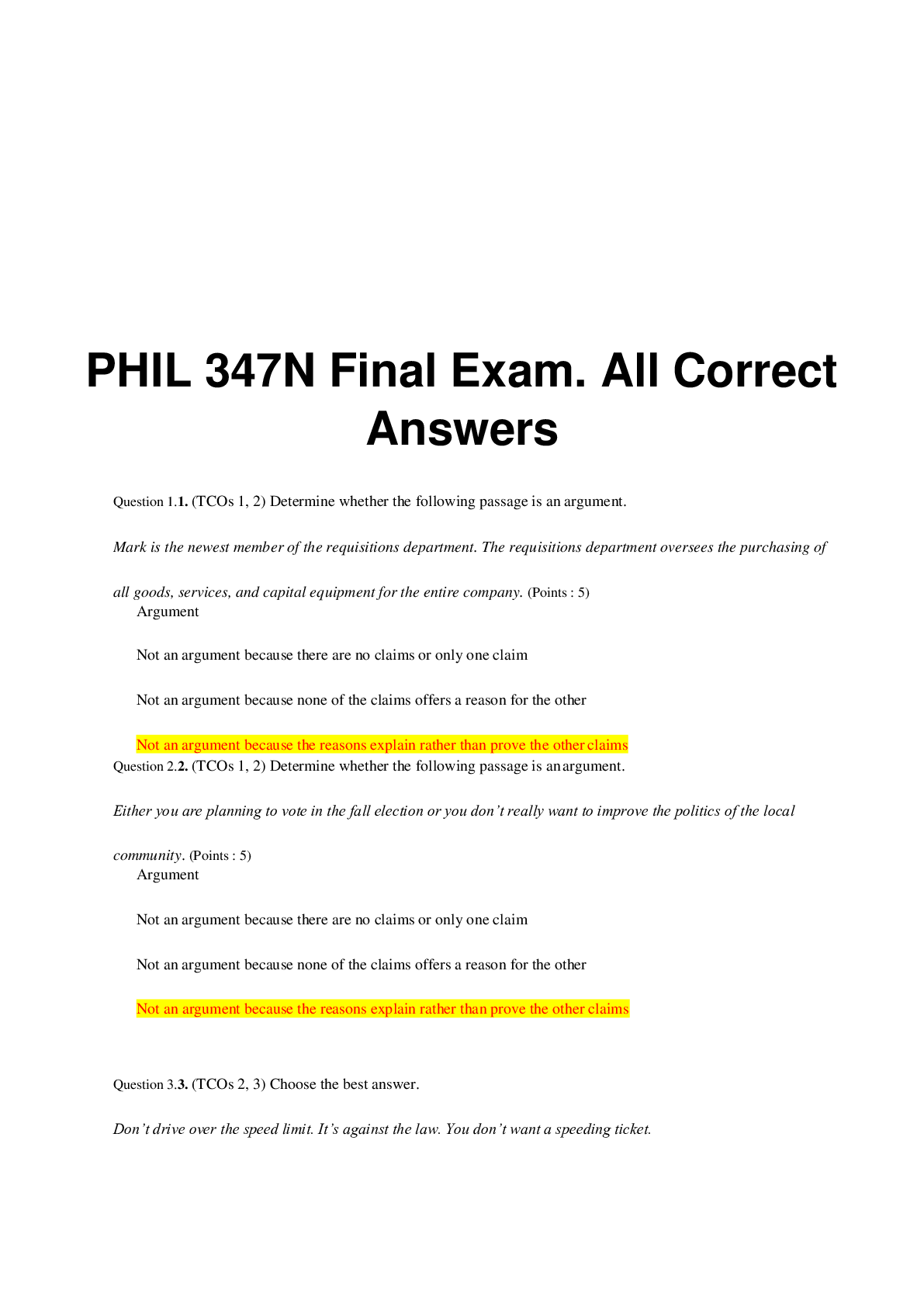
*NURSING > QUESTIONS & ANSWERS > Chamberlain College of Nursing - PATHOPHYSI NR 507WK2TD3: Week 2: Respiratory Disorders and Alterati (All)
Chamberlain College of Nursing - PATHOPHYSI NR 507WK2TD3: Week 2: Respiratory Disorders and Alterations in Acid/Base Balance, Fluid and Electrolytes - Discussion Part Three. (All Grade A Content. Thread)
Document Content and Description Below
Week 2: Respiratory Disorders and Alterations in Acid/Base Balance, Fluid and Electrolytes - Discussion Part Three Loading... This week's graded topics relate to the following Course Outcomes (COs)... . Analyze pathophysiologic mechanisms associated with selected disease states. (PO 1) Differentiate the epidemiology, etiology, developmental considerations, pathogenesis, and clinical and laboratory manifestations of specific disease processes. (PO 1) Examine the way in which homeostatic, adaptive, and compensatory physiological mechanisms can be supported and/or altered through specific therapeutic interventions. (PO 1, 7) Distinguish risk factors associated with selected disease states. (PO 1) Describe outcomes of disruptive or alterations in specific physiologic processes. (PO 1) Distinguish risk factors associated with selected disease states. (PO 1) Explore age-specific and developmental alterations in physiologic and disease states. (PO 1, 4) iscussion Part Three (graded) A nursing student comes into your office because they are struggling with the concept of Week 2: Respiratory Disorders and Alterations in Acid/Base Balance, Fluid and Electrolytes - Discussion Part Three Loading... This week's graded topics relate to the following Course Outcomes (COs). Analyze pathophysiologic mechanisms associated with selected disease states. (PO 1) Differentiate the epidemiology, etiology, developmental considerations, pathogenesis, and clinical and laboratory manifestations of specific disease processes. (PO 1) Examine the way in which homeostatic, adaptive, and compensatory physiological mechanisms can be supported and/or altered through specific therapeutic interventions. (PO 1, 7) Distinguish risk factors associated with selected disease states. (PO 1) Describe outcomes of disruptive or alterations in specific physiologic processes. (PO 1) Distinguish risk factors associated with selected disease states. (PO 1) Explore age-specific and developmental alterations in physiologic and disease states. (PO 1, 4) Discussion Part Three (graded) Topic Print View http://threadcontent.next.ecollege.com/(NEXT(9e2c2ee14f09456db4bdd... 1 of 27 5/16/2016 10:53 PMpulmonary function. They know you as an experienced FNP and so they are comfortable asking if you could clarify the terms residual volume (RV), functional reserve capacity (FRC), total lung capacity (TLC) inspiratory reserve volume (IRV), and expiratory reserve volume (ERV). Give her a definition of each? List three (3) disorders that can alter the residual volume and explain how they do so? Residual volume (RV) – The amount of air that remains in the lungs after maximum expiratory exertion. This amount cannot be measured. It is, however, calculated from the FRC -ERC (Daniels, 2014). Functional reserve capacity (FRC) - The volume of air that stays in the lungs after normal expiration (Daniels, 2014). Total lung capacity (TLC) - Total amount of air the lungs can hold after maximal inspiration (Daniels, 2014). Inspiratory reserve volume (IRV) - The maximum amount of air inhaled at the point of maximum expiration (Daniels, 2014). Expiratory reserve volume (ERV) – Maximum amount of air exhaled at a slow pace at the point of maximum inspiration (Daniels, 2014). List three (3) disorders that can alter the residual volume and explain how they do so? Asthma – Gould and Dyer (2011) – tell us that when exploring asthma and it’s symptoms, there is a partial obstruction in the small bronchi and bronchioles that result in air trapping and hyperinflation of the lungs. The air passes through into the areas distal to the obstruction and the alveoli, but this is only partially expired. Expiration is a passive process and because it is there is less force available to move the air out. The forced expiration will often collapse the bronchial wall, and this creates a further inability for the expiratory airflow. The residual volume increases which make it more difficult to take in fresh air or a cough with enough force to remove the mucus. When there is total obstruction mucus will block the air that is already in a narrowed passage. This condition will lead to atelectasis or an inability to aerate the tissue that is distal from the STAT!Ref Online Electronic Medical Library. http://online.statref.com.proxy.chamberlain.edu:8080/Document.aspx?fxId=59& docId=462. 5/12/2016 8:53:38 AM CDT (UTC -05:00). Gould, B. E., & Dyer, R. (2011). Respiratory disorders. In Pathophysiology for the health professions (4th ed., p. 352, 358, 359). St. Louis, MO: Saunders/Elsevier. McCance, K. L. & Huether, S. E., (2014). Alterations of pulmonary function. In Brashers, V. L (Ed.), Pathophysiology: The biologic basis for disease in adults and children (7th ed., pp. 1258, 1267). St. Louis, MO: Mosby List three (3) disorders that can alter the residual volume and explain how they do so? Pulmonary hyperinflation occurs due to the decreased elasticity of the lung parenchyma, increased airway resistance, and air trapping, as chronic obstructive pulmonary disease (COPD) progresses. In COPD with emphysema, the lung recoil pressure is further reduced by a reduced elastic load related to smoking or α1-antitrypsin deficiency (Gagnon, 2014). References Chamberlain College of Nursing. (2016). NR-507 Week 2: Respiratory disorders and alterations in acid-base, fluid balance, and electrolytes [Online lesson]. Downers Grove, IL: DeVry Education Group. Gagnon, P., Guenette, J. A., Langer, D., Laviolette, L., Maninguy, V., Maltais, F.,…Saev. D. (2014). Pathogenesis of hyperinflation in chronic obstructive pulmonary disease. International Journal of Chronic Obstructive Pulmonary Disease, 9. doi: 10.2147/COPD.S38934 Johnson, J. D. & Theurer, W. M. (2014). A stepwise approach to the interpretation of pulmonary function tests. American Family Physician, 89(5). Retrieved from http://www.aafp.org/afp/2014/0301/p359.html Selvi, C., Rao, K. K., & Malathi. (2013). Should the functional residual capacity be ignored? Journal of Clinical & Diagnostic Research, 7(1). doi: 10.7860/JCDR/2012/4876.2666 Shin, T. R., Oh, Y., Park, J. H., Lee, K. S., Oh, S., Ryoung, D.,…Lee, S. D. (2015). The prognostic value of residual volume/total lung capacity in patients with chronic obstructive pulmonary disease. Journal of Korean Medical Science, 30(10). doi: 10.3346/jkms.2015.30.10.1459 Jaimie Buckner 5/12/2016 12:39:37 P [Show More]
Last updated: 2 years ago
Preview 1 out of 27 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$9.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jul 06, 2020
Number of pages
27
Written in
Additional information
This document has been written for:
Uploaded
Jul 06, 2020
Downloads
0
Views
74