... ase Study STUDENT Jack Holmes, 72 years old Primary Concept Perfusion Interrelated Concepts (In order of emphasis) Inflammation Infection Tissue Integrity Clinical Judgment Patient Education Communication NCLEX Client Need Categories Percentage of Items from Each Category/Subcategory Covered in Case Study Safe and Effective Care Environment Management of Care 17-23% Safety and Infection Control 9-15% Health Promotion and Maintenance 6-12% Psychosocial Integrity 6-12% Physiological Integrity Basic Care and Comfort 6-12% Pharmacological and Parenteral Therapies 12-18% Reduction of Risk Potential 9-15% Physiological Adaptation 11-17% History of Present Problem: Jack Holmes a 72-year-old Caucasian male brought to the ED by ambulance from a skilled nursing facility (SNF). According to report from the paramedic, when the SNF nursing staff attempted to wake him this morning, he would not respond, and his BP was 74/40 with a MAP of 51. He has a history of Parkinson’s disease, COPD, CHF, HTN, depression, and a stage IV decubitus ulcer on his coccyx that developed three months ago. He does not follow commands, is unresponsive to verbal stimuli, but responds to a sternal rub with grimacing and withdrawing from stimulus. Personal/Social History: He has lived in the skilled nursing facility the past three years and has been bed bound the past year due to his advanced Parkinson’s disease. He was a heavy smoker, 1 PPD for 40 years until he moved to the SNF. What data from the histories are RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential) RELEVANT Data from Present Problem: Clinical Significance: BP of 74/40 History of Parkinson’s Disease, COPD, CHF, HTN, depression Stage IV decubitus ulcer Found unresponsive this morning, does not respond to verbal stimuli, only sternal rubbing The blood pressure is way too low to maintain adequate perfusion of the tissues The patient has a lot of chronic illnesses that the nurse needs to take into consideration Ulcers, especially of this stage, are a large source of infection The nurse needs to start brainstorming on why the patient could be unresponsive, and it is important to note that the patient is still able to respond to verbal stimuli; the nurse also needs to be sure to document this as a baseline level of consciousness RELEVANT Data from Social History: Clinical Significance: Bed bound for the past year Was a heavy smoker Patient’s who are bed bound are at a much higher chance of illness due to decreased movement, the formation of bed sores, decreased exercise and most likely poor nutrition Heavy smokers are at a greater risk of developing respiratory infections and impairment due to the damage done to the alveoli and lung tissue after years of smoking Patient Care Begins Current VS: P-Q-R-S-T Pain Assessment: T: 103.4 F/39.7 C (oral) Provoking/Palliative: Not responsive verbally, withdraws to pain, no other indicators of pain P: 135 (irregular) Quality: R: 32 (regular) Region/Radiation: BP: 76/39 MAP: 51 Severity: O2 sat: 91% 2 liters n/c Timing:What VS data are RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Health Promotion and Maintenance) RELEVANT VS Data: Clinical Significance: Temperature of 103.4 F Irregular pulse, 135 bpm Respiration rate of 32 BP of 76/39 O2 sat of 91% on 2L NC Unresponsive, by withdraws from pain A significant temperature, a sign of infection or inflammation occurring in the body Pules is fast and irregular, could be due to an electrolyte imbalance and could also be due to the heart trying to compensate for some other disease process going on Respirations are increased due to poor oxygenation and the body trying to compensate for poor perfusion Blood pressure is significantly low, the body tissues are not able to be perfused as well as they should be Oxygen level is low due to poor perfusion; this is the cause of the increased respiration rate The nurse should be brainstorming on why he patient is unresponsive; in this case the nurse could infer that it is also a result of the decreased perfusion Current Assessment: GENERAL APPEARANCE: Pale and warm to touch. Appears tense. RESP: Tachypneic and working hard to breathe, intercostal and suprasternal retractions present. Breath sounds diminished and light crackles in lower lobes bilat. Nail beds have noticeable clubbing, barrel chest present. CARDIAC: Pale, 1+ pitting edema lower extremities, systolic murmur with an irregular rhythm, radial pulses weak and thready, cap refill 3 seconds NEURO: Does not open eyes to sound or pain, withdraws to pain, incomprehensible sounds to painful stimuli, does not follow commands but does not resist when moved on a stretcher. PERRL GI: Distended abdomen, firm/nontender, bowel sounds hypoactive in all quadrants GU: Foley catheter placed to monitor urine output. 50 mL tea-colored urine with no sediment, and no odor present SKIN: Stage IV decubitus to coccyx 1 cm x 0.5 cm x 0.5 cm depth, wound bed with visual bone noted at the base with large areas of necrosis on both sides of the sacrum bone. When dressing was removed, a large amount of yellow/green purulent drainage on dressing with a foul odor. Mucus membranes dry and pale. Determine current Glasgow coma scale score based on neurological assessment data: Glasgow Coma Scale Eye Opening Spontaneous 4 To sound 3 To pain 2 Never 1 Motor Response Obeys commands 6 Localizes pain 5 Normal flexion (withdrawal) 4 Abnormal flexion 3 Extension 2 None 1 Verbal Response Oriented 5 Confused conversation 4 Inappropriate words 3 Incomprehensible sounds 2 None 1 Total 8What assessment data is RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Health Promotion & Maintenance) RELEVANT Assessment Data: Clinical Significance: Pale skin color Tachypneic, working hard to breathe Diminished breath sounds, crackles in lower lobes Nail clubbing and barrel chest +1 pitting edema in lower extremities Systolic murmur Irregular heart rhythm, weak thready radial pulses Cap refill = 3 seconds Won’t open eyes, only responds to pain PERRL Firm, distended abdomen with hypoactive bowel sounds Tea colored urine with no odor or sediment Stage IV decubitus ulcer on sacrum; areas of necrosis Yellow/green drainage from pressure wound with foul odor Mucous membranes dry GCS of 8 Pale skin is a result of decreased blood flow and poor perfusion The patient is really trying hard to breathe to compensate for poor perfusion and to compensate for metabolic acidosis Crackles in the lower lobes indicate that there is fluid built up- did the patient potentially aspirate? Or is this fluid build up a result of poor cardiac output? Nail clubbing and barrel chest are long term effects of poor perfusion, most likely due to the patients extensive history of smoking and COPD There is slight pitting edema as a result of poor blood return to the heart (the blood is pooling) and as a result of capillary leak (which occurs in septic shock) Systolic murmurs are commonly heard when there are issues with the valves of the heart, but can also result from pulmonary or aortic stenosis, which could be a result of his PMH Irregular rhythms are a result of an electrolyte imbalance, weak pulses are a result of the heart being unable to pump well enough Cap refill is 3 seconds which indicates that it takes longer than it should for blood to return to the tissues Patient is unresponsive, but responds to pain; important for the nurse to note this as a baseline for the patient, which can be used to indicate if the patient’s condition is getting better or worse Pupils are equal, round and reactive, which indicates that there is not a brain injury occurring A distended abdomen can indicate an infection in the abdomen (peritonitis), but it can also indicate an obstruction, especially since there is hypoactive bowel sounds Urine is dark in color which indicates that the patient may be dehydrated; it is important to note that there is no sediment, which can be an indicator of a UTI There is a large ulcer on the sacrum, stage IV indicates that there is damage down to the bone, necrosis indicates that the tissue around the wound is now dead Yellow/green drainage is an indicator that there is infection occurring Dry mucous membranes helps to support the assumption that the patient is dehydrated GCS should be reevaluated often (hourly) to indicate if there is a change in the patient’s status; he is close to having a GCS low enough to indicate the need for intubationRadiology Reports: What diagnostic results are RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Physiologic Adaptation) Radiology: Chest X-Ray Results: Clinical Significance: Cardiac silhouette slightly enlarged. No infiltrates present. Heart is enlarged, it has been working hard, which essentially builds up the muscle and makes the heart larger Lab Results: Complete Blood Count (CBC) WBC HGB PLTs % Neuts Bands Current: 18.5 13.1 250 85.2 3 Most Recent: 12.4 13.2 175 64 0 What lab results are RELEVANT and must be recognized as clinically significant by the nurse? (Reduction of Risk Potential/Physiologic Adaptation) RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: WBC of 18.5 Neutrophils of 85.2% Bands 3 WBC count is elevated about normal limits, indicating infection Neutrophils are elevated, which supports the assumption that there is an infection occurring Bands are elevated, normally they are 0; this indicates that there are immature neutrophils in the blood, which indicates that there is a large systemic infection Worsening Worsening Worsening Basic Metabolic Panel (BMP) Na K Gluc. Creat. Current: 147 5.2 172 1.6 Most Recent: 138 4.4 98 0.88 Cardiac Telemetry Strip: Regular/Irregular: irregular P wave present? NO PR: regular length QRS: regular length Interpretation: Atrial fibrillation Clinical Significance: The patient’s rhythm is very fast, very irregular, it looks like atrial fibrillation I would say that this bizarre rhythm is a result of an electrolyte imbalance; I believe the random firings are occurring in the atria because there is an obvious QRS complex and it is within a normal size range (3 small boxes).What lab results are RELEVANT and must be recognized as clinically significant by the nurse? (Reduction of Risk Potential/Physiologic Adaptation) RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: Sodium 147 Potassium 5.2 Glucose 172 Creatinine 1.6 With kidney failure, sodium levels increase, which can lead to arrythmias Potassium is retained as kidneys begin to fail; also, with septic shock, the increased capillary permeability causes the cells to lyse, which releases potassium; increased potassium can lead to arrythmias The liver begins to release glucose in response to anaerobic metabolism, as the cells are not receiving enough oxygen Creatinine levels increase as the kidneys begin to fail and are not working as they should Worsening Worsening Worsening Worsening Misc. Lactate PT/INR GFR Current: 7.4 1.6 45 Most Recent: n/a 0.9 >60 What lab results are RELEVANT and must be recognized as clinically significant by the nurse? (Reduction of Risk Potential/Physiologic Adaptation) RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: Lactate 7.4 PT/INR 1.6 GFR 45 Lactate, AKA lactic acid builds up as a result of the cells undergoing anaerobic metabolism due to the decreased amount of oxygen as a result of poor perfusion Clotting times increase (clotting takes longer) as the clotting cascade is activated as a result of the shock; the patient is at risk of bleeding GFR decreases as the kidneys are not working as they should as a result of decreased perfusion to them (the rate at which they are filtering is decreasing) Worsening Worsening Worsening Liver Panel Albumin Total Bili Alk. Phos. ALT AST Current: 2.9 5.1 285 134 175 Most Recent: 3.1 0.9 48 17 12 What lab results are RELEVANT and must be recognized as clinically significant by the nurse? (Reduction of Risk Potential/Physiologic Adaptation) RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: Albumin 2.9 Bilirubin 5.1 Alkaline Phosphate 285 ALT/AST both elevated This is a protein made by the liver that helps keep the vessel walls at a certain level of permeability (so that fluid does not shift out of them); it was already on the lower side, but now it is even lower as a result of liver failure due to decreased perfusion; it is important to monitor this because fluid (blood) can shift out of the vessels, decreasing vascular volume, causing edema, and worsening the shock Bilirubin is excreted from the liver through bile, but when the digestive tract is failing (signs of this included distension and hypoactive bowel sounds), the bilirubin is backed up into the liver and released in the blood stream Alkaline phosphate is used by the liver to help break up proteins, an increase in this indicates that there is liver failure occurring ALT and AST are measurements of liver enzymes, when these are Worsening Worsening Worsening Worseningincreased, it is a good indicator that there is liver failure occurring Urinalysis + UA Micro Color: Clarity: Sp. Gr. Protein Nitrite LET RBCs WBCs Bacteria Epithelial Current: Tea Clear 1.050 NEG NEG NEG <5 <5 NEG None Most Recent: Yellow Clear 1.025 NEG NEG NEG <5 <5 NEG None What lab results are RELEVANT and must be recognized as clinically significant by the nurse? (Reduction of Risk Potential/Physiologic Adaptation) RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: Tea colored urine Specific gravity 1.050 Nitrate, WBC’s, bacteria all negative Darker colored urine is an indicator of dehydration Higher specific gravity (1.005-1.030 is WNL) indicates that the patient is dehydrated It is important to note that nitrate, WBC’s and bacteria are negative because this can help eliminate the concern that there is a urinary tract infection Stable, although this is a concern of dehydration Stable, although this is a concern of dehydration StableLab Planning: Creating a Plan of Care with a PRIORITY Lab: (Reduction of Risk Potential/Physiologic Adaptation) Lab: Normal Value: Clinical Significance: Nursing Assessments/Interventions Required: Lactate Value: 7.4 Critical Value: 4 is an indicator of sepsis Lactate is important to note because it is a good indictor that there is sepsis or septic shock occurring. It is important to monitor and trend this lab. A dangerously high lactate indicates that the patient is in metabolic acidosis Monitor lactate levels and note any improving or worsening trends Monitor other lab values, such as liver function and kidney function to note any improving or worsening organ damage Administer fluids as ordered to maintain adequate volume Administer O2 as ordered and monitor respiratory status and pulse ox constantly Keep the patient attached to a heart monitor at all times as acidosis can cause arrythmias Administer sodium bicarbonate as ordered and continue to monitor vitals frequently (q 5-15 minutes) Perform neuro assessments frequently and notify the provider of decreasing LOC Clinical Reasoning Begins… 1. Interpreting relevant clinical data, what is the primary problem? What primary health related concepts does this primary problem represent? (Management of Care/Physiologic Adaptation) Problem: Pathophysiology of Problem in OWN Words: Primary Concept: Septic shock The patient has entered septic shock as a result of a stage IV ulcer wound on the sacrum that has not been cared for properly and is now necrotic and infected. The patient appears to be dehydrated as well. As a result of both of these problems, the patient has entered septic shock. His body is unable to perfuse the tissues and the organs as it normally would, and now he is experiencing MODs (multiple organ dysfunction). Along with the MODs, the patient is experiencing severe electrolyte imbalances as a result of kidney failure and cell lysis secondary to increased capillary permeability. These electrolyte imbalances are causing cardiac arrythmias on his already over-working (trying to compensate for decreased blood pressure and decreased perfusion), poorly perfused heart The septic shock is causing decreased perfusion to the entire body including the tissues and organs, which is manifesting in his vital signs, decreased LOC and through his lab workCollaborative Care: Medical Management (Pharmacologic and Parenteral Therapies) Care Provider Orders: Rationale: Expected Outcome: Two large bore (18 g) IVs Fluid bolus 0.9% NS 30 mL/kg (2250 mL) Blood cultures x2 Urine culture Wound culture Vancomycin 2 g IV after cultures collected Clindamycin 600 mg IV every 6 hours If MAP remains <65 after 2250 mL of 0.9% NS…start Norepinephrine 1-12 mcg/min to maintain MAP >65 If MAP remains <65 after norepinephrine at 1 mcg/kg/min…start Vasopressin 0.04 units/minute to maintain MAP >65 Continuous cardiac monitor VS every 5-15” Acetaminophen 1000 mg PR every 6 hours PRN for fever >101 Two IV’s are needed to administer all of the medications that the patient needs NS helps to restore normal fluid levels, in this case, the patient is dehydrated Cultures will need to be obtained before any antibiotics are given; once the exact infective organism is identified, a better course of antibiotics can be prescribed Vancomycin and Clindamycin are both braid spectrum antibiotics, used to halt the growth of bacteria, used commonly to treat infections in the blood stream The NS is used to help restore the blood volume, once the volume is sufficient, the Norepinephrine can be given to help vasoconstrict, thus raising the blood pressure Vasopressin used in conjunction with norepinephrine will help to vasoconstrict the vessels to help maintain a sufficient blood pressure Keep the patient on the monitor to continue to assess heart rate and to watch for any changes in the cardiac rhythm VS are needed often to note any acute changes that could predict a worsening condition Acetaminophen will help to lower temperature, which is important, because with higher body temperatures, the faster the metabolism, and more oxygen and energy is used Two patent large IV sites inserted Vascular volume increased Cultures sent to the lab to be grown ASAP Both antibiotics are used to slow the growth of the infection It is important to be sure that there is sufficient volume in the vascular system before having the vessels constrict The nurse can constantly monitor for any arrhythmias Any VS changes will be noted quickly Once the body’s temperature is lowered, there will be a decrease in the metabolic rate, which will decrease the amount of oxygen being used and a less amount of lactate being built upPRIORITY Setting: Which Orders Do You Implement First and Why? (Management of Care) Care Provider Orders: Order of Priority: Rationale: 2 large bore (18 g) IVs Vancomycin 2 gram IV after cultures collected Clindamycin 600mg IV every 6 hours Fluid bolus 0.9% NS 30 mL/kg (2250 mL) Blood cultures, urine culture, wound culture Cardiac telemetry VS every 5-15” Acetaminophen 1000 mg PR every 6 hours PRN for temp >101 1. VS every 5-15 minutes 2. Cardiac telemetry 3. 2 large bore IVs 4. Obtain all cultures 5. Fluid bolus 6. Vancomycin 7. Clindamycin 8. Acetaminophen 1. It is important to obtain a baseline and know exactly what is going on with the patient before beginning interventions 2. You will want to know exactly what the heart is doing before beginning interventions (for example, if the patient is in a deadly rhythm, you’ll want to treat that before doing anything else) 3. You will need two IV’s to administer any medications ad begin other interventions 4. The nurse can draw lab samples straight off of the IV before flushing it; you’ll want to have true, unaffected cultures to grow before administering any fluids or antibiotics 5. Begin a fluid bolus to treat the patient’s decreased vascular volume to help raise blood pressure and increase perfusion 6. Vancomycin is ordered only once at this time as a bolus, it is important to start antibiotics within one hour of the patient’s arrival 7. Clindamycin is ordered every 6 hours, this will be started after the fluids and Vancomycin has been started; it is important to administer only one antibiotic at a time to determine the cause of any adverse effects or reactions 8. Acetaminophen is needed if the temperature is above 101, which it is at this time, but it can be administered after the fluids and antibiotics have been started Collaborative Care: Nursing 2. What nursing priority (ies) will guide your plan of care? (Management of Care) Nursing PRIORITY: Have baseline information to help determine worsening or improving conditions Start fluids and antibiotics ASAP Continually monitor the patient’s vitals and condition Provide a calm, quiet environment PRIORITY Nursing Interventions: Rationale: Expected Outcome: Obtain vitals, cardiac monitoring, assessment baseline Monitor labs for any changes Administer oxygen Administer IVF as ordered Baseline information is so important because it can help guide the course of care; when the patient’s condition is noted to be improving (or worsening), it helps the healthcare team determine if the current interventions are working or if there needs to be changes made Labs are a guide to what is truly going on inside of the patient’s body, and just like mentioned above, will help note if the patient’s condition is worsening or improving Increasing oxygenation saturation may help improve the patient’s respiration rate, and an increased amount of O2 allows the chance for more oxygen to reach the blood and be delivered to the body; this can also help determine if there is a chance that the patient needs to be intubated Administering fluids can help increase the vascular volume, but at the same time, it is important to continue to monitor lung sounds and Baseline and continuous assessments will be done Labs will be obtained at least once per shift Respiration rate will decrease, oxygenation may slightly improve Blood pressure will increase and the nurse will continue to monitorAdminister antibiotics (after cultures have been obtained!) Keep the patient on contact precautions watch for edema; you do not want to cause fluid overload in the patient, especially since there were crackles heard in the lower lobes of the lungs IV antibiotics should be started ASAP (ideally within one hour of the patient’s arrival), but first cultures must be obtained. When the unaffected cultures are obtained, this can help the lab determine the exact kind of antibiotic needed to treat the infection It is important to initiate precautions until the exact cause of the infection is determined, in the case that the infective agent could be MRSA lungs sounds and assess pitting edema IV cultures grown and antibiotics began within one hour of patient’s arrival Contact precautions will help the nurse avoid spreading the infection to herself and other patients 3. What body system(s) will you assess most thoroughly based on the primary/priority concern? (Reduction of Risk Potential/Physiologic Adaptation) PRIORITY Body System: PRIORITY Nursing Assessments: Cardiovascular system Monitor pulse and blood pressure Keep the patient on a continuous cardiac monitor Monitor pulse ox (perfusion) Monitor skin color and temperature Monitor capillary refill Monitor edema Auscultate heart sounds and lung sounds (crackles and murmurs can indicate fluid backing up = heart failure)4. What is the worst possible/most likely complication(s) to anticipate based on the primary problem of this patient? (Reduction of Risk Potential/Physiologic Adaptation) Worst Possible/Most Likely Complication to Anticipate: MODs (multiple organ dysfunction syndrome) Nursing Interventions to PREVENT this Complication: Assessments to Identify Problem EARLY: Nursing Interventions to Rescue: Monitor trends in BP and pulse Monitor labs Monitor LOC Monitor for decrease in pulse and BP (a sign of heart failure, as the heart is no longer able to compensate) Increase in lactate, changes in ABG Decreasing LOC, perhaps unresponsive to pain Administer IVF, may need vasopressors or positive inotropes Monitor labs frequently and notify the provider of any changes Notify provider immediately 5. What psychosocial/holistic care PRIORITIES need to be addressed for this patient? (Psychosocial Integrity/Basic Care and Comfort) Psychosocial PRIORITIES: Family needs to be updated, the may be scared, upset, confused PRIORITY Nursing Interventions: Rationale: Expected Outcome: CARE/COMFORT: Caring/compassion as a nurse Physical comfort measures In this case, the patient is not responsive. It is still important as the nurse to talk to the patient, let them know you are there and what is going on or what is about to be done to them. There is research indicating that a person may still be able to hear, even if they are unresponsive. It is also important to be compassionate with the family. They may be angry and upset. Allow them to voice their concerns. Ask them if they have questions and answer them as well as you can. Keep them informed It is important to keep the patient in a calm, private, quiet environment. Try to do little things for them that may increase their comfort, such as dimming the lights or using warm water to bathe them. Offer the family privacy and a safe, quiet place to talk. Offer them beverages, and a private area to converse Both the patient and the family will feel more comfortable in the setting, you will build a relationship with them and they will begin to trust you as their nurse When the patient is comfortable, there is a greater chance of better and faster healing. When the family is comfortable, they will be more likely to open up, they may be able to process their feelings better, and this will also help to build a trusting relationship with the nurse EMOTIONAL (How to develop a therapeutic relationship): Discuss the following principles needed as conditions essential for a therapeutic relationship: Rapport Trust Respect Genuineness Empathy Rapport is building a relationship with someone, as the patient and the family gets to know the nurse ad begin to trust her, the relationship will become stronger Trust is when the nurse is completely honest with the patient and the family, do not sugar things, but be sure to explain things to them in a way that they understand and in a way that is not blunt or rude Respect is allowing the patient and the family to voice their concerns and by respecting their wishes The patient and family will feel comfortable with the nurse The patient and family will trust the nurse The patient and family will feel respected and comfortable in the environmentGenuineness is when you stick to what you say you are going to do Empathy is when you feel the patient’s or the families emotions with them; allow them to vent and voice their concerns and really sit and listen with them; give them your time; do not say statements such as “I understand”, or “it could be worse” and this could be dismissive about their feelings The patient and the family will feel as though the nurse truly does care about them and their situation The patient and the family will feel as though they are cared for by the nurse CULTURAL Considerations (IF APPLICABLE) N/A- there was no mention of the patient’s cultural background N/A- it is important to be aware of the patient’s culture and background, but remember to be aware of your own biases and do not group people of the same culture/religion together as all being the same Evaluation: Evaluate the response of your patient to nursing and medical interventions during your shift. All physician orders that have been implemented are listed under medical management. Two hours later… The patient received 2,250 mL 0.9% NS, and a right internal jugular central line was placed in the ED. He has required norepinephrine 6 mcg/min to maintain a MAP >65. He was transferred to the ICU an hour ago and appears to be resting comfortably. He has received both antibiotics and acetaminophen. His lactate was repeated and is now 4.8. Current VS: Most Recent: Current PQRST: T: 101.4 F/38.6 C (oral) T: 103.4 F/39.7 C (oral) Provoking/Palliative: Denies pain P: 124 (irregular) P: 135 (irregular) Quality: R: 24 (regular) R: 32 (regular) Region/Radiation: BP: 86/56 MAP: 66 BP: 76/39 MAP: 51 Severity: O2 sat: 93% 2 liters n/c O2 sat: 91% 2 liters n/c Timing: Current Assessment: GENERAL APPEARANCE: Calm, body relaxed, no grimacing, appears to be resting comfortably RESP: Breath sounds diminished with crackles in lower lobes bilat, remains tachypneic but breathing not as labored CARDIAC: Pale, warm and dry, edema to BLE, heart sounds irregular with a murmur, pulses weak & equal, cap refill 2 seconds NEURO: Opens eyes to voice obeys simple commands, oriented to person only, thought he was at nursing home and had no idea what year it was. GI: Abdomen distended, firm/nontender, bowel sounds hypoactive per auscultation in all four quadrants GU: Foley in place with tea colored, clear urine 30 mL last two hours SKIN: Dressing on coccyx replaced in ED, no drainage present on dressing Determine current Glasgow coma scale score based on neurological assessment data:Glasgow Coma Scale Eye Opening Spontaneous 4 To sound 3 To pain 2 Never 1 Motor Response Obeys commands 6 Localizes pain 5 Normal flexion (withdrawal) 4 Abnormal flexion 3 Extension 2 None 1 Verbal Response Oriented 5 Confused conversation 4 Inappropriate words 3 Incomprehensible sounds 2 None 1 Total 131. What data is RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Health Promotion and Maintenance) RELEVANT VS Data: Clinical Significance: Temperature of 101.4 Pulse 124 Respiration rate of 24 BP 86/56 (MAP of 66) O2 sat at 93% on 2 liters NC Temperature is still slightly elevated, but has decreased 2 degrees, improving Pulse is still elevated, but has decreased and is stabilizing Respirations are still elevated but have significantly decreased BP is still low, but has improved since arrival Although pulse ox is still on the low side, it has increased 2% since the patients arrive; gas exchange in improving RELEVANT Assessment Data: Clinical Significance: Calm, body relaxed Crackles remain in lower lobes Breathing not as labored as before Pale, warm skin Edema to BLE Weak pulses, but equal Capillary refill 2 seconds Opens eyes to voice and obeys simple commands, oriented to person only Abdomen distended and hypoactive Foley in place, 30 mL of output in last two hours Dressing placed on coccyx with no drainage The patient does not appear to be in any pain Crackles are still a concern, but this is not a new finding; could this be from fluid backing up or is there a chance of a respiratory infection? Work of breathing is improving, patient is having better gas exchange in the lungs Skin is still pale, but it is no longer cold, which is a good indicator that perfusion is improving Edema will need to be continuously monitored; this could be a sign of third spacing as a result of low albumin levels Pulses are weak due to low blood pressure, but they have improved as they are now equal, palpable and no longer thready Capillary refill is within expected range, no longer taking three seconds, so perfusion is improving Patient has an increased LOC, before he was only able to respond to verbal stimuli, and although he is not back at his baseline LOC, it is a great improvement The nurse should continue an abdominal assessment; could the distension and hypoactive bowel sounds be a result of not eating or could it be a sign of something worse, such as peritonitis or an obstruction? The patient has a low urine output, which can be expected with septic shock, but it needs to be monitored; normal urine output is at least 30 mL per hour The wound is dressed and is no longer draining green/yellow drainage at this time; the nurse needs to continue to monitor for any drainage 2. Has the status improved or not as expected to this point? Does your nursing priority or plan of care need to be modified in any way after this evaluation assessment? (Management of Care, Physiological Adaptation) Evaluation of Current Status: Modifications to Current Plan of Care: The patient’s status has greatly improved, although he is no where near his baseline, so intensive care and monitoring needs to continue I do not think that there needs to be any changes to the care. The care that the patient has received is why the patient’s condition is improving. I do think that strict monitoring needs to continue, because the patient is not fully at his baseline yet. I do think that the nurse can associate more in depth neuro assessments on the patient now that he is more awake and alert. I also think it is important to corporate oral hydration and nutrition into his care plan now that he is awake and alert. By this time, the cultures may be retuning from the lab and a new course of antibiotics may be ordered. Wound care needs to be addressed for the stage IV ulcer on his sacrum 3. Based on your current evaluation, what are your CURRENT nursing priorities and plan of care? (Management of Care)CURRENT Nursing PRIORITY: maintain perfusion PRIORITY Nursing Interventions: Rationale: Expected Outcome: Continue to monitor the patient’s vitals and cardiac telemetry Improve patients hydration, thus improving vascular volume Help the patient to a sitting position There still could be changes in the patient’s status and it is important to continually monitor the patients vitals, LOC and cardiac rhythms Continue to administer IVF as ordered, but consult with he provider about offering the patient oral rehydration (of course after ensuring that there is no ileus or bowel obstruction aeb hypoactive bowel sounds) Having the patient sit up will allow better expansion of the lungs, thus increasing oxygenation and increasing perfusion The nurse will note any acute changes in the client’s status, along with improvements The patient will begin taking sips of water The patient will sit in a low-Fowler’s positionIt is now the end of your shift. Effective and concise handoffs are essential to excellent care and, if not done well, can adversely impact the care of this patient. You have done an excellent job to this point; now finish strong and give the following SBAR report to the nurse who will be caring for this patient: (Management of Care) Situation: Name/age: This is Jack Holmes, a 72 year old male BRIEF summary of primary problem: Was brough into the hospital unresponsive, had an initial GCS of 8, severely hypotensive and was noted to have a large stage IV ulcer on his coccyx; his WBC was elevated, his lactate was over 7, his liver and kidney enzymes were elevated, his urine came back clean, but blood cultures were sent to the lab. He was started on Clindamycin and Vancomycin, was given 2250 ml of NS and was given norepinephrine and vasopressin along with acetaminophen to bring his fever of 103.4 down Day of admission/post-op #: day of admission Background: Primary problem/diagnosis: septic shock RELEVANT past medical history:Parkinson’s disease, COPD, CHF, HTN, depression, stage IV ulcer on coccyx, history of smoking RELEVANT background data: patient lives in a nursing facility die to an increase in his Parkinson’s symptoms Assessment: Most recent vital signs: His temperate has decreased to 101.4 degrees, his pulse has become more regular at 124 bpm, respirations have decreased to 24, his work of breathing is much better, his O2 sat is at 93% on 2 liters NC, and his BP has improved a bit to 86/56 RELEVANT body system nursing assessment data: We have inserted an internal jugular line on the right side. He does not appear to be in any pain, his work of breathing is much better, although I do hear crackles in his lower lobes. His skin color and temperature have improved along with his cap refill. He is now awake and responsive, GCS has increased to 13, he is only oriented to himself, but that is much better than before when he would only respond to pain. He has a Foley in place and only 30 mL have drained in the last two hours. There is a dressing placed to the wound on his coccyx, andthere has been no further drainage since placing the dressing. His abdomen is distended and I have heard hypoactive bowel sounds. RELEVANT lab values: The only lab that has been repeated is his lactate, which is now 4.8 TREND of any abnormal clinical data (stable-increasing/decreasing): He is starting to stabilize, vitals are slowly stabilizing, but definitely not at his baseline yet. His LOC is improving as well, he seems to be perfusing much better now than when he arrived in the ED. How have you advanced the plan of care? I have administered IVF, along with the antibiotics and norepinephrine. I also administered acetaminophen to help alleviate his fever Patient response: he has responded well to the interventions, he does not appear to be in pain and he has not had any reactions. It appears as though his lactate is improving, his blood pressure has improved and his heart rate and rhythm has stabilized. His temperate is still not within a desired range, but it has decreased 2 degrees since administering acetaminophen INTERPRETATION of current clinical status (stable/unstable/worsening): unstable, but condition is improving Recommendation: Suggestions to advance the plan of care: I believe there should be an x-ray or CT scan performed, the crackles in the lungs and the distension of the abdomen are concerning to me. The labs should beredrawn soon to note any changes in electrolytes or liver and kidney function. I am concerned with his low urine output, so I would keep an eye on his kidney lab values. I would continue to monitor vitals and neuro assessments closely. I also think it is important for him to eat and drink something soon, as soon as he is cleared from his abdominal CT scan.Education Priorities/Discharge Planning What educational/discharge priorities will be needed to develop a teaching plan for this patient and/or family? (Health Promotion and Maintenance) Education PRIORITY: Management of infection PRIORITY Topics to Teach: Rationale: Wound care Noting signs of infection or inflammation Hand hygiene Promote ambulation and exercise Make sure to stay hydrated and eat healthy, nutritious meals The cause of the patients infection came from the wound on his coccyx; it is important to teach the patient and the family how to properly care for a wound such as this As soon as the patient feels any pain, note any drainage, develops a fever, or just begins to feel generally unwell, it is important to notify their PCP immediately Make sure to wash the hands thoroughly before and after caring for a wound The more someone is up and moving around, the less likely the chances are of a pressure sore forming Good nutrition and hydration are so important for the body in defending itself from foreign pathogens and in healing; encourage the utilization of protein shakes Caring and the “Art” of Nursing What is the patient likely experiencing/feeling right now in this situation? What can you do to engage yourself with this patient’s experience, and show that he/she matters to you as a person? (Psychosocial Integrity) What Patient is Experiencing: How to Engage: Fear, anxiety, confusion Be present with the patient. Ask them what they have questions about. With time, nurses can get an intuition and they can gauge how their patient is feeling and how ready they are for learning. In this case, the patient is only oriented to himself, so maybe it would be a better approach for the nurse to explain the take patient that he is in the hospital and that he has an infection, rather than jumping right in and educating the patient and overwhelming him with information. Offer your time with the patient, be there to answer questions and to comfort them when they are upset. It is also important to involve the family with the patient’s care, sometimes seeing someone that they are familiar with can help ease their anxieties Use Reflection to THINK Like a Nurse Reflection-IN-action (Tanner, 2006) is the nurse’s ability to accurately interpret the patient’s response to an intervention in the moment as the events unfold to make a correct clinical judgment. What did I learn from this scenario? How can I use what has been learned from this scenario to improve patient care in the future? What Did You Learn? How to Use to Improve Future Patient Care: I learned how important it is to closely trend assessment, vital sings and labs I also learned how important it is to involve the family in the patients care, sometimes being a nurse isn’t just for the patient, its for the family as well [Show More]
Last updated: 2 years ago
Preview 1 out of 22 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Nov 08, 2022
Number of pages
22
Written in
Additional information
This document has been written for:
Uploaded
Nov 08, 2022
Downloads
0
Views
112