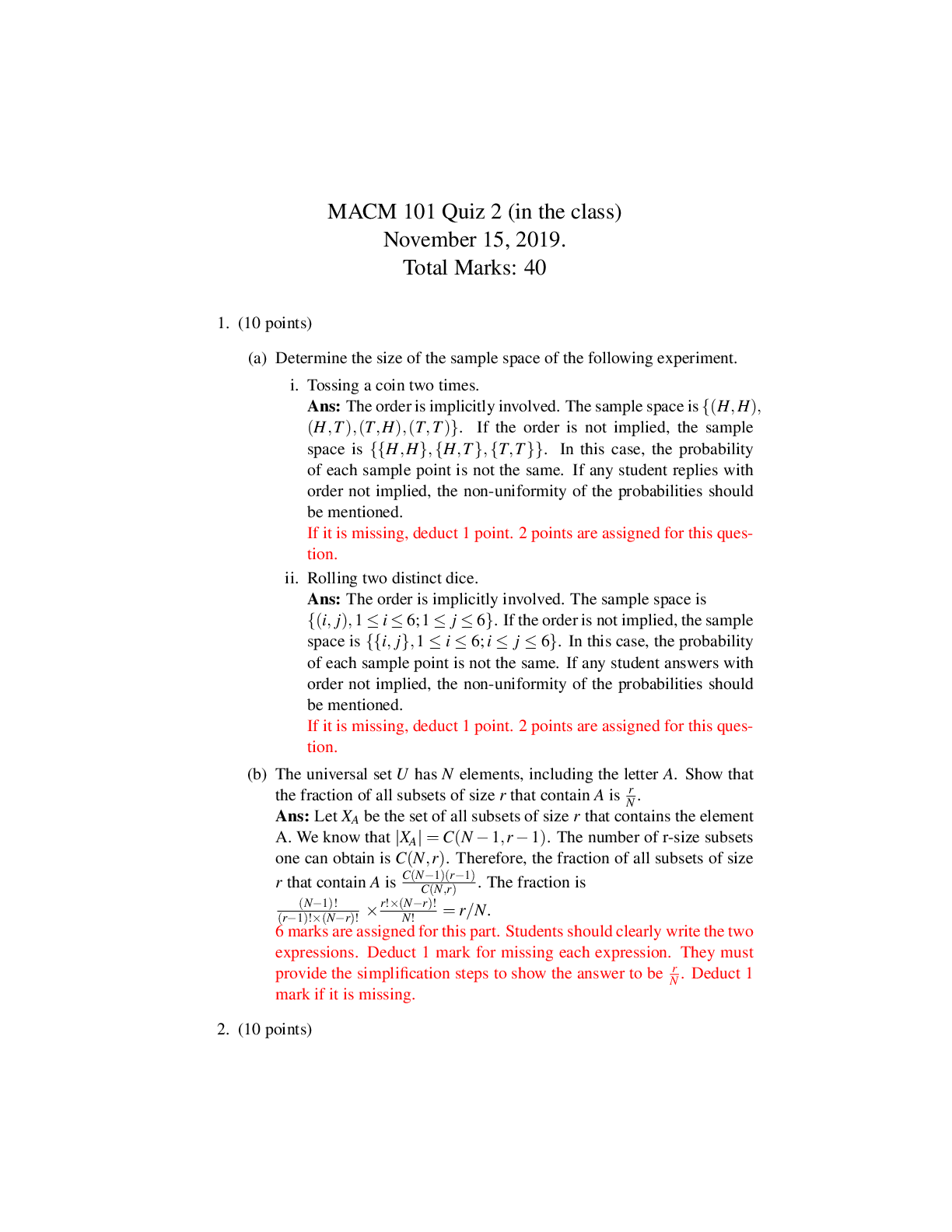
NUR 335 Exam 1 Guide
Math
1.Basic dosage
Desired/Available * Quantity
2.Formula: IV DROP Rate
Volume (mL)
Time (min)
x Drop Factor (gtts/mL) = Y (Flow Rate in gtts/min)
Example: Calculate the IV flow rate for 120
...
NUR 335 Exam 1 Guide
Math
1.Basic dosage
Desired/Available * Quantity
2.Formula: IV DROP Rate
Volume (mL)
Time (min)
x Drop Factor (gtts/mL) = Y (Flow Rate in gtts/min)
Example: Calculate the IV flow rate for 1200 mL of NS to be infused in 6 hours. The infusion set
is calibrated for a drop factor of 15 gtts/mL.
Volume (mL)
Time (min)
x Drop Factor (gtts/mL) = Y (Flow Rate in gtts/min)
Convert 6 hours to minutes.
min ← hr ( x by 60 )
6 hr x 60 = 360 min
1200 mL
360 min
x 15 gtts/mL = 50 gtts/min
3. Formula: IV ml rate
Ordered Per Hour
Have
x Volume (mL) = Y (Flow Rate in mL/hr)
Example: Give patient 500 mg of dopamine in 250 mL of D5W to infuse at 20 mg/hr. Calculate
the flow rate in mL/hr.
Ordered Per Hour
Have
x Volume (mL) = Y (Flow Rate in mL/hr)
20 mg/hr
500 mg
x 250 mL = 10 mL/hr
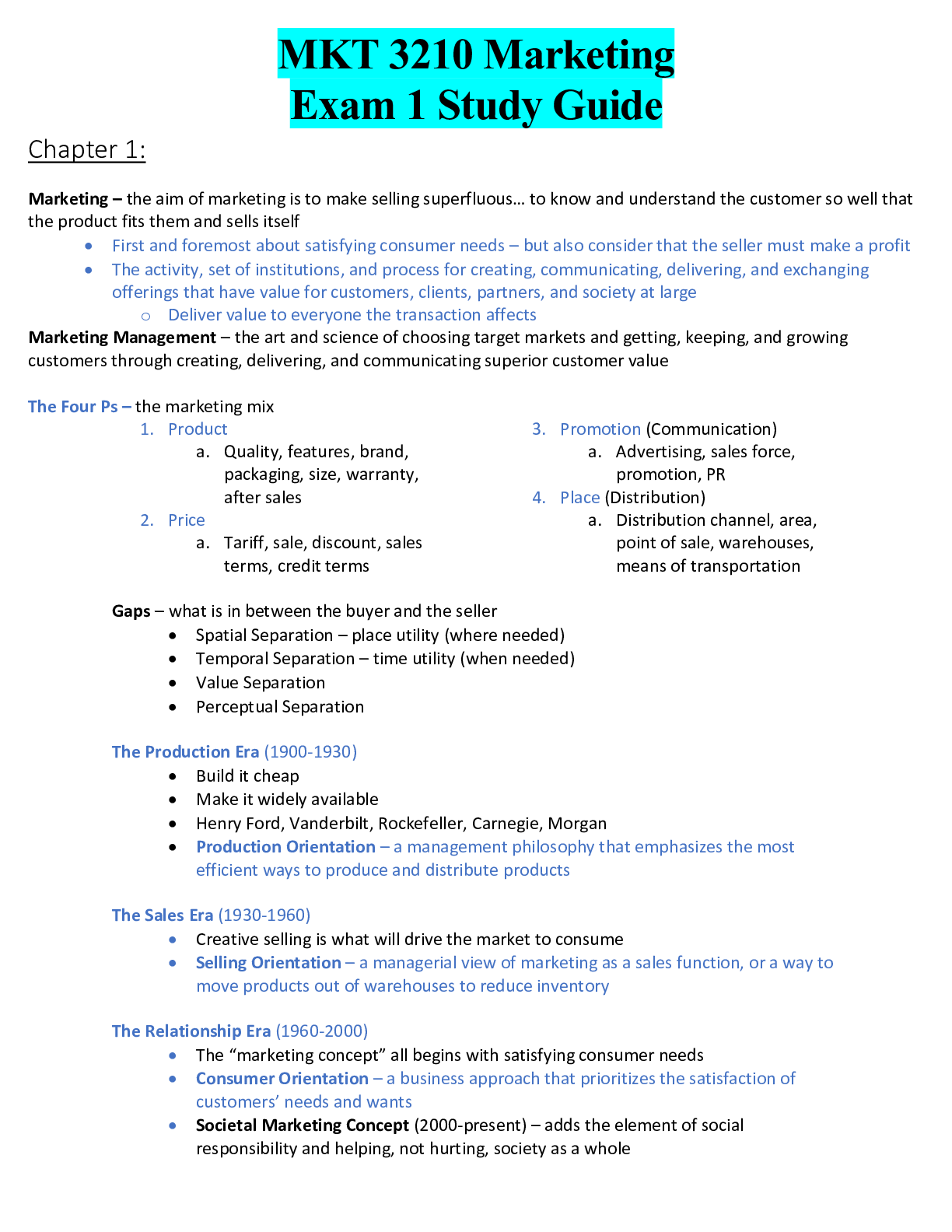
Chapter 1
****The nursing process includes assessment, diagnosis, planning, implementation, and
evaluation
A nurses number one job is to make sure the patient and their family understands treatment plans
and discharge teachingDomains of Nursing Practice for Medical-Surgical Nursing
Certification
1. Helping Role
2. Teaching-Coaching Function
3. Diagnostic and Patient Monitoring
4. Effective Management of Rapidly Changing Situations
5. Administering and Monitoring Therapeutic Interventions and Regimens
6. Monitoring and Ensuring the Quality of Healthcare Practices
7. Organizational and Work Role Competencies
Steps of Evidence-Based Practice
1. Develop the question.
2. Search and collate the best evidence.
3. Evaluate the quality of the evidence.
4. Integrate evidence into practice.
5. Evaluate outcomes of practice change.
6. Disseminate the evidence.
Evaluating Levels of Evidence
1. Level I Evidence from systematic reviews of randomized controlled studies (RCTs)
2. Level II Evidence from at least one RCT
3. Level III Evidence from quasi-experimental studies
4. Level IV Evidence from case-control and cohort studies
5. Level V Evidence from systematic reviews of descriptive or qualitative studies
6. Level VI Evidence from a single descriptive or qualitative study
7. Level VII Evidence from expert individual authorities or committees
National Patient Safety Goals
1. Identify patients correctly
2. Improve staff communication
3. Use medicines safely
4. Use alarms safely
5. Prevent infection
6. Identify patient safety risks
7. Prevent mistakes in surgery
The SBAR Approach for Effective Communication
SBAR is an acronym that correlates to:
Situation: Brief statement of the problem or issue being addressed
EX: Hello, Dr. Jones. This is Steve, the registered nurse caring for Ms. Sandra Williams in
Room 732 on South Wing. I am contacting you because she arrived from the post-anesthesia
care unit (PACU) and has not voided in more than 6 hours. Vitals will be here also
Background: Data related to the current situation
EX: She was admitted to the hospital this morning, and you performed a lumbar laminectomy
this morning for a herniated disc at L4–L5.Assessment: Summary of causes, significance, severity of situation
EX:Ms. Williams is complaining of inability to void. According to her operative reports, she
received 1,500 mL of IV fluid during the surgical procedure and in the PACU, and the
indwelling catheter was removed prior to transfer from the PACU 6 hours ago; at the time, she
had 800 mL of urine output. She has received an additional 250 mL of IV fluid since arriving on
the unit.
Recommendation: Specific actions needed to address the situation
EX: I recommend that an intermittent catheterization be performed at this time.
Interprofessional practice
1. Provides patient centered care
2. Work in interdisciplinary teams
3. Employ evidence-based practice
4. Apply quality improvement
5. Utilize informatics
Interprofessional collaboration
Partnership between a healthcare team and the client to make decisions around health and social
Issues
ADPIE
Assessment
Diagnosis
Planning
Implementation
Evaluating
Patient centered care
Effective communication skills
Empathy
Caring
Compassion
Hospital Consumer Assessment of Healthcare Providers and Systems (H C A H P S)
The Joint Commission (T J C)
The Beryl Institute
****Treating patients and families with dignity and respect
Involving patients and families in decision making
Quality and Safety Education for Nurses (Q S E N)
Patient-Centered Care
Teamwork and Collaboration
Evidence-Based Practice (E B P)
Quality Improvement (Q I)
SafetyInformatics
****In medical surgical nursing your biggest responsibility is to make sure your patient
understands an procedure and they understand their discharge teaching
****The nurse has to have empathy, be caring, and have compassion
Chapter 15
Use 18g for IV blood products
Always make sure you have consent for everything consent is your biggest responsibility
(Surgeon gets consent)
Make sure patient understands the procedure and everything that follows. Make sure that the patient
has no questions
(Nurses responsibility)
They need to know the doctors name
Informed Consent
Components include:
Consent for procedure itself
Name of surgeon to perform surgery
Reason intervention will benefit the patient
Alternative options to surgery
Consent for anesthesia
Consent to administer blood products
***Although obtaining consent is not the role of the nurse but that of the provider, it is the
nurse’s responsibility to ensure that the patient has all the information needed to make an
informed decision about the procedure being offered
Obtaining Consent
The role of the surgeon is to obtain consent for the procedure. The surgeon is solely responsible
for obtaining consent in the presence of the patient and one witness.
The role of the preoperative nurse is to clarify information and ensure patient understanding.
Nurses correct common misconceptions and ease concerns of the patient, family members, or
support persons
Advanced Directives
Defines patient’s wishes
Name a power of attorney
SurgeryCorrect patient
Correct procedure
Correct Surgical Site
*** Always remember my right may be your left and your left may be my right she make sure
your on the correct side
Always assess patients
Their medical history is important( always ask about bleeding problems)
Make sure patients has understanding of how to use assistant devices incase needed
Surgical and anesthesia history
Do you have poor healing, any pervious surgeries, negative responds to anesthesia, or any
allergies
***If allergies put on alert bracelet
Last oral intake
Guidelines dependent upon institution and population
Full stomach increases risk for aspiration
***A patient who has eaten within 8 hours is at risk of aspiration, the introduction of food particles into
the lungs through emesis
***According to recent guidelines for elective procedures, the patient may be advised to be NPO 6 to 8
hours for solid foods and 2 hours for clear fluids.
Physical preparations
Intravenous line
An IV line is inserted during the preoperative admission, typically for the purpose of the
administration of anesthesia and fluids during the surgery. An 18-gauge catheter is preferred
because this size is required for the administration of all blood products.
Bowel and bladder preparation
Patients receiving abdominal, intestinal, gynecological, or rectal surgery may be asked to
perform a bowel preparation. This may be done by use of an enema or gentle laxatives that the
patient self-administers at home the night before the procedure. The nurse should confirm and
document that this preparation has been performed. Patients scheduled for abdominal,
gynecological, or long procedures may also require the insertion of an indwelling catheter to
drain urine. This will keep the bladder empty during a procedure, preventing injury to the
bladder. It also allows the surgical team to monitor output in the operating room and PACU.
Skin preparation
Prior to surgery, skin preparation is done to help prevent infection at the surgical site. Patients
may be instructed to shower and wash with Betadine or hexachlorophene soap prior to
admission. A surgical shave may be necessary depending on the patient’s skin type and the
location of the incision. If a shave is appropriate, the nurse uses a sterile electric clipper. A razor
is not recommended because of the risk of infection caused by small nicks in the skin that may
occur with a razor.
Medications
Preoperative medications may be required. Patients with preoperative anxiety may be prescribed
a benzodiazepine such as midazolam HCl, diazepam, or lorazepam. Antiemetics such asmetoclopramide HCl or ondansetron HCl may be used preoperatively if a patient has a history of
nausea and vomiting due to anesthesia.
Medications
You need to know if the patient takes any medications or herbal medications
3’G’s Ginger. Ginkgo Biloba, Garlic
Taking anticoagulants
Priority assessments
Cardiovascular
Respiratory
Integumentary
Priority labs
CBC
PTT/INR
You want to try to prevent DVT (DVT Prophylaxis)- Sequential compression devices
Prevent Pneumonia- Incentive Spirometer(Inhale than breathe out) use at least 10 in an hour
Also do deep breathing and coughing
Always remove jewelry and prosthetics before surgery
****Patient teaching is very important they should verbalize and demonstrate their
understanding
Chapter 16
Impatient- Require close monitoring and recovery more than 24 hours after completion
Same day- Require less than 24 hours of monitored recovery
Elective Surgery- The patient Chooses
Urgent Surgery- May not be up to the patient
***The patient has the right to deny any produce
Table 16.1 Suffixes for Surgical Procedures
Suffix Meaning Examples
-centesis Puncture Amniocentesis, thoracentesis
-ectomy Removal Cholecystectomy, hysterectomy
-lysis Destruction Electrolysis
-oscopsy View with scope Arthroscopy, endoscopy***Make sure the patient understands and consents to everything
Sterile team members
Surgeon
Surgical assistants
Scrub nurse or surgical technologist
Nonsterile team members
Anesthesia provider
Circulating R N
Unlicensed assistive personnel
O R director/coordinator/manager
Surgical pause
Correct patient
Correct procedure
Correct surgeon
Correct position
Correct equipment
Correct imaging studies
Hand Washing
Scrub hands for 3-5 min
Remove jewelry
Make sure nails are cut, short, and clean
Donning
Hand hygiene
Gown
Mask
Goggles
Gloves
Removing
Gloves
Goggles
Gown
Mask
Hand hygiene
-ostomy Create an opening Colostomy, ileostomy
-otomy Incision Episiotomy, tracheotomy
-plasty To reshape or repair Abdominoplasty, mammoplasty***Everything has to be above the waist to be sterile
General anesthesia
Being put to sleep
Reversible unconscious state
Variety of methodologies
Volatile agents
I V agents
Muscle relaxants
Complications
Hypoxia(Low oxygen)
Hypotension(low blood pressure)
Hypertension(High blood pressure)
Residual muscle paralysis(Weakness)
Malignant hyperthermia(fast rise in body temp)
Regional anesthesia
Spinal
Epidural
Caudal
Nerve block
Objectives
Maintenance of consciousness
*Elevation of pain threshold
Enhanced cooperation
Some degree of amnesia
*Minimal variation in vital signs
*Quick and safe return to activities of daily living
Airway management
Protecting and ensuring proper oxygenation and ventilation
Complications:
o Laryngospasm
o Bronchial intubation
o Tracheal and esophageal perforation
o Aspiration
PositionsSupine
Prone
Lateral
Lithotomy
***Patient education is important and making sure family is updatedChapter 6
65-75: young old
75-85: old
Older than 85: old old
Age related changes
Senescence – Normal age-related changes in organ systems
*Sclerosis – Hardening of tissue due to fibrous tissue overgrowth
Stenosis – Narrowing or constricting of a passage or orifice
*Atrophy – Wasting away or decrease in the size of an organ
*Calcification – Calcium and calcium salts are deposited in abnormal locations, like blood
vessels
Risk factors Cardiovascular problems
Stoke
Hypertension
High cholesterol
Diabetes
Smoking
Obesity
Poor Diet
Physical activity
Common Illnesses
Pneumonia – Older adults at higher risk due to decrease in lung’s elastic recoil, weakened cough
reflex, weakened diaphragm strength, and impaired swallowing
Chronic obstructive pulmonary disease – Smoking is greatest risk factor
Dementia – Progressive cognitive decline that affects a person’s social and occupational
functioning
Depression – Difficult to diagnose in older adults and may include low energy levels, difficulty
sleeping, less appetite, aches and pains, difficulty remembering details
Parkinson’s disease – Degenerative condition primarily affecting movement, causing tremor,
rigidity, gait disturbance, and speech disturbance
Cerebrovascular accident – Stroke; vascular disease manifesting as paralysis, weakness, speech
and vision impairment
Episodic memory diminishes with age – Evident in tasks requiring learning and recall of items
that are not meaningful, for example, phone numbers
Free recall diminishes – The ability to recall unrelated words from a list decreasesWorking memory ability decreases – The ability to multitask successfully declines with aging,
along with reduced ability to process complex incoming information
Semantic memory maintained or may increase – Memory of facts and meanings and intellectual
ability are unchanged
Processing speed decreases – If speed is not crucial, information is retrieved as well as in
younger people
Increased risk of dehydration
General decline in bladder function and capacity.
Sexual dysfunction related to hormone decreases, organ atrophy, and decreased sexual fluids
Senses of taste and smell diminish, making food seem less appealing
Premature feelings of fullness leading to malnutrition
Constipation and impaction
Dentition/chewing limiting available foods
Dysphagia leading to aspiration or pocketing of food
***Delirium- Is a quick onset of confusion
***Dementia- Slow and progressive over time
Always ask about medications and what and when are they taking these meds
Polypharmacy- Taking any and everything not really knowing what it is
You want to protect them from abuse and watch for S&S
Ask about their living will and do they have an DNR
Medicaid- Medical coverage to low income families. The state and government share the cost
Medicare- Is very important to elderly. Is a federal program that provides health care to people
65+
Part A(Hospital Insurance) – Covers inpatient hospital stays
Part B(Medical insurance)- Covers doctors services
Part C- Private companies that cover what part A and B don’t
Part D(Prescription)- Covers medication cost
***Some parts some people can’t get
*** When you document you want to watch what you put in when it comes to Medicare
*** Always remember safety is a priority with elderly
***Everything decreases but blood pressure
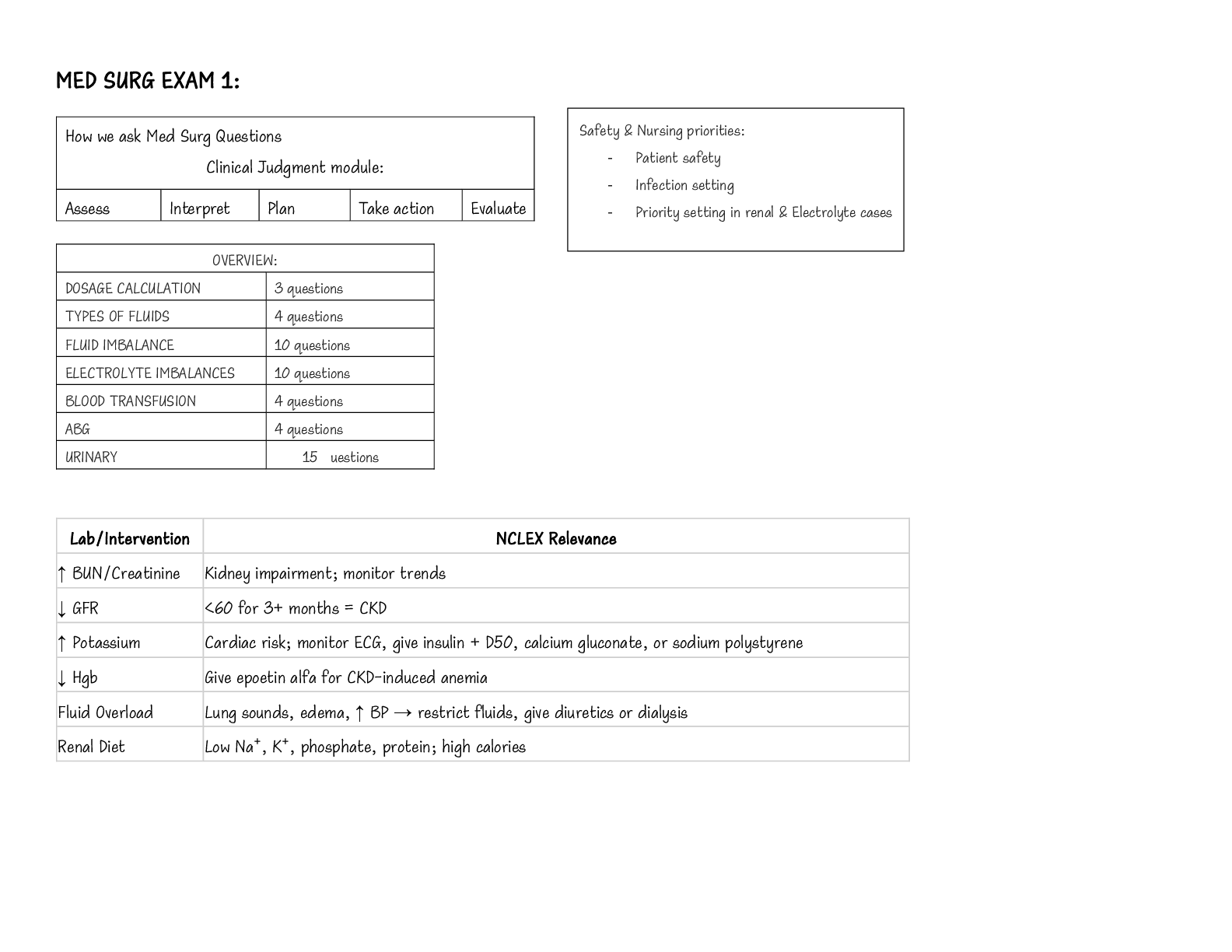
Chapter 8
Intracellular fluid (ICF) – about two thirds by volume, contained in cells
Extracellular fluid (ECF) – consists of two major subdivisions
Plasma – the fluid portion of the blood
Interstitial fluid (IF) – fluid in spaces between cells
2500 ml/ day in so 2500ml/ day out
Whatever the patient takes in it needs to come outUrine output 1500mL / 30ml/hr
Osmosis-Low concentration to high concentration
Diffusion- High concentration to low concentration
Fluid Spacing
First spacing
normal distribution of fluids in the ICF & ECF compartments
Second spacing
abnormal accumulation of interstitial fluid as seen in edema
Third spacing
accumulation of fluid in portions of the body which is not easily exchanged with the rest of the
ECF
Regulates Water Balance
Hypothalamic
Pituitary
Release of ADH
Increase in plasma osmolality or decrease in blood volume will stimulate thirst and the
release of ADH
Signs and Symptoms of Diabetes
Polyuria: LOTS of urine 4L to 24 L per day
Polydipsia: body’s way of trying to keep water in the body….crave water/ice
Dry mucous membranes, dry skin, decrease skin tugor…very dehydrated
Urine diluted….low urinary specific gravity
Hypotension (due to the severe dehydration and remember ADH is responsible for
constricting blood vessels…here the vessel will be dilated which causes hypotension) Extreme fatigue and muscle pain/weakness
Hypernatremic (due to the concentrate sodium in the body from low water levels)
Solutions
Isotonic(NO CHANGE)
No change in the concentration of solute and water in the bloodstream
Osmosis neither moves water into the circulation nor pulls it out.
0.9 NACL ; LR; D5W (functions as hypotonic once glucose is metabolized)
Treatment for ECF deficits – expands ECF volume
Hypotonic(BIG CELLS)
Lower osmolality than blood serum
More water (relative to solute) is being infused than is already present in the vessel and inside
the cells.
Therefore, water moves into the cells
Indicated for hypernatremia and hyperosmolar conditions Replaces cellular fluid & provides free
water
Can cause cerebral edema and Hypotension from intravascular depletion
Contraindicated in edema and third spacing
0.45 NS (1/2 NS) , D5 .45
Hypertonic(SMALL CELLS)
Higher osmolality than blood serum
Osmosis pulls water out of the cells
Cell shrinkage
Increased osmolality of ECF - expands it
Indications: Hyponatremia
3% NACL, D10W, D50W
Plasma Volume Expanders
Stays in the intravascular compartment and increases oncotic pressure
Colloids
Protein solutions - albumin (5% or 25%)
Synthetic molecules - Dextran, Hespan (Hetastarch)
Whole blood or packed red blood cells [PRBCs]
**Indicated for fluid losses from ECF (hemorrhage or sepsis)
Edema(Swelling)2mm or less = +1
Slight pitting, No visible distortion, Disappears rapidly
2-4mm = +2
Somewhat deeper pit, No readably detectable distortion, Disappears in 10-15 seconds
4-6mm = +3
Pit is noticeably deep, May last more than 1 minute, Dependent extremity looks fuller and swollen (4-
6mm)
6-8mm = +4
Pit is very deep, Lasts as long as 2-5 minutes, Dependent extremity is grossly distorted (6-8mm)
Daily Weight
Single most important measurement for fluid volume status
Same time, same scale, same clothing
1L = 1kg = 2.2lbs
1 L (2.2 lbs) = 1 liter of fluid (lost or retained)
Hypervolemia( increased water and sodium)
Causes
Increased water and sodium retention
Cirrhosis
Heart failure
Stress conditions
Use of corticosteroids
Sodium intake
Clinical manifestations
Weight gain
Ascites
Edema
Increased urine output
Cardiac symptoms
Respiratory symptoms
Medical management
Correcting and managing underlying cause
Treating clinical manifestations Fluid restriction
Discontinue I V fluids
Diuretics
Dialysis( to remove fluid out of body)
Complications
Pulmonary edema
Nursing management
Collecting health history
Physical assessment
Reviewing laboratory data
Monitoring weight
Calculating I&O
Hypovolemia
Order 0.9 NaCI
Laboratory values
Electrolytes
Hemoglobin and hematocrit
Serum osmolality
BUN and creatinine
Urine specific gravity
Urine osmolality
Clinical manifestations
Weight loss
Decreased skin turgor
Concentrated urine output
Oliguria<30 mL per hour
Thirst
Dry mucous membranes
Medical management
Identify and treat cause
Intake of oral fluids
IV isotonic solutions Close monitoring
Complications
Hypovolemic shock
Hypotensin
Tachycardia
Signs of organ hypoperfusion
Nursing management
Collection of health history
Physical assessment
Vital signs
Mucous membranes, skin turgor
Urine specific gravity, color, volume
I&O
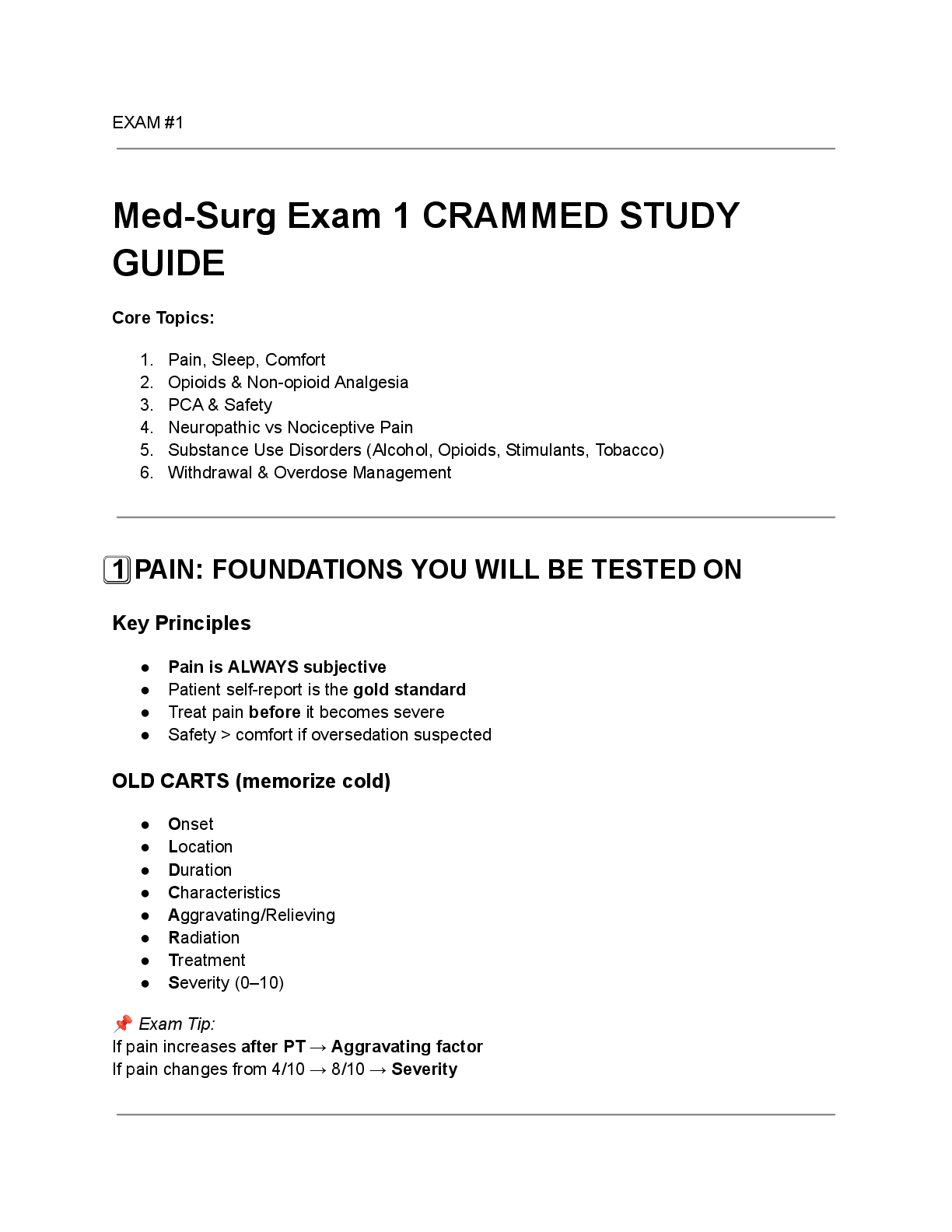
Sodium 135-145
Hyponatremia(low sodium)
Causes
Medications (diuretics)
Diarrhea or vomiting
Hyperglycemia with glucosuria
Perspiration
S I A D H Hypothyroidism
Adrenal insufficiency
Psychotic polydipsia
Heart failure
Cirrhosis
Nephrotic syndrome
Clinical manifestations
Related to cerebral edema and neurological decline, Lethargy, Headache, Confusion, Gait
disorders, Nausea and vomiting, Seizure, coma, permanent brain damage, death if not treated
Nursing management
Monitor I&O, Ensuring adequate water intake, Monitor daily weight, Monitor serum sodium,
patient education
Complications
Lethargy, Confusion, Weakness, Fatigue, Muscle cramps, Postural hypotension, Severe: Seizure,
coma, death
: Replacement of sodium, Oral, enteral, parenteral, Fluid restriction, Hypertonic saline if neuro
involvement
Diuretics.
Hypernatremia(High Sodium)
Causes
Reduced water intake
Limited ability to express thirst
Diabetes insipidus
Hyperglycemia
Neoplasms
Hypercalcemia
Hyperkalemia
Medications
Clinical manifestations
Nonspecific neurological changes
Neuromuscular irritability, agitation, restlessness, lethargy, coma, seizure
Severe: hallucinations, delusions, disorientation
Thirst Signs of dehydration
Medical management
Limiting sodium intake
Replacing water deficits
Complications
Restlessness
Weakness
Disorientation
Delusions
Hallucinations
Severe: Seizures, stupor, coma, death
Nursing management
Monitor I&O
Ensuring adequate water intake
Monitor daily weight
Monitor serum sodium
Potassium 3.5-5.0
Hypokalemia(low potassium)
Clinical manifestations
Weakness
Lethargy
Hyporeflexia
Nausea/vomiting
Constipation
Abdominal cramping
Electrocardiogram changes: ST depression
Severe: Cardiac or respiratory arrest
Medical management
Potassium supplementation
Cardiac monitoring
Intravenous access
Complications
Muscle weakness and cramping
Decreased G I motility
Cardiac dysrhythmias
Respiratory failure
Cardiac or respiratory arrest
Death
Nursing management
Assessment
Monitor digitalis levels if applicable
Patient education
Administer potassium replacement***Needs to be on telemetry floor
They have ventricular dysrhythmias > Ventricular fibrillation
Never push Potassium
Hyperkalemia(To much potassium)
Clinical manifestations
Generalized fatigue
Muscle cramps
Palpitations
Paresthesias
Weakness
E C G changes
Cardiac arrest
Medical management
Obtain E C G
Serial serum potassium levels, Loop diuretics
Dialysis
Dietary modification
Correction of metabolic acidosis
Complications
Nausea and diarrhea
Muscle weakness
Cardiac dysrhythmias
Cardiac arrest
DeathNursing management
Assessment
Monitoring and reporting lab values
Continuous cardiac monitoring and
E C G
Administer medications as ordered
Patient education
*** T wave peak, ST depression, QT shorten
Calcium 8.2-10.2
Positive Trousseau sign. With inflation of the blood pressure cuff, the fingers go into carpal
spasm, indicating hypocalcemia.
Chvostek sign. Tapping over the facial nerve leads to twitching of the face related to
hyperexcitability of the neuromuscular junction due to hypocalcemia.
Hypocalcemia(To little Calcium) Less than 6.5
Clinical manifestations
Excitability of nerves and muscles
Smooth muscle spasms Prolonged Q T interval
Decreased myocardial contractility
Anxiety, confusion, irritability
Positive Trousseau and Chvostek sign
Medical management
Protection and maintenance of airway
Cardiac monitoring
I V access
I V replacement of calcium
Treat other electrolyte abnormalities, especially magnesium
Oral calcium and vitamin D supplements
Complications
Cardiovascular collapse
Refractory hypotension
Laryngospasm
Dysrhythmias
Decompensated heart failure
Nursing management
Assessment
Maintain access to emergency equipment
Seizure precautions
Maintain quiet environment
Patient education
Encourage smoking cessation
Encourage limiting caffeine and alcohol
*** Use calcium gluconate with D5W/ 0.5mg/kg/hr IV IN D5W
*** Re-evaluation of serum calcium levels should be done every 4 to 6 hours during replacement
therapy to prevent hypercalcemia
Hypercalcemia(To much Calcium)
Clinical manifestations Bradycardia, Hypertension
Thirst, Lethargy
Muscle weakness and soreness, Abdominal discomfort
Constipation, Decreased deep tendon reflexes, Anorexia, Nausea, vomiting
Lethargy, Confusion, Renal calculi and renal failure, bone pain
Medical management
Stabilization and reduction of calcium levels
Hydration with 0.9% NaCl
Dialysis
I V biphosphates
Calcitonin
Treatment of malignancy
Removal of parathyroid gland
Complications
Cardiac rhythm changes
T-wave changes
Heart block
Cardiac arrest
Confusion
Lethargy
Coma
Nursing management
Assessment and monitoring
Cardiac rhythm
Mental status
Encourage early and frequent ambulation
Encourage hydration
*** Number one thing they present with is Joint and bone pain
*** You give 0.9% NaCI
*** They need lots of fluids to rid the body of the extra calcium
***Maintain urine output 100-150ml/hr
*** Doctor will order Bisphosphates
Extra Notes
****Remember BMP is Basic Metabolic PanelEKG Wave
CBC Values
WBC 4,500-11,000
PLT -140,000-450,000
RBC- Male 4.5-5.5
Female 4-4.9
Hgb- Male 13.5- 16.5
Female 12-15
HCT- Male 41- 50
Female 36-44
Other levels
Mg- 1.6-2.2
Cl- 97- 107
P- 2.5-4.5
ABG’s (Arterial Blood Gas)
[Show More]