*NURSING > QUESTIONS & ANSWERS > Chamberlain College of Nursing - NR 509Cardiac SOAP (All)
Chamberlain College of Nursing - NR 509Cardiac SOAP
Document Content and Description Below
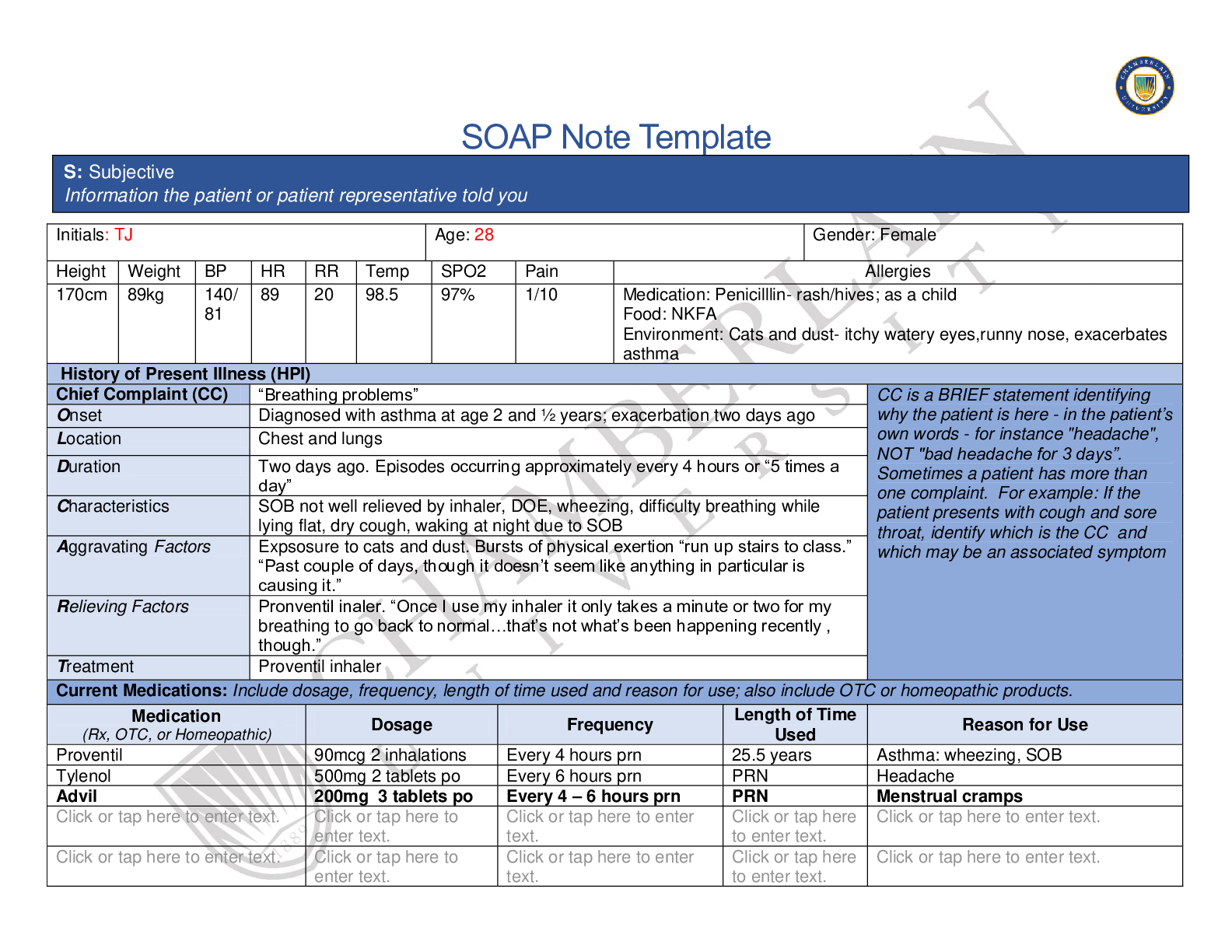
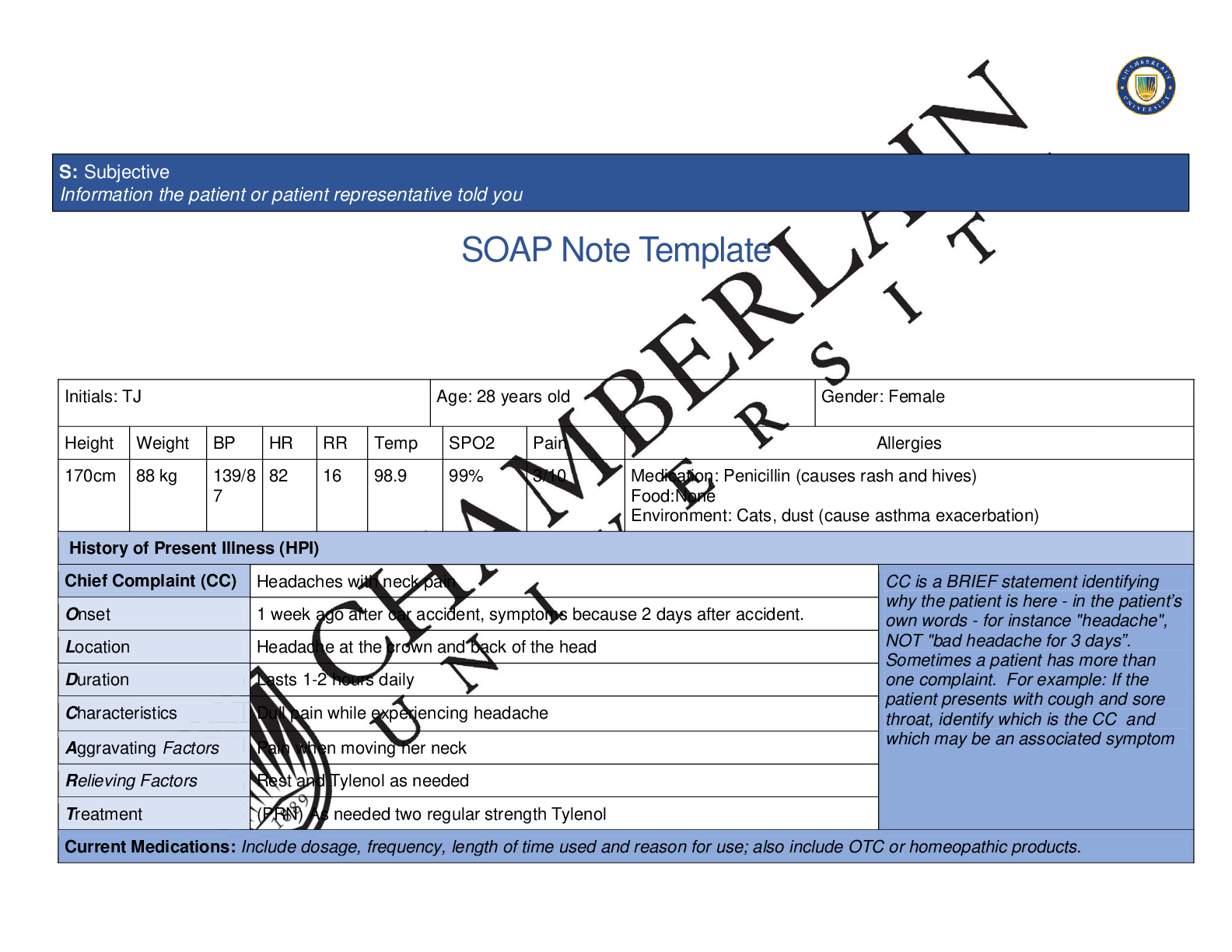
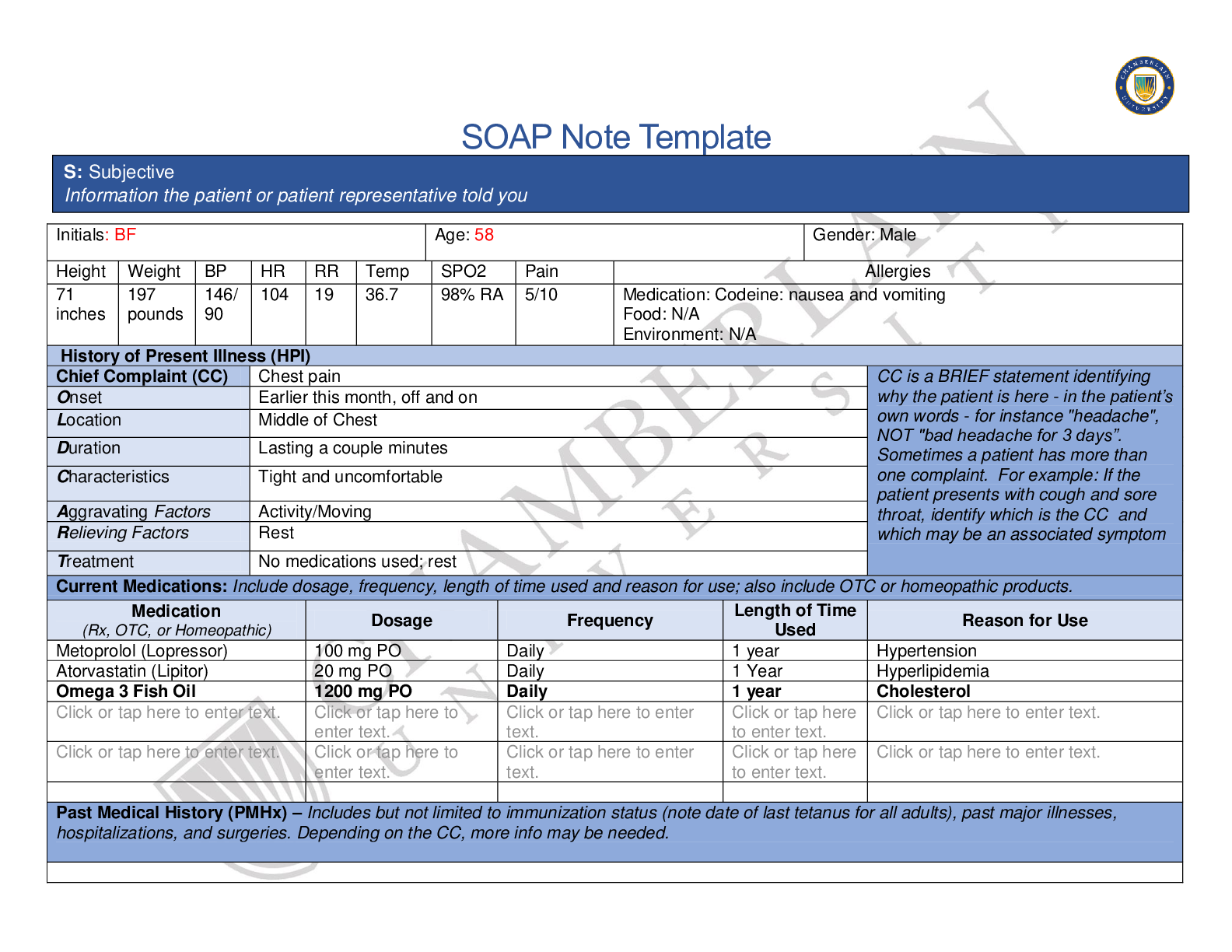
SOAP Note Template Initials: BF Age: 58 Gender: Male Height Weight BP HR RR Temp SPO2 Pain Allergies 71 inches 197 pounds 146/ 90 104 19 36.7 98% RA 5/10 Medication: Codeine: nausea and vomit... ing Food: N/A Environment: N/A History of Present Illness (HPI) Chief Complaint (CC) Chest pain CC is a BRIEF statement identifying why the patient is - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a patient has more than one complaint. For example: If the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom Onset Earlier this month, off and on Location Middle of Chest Duration Lasting a couple minutes Characteristics Tight and uncomfortable Aggravating Factors Activity/Moving Relieving Factors Rest Treatment No medications used; rest Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products. Medication (Rx, OTC, or Homeopathic) Dosage Frequency Length of UsedTime Reason for Use Metoprolol (Lopressor) 100 mg PO Daily 1 year Hypertension Atorvastatin (Lipitor) 20 mg PO Daily 1 Year Hyperlipidemia Omega 3 Fish Oil 1200 mg PO Daily 1 year Cholesterol . . . to . . to . . Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses, hospitalizations, and surgeries. Depending on the CC, more info may be needed. S: Subjective Information the patient or patient representative told youPatient stated current and up to date with immunizations including annual flu shot and tetanus (10/2014). All childhood immunizations were received. Patient denies past surgical history or hospitalizations. No past history of angina. Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent data. Include health promotion such as use seat belts all the time or working smoke detectors in the house. Patient denies smoking and smokeless tobacco use; denies illicit drug use including marijuana. Patient stated drinking approximately 2-3 beers per week. Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if pertinent. Father: deceased at 75 (colon cancer); PMH: hypertension, hyperlipidemia, obesity Mother: alive (80 y/o); PMH: DM type 2, hypertension Brother: deceased at 24- MVC Sister: alive (52 y/o); PMH: DM type 2, hypertension Maternal grandmother: deceased age 65- breast cancer Maternal grandfather: deceased age 54- MI Paternal grandmother: deceased age 78- pneumonia Paternal grandfather: deceased age 85- natural causes Son: alive, age 26; no PMH Daughter: alive, age 19; PMH: asthma Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive symptom and provide additional details. Constitutional Skin HEENT ☐Fatigue to . ☐Weakness . ☐Fever/Chills . ☒Weight Gain approx. 20 pounds over last year or so ☐Weight Loss . ☐Itching . ☐Rashes . ☐Nail Changes Click or tap . ☐Skin Color Changes . ☐Diplopia . ☐Eye Pain . ☐Eye redness Click or tap . ☐Vision changes Click or tap . ☐Photophobia Click or tap . ☐Earache to . ☐Tinnitus to . ☐Epistaxis . ☐Vertigo to . ☐Hearing Changes Click or tap . ☐Hoarseness to . ☐Oral Ulcers to . ☐Sore Throat to . ☐Congestion to . ☐Rhinorrhea to .☐Trouble Sleeping Click or tap . ☐Night Sweats . ☐Other: . ☐Other: . ☐Eye discharge Click or tap . ☐Other: . Respiratory Neuro Cardiovascular ☐Cough . ☐Hemoptysis . ☐Dyspnea . ☐Wheezing . ☐Pain on Inspiration to . ☐Sputum Production . . . ☐Other: . ☐Syncope or Lightheadedness . ☐Headache to . ☐Numbness to . ☐Tingling . ☐Sensation Changes . ☐Speech Deficits . ☐Other: . ☒Chest pain intermittent x 1 month, approx. 3 episodes ☐SOB . ☐Exercise Intolerance to . ☐Orthopnea . ☐Edema . ☐Murmurs . ☐Palpitations . ☐Faintness to . ☐OC Changes . ☐Claudications . ☐PND . ☐Other: . MSK GI GU PSYCH ☐Pain . ☐Stiffness . ☐Crepitus . ☐Swelling . ☐Nausea/Vomiting . ☐Dysphasia . ☐Diarrhea . ☐Appetite Change . ☐Urgency . ☐Dysuria . ☐Burning . ☐Hematuria to . ☐Stress . ☐Anxiety . ☐Depression to . ☐Suicidal/Homicidal Ideation .☐Limited ROM . ☐Redness . ☐Misalignment . ☐Other: . ☐Heartburn . ☐Blood in Stool . ☐Abdominal Pain . ☐Excessive Flatus . ☐Food Intolerance . ☐Rectal Bleeding . ☐Other: . ☐Polyuria . ☐Nocturia . ☐Incontinence . ☐Other: . ☐Memory Deficits . ☐Mood Changes . ☐Trouble Concentrating Click or tap . ☐Other: . GYN ☐Rash . ☐Discharge . ☐Itching . ☐Irregular Menses . ☐Dysmenorrhea . ☐Foul Odor . ☐Amenorrhea . ☐LMP: . ☐Contraception . ☐Other:. Body System Positive Findings Negative Findings General . Approximately 20 pound weight gain over last couple of years Patient denies Fever, chills, fatigue Skin . N/A Inspection of upper body revealed no abnormalities HEENT . O: Objective Information gatd during the physical examination by inspection, palpation, auscultation, and palpation. If unable to assess a body system, write “Unable to assess”. Document pertinent positive and negative assessment findings.Respiratory . Auscultation: fine crackles noted at bilateral posterior bases Auscultation: clear lung sounds throughout anteriorly; clear lung sounds upper posterior Neuro. Cardiovascular Ausculatation points (aortic, pulmonic, Erb’s point, Tricuspid, mitral): revealed S3 heart sounds, ventricular gallop Carotid Auscultation: Right sided positive for bruit Abdominal Aorta auscultation: positive for bruit Palpation: Right carotid artery positive for thrill (3+) Popliteal, Tibial, and Dorsalis Pedis artery palpation: no thrill, amplitude 1+ bilaterally Auscultation: left carotid- no bruit noted; no bruit noted in right renal artery, left renal arter, right iliac artery, left iliac artery, right femoral artery, left femoral artery Inspection: No JVD noted (3cm at sternal angle), chest symmetrical with no abnormalities Capillary refill less than 3 seconds (both hands and feet) No edema noted on bilateral lower extremities Palpation: Left carotid artery negative for thrill (2+); PMI: displaced laterally, 3 cm; brisk and tapping Brachial, Radial, and Femoral artery palpation: no thrill, amplitude 2+ bilaterally EKG: regular sinus rhythm with no ST elevation Skin tugor WNL Musculoskeletal . Gastrointestinal . N/A Inspection: abdomen is symmetrical in shape, rounded Abdominal palpation: no areas of tenderness or palpable masses; kidneys and spleen not palpable, liver palpable Auscultation: no friction rub noted with liver or spleen Percussion: All areas generally tympanic Genitourinary . Psychiatric . N/A Denies SI/HI, depressionProblem List 1. Intermittent Chest Pain 6 . 11 . 2 Fine Crackles in B/L bases 7 . 12 . 3 abnormal heart sounds (S3) 8 . 13 . 4 carotid bruit (right) 9 . 14 . 5 . 10 . 15 . Diagnostics: List tests you will order this visit Test Rationale/Citation Troponin To see if the patient has any cardiac ischemia; rule out NSTEMI BNP Adventitious lung sounds with abnormal heart sounds- rule out CHF Chest X-ray Adventitious lung sounds, rule ou inflammatory process Crotid ultrasound Possible carotid artery stenosis or occlusion; positive right side bruit. Gunduz et al., (2019) noted t Gynecological . , N/A , N/A Diagnosis ICD-10 Code Pertinent Findings Angina Pectoris, unspecified I20.9 Intermittent chest pain; increased with activity, relieved with rest Abnormal heart sounds R01.2 S3, ventricular gallop noted on auscultation Carotid Artery Syndrome, hemispheric G45.1 Right carotid artery bruit noted on auscultation P: Plan Address all 5 parts of the comprehensive treatment plan. If you do not wish to order an intervention for any part of the treatment plan, write “None at this time” but do not leave any heading blank. No intervention is self-evident. Provide a rationale and evidence-based in- citation for each intervention. A: Assessment Medical Diagnoses. Provide 3 differential diagnoses which may provide an etiology for the CC. The first diagnosis (presumptive diagnosis) is the diagnosis with the highest priority. Provide the ICD-10 code and pertinent findings to support each diagnosis.is a high risk correlation between patients with carotid artery stenosis and coronary artery disease. This study showed that doppler/ultrasound can be utilized in assisting proper course of treatment (stenting versus medical management). Echocardiogram Abnormal heart sounds on auscultation- possible valvular disease Medications: List medications/treatments including OTC drugs you will order and “continue previous meds” if pertinent. Drug Dosage Length of Treatment Rationale/Citation Nitroglycerin 0.4 mg sublingual: 1 tab every 5 minutes x 3 PRN PRN Acute attacks of chest pain can be relieved by sublingual nitroglycerin and help promote vasodilation of possible spasm (Malik, Porter, Pavlides, & Chatzizisis, 2017). Continue previous medications . . . Referral/Consults: Cardiology Rationale/Citation Pertinent for follow up of intermittent chest pain/stable angina. Possible need for further evaluation and treatment with invasive diagnostics and intervention. Education: Diet for cardiac patients Rationale/Citation Patient may need additional information related to cholesterol and heart healthy diet. History of high cholesterol puts patient at risk for plaque buildup in arteries. Follow Up: Indicate when patient should return to clinic and provide detailed instructions indicating if the patient should return sooner than scheduled or seek attention elsew. 1 week Rationale/Citation Follow up on blood work. If chest pain occurs, take SL nitro and go to nearest Emergency Department. References Include at least one evidence-based peer-reviewed journal article which relates to this case. Use the correct APA 6th edition formatting. Gunduz, Y., Akdemir, R., Gunduz, H., Varim, P., Ayhan, L., Cakar, M., … Kilic, H. (2019). Relationship between carotid artery doppler flow velocity and extent of coronary artery disease. Pakistan Heart Journal, 52(2), 124–131. Retrieved from https://search-ebscohostcom.chamberlainuniversity.idm.oclc.org/login.aspx?direct=true&db=a9h&AN=138683220&site=eds-live&scope=site Malik, S., Porter, T., Pavlides, G., & Chatzizisis, Y. (2017). Vasospastic angina presenting with syncope and chest pain: A case report and brief literature review. South Dakota Medicine: The Journal Of The South Dakota State Medical Association, 70(11), 498–502. Retrieved from https://search-ebscohost-com.chamberlainuniversity.idm.oclc.org/login.aspx?direct=true&db=mdc&AN=29088521&site=eds-live&scope=site [Show More]
Last updated: 2 years ago
Preview 1 out of 8 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jun 07, 2020
Number of pages
8
Written in
Additional information
This document has been written for:
Uploaded
Jun 07, 2020
Downloads
0
Views
107






.png)
.png)
.png)
.png)
.png)
.png)
.png)