*NURSING > QUESTIONS & ANSWERS > Chamberlain College of Nursing - NR 509Brown_ Susan_NR509_Week 2_SOAP_Note (All)
Chamberlain College of Nursing - NR 509Brown_ Susan_NR509_Week 2_SOAP_Note
Document Content and Description Below
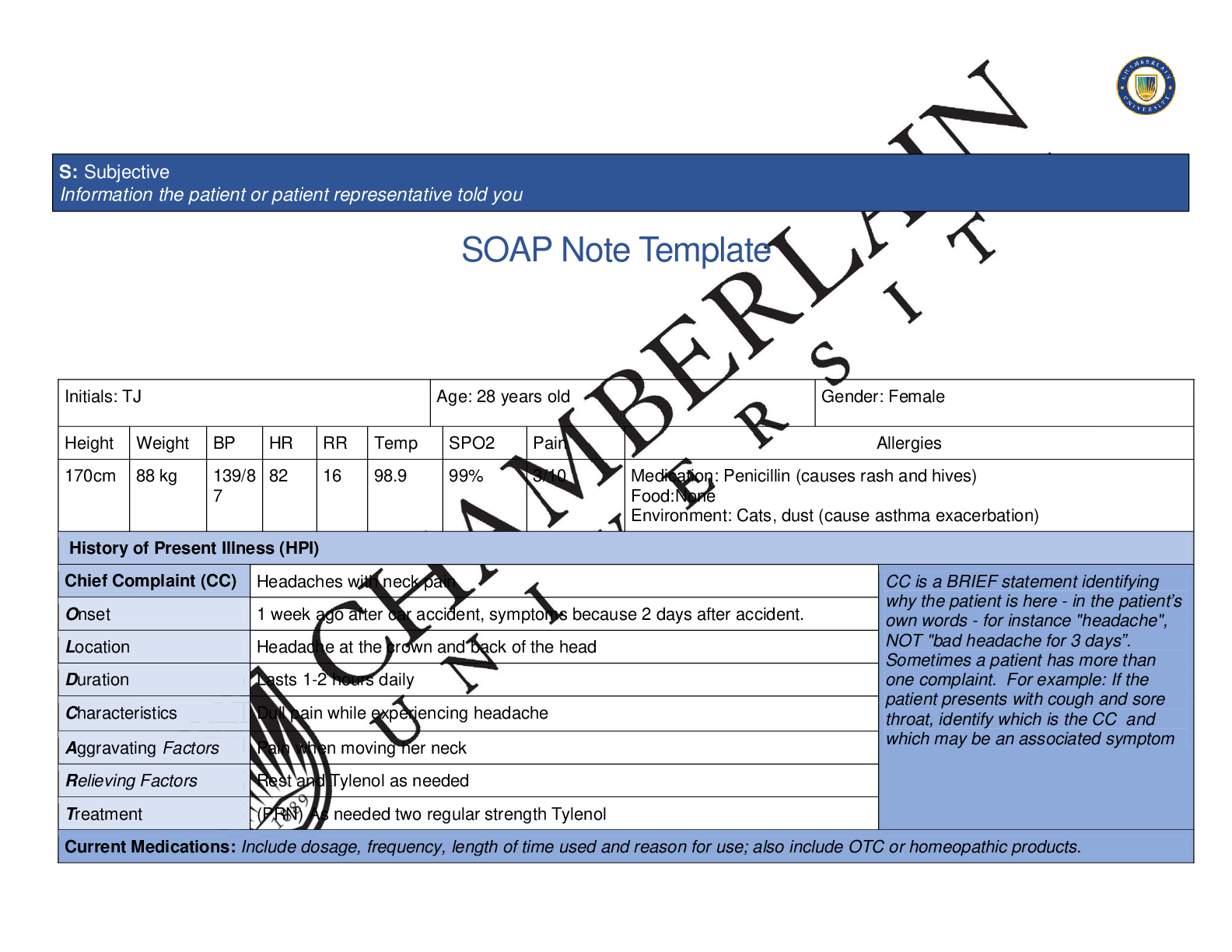
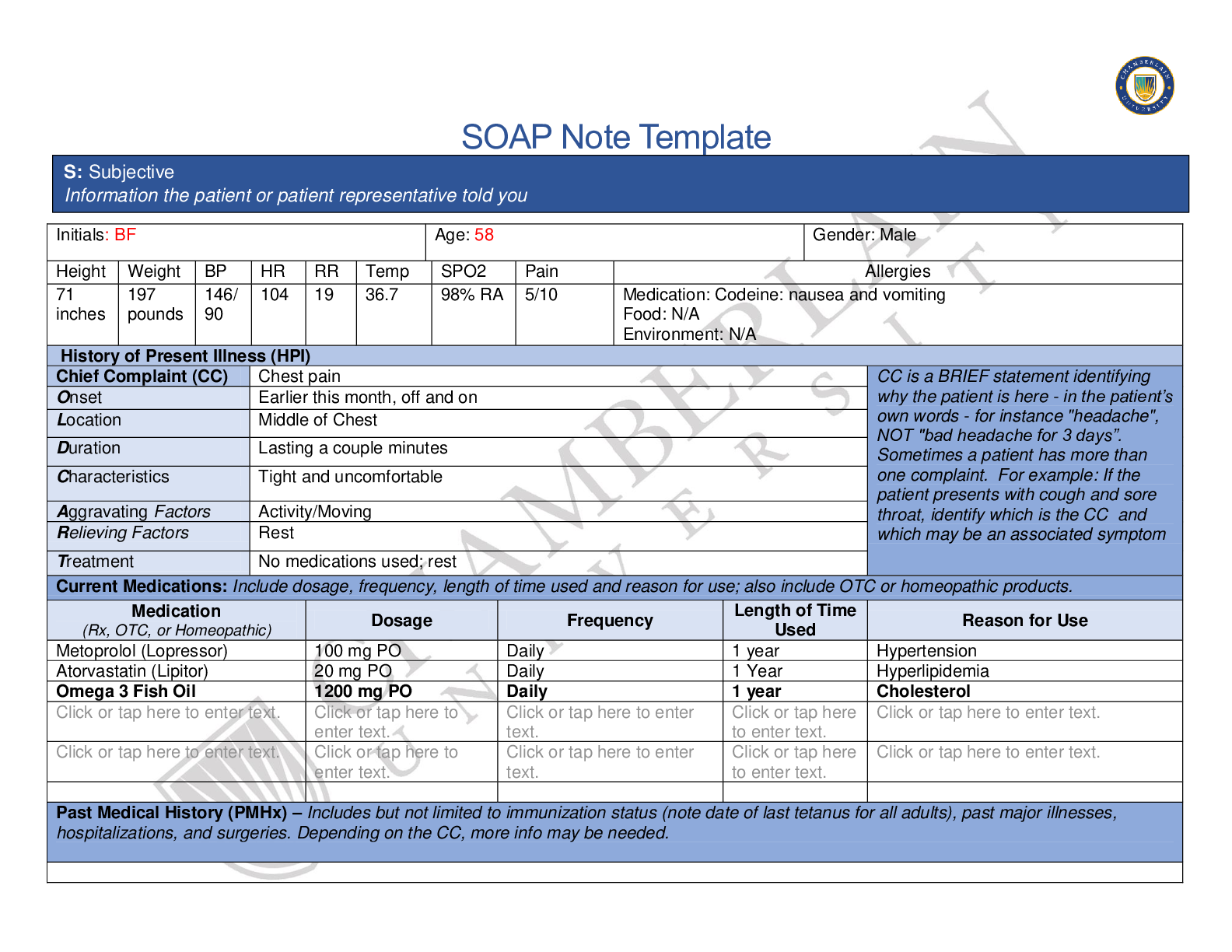
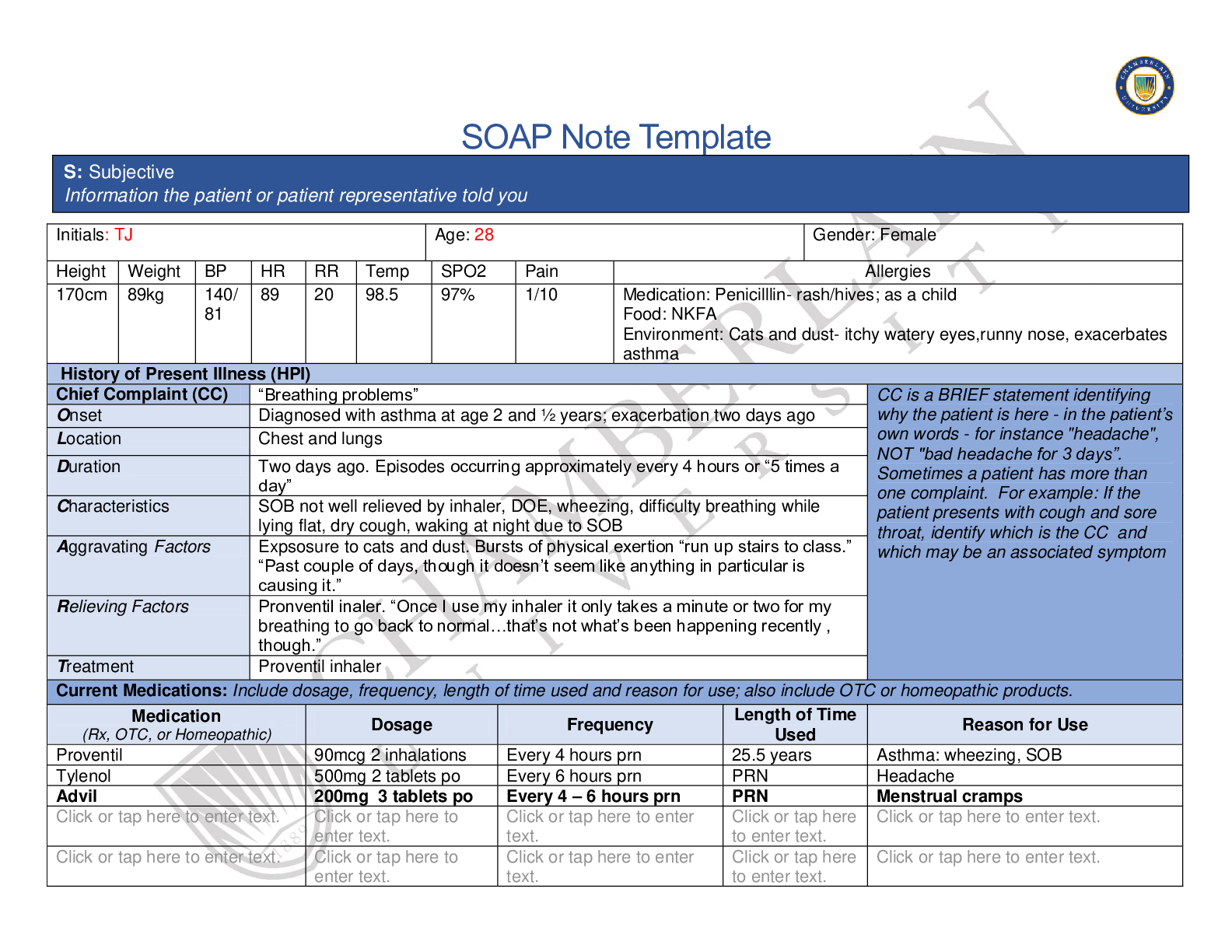
SOAP Note Template Initials: TJ Age: 28 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 170cm 89kg 140/ 81 89 20 98.5 97% 1/10 Medication: Penicilllin- rash/hives; as a child Food... : NKFA Environment: Cats and dust- itchy watery eyes,runny nose, exacerbates asthma History of Present Illness (HPI) Chief Complaint (CC) “Breathing problems” CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a patient has more than one complaint. For example: If the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom Onset Diagnosed with asthma at age 2 and ½ years; exacerbation two days ago Location Chest and lungs Duration Two days ago. Episodes occurring approximately every 4 hours or “5 times a day” Characteristics SOB not well relieved by inhaler, DOE, wheezing, difficulty breathing while lying flat, dry cough, waking at night due to SOB Aggravating Factors Expsosure to cats and dust. Bursts of physical exertion “run up stairs to class.” “Past couple of days, though it doesn’t seem like anything in particular is causing it.” Relieving Factors Pronventil inaler. “Once I use my inhaler it only takes a minute or two for my breathing to go back to normal…that’s not what’s been happening recently , though.” Treatment Proventil inhaler Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products. Medication (Rx, OTC, or Homeopathic) Dosage Frequency Length of Time Used Reason for Use Proventil 90mcg 2 inhalations Every 4 hours prn 25.5 years Asthma: wheezing, SOB Tylenol 500mg 2 tablets po Every 6 hours prn PRN Headache Advil 200mg 3 tablets po Every 4 – 6 hours prn PRN Menstrual cramps . . enter text. to . . . . enter text. to . . S: Subjective Information the patient or patient representative told youPast Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses, hospitalizations, and surgeries. Depending on the CC, more info may be needed. Asthma: Diagnosed with asthma at age 2 and ½ years Diabetes: Diagnosed at 24 years of age. Has not taken medication for diabetes for 3 years. Manages diabetes by avoiding sugar and trying to stay active. Does not self monitor blood glucose. Hospitalizations: Patient estimates being hospitalized 5 times for asthma as a child. Last hospitalization age 16 years. Denies previous intubation for asthma. Chest X-ray: at age 16 years Surgical: Denies Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent data. Include health promotion such as use seat belts all the time or working smoke detectors in the house. Patient moved back home with mother and little sister after the death of her father. Finds support through family, church, and her spirituality. Patient is employed and attends college. Exercise: Low level of activity: Exercise consists of “Being on feet at work and walking around campus.” Tobacco: denies use of tobacco products, vape, or e-cigarette. Not exposed to second hand smoke at home. Recreational drug use: Smoked marijuana for 5 to 6 years, last smoked marijuana at age 21 years of age. Stopped because “It just wasn’t fun anymore, plus it bothered my asthma.” Denies every using other illicit drugs or inhaling substances. Environmental: Carpet in bedrooms, no pets, changes bed linens once a week. “ We keep it pretty neat and tidy.” Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if pertinent. Asthma: younger sister; no other family members with asthmaCOPD/Emphysema: denies Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive symptom and provide additional details. Constitutional Skin HEENT ☒Fatigue : low energy ☐Weakness here to . ☐Fever/Chills here to . ☐Weight Gain here to . ☐Weight Loss here to . ☒Trouble Sleeping not sleeping well past couple of night; sob when lies flat ☒Night Sweats : ☐Other: enter text. ☐Itching here to . ☐Rashes here to . ☐Nail Changes Click or tap here to enter text. ☒Skin Color Changes Dark skin around neck, worse past couple months ☒Other: Mild acne“ my skin breaking out” ☐Diplopia here to . ☐Eye Pain here to . ☐Eye redness Click or tap here to . ☐Vision changes Click or tap here to . ☐Photophobia Click or tap here to . ☐Eye discharge Click or tap here to . ☐Earache to . ☐Tinnitus to . ☐Epistaxis here to . ☐Vertigo to . ☐Hearing Changes Click or tap here to . ☐Hoarseness to . ☐Oral Ulcers to . ☐Sore Throat to . ☐Congestion to . ☐Rhinorrhea to . ☐Other: . Respiratory Neuro Cardiovascular ☒Cough :dry, non-productive cough x 2 days ☐Hemoptysis . ☒Dyspnea : SOB onset 2 days, not relieved completely by inhaler, worse at night and when lies down ☒Wheezing onset 2 days ago, worsened by exposure to cats, dust, and physical excertion ☒Pain on Inspiration :chest tightness, when taking a deep breath ☐Syncope or Lightheadedness here to . ☒Headache : Once a week, when reads a lot ☐Numbness to . ☐Tingling . ☐Sensation Changes . ☐Chest pain enter text. ☒SOB : onset 2 days ago with asthma exacerbation, not completely relieved by inahler ☒Exercise Intolerance DOE, SOB, and wheezing ☐Orthopnea enter text. ☐Edema . ☐Murmurs enter ☐Palpitations here to . ☐Faintness to . ☐OC Changes here to . ☐Claudications here to . ☐PND . ☐Other: ☐Sputum Production ☐Other: enter text. ☐Speech Deficits here to . ☐Other: . text. . MSK GI GU PSYCH ☐Pain enter text. ☐Stiffness . ☐Crepitus . ☐Swelling . ☐Limited ROM . ☐Redness . ☐Misalignment . ☐Other: enter text. ☐Nausea/Vomiting . ☐Dysphasia enter text. ☐Diarrhea enter text. ☒Appetite Change : Increased hunger ☐Heartburn enter text. ☐Blood in Stool . ☐Abdominal Pain . ☐Excessive Flatus . ☐Food Intolerance . ☐Rectal Bleeding . ☐Other: . ☐Urgency . ☐Dysuria . ☐Burning . ☐Hematuria to . ☐Polyuria . ☐Nocturia . ☐Incontinence here to . ☐Other: . ☐Stress . ☒Anxiety : concerned about asthma and why it is not getting better ☐Depression to . ☐Suicidal/Homicidal Ideation . ☐Memory Deficits here to . ☐Mood Changes here to . ☐Trouble Concentrating Click or tap here to . ☐Other: . GYN ☐Rash . ☐Discharge . ☐Itching . ☐Irregular Menses . ☒Dysmenorrhea : Takes OTC Ibuprofen for menstrual cramps ☐Foul Odor . ☐Amenorrhea . ☐LMP: . ☐Contraception . ☐Other:.Body System Positive Findings Negative Findings General . Ms. Jones is a 28 year-old obese African-American female. She is healthy in appearance, well groomed, pleaseant, with appropriate speech, and makes good eye contact. She is alert and oriented to her surroundings. Facial features are symmetrical with movement and there are no obvious signs and symptoms of acute distress. Height 170cm, weight 89kg, BMI 30.8, BP 140/81, HR 89, RR 20, O2sat 97%, Temp 98.5, FVC 3.91, FEV1 3.15 FVC/FEV ratio 80.56%, Random BS 224 . Skin . Acanthosis nigricans noted around the neck Nevi noted on the right scapular region, dark in color, uneven margins (unable to measure size) Unable to assess HEENT . Unable to assess Unable to assess Respiratory . Auscultation: Wheezes noted in the right and left posterior lower lobes Bronchophony: positive Spirometry: FVC 3.91 FEV1 3.15 FVC/FEV ratio 80.56% Inspection: chest symmetric Palpation: chest expansion equal bilaterally tactile fremitus equal bilaterally Auscultation: Breath sounds present in all areas Neuro . Unable to assess Unable to assess Cardiovascular Unable to assess Unable to assess O: Objective Information gathered during the physical examination by inspection, palpation, auscultation, and palpation. If unable to assess a body system, write “Unable to assess”. Document pertinent positive and negative assessment findings.Problem List 1. Asthma exacerbation 6 Environmental allergies 11 . 2 Asthma uncontrolled 7 Acanthosis nigricans 12 . 3 Diabetes uncontrolled 8 Dysmenorrhea 13 . 4 Hypertension undiagnosed 9 . 14 . 5 Obesity 10 . 15 . . Musculoskeletal . Unable to assess Unable to assess Gastrointestinal . Unable to assess . Genitourinary . Unable to assess . Psychiatric . Anxiety related to the inability of asthma inhaler not relieving sysmptoms as before Good support from family and church. Strong spiritual beliefs Gynecological . Unable to asess Unable to assess Diagnosis ICD-10 Code Pertinent Findings A: Assessment Medical Diagnoses. Provide 3 differential diagnoses which may provide an etiology for the CC. The first diagnosis (presumptive diagnosis) is the diagnosis with the highest priority. Provide the ICD-10 code and pertinent findings to support each diagnosis.Diagnostics: List tests you will order this visit Test Pulmonary function test (PFT) Pulmonary function tests (PFT) measure's lung volume, capacity, rate of airflow, and the amount of gas exchange. Spirometry is a test that measures the lung volume during maximal inhalation and maximal exhalation. These tests can be evaluated before the administration of a bronchodilator and after administration of a bronchodilator. A bronchodilator response should be demonstrated in most cases of airflow limitation associated with asthma (Irvin, 2019). PFT’s are more precise than spirometry at measuring lung volume, capacity, rates of flow, and gas exchange (American Lung Association, 2017). Chest xray . Brain natriuretic peptide (BNP) BNP levels can assist in differentiation of symptoms and determine whether they are related to congestive heart failure. A BNP blood test accurately identifies heart failure about 90% of the time. (York et al., 2018). Complete blood count (CBC) An elevation in the number of white blood cells is indicative of the presence of infection (Sepsis Alliance, 2019). . . Medications: List medications/treatments including OTC drugs you will order and “continue previous meds” if pertinent. Drug Dosage Length of Treatment Referral/Consults: Acute respiratory infection unspecified J06.9 SOB, DOE, wheezing, and cough. FVC/FEV ratio 80.56% Congestive heart failure, left side unspecified I50.1 SOB, DOE, cough. SOB worse at night and when lies down Chronic obstructive airway, unspecifieddisease J44.9 SOB, DOE, cough, SOB. Symptoms not allievated with normal measures that have previously worked. P: Plan Address all 5 parts of the comprehensive treatment plan. If you do not wish to order an intervention for any part of the treatment plan, write “None at this time” but do not leave any heading blank. No intervention is self-evident. Provide a rationale and evidence-based in-text citation for each intervention.. . Education: . . Follow Up: Indicate when patient should return to clinic and provide detailed instructions indicating if the patient should return sooner than scheduled or seek attention elsewhere. . . References Include at least one evidence-based peer-reviewed journal article which relates to this case. Use the correct APA 6th edition formatting. . . [Show More]
Last updated: 2 years ago
Preview 1 out of 8 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jun 07, 2020
Number of pages
8
Written in
Additional information
This document has been written for:
Uploaded
Jun 07, 2020
Downloads
0
Views
120






.png)
.png)
.png)
.png)
.png)
.png)
.png)