NSG 3023 Final Exam Study Guide
CHAPTER 18
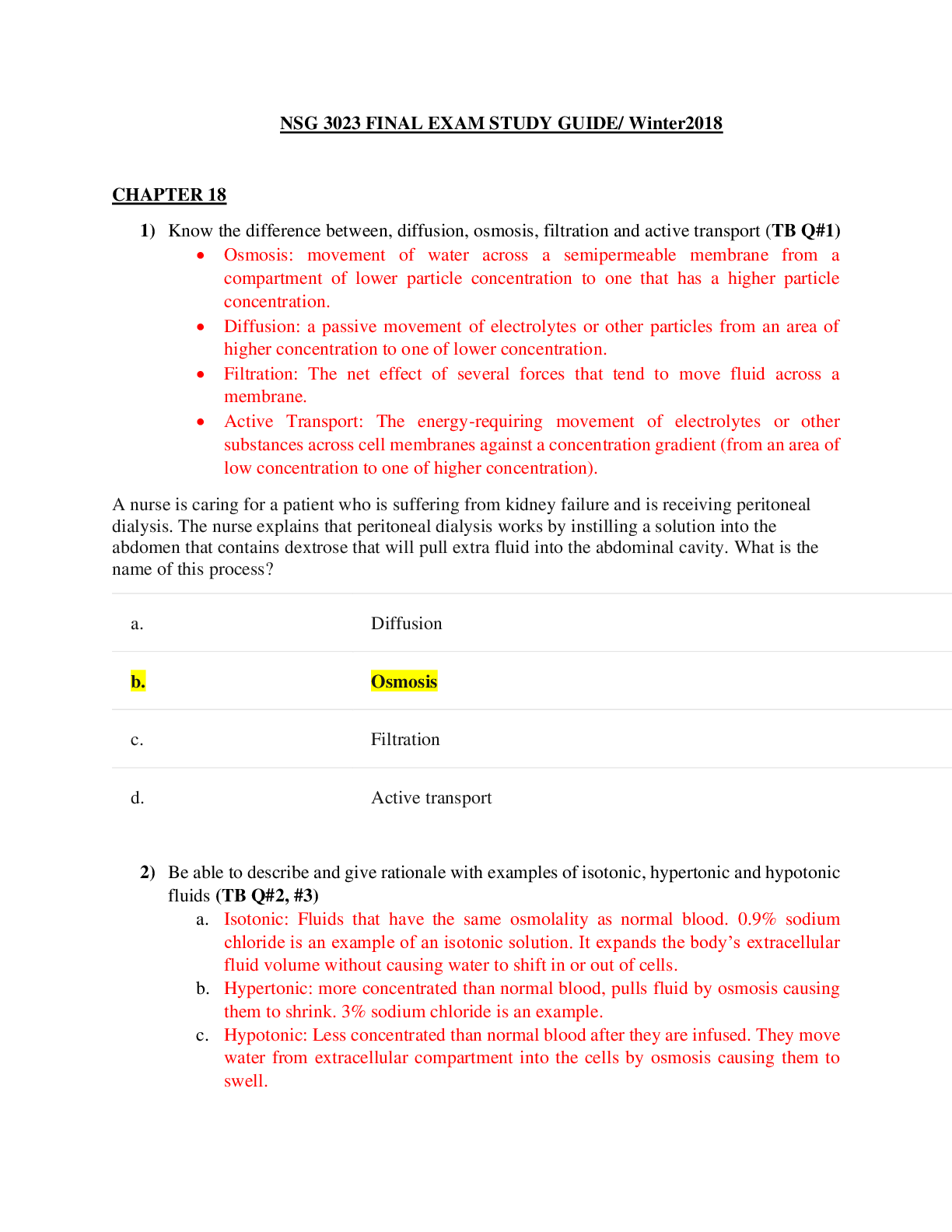
1) Know the difference between, diffusion, osmosis, filtration and active transport (TB Q#1)
• Osmosis: movement of water across a semipermeable membrane from a compartment
...
NSG 3023 Final Exam Study Guide
CHAPTER 18
1) Know the difference between, diffusion, osmosis, filtration and active transport (TB Q#1)
• Osmosis: movement of water across a semipermeable membrane from a compartment of lower particle concentration to one that has a higher particle concentration.
• Diffusion: a passive movement of electrolytes or other particles from an area of higher concentration to one of lower concentration.
• Filtration: The net effect of several forces that tend to move fluid across a membrane.
• Active Transport: The energy-requiring movement of electrolytes or other substances across cell membranes against a concentration gradient (from an area of low concentration to one of higher concentration).
A nurse is caring for a patient who is suffering from kidney failure and is receiving peritoneal dialysis. The nurse explains that peritoneal dialysis works by instilling a solution into the abdomen that contains dextrose that will pull extra fluid into the abdominal cavity. What is the name of this process?
a. Diffusion
b. Osmosis
c. Filtration
d. Active transport
2) Be able to describe and give rationale with examples of isotonic, hypertonic and hypotonic fluids (TB Q#2, #3)
a. Isotonic: Fluids that have the same osmolality as normal blood. 0.9% sodium chloride is an example of an isotonic solution. It expands the body’s extracellular fluid volume without causing water to shift in or out of cells.
b. Hypertonic: more concentrated than normal blood, pulls fluid by osmosis causing them to shrink. 3% sodium chloride is an example.
c. Hypotonic: Less concentrated than normal blood after they are infused. They move water from extracellular compartment into the cells by osmosis causing them to swell.
A patient has been admitted to the postsurgical nursing unit after surgery. The health care provider has ordered the patient to have an IV of 0.9% sodium chloride. The nurse who is caring for the patient recognizes this as what type of solution?
a. Hypotonic
b. Isotonic
c. Hypertonic
d. Hypnotic
3) Be able to describe the mechanism behind thirst (TB Q#4)
a. Thirst is a conscious desire of water. It regulates fluid intake when plasma osmolality increases (osmoreceptor-mediated thirst) or the blood volume decreases. The thirst-control mechanism is in the hypothalamus of the brain. Osmoreceptors there continually monitor plasma osmolarity; when osmolality increases, the hypothalamus stimulates thirst.
Two nursing students were having pizza one evening as they were studying. One student remarked that whenever she ate pizza, she was incredibly thirsty. The second student explained that this thirst was caused by:
a. colloid osmotic pressure.
b. osmoreceptors.
c. oncotic pressure.
d. hydrostatic pressure.
4) Describe insensible water loss and the effects on particular organs (TB Q#5)
a. Fluid output occurs through 4 organs: the skin, GI tract, lungs and kidneys (Insensible water loss is not visible). It is continuous and occurs through the skin and lungs. Insensible water output increases with fever.
A 7-year-old patient was admitted to the hospital with a high fever. The nurse caring for the child knows that the child has increased insensible water loss resulting from the fever and should receive additional water to prevent hypernatremia. Insensible water loss occurs through which organ?
a. Kidneys
b. GI tract
c. Skin
d. Stomach
5) Be able to describe the mechanism in which fluid and electrolyte balance is maintained or regulated partially by hormones (TB Q#7)
a. The hypothalamus controls release of ADG from the posterior pituitary gland. Antidiuretic hormone circulates to the kidneys, where it acts on the collecting ducts causing them to reabsorb water.
The bodys fluid and electrolyte balance is maintained partially by hormonal regulation. The nurse conveys an understanding of this mechanism in which statement?
a. The pituitary gland secretes aldosterone.
b. The kidney secretes antidiuretic hormone.
c. The adrenal cortex secretes antidiuretic hormone.
d. The pituitary gland secretes antidiuretic hormone.
6) Educations for clients at risk for hyperthermia.ie; (hypothalamus injury)
Any injury to the hypothalamus impairs heat loss mechanisms. Educate patients at risk for hyperthermia to do which of the following? (Select all that apply.)
a. Avoid strenuous exercise in hot, humid weather.
b. Avoid exercising in areas with poor ventilation.
c. Drink clear fluids before and after exercising, not during.
d. Wear light, loose-fitting clothing.
e. Do not visit hot climates.
7) A head injury could result in injury of hypothalamus or pituitary which could affect which organs
or functions? (TB Q#8)
a. It can affect/alter urine output.
A 15-year-old patient suffered a head injury as the result of a bicycle accident. The nurse is concerned about potential fluid complications caused by the injury. What should the nurse monitor most closely?
a. Aldosterone release
b. Urine output
c. Renin release
d. Body temperature
8) Be able to describe signs and symptoms of hyponatremia, hypokalemia, and hypochloremia. (TB Q#9)
a. Hyponatremia: water enters cells by osmosis causing them to swell. Signs of cerebral dysfunction occur when the brain cells swell
b. Hypokalemia: causes muscle weakness and if severe, cardiac dysrhythmias.
c. Hypochloremia: abnormally high blood chloride levels which occur with some types of acidosis some renal conditions and other electrolyte imbalances but has no unique signs or symptoms.
The patient is taking furosemide (Lasix) and has been complaining of muscle weakness. The nurse should be most concerned about which imbalance?
a. Hyponatremia
b. Hypokalemia
c. Hypochloremia
d. Hyperchloremia
9) What concerns would a health care provider anticipate with a patient on a ventilator related to acid base imbalance? (TB Q#10)
a. The healthcare provide would have concerns regarding the acid-base status. In determining the levels of the acid-base, the healthcare provider would do an Arterial blood gas analysis (ABG). It is an effective method of evaluating acid-base balance and oxygenation.
The patient is on a ventilator. The health care provider has indicated concern about the patients acid-base status. The nurse anticipates that the health care provider will determine the acid-base levels via:
a. PaO2 measurement.
b. SaO2 levels.
c. chloride levels.
d. arterial blood gas analysis.
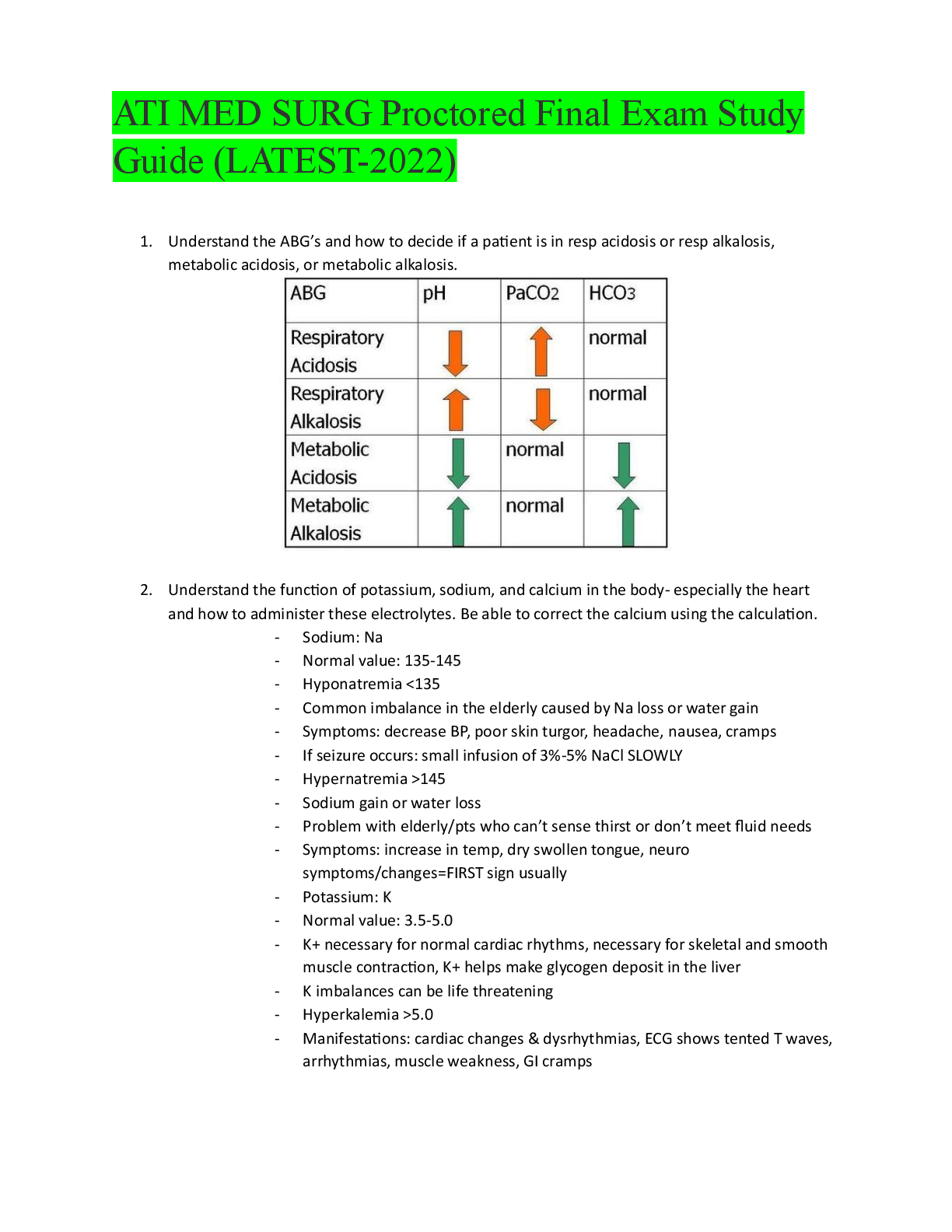
10) Be able to look at labs and distinguish between respiratory acidosis & alkalosis also metabolic acidosis and alkalosis by reading results of arterial blood gases (know the appropriate ranges of arterial blood gases) (TBQ#11, 12 and 13)
a. Respiratory acidosis: is an increased PaCO2 and an increased hydrogen ion concentration (pH below 7.35) that reflects the excess carbonic acid (H2CO3) in the blood.
b. Respiratory alkalosis: is a decrease PaCO2 and increases pH (above 7.45) that reflects the deficit of carbonic acid (H2CO3) in the blood.
c. Metabolic acidosis results from conditions that increase metabolic acids in the body or decrease the amount of base (bicarbonate). The bicarbonate level is always low because the bicarbonate system buffers metabolic acids.
d. Metabolic alkalosis: this results from a gain of bicarbonate or excessive excretion of metabolic acid.
***** Normal arterial blood pH value is 7.35-7.45 (acidic is less than 7.35 and alkalotic is greater than 7.45) *****
A 76-year-old patient is hospitalized with pneumonia and has become increasingly confused throughout the shift. The nurse becomes concerned about the patients condition and contacts the health care provider, who orders arterial blood gas analysis. The blood gas report shows a pH of 7.33, PaCO2 of 47, PaO2 of 78, and bicarbonate of 26. This indicates which imbalance?
a. Respiratory alkalosis
b. Respiratory acidosis
c. Metabolic alkalosis
d. Metabolic acidosis
A patients arterial blood gas levels indicate a pH of 7.51, PaCO2 of 40 mm Hg, PaO2 of 85 mm Hg, and HCO3 of 32 mEq/L. The patient has been vomiting. The nurse knows the patient has which imbalance?
a. Metabolic acidosis
b. Metabolic alkalosis
c. Respiratory acidosis
d. Respiratory alkalosis
A college freshman has bulimia. She vomits after eating and has recently noticed tingling of her fingers and toes and muscle cramps. Her roommate is a nursing student and is concerned about which imbalance?
a. Respiratory acidosis
b. Metabolic acidosis
c. Respiratory alkalosis
d. Metabolic alkalosis
11) What makes the most sense for fluid allotment times for a client with low sodium diet and fluid restriction? (TBQ#18)
a. Between 7am and 3pm. Fluid restrictions often allot half the oral fluids between that time frame. The period when patients are usually more active, receive two meals and take most of their oral medications.
A patient has recently been diagnosed with heart failure and has been put on a low sodium diet in the hospital. In addition, the patient has a fluid restriction. The nurse should suggest that half the total oral fluid allotment occur between which two times?
a. 7 AM; 7 PM
b. 3 AM; 3 PM
c. 7 AM; 3 PM
d. 3 PM; 7 AM
12) What is the best method to administer nutrition for a client with no bowel sounds? (TBQ#19)
a. Parenteral nutrition is a nutritionally adequate solution that consist of glucose, other nutrients and electrolytes that is administered through a central venous catheter. This is the best method to use because it meets nutritional needs when the GI tract is nonfunctional.
The patient is unable to eat and there are no bowel sounds, indicating that his bowels are not functioning. The best approach to providing nourishment would be:
a. intravenous crystalloids.
b. blood product administration.
c. parenteral nutrition (PN).
d. colloid administration.
13) Know when it is appropriate to administer an implanted port, peripheral IV catheter, central line or a peripherally inserted central catheter (TB Q#21)
a. Implanted port: Long term use
b. Peripheral IV catheter: Short-term use (i.e to restore fluid volume)
c. Central Line: Long-term use
d. Peripherally inserted central catheter: Long-term use
A 15-year-old adolescent has been recently diagnosed with cancer. The patient will be receiving IV chemotherapy for several weeks. Which vascular access device should be used for short-term administration of his IV fluid?
a. Implanted port
b. Peripherally placed IV catheter
c. Central line
d. Peripherally inserted central catheter
14) Know the steps to starting a peripheral intravenous catheter
a.
15) Know the signs of phlebitis, infiltration, thrombophlebitis, and local inflammation (TBQ#24)
a. Phlebitis: inflammation of the vein. Redness, tenderness and warmth along the course of the vein starting at the access site with possibly a red streak and/or palpable cord along the vein.
b. Infiltration: causes swelling (from increases interstitial fluid), paleness and coolness (from decreased circulation) around the venipuncture site.
c. Thrombophlebitis: blood clots
d. Local inflammation: redness and/or edema, exudate can occur
During a clinical rotation at an orthopedic unit, a nursing student is caring for a 67-year-old patient who has undergone a knee replacement. The patient is complaining of pain at the IV site. The nursing student assesses the site and finds that the site is cool and pale. The student stops the IV and reports the situation to the nurse. What does the nursing student suspect?
a. Phlebitis
b. Infiltration
c. Thrombophlebitis
d. Local inflammation
A patient has a peripheral IV. The nurse should assess the IV site for what primary signs and
symptoms of infiltration? (Select all that apply.)
a. Redness
b. Swelling
c. Pallor
d. Warmth
e. Red streaks
16) Know the procedure when experiencing a blood transfusion reaction and also if the nurse wants to keep the access open (TBQ#26)
a. When experiencing a blood transfusion reaction the nurse should remove the blood component and tubing containing the blood product and replace it with new primed tubing with a container od 0.9% sodium chloride (normal saline). Connect the tube to the hub of the IV catheter. Do not turn off the blood and simply turn on the normal saline that is connected to the Y-tubing infusion set.
The nurse suspects that the patient is experiencing a blood transfusion reaction. The nurse stops the infusion but is concerned about losing the IV line if blood clots in the catheter. The nurse should:
a. replace the entire transfusion line with a new set primed with normal saline.
b. turn off the blood and turn on the normal saline infusion to flush the tubing.
c. discontinue the IV and start a new IV of lactated Ringers in the other extremity.
d. maintain the patency of the current IV line by hanging a new IV bag of D5W.
A patient complains of chills, dizziness, and feeling hot during a blood transfusion. What are the nurses most appropriate actions? (Select all that apply.)
a. Check the patients vital signs.
b. Stop the blood transfusion.
c. Slow the rate of infusion.
d. Notify the physician and blood bank.
CHAPTER 37
17) Know the difference between reactive hyperemia, blanchable-hyperemia, nonblanchable hyperemia and tissue ischemia (TBQ#1)
a. Hyperemia: blanches; it is redness of the skin resulting from dilation of the superficial capillaries.
b. Blanchable-hyperemia: red area appears warm and will turn lighter in color (blanch) following a fingertip palpation.
c. Nonblanchable hyperemia: redness that persists after palpation indicating tissue damage
d. Tissue Ischemia: decreased blood flow to tissues that result in the death of tissues which occur when capillary blood flow is obstructed from pressure
An elderly patient is admitted to the hospital for a bowel obstruction. The patient is immobile and the nurse notices that there is a reddened area on the right heel. When the nurse presses on the area it does not turn lighter in color. How should the nurse document the tissue condition?
a. Reactive hyperemia
b. Blanchable hyperemia
c. Nonblanchable hyperemia
d. Tissue ischemia
18) Know the difference between friction and shear on the skin, also tunneling and moisture effects (TBQ#2)
a. Friction: damage of the surface caused by the skin rubbing against another surface resulting in abrasion.
b. Shear: when force is exerted against the skin while the skin remains stationary and the bony structures move.
c. Tunneling: deep tissue destruction resulting in larger pockets of necrotic tissue beneath the opening of the main wound. It resembles a tunnel
d. Moisture: increases the risk for ulcer formation as it softens the skin and reduces its resistance to other physical factors.
The student nurse asks a nursing assistive personnel (NAP) to help move a patient up in bed. The student nurse instructs the NAP to position the patient in bed to avoid which of the following factors that would contribute to pressure ulcer formation?
a. Friction
b. Shear
c. Moisture
d. Tunneling
On admission a patient is noted to have an alteration in skin integrity on the right heel. The nurse uses the Braden Scale. Which areas will the nurse assess when using this scale? (Select all that apply.)
a. Mobility
b. Nutrition
c. Infection
d. Friction and shear
e. Sensory perception
19) What factors could put a client at risk for pressure ulcers (TBQ#3)
a. Having a poor nutrition can cause soft tissue to become susceptible to breakdown
An elderly patient has been admitted to the hospital for pneumonia. Which factor could put this patient at risk for a pressure ulcer?
a. A diet low in protein
b. Braden Scale results of 22
c. Primary health care provider orders that read activity as tolerated
d. Being repositioned every 2 hours
20) What parameters are assessed when doing a wound assessment? (TBQ#2 select all that apply)
a. Anatomical location
b. extent of tissue involvement (full or partial thickness)
c. size (dimensions and depth of wound)
d. tissue type (viable or nonviable)
e. volume and color of wound exudate
f. condition of the surrounding skin
A pre-teen quadriplegic patient was admitted with pressure ulcers to both ankles. The nurse should assess which parameters for a wound assessment? (Select all that apply.)
a. Size
b. Viable versus nonviable tissue
c. Tissue type involvement
d. Preventive measures
e. Anatomical location
...................Continued
[Show More]