Biology > STUDY GUIDE > BIO 351 Health Assessment Quiz 3 (A GRADED) Study Guide | 100% Verified (All)
BIO 351 Health Assessment Quiz 3 (A GRADED) Study Guide | 100% Verified
Document Content and Description Below
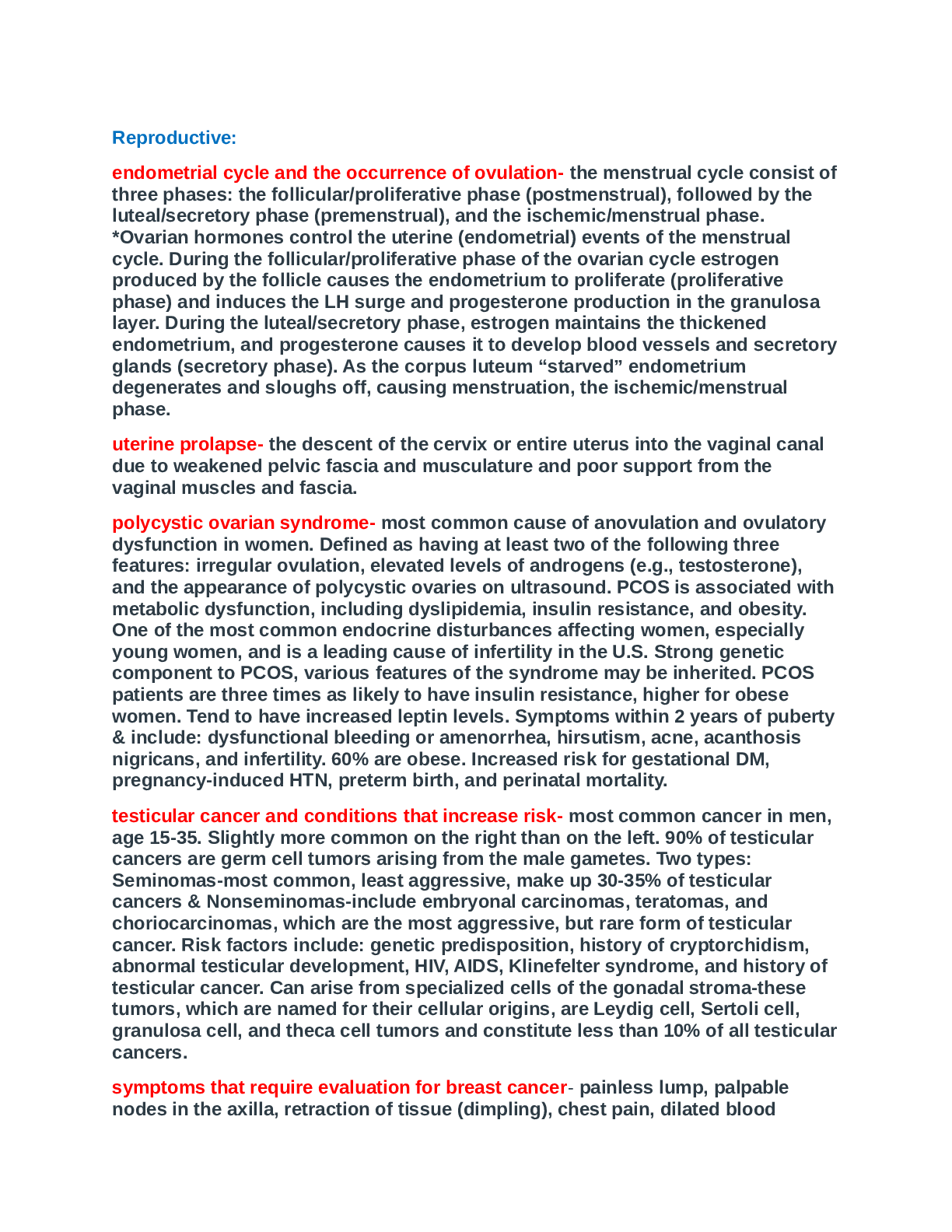
Health Assessment Quiz 3 Thorax and Lungs • Structures of the thoracic cavity o Thoracic cage- borders ▪ Bony structures; sternum, rubs, vertebrae, diaphragm ▪ ▪ Sternal notch: g... ives you a baseline of where the trachea alignment is ▪ Costal angle: 90 or less, unless hyersema (hyper inflation of the lungs) • Anterior thoracic landmarks o Suprasternal notch: U-shaped depression just above sternum o Sternum: breastbone: manubrium, body, xiphoid process o Sternal angle ▪ Bony ridge, few centimeters down on manubrium ▪ Also called “angle of Louis” ▪ Useful for starting to count ribs, fused with 2nd rib o • Posterior thoracic landmarks o Vertebra prominens; C-7 o Spinous processes; knobs ▪ T-1 down to T-4 align with same number ribs ▪ After T-4 spinous processes angle downward o Inferior border of scapula ▪ Lower tip of scapula is at the 7th or 8th rib o Twelfth rib ▪ Palpate midway between spine and persons sides to feel its free tip o • Reference lines o Midsternal line o Midclavicular line o Scaplar line o Vertebral line o Anterior- posterior midaxillary line • Thoracic cavity o Mediastinum ▪ Middle section of the thoracic activity ▪ Contains esophagus, trachea, heart and great vessels ▪ Right and left pleural cavities on either side contain lungs o Lobes of lungs ▪ Lobes separated by fissures ▪ Not symmetrical ▪ Left • 2 lobes • Narrower related to heart bulges to left ▪ Right • Shorter related to liver • 3 lobes o Anterior chest ▪ Apex: 3-4 cm above inner 1/3 of clavicle ▪ Base: lies on diaphragm at 6th rib in midclavicular line o Posterior ▪ C-7 marks the apex and T-10 marks the base (T-12 with deep inspiration) o Lateral ▪ Lies from apex of axilla to 7th or 8th rib o o o Pleurae ▪ Thin slippery envelope between the lung and the chest wall ▪ Visceral pleura lines outside of lungs dipping down into the fissures and is continuous with the parietal plerua lining the inside of the chest wall and diaphragm ▪ Tiny space between visceral and parietal pleura (few mm) filled with fluid ▪ At base of lungs pleurae extend 3cm further than lungs forming costodiaphragmatic recess (normally empty space) ▪ • Important points o Left lung has no middle lobe o Anterior chest- contains upper and middle lobes (right) with very little lower lobe o Posterior chest- has almost all lower lobe; right middle lobe does not project into posterior chest • Trachea and bronchi o Location of trachea and bronchi ▪ Dead space= passage for air to get into lungs but no air exchange ▪ Acinus: bronchi ▪ Alveoli: sac ▪ Transform gases from the environment ▪ o • Respiration o Mechanics for respiration ▪ Four functions of respiratory system • Supply of O2 for energy production • Removing CO2 • Maintaining acid-base balance of arterial blood ▪ Changing chest size during respiration • Inspiration • Expiration ▪ ▪ • Developmental considerations o Infant ▪ Round thorax ▪ Chest 30-36cm; 2 cm smaller than head of circumference ▪ Chest wall thin and little musculature ▪ Ribs and xiphoid are prominent ▪ Thoracic cage soft and flexible ▪ Breathes through nose until 3 months ▪ Abdominal bulge with each inspiration due to diaphragm major muscle used and intercostal muscles poorly developed o Child ▪ Carrel shape after age 6 could indicate asthma or CF o Aging adult ▪ Less mobile thorax ▪ Respiratory muscle strength decreases after age 50 and continues through age 70 ▪ Decrease in elastic properties making lungs more rigid and more difficult to inflate • • • Subjective data o Cough, SOB (paroxysmal, nocturnal, dyspnea), chest pain w/ breathing, past history for respiratory infections, smoking, environmental exposure, self-care behaviors, culture • Objective data o Preparation ▪ Position: upright ▪ Draping • Male • Female: gown open on back ▪ Timing during complete examination • After thyroid palpation • Posterior than anterior ▪ Cleaning stethoscope end piece o Posterior chest- inspect ▪ Thoracic cage • Shape and configuration of chest wall • Anteroposterior: transverse diameter • Position of person • Skin color and condition o Posterior chest- palpate ▪ Symmetric expansion • ▪ Tactile (or vocal) fremitus • Technique • Factors that affect normal intensity of tactile fremitus • Palpate entire chest wall (posterior) • Predominant note over lung fields • Diaphragmatic excursion • • ▪ Auscultate • Breath sounds- normal o Technique ▪ o Bronchial ▪ Pitch- high ▪ Amplitude- loud ▪ Duration- inspiration> expiration ▪ Quality- harsh, hollow tubular ▪ Normally- trachea and larynx ▪ o Bronchovesicular ▪ Pitch- moderate ▪ Amplitude- moderate ▪ Duration- inspiration=expiration ▪ Quality- mixed ▪ Normally- over major between bronchi between scapula (anterior around upper sternum) o Vesicular ▪ Pitch- low ▪ Amplitude- soft ▪ Duration- inspiration>expiration ▪ Quality- rustling ▪ Normally- peripheral lung fields (smaller bronchioles and alveoli) ▪ • Voice sounds o Bronchophony o Egophony o Whispered pectoriloquy o Anterior chest- inspect ▪ Shape and configuration of chest wall ▪ Facial expressions ▪ Level of consciousness ▪ Skin color and condition ▪ Quality of respirations ▪ Accessory muscles o Anterior chest- palpate ▪ Symmetric chest expansion • ▪ Tactile fremitus ▪ Palpate the anterior chest wall ▪ ▪ o Anterior chest- percuss ▪ Predominant note over lung fields ▪ Borders of cardiac dullness ▪ o Anterior chest-auscultate ▪ Breath sounds ▪ Abnormal breath sounds ▪ Adventitious sounds (not normal) • Crackles o Roll strand of hair near ear (fine) vs open Velcro (coarse) • Wheeze o High or low pitched (sonorous rhonchi) o Passageways narrowed, constricted • Stridor o Crowning, louder in neck o Originates from trachea and pharynx • Pleural friction rub o 2 pieces of leather o Measurement of pulmonary function status ▪ Forced expiration time; 4 sec or less normal ▪ Pulse oximeter ▪ 6- minute walk test (6MWT): set own pace to cover as much ground in 6 minutes (can slow down or stop at any time): looking for >300 meters in 6 minutes o Infants and children ▪ Let parent hold child ▪ Ignore usual exam sequence ▪ Encourage participation with age ▪ APGAR scoring system (pg 437) • Done at 1 minute and 5 minutes after birth • • Documentation o Subjective o Higher the score, the better in shape (7-10) o 3-6 moderately depressed o Less than that, ICU ▪ No cough, SOB or chest pain with breathing. No history of respiratory distress. Has one or no colds per year. Has never smoked. Works in well-ventilated office on smoke-free campus. Last TB test 4 years PTA (negative). Never had CXR. o Objective ▪ Inspection • AP< transverse diameter, resp. 16/min, relaxed and even ▪ Palpation • Chets expansion symmetric. Tactile fremitus equal bilaterally. No tenderness. No lumps or lesions ▪ Percussion • Resonant over lung fields. Diaphragmatic excursion 5 cm and equally bilateral ▪ Auscultation • Vesicular breath sounds over lung fields and equal bilaterally. No adventitious sounds o Assessment ▪ Intact thoracic structures ▪ Llung sounds clear and equal • Abnormal findings o Configurations of the thorax ▪ Barrel chest • ▪ Pectus excavatum ▪ Pectus carinatum ▪ Scoliosis • ▪ Kyphosis • ▪ Normal • ▪ Funnel chest • • Not often symptomatic o Respiration patterns ▪ Sigh, tachycardia, bradycardia, hyperventilation, hypoventilation, Cheyne-stokes respiration (periods of not breathing), biot’s respiration, chronic obstruction breathing (expiration is longer) o Abnormal tactile fremitus ▪ Increased tactile fremitus • Occurs when conditions that increase the density of lung tissue, thereby making a better conducting medium for vibrations compression or consolidation, pneumonia ▪ Decreased tactile fremitus • Occur when anything obstructs transmission of vibrations obstructed bronchus, pleural effusion or thickening, pneumothorax, emphysema ▪ Rhonchal fremitus • Vibrations felt when inhaled air passes, through thick secretions in the larger bronchi; may decrease somewhat by coughing ▪ Pleural friction fremitus • Produced when inflammation of parietal or visceral pleura causes a decrease in the normal lubricating fluid. Opposing surfaces make a coarse grating sound when rubbed together during respirations. Best detected by auscultation. “palpable friction rub” o Common respiratory conditions ▪ Atelectasis ▪ Pneumonia • Infection and /or inflammation of the lungs o Air sacs in the lungs fill with pus or other liquid • Can affect lungs in two ways o Affects a section (lobe) of a lung • Bronchial pneumonia (or bronchopneumonia) o Affects patches throughout both lungs • Five main causes: o Bacteria ▪ Tissue of part of a lobe or lobes becomes completely filled with liquid (consolidation). The infection quickly spreads through the bloodstream and the whole body is invaded. ▪ Streptococcus pneumoniae most common cause ▪ Vaccine preventable ▪ Symptoms: • Onset varies gradual to sudden, may experience shaking chills, severe chest pain, cough that produces rust-colored or greenish mucus. • Temp may rise as high as 105 degrees F diaphoresis, tachycardia, tachypnea, cyanotic nail beds o Virus ▪ Symptoms: • Same as influenza symptoms: fever, a dry cough, headache, muscle pain, and weakness. Within 12 to 36 hours, increasing breathlessness; cough worsens and produces a small amount of mucus. High fever o Mycoplasmas o Fungi o Various chemicals • Treatment o Antibiotics if bacterial o Rarely antivirals may be ordered for viral o Supportive treatment: proper diet, O2, analgesics, rest • Prevention o Annual flu vaccine because pneumonia is a common complication of influenza. o A vaccine for pneumococcal pneumonia, one type of bacterial pneumonia; given only to high risk/older adult o Highest risk groups: ▪ Chronic illnesses such as lung disease, heart disease, kidney disorders, sickle cell anemia, or diabetes. ▪ recovering from severe illness ▪ Bronchitis ▪ nursing homes or other chronic care facilities ▪ age 65 or older o Most important preventive measure is to be alert to any symptoms of respiratory symptoms that linger longer than a few days. o Health promotion-; proper diet and hygiene, rest, regular exercise • Inflammation of the lining in bronchial tubes • Less air is able to flow • Productive cough with heavy mucus or phlegm • May be acute (usually associated with URI and no fever) or chronic • Chronic o Mucus-producing cough most days of the month, 3 months of a year for 2 successive years without other underlying disease o Inflammation eventually leads to scarring of the lining of the bronchial tubes o After irritated over a long period of time, the lining of the bronchial tubes becomes thickened, an irritating cough develops, air flow may be hampered and the lungs become scarred. The bronchial tubes then make an ideal breeding place for infections • Risk factors o URI or viral infection o Smoking o Exposure to industrial dust and fumes o Air pollution • Treatment o Antibiotics if associated with bacterial infection o Bronchodilators o Corticosteroids o Eliminate sources of irritation and infection in the nose, throat, mouth, sinuses, and bronchial tubes; avoid polluted air and dusty working conditions, smoking cessation o Ex: prednisone, PO, worried about abruptly stopping, risk for constipation • ▪ Emphysema • Destruction of air sacs (alveoli) in the lungs where oxygen from the air is exchanged for carbon dioxide in the blood • Walls of the air sacs are thin and fragile and damage to the air sacs is irreversible and results in permanent "holes" in the tissues of the lower lungs • As air sacs are destroyed, the lungs are able to transfer less and less oxygen to the bloodstream, causing shortness of breath. • Lungs lose their elasticity pt. has difficulty exhaling • Insidious onset, most often due to smoking • Symptoms o Cough, shortness of breath and a limited exercise tolerance • Diagnosis o Pulmonary function tests, along with the patient's history, examination and other tests. • ▪ Asthma ▪ Pleural effusion thickening • Collection of fluid in the intrapleural space (b/t visceral and parietal pleurae) with compression of overlying lung tissue • Fluid may be blood, purulent matter, exudate, or lymphatic fluid • Breath sounds and voice sounds decreased or absent • Symptoms; chest pain, dyspnea. Many cause no symptoms but are discovered during the physical examination or seen on a chest x-ray. • Causes; heart failure, renal failure hypoalbuminemia infections (TB, bacterial, fungal, viral), pulmonary embolism, and malignancies, 20% cause unknown • ▪ CHF • Pump failure with increasing cardiac overload causes pulmonary congestion or increases amount of blood present in pulmonary capillaries • Pulmonary capillaries engorged and dependent air sacs deflate • Bronchial mucosa swollen • Symptoms; Increased RR, SOB on exertion, orthopnea, paroxysmal nocturnal dyspnea, nocturia, ankle edema, pallor • Crackles at bases • ▪ Pneumothorax • Spontaneous pneumothorax o Sudden collection of air or gas in the chest that causes the lung to collapse in the absence of a traumatic injury to the chest or lung o Occurs in pts. with no known lung disease. o Affects close to 9,000 persons in the United States each year- most often among tall, thin men between 20 and 40 years old. o Cause of this type of pneumothorax is the rupture of a bleb or cyst in the lung • Symptoms o Chest pain on affected side o Dyspnea (shortness of breath) o Cough o Abnormal breathing movement o Rapid respiratory rate • Spontaneous pneumothorax is diagnosed by chest radiographs. • Treatment o Objective is to remove the air from the pleural space, allowing the lung to re-expand. o Small pneumothorax will resolve on its own in 1 to 2 weeks o Larger require needle aspiration or a chest tube o Reexpansion of the lung may take several days with the chest tube left in place o Surgery may be performed for a repeated episode to prevent recurrence • SECONDARY PNEUMOTHORAX o Occurs in pts. with known lung disease, most often chronic obstructive pulmonary disease (COPD) o Commonly causes include tuberculosis, pneumonia, asthma, cystic fibrosis, lung cancer, and certain forms of interstitial lung disease o Generally severe and often life threatening o Symptoms o Identical to primary spontaneous pneumothorax o Treatment o Same as those for primary spontaneous pneumothorax, but the circumstances are much more urgent. o small pneumothorax can be life threatening and virtually all patients are treated with chest tubes o Sudden death may occur before chest tubes can be place and respiratory failure can occur within hours after the tubes are inserted o Mortality rate associated with secondary pneumothorax is high (15%) • ▪ TB • An infectious disease that usually attacks the lungs but can attack almost any part of the body • Airborne • Active disease or latent • High risk o HIV/AIDS o Close contact of pt. with TB o Chronic disease or immunocompromised o Pts. from countries with high TB rates o Some racial or ethnic minorities o People who work in or are residents of long-term care facilities (nursing homes, prisons, some hospitals) o Health care workers and others such as prison guards o Malnourished o Alcoholics, IV drug users and homeless • A person with TB infection will have no symptoms. A person with TB disease may have any, all or none of the following symptom o Persistent cough o Feeling tired all the time o Weight loss o Loss of appetite o Fever o Coughing up blood o Night sweats • A person with TB disease may feel perfectly healthy or may only have a cough from time to time; important to screen high risk groups with skin test (PPD) • Treatment o Depends on whether a person has active TB disease or only TB infection. ▪ PE o Infected with TB, but no active TB disease o May be given preventive therapy to kill germs that are not doing any damage right now, but could so do. o Daily dose of isoniazid (also called "INH"); an inexpensive TB medicine. The person takes INH for nine months (up to a year for some patients), with periodic checkups to make sure the medicine is being taken as prescribed o Treatment for active TB (months of drug therapy) o First-line anti-TB agents ▪ isoniazid (INH) ▪ rifampin (RIF) ▪ ethambutol (EMB) ▪ pyrazinamide (PZA) • Undissolved material (thrombus or air bubbles or fat globules) originating in legs or pelvis detach and travel through venous system returning blood to right heart, and lodge to occlude pulmonary vessels. • Over 95% r/t DVT in lower legs • Results in ischemia, increased pulmonary artery pressure, decreased cardiac output, and hypoxia • Chest pain worse on inspiration • Restless, anxiety, MS changes, cyanosis, cough <80 Pox, diaphoresis, hypotension, • Crackles and wheezes • ▪ Acute respiratory distress syndrome (ARDS) Examination of the Abdomen • Ascites o An accumulation of fluid in the peritoneal cavity o • Landmarks related to the abdomen o Large oval cavity extending from the diaphragm to the brim of the pelvis o Bordered in back by vertebral column and paravertebral muscles o On the sides and front by the lower rib cage and abdominal muscles o RLQ, RUQ, LUQ, LLQ • Roles of the GI tract o The gastro-intestinal tract (GIT) commences at the oral cavity and continues through the pharynx, esophagus, stomach, small intestine and colon (large intestine) ending up at the rectum o The major role of the GIT is to digest and absorb nutrients from food and is helped in this function by the accessory organs o o o • Solid viscera o All abdominal organs are referred to as viscera o Solid viscera maintain characteristic shape ▪ Liver ▪ Pancreas ▪ Spleen ▪ Adrenal Glands ▪ Kidneys ▪ Ovaries and uterus • Hollow viscera o Shape depends on the contents ▪ Stomach ▪ Gall Bladder ▪ Small intestine ▪ Colon ▪ Bladder o o o • Aorta o Just left to the midline in the upper part of the abdomen o 2 cm below umbilicus, it bifurcates into the right and left common renal arteries which become the iliac arteries o Right and left iliac arteries become the femoral arteries in the groin area o Aorta and femoral arteries can be palpated o • Costovertebral angle o Bean shaped kidneys are retroperitoneal (posterior) to the abdominal contents o Protected by posterior ribs and muscles o 12th rib forms an angle with vertebral column called costovertebral angle o Kidneys lie at 11th and 12th rib o Because of liver, R kidney 1-2cm lower than L kidney o Indirect or direct percussion • Subjective data o Appetite ▪ Any changes? Loss of appetite? ▪ Any change in weight? If so, was it purposeful? ▪ How much weight lost or gained ▪ Over what period of time? ▪ If it was intentional or not ▪ Bowel movements (normal, characteristics, pain/ difficulty) ▪ Dentures o Dysphagia ▪ Any difficulty swallowing? ▪ When first noticed? ▪ What makes it better? Worse? o Food intolerances ▪ Any foods you cannot eat? ▪ What happens if you eat them? ▪ Allergic reaction? Heartburn? Belching? Bloating? Indigestion? ▪ Use of antacids? How often? o Abdominal pain ▪ One spot or does it move? ▪ Constant or intermittent? Describe character ▪ Worse or relieved with food? ▪ Associated symptoms? ▪ What makes it better? ▪ What have you used to remedy the pain? ▪ A stomach ulcer (also called a peptic ulcer) is a small erosion (hole) in the gastrointestinal tract. The most common type, duodenal, occurs in the first 12 inches of small intestine beyond the stomach. Ulcers that form in the stomach are called gastric ulcers. An ulcer is not contagious or cancerous. Duodenal ulcers are almost always benign, while stomach ulcers may become malignant. ▪ Infection with the bacterium Helicobacter pylori is thought to play an important role in causing both gastric and duodenal ulcers. Helicobacter pylori may be transmitted from person to person through contaminated food and water. ▪ Another major cause of ulcers is the chronic use of anti-inflammatory medications, such as aspirin. Cigarette smoking is also an important cause of ulcer formation and ulcer treatment failure ▪ The major symptom of an ulcer is a burning or gnawing feeling in the stomach area that lasts between 30 minutes and 3 hours. This pain is often interpreted as heartburn, indigestion or hunger. The pain usually occurs in the upper abdomen, but sometimes it may occur below the breastbone. In some individuals the pain occurs immediately after eating. In other individuals, the pain may not occur until hours after eating. The pain frequently awakens the person at night. Weeks of pain may be followed by weeks of not having pain. Pain can be relieved by drinking milk, eating, resting, or taking antacids. o Nausea/ vomiting ▪ How often?How much? Color? Odor? ▪ Bloody? ▪ Associated with colicky pain, diarrhea, fever, chills? ▪ What have you eaten over last 24 hours? ▪ Anyone else with same symptoms? ▪ Hematemesis: The medical term for bloody vomitus. • The word "hematemesis" is made up of "hema-", blood + "emesis", vomit = bloody vomit o Bowel habits ▪ How often? ▪ Color? Consistency? ▪ Diarrhea or Constipation? How long? ▪ Any recent changes in bowel habits? ▪ Use of laxatives? • Medical Complications from Laxative Abuse o Laxative abuse is very taxing on the body and as such, it can result in a number of health complications. The severity of the following medical conditions is dependent on a number of criteria, specifically, the types and amounts of laxatives used as well as the length of time they were being used. The most common health conditions that arise from laxative abuse include: o Severe dehydration and electrolyte imbalances o Severe constipation or chronic diarrhea o Edema (swelling) o Blood in the stools which may cause anemia o Laxative dependency o Laxative abuse may result in an increased risk of colon cancer ▪ Who is at risk for colon cancer????? • Anyone can get colorectal cancer. But some people seem to be at a higher risk of this disease. • You may be at risk of getting colorectal cancer... o > if you have a condition called Crohn's disease o > if you are over 50 o > if a member of your family has had colon cancer o > if you have had cancer of the breast, ovary, or uterus o > if you smoke o > if you are overweight o > if you eat a diet that is high in fat and low in fiber • Possible signs o if you have more diarrhea or constipation than usual o if you see blood in your stool (the blood can be bright red or very dark to black in color) o if you see blood on your toilet paper after you have a bowel movement o if you always seem to feel full or bloated o if you always seem to have cramps or an upset stomach o if you have gas pains more often than usual o if you are losing weight without dieting o if you feel more tired than usual o if you notice any other changes in the way you feel • Reducing risk factors o Eat a variety of fruits and vegetables and whole grains each day o Cut back on foods that have a lot of fat (processed foods, fried foods, whole-milk dairy products, and snacks) o Quit smoking o Exercise every day by walking, swimming, bike riding, or other activity o Have regular checkups with your doctor * o Keep all of your doctor's appointments * o Colonoscopy at age 50 or earlier if family history o Past abdominal history ▪ GI problems? Ulcer? GB? Hepatitis? Jaundice? Appendicitis? Colitis? Hernia? ▪ Any surgeries? Describe? ▪ Any X-ray studies of abdomen? What kind? Do you know the results? o Medications ▪ What meds? Alcohol use? Smoking history? o Nutritional assessment ▪ 24 hour recall ▪ With Elderly: • How do you acquire groceries? • Do you eat alone? • Bowel Habits • Initial evaluation o When you walk in the room, what do you see? ▪ Comfortable- generally benign ▪ Writhing- renal or biliary colic ▪ Still- acute abdomen ▪ Fetal position- cramp GI • Important tests o Heel Tap ▪ Tap the heel hard, motion is transferred up to the muscles beneath the peritoneal cavity ▪ If pain is present, peritoneal sign ▪ Patient is supine o Obturator sign ▪ Flex hip and adduct across the abdomen ▪ If pain, peritoneal sign, due to inflammation to the obturator muscle lying underneath the peritoneal cavity ▪ Checking for appendicitis o Murphy’s sign ▪ Palpate deeply in the RUQ while patient inhales deeply ▪ Tenderness can indicate gallbladder disease o Guarding ▪ Press on abdomen, if muscles tighten, this is guarding ▪ Voluntary guarding is when patient makes their muscles flex (sometimes patient needs a distraction to evaluate accurately) o Rebound tenderness ▪ Press on abdomen and then release suddenly ▪ If pain is worse during the release, positive peritoneal sign o Iliopsoas muscle test ▪ Used when acute abdominal pain or appendicitis is suspected ▪ Lift R leg straight up, flexing at the hip then push down while having patient resist ▪ When test negative, person feels no change; when positive, pain felt in R lower quadrant o (listening for a bruit- should hear nothing) ▪ Aorta, renal, iliac, femoral • Quadrant evaluation o o All women from puberty to menopause with LQ pain are pregnant until proven otherwise • Pregnancy o • Referred pain from the abdomen o o • Physical examination of the abdomen o Facilitating the exam ▪ Employ measures that will enhance abdominal wall relaxation. ▪ If the abdomen is to be assessed accurately, patient relaxation is essential. The bladder must be empty, the room a comfortable temperature, the patient comfortable with knees supported, arms at the sides, and good lighting and visualization of the entire abdomen available o Approach ▪ From which side does the nurse approach the patient to conduct the physical examination? RIGHT SIDE ▪ What are the reasons for doing this? (LIVER, CARDIAC, MOST ARE RIGHT HANDED) o Inspect ▪ ▪ Describing contour of abdomen • Rounded, flat, scaphoid (sunken in), protruding • Striae o Stretch marks ▪ Red- new ▪ Silver-old • Surgical scars o Location, measure, describe healing, where scar is from • Noting scars ▪ Veins • Are they usually seen when examining the abdomen? • Prominent dilated veins occur with what disease entities? • Hypertension, portal hypertension, cirrhosis, ascites, vena cava obstruction, malnutrition o Findings on inspection ▪ Interpret findings obtained during inspection of the abdomen • Contour, symmetry, shape of the umbilicus, condition of the skin on the abdomen, and presence of pulsations or movement all must be observed during inspection of the abdomen. • The examiner must discriminate between normal and abnormal findings and use the information obtained through inspection as a basis for further exploration if indicated. The pattern of pubic hair growth and demeanor of the patient should be assessed with inspection. o Auscultation ▪ Interpret findings obtained during auscultation of the abdomen. • Auscultation of the abdomen is an important nursing assessment, especially for postoperative patients. Although the clicks of a normal bowel can occur anywhere from 5 to 30 times per minute, the nurse must listen for up to 5 minutes before deciding that bowel sounds are completely absent. In addition to bowel sounds, the examiner must note whether any vascular sounds or bruits are present. ▪ Hyperactive bowel sounds • • • o Percussion ▪ Reveals the relative density of the abdominal contents. ▪ Because of air in the intestines, tympany is the predominant sound. ▪ Dullness may be heard over a distended bladder, adipose tissue, fluid, or a mass. ▪ A change from lung resonance to dullness will identify the borders of the liver, which ranges from 6 to 12 cm in width and, on some individuals, splenic dullness, which is 7 cm in width or less, may be noted between the ninth to eleventh intercostal spaces behind the left midaxillary line. ▪ A change in tone may be noted over the descending colon if there is a need for evacuation. • Tympani: hallow sound • Over an organ: dull sound ▪ o Palpation ▪ Light and deep palpation provides the examiner with the ability to distinguish between normal organs, enlarged organs, abnormal masses, and unusual sensations elicited ▪ ▪ Looking for tenderness, facial expressions, voluntary or involuntary guarding ▪ Light palpation (one hand), deep palpation (two hands) ▪ Palpating the aorta (between umbilicus and xiphoid process) ▪ Palpating the liver • • Enlarged o Late portal cirrhosis, metastic CA, teritary syphilis ▪ Palapting the spleen • • Stopped by diaphargm, enlarges downward • Acute infection such as mono ▪ Palpating right kidney (pressing together) • • Enlarged kidney- hydronephrosis, cyst, neoplasm o Tests useful in special situations ▪ Rebound tenderness • Rebound is regarded as one of the classic local signs of peritonitis which can occur in diseases like appendicitis, and may occur in ulcerative colitis with rebound tenderness in the right lower quadrant. The others are tenderness and abdominal guarding. • However, in recent years the value of rebound tenderness has been questioned, since it may not add any diagnostic value beyond the observation that the patient has severe tenderness • Palpate deeply then quickly release, if in pain when releasing, rebound • Another name for this: Blumberg’s sign o Positive determines peritoneal inflammation ▪ Costovertebral angle tenderness • Associated with renal disease • Use heel of closed fist to strike patient firmly over costovertebral area ▪ Shifting dullness • Shifts when patient is rolled on one side, peritoneal fluid (ascites) may be present • What diseases present with ascites? o HF, portal HTN, cirrhosis, Hep, pancreatitis, cancer o Abnormal findings upon inspection ▪ Umbilical hernia • ▪ Epigastric hernia ▪ Incisional hernia ▪ Diastasis recti • Diastasis recti is a separation between the left and right side of the rectus abdominis muscle, which covers the front surface of the belly area. • Symptoms o A diastasis recti looks like a ridge, which runs down the middle of the belly area. It stretches from the bottom of the breastbone to the belly button, and increases with muscle straining. o In infants, the condition is most easily seen when the baby tries to sit up. It may not be seen when the child lies on the back and is relaxed. When the infant is relaxed, you can often feel the edges of the rectus muscles. o Diastasis recti is commonly seen in women who have multiple pregnancies, because the muscles have been stretched many times. Extra skin and soft tissue in the front of the abdominal wall may be the only signs of this condition in early pregnancy. In the later part of pregnancy, the top of the pregnant uterus is often seen bulging out of the abdominal wall. An outline of parts of the unborn baby may be seen in some severe cases. o Separation of the abdominal rectus muscle. Two out of three women experience a separation of the rectus abdominis muscle, the long muscle located in the middle of the abdomen, during their pregnancy. o Abnormal findings- auscultation ▪ Succession splash • The sound elicited by shaking the body of a person who has free fluid and air or gas in a hollow organ or body cavity. This sound may be present over a normal stomach but also may be heard with hydropneumothorax, large hiatal hernia, or intestinal or pyloric obstruction o Abnormal findings- palpation ▪ Obesity, air or gas, Ascites, ovarian cyst, Pregnancy, Feces, Tumor o Sample charting (subjective) ▪ States appetite is good with no recent change, no dysphagia, no food intolerance, no pain, no N/V. Has one formed BM/day. Takes vitamins, no other prescribed or OTC meds. No hx abdominal disease, injury, or surgery. • Objective o Inspection: flat, symmetric with no apparent masses. Skin smooth with no striae, scars, or lesions o Auscultation: BS present; no bruits o Percussion: Tympany predominates in all four quadrants o Palpation: Abdomen soft, no organomegaly, no masses, no tenderness Breast & Regional Lymphatics • Basics o Mammary glands o Present in both females and males (in men they are at a basic form throughout life) o Female breasts are accessory reproductive organs; function is to produce milk for nourishing newborn o Breast have extensive lymphatic drainage ▪ Most of lymph, more than 75%, drains into ipsilateral (same side) axillary nodes • • • • Lymphatics o Breast has extensive lymphatic drainage ▪ More than 75%, drains into ipsilateral axillary nodes o Four groups of axillary nodes are present ▪ Central axillary nodes: high up in middle of axilla, over ribs and serratus anterior muscle; receive lymph from other three groups of nodes ▪ Pectoral (anterior): along lateral edge of pectoralis major muscle, just inside anterior axillary fold ▪ Subscapular (posterior): along lateral edge of scapula, deep in posterior axillary fold ▪ Lateral: along the humerus, inside upper arm o • Male breasts o Rudimentary structure consisting of a thin disk of undeveloped tissue underlying nipple o Areola well developed, although nipple is small o Gynecomastia: during adolescence, it is common for breast tissue to temporarily enlarge ▪ Condition is usually unilateral and temporary ▪ Reassurance is necessary for adolescent male, whose attention is riveted on his body image ▪ Gynecomastia may reappear in aging male and may be due to testosterone deficiency • Development: adolescent o At puberty estrogen stimulates breast changes ▪ Onset of breast development occurred at an average (mean) age between 8 and 10 years ▪ Occasionally, one breast may grow faster than other, producing a temporary asymmetry ▪ *May cause some distress; reassurance is necessary ▪ Full development from stage 2 to stage 5 takes an average of 3 years (TANNER Staging) ▪ During this time, pubic hair develops, and axillary hair appears 2 years after onset of pubic hair • Sexual maturity rating in girls o Preadolescent o Breat bud stage o Breast and areolar enlarge o Breast and nipple form a secondary mound o Mature breast • Adolescent: Menarche o Beginning of breast development precedes menarche by about 2 years ▪ Menarche occurs in breast development stage 3 or 4, usually just after peak of adolescent growth spurt around age 12 ▪ Breasts of nonpregnant woman change with ebb and flow of hormones during monthly menstrual cycle ▪ Nodularity increases from midcycle up to menstruation ▪ During the 3 to 4 days before menstruation, breasts feel full, tight, heavy, and occasionally sore; breast volume is smallest on days 4 to 7 of menstrual cycle ▪ Can start palpating the breast 7 days after first period (won’t be enlarged then) • Development of pregnancy o Breast changes start during the second month of pregnancy and are an early sign for most women o Pregnancy stimulates expansion of ductal system and supporting fatty tissue as well as development of true secretory alveoli o Thus breasts enlarge and feel more nodular; nipples are larger, darker, and more erectile o Areolae become larger and grow darker brown as pregnancy progresses, and tubercles become more prominent o Venous pattern prominent over skin surface o Colostrum may be expressed after fourth month ▪ This thick yellow fluid is precursor for milk, containing same amount of protein and lactose, but practically no fat ▪ Breasts produce colostrum for first few days after delivery ▪ It is rich with antibodies that protect newborn against infection, so breastfeeding is important ▪ Lactation, milk production, begins 1 to 3 days post-partum; whitish color is from emulsified fat and calcium caseinate • Development: aging women o After menopause, ovarian secretion of estrogen and progesterone decreases, causing breast glandular tissue to atrophy ▪ This is replaced with fibrous connective tissue; fat envelope atrophies also, beginning in middle years and becoming marked in eighth and ninth decades ▪ These changes decrease breast size and elasticity so breasts droop and sag, looking flattened and flabby ▪ Drooping accentuated by kyphosis in some older women • Cultural competence o Incidence of breast cancer varies in cultural groups o African American women had a 36% higher death rate than white women o Racial difference in mortality may relate to insufficient use of early detection procedures, including mammograms and breast self-examinations o Factors contribute to breast health care access include low income, lack of health insurance, geographic, cultural, and language barriers, and racial bias • LGBT population o Greater risk for breast cancer than other women ▪ Not having children or having later in life ▪ Higher rates of obesity and alcohol use o Screening ▪ May not get routine screening tests- why? ▪ Transgender people ▪ Data on risk is limited • Subjective data o Breast ▪ Pain ▪ Lump ▪ Discharge ▪ Rash ▪ Swelling ▪ Trauma ▪ History of breast disease o General ▪ Surgery ▪ Self-care behaviors ▪ Perform breast self-examination ▪ Last mammogram o Axilla ▪ Tenderness, lump, or swelling ▪ Rash o Matters pertaining to breasts affect woman’s body image and generate emotional responses ▪ This emotionality may take strong forms that you observe as you discuss woman’s history ▪ Embarrassment may be evident ▪ A young adolescent is acutely aware of her own development in relation to her peers o A woman who has found a breast lump may come to you with fear, anxiety, and panic ▪ Although many breast lumps are benign, women initially assume worst possible outcome, including cancer, disfigurement, and death ▪ While you are collecting subjective data, tune in to cues for these behaviors that call for a reasoned and straightforward attitude o Pain ▪ Any pain or tenderness in breasts? When did you first notice it? ▪ Where is pain? Localized or all over? ▪ Is painful spot sore to touch? Do you feel a burning or pulling sensation? ▪ Is pain cyclic? Any relation to your menstrual period? ▪ Is pain brought on by strenuous activity, especially involving one arm; a change in activity; manipulation during sex; part of underwire bra; exercise? o Lump ▪ Ever noticed lump or thickening in breast? Where? ▪ When did you first notice it? Changed at all since then? ▪ Does lump have any relation to your menstrual period? ▪ Noticed any change in overlying skin: redness, warmth, dimpling, and swelling? o Discharge ▪ Any discharge from nipple? When did you first notice this? ▪ What color is discharge? ▪ Consistency; thick or runny? Odor? o Rash ▪ Any rash on breast? ▪ When did you first notice this? ▪ Where did it start? On the nipple, areola, or surrounding skin? o Swelling ▪ Any swelling in breasts? In one spot or all over? ▪ Related to your menstrual period, pregnancy, or breastfeeding? ▪ Any change in bra size? o Surgery ▪ Ever had surgery on the breasts? Was this a biopsy? What were the biopsy results? ▪ Mastectomy? Mammoplasty, augmentation, or reduction? ▪ Ever had mammography, a screening x-ray examination of breasts? When was last x-ray? o Self-care behaviors ▪ Have you ever been taught breast self-examination (SBE)? ▪ (If yes) How often do you perform it? What helps you remember? It is an excellent way to be in charge of your own health; I would like you to show me your technique after we do your examination ▪ (If not) This will be an excellent way that you can take charge of your own health; you can make breast self-examination a very routine health habit, just like brushing your teeth; I will teach you the technique after we do your examination • Breast cancer o Second major cause of death from cancer in women o However, early detection and improved treatment have increased survival rates o The 5-year survival rate for localized breast cancer has increased from 78% in 1940s to 98% today o If cancer has spread regionally, survival rate is 88% o Age increases risk o Age > 65 years o Inherited genetic mutations (BRCA1 & BRCA 2) o Mammographically dense breasts o First-degree relatives with breast cancer o More risk factors in Jarvis… • Objective data o General appearance ▪ Note symmetry of size and shape; common to have a slight asymmetry in size; often left breast is slightly larger than right o Skin ▪ Normally is smooth and of even color ▪ Note any localized areas of redness, bulging, or dimpling; also any skin lesions or focal vascular pattern ▪ Fine blue vascular network visible during pregnancy; pale linear striae, or stretch marks, follow pregnancy ▪ Normally no edema is present o Lymphatic drainage ▪ Observe axillary and supraclavicular regions; note any bulging, discoloration, or edema o Nipple ▪ Should be symmetrical on same plane on both breasts ▪ Nipples usually protrude, although some are flat and some are inverted ▪ Normal nipple inversion may be unilateral or bilateral and usually can be pulled out ▪ Note any dry scaling, any fissure or ulceration, and bleeding or other discharge o Maneuvers to screen for retraction ▪ Ask her to lift arms slowly over head; both breasts should move up symmetrically ▪ Next ask her to push her hands onto her hips and then to push her two palms together; these maneuvers contract pectoralis major muscle; slight lifting of both breasts will occur o Concerns ▪ Sudden increase in size ▪ Retraction of breast or nipple: growing neoplasm ▪ Fixation to chest wall ▪ Nipple discharge (abnormal unless pregnant or lactating) ▪ Lag in movement of one breast ▪ Edema, hyperpigmentation, inflammation o o Inspection ▪ Inspect and palpate the axillae • Examine axillae while woman is sitting o Palpation • Inspect skin, noting any rash or infection; lift woman’s arm and support it, so that her muscles are loose and relaxed; use right hand to palpate left axilla • Reach fingers high into axilla; move them firmly down in four directions • Move woman’s arm through range-of-motion to increase surface area you can reach • Usually nodes are not palpable, although you may feel a small, soft, non- tender node in central group • Note any enlarged and tender lymph nodes ▪ Tuck a small pad under side to be palpated and raise her arm over her head to flatten breast tissue and displace it medially; any significant lumps will then feel more distinct ▪ Use pads of your first three fingers and make a gentle rotary motion on breast; vary pressure palpating light, medium, and deep tissue in each location ▪ Vertical strip pattern currently recommended to detect a breast mass, but two other patterns are in common use: ▪ From the nipple palpating out to periphery as if following spokes on a wheel ▪ Palpating in concentric circles out to periphery ▪ ▪ In nulliparous (never had children) women, normal breast tissue feels firm, smooth, and elastic ▪ After pregnancy, tissue feels softer and looser ▪ Premenstrual engorgement is normal from increasing progesterone ▪ Consists of slight enlargement, tenderness to palpation, and generalized nodularity; lobes feel prominent and their margins more distinct ▪ If you feel a lump or mass, note characteristics • Location: as with clock face, describe distance in centimeters from nipple; or diagram breast in woman’s record and mark in location of lump • Size: judge in centimeters in three dimensions: width, length, and thickness • Shape: state whether lump is oval, round, lobulated, or indistinct • Consistency: state whether lump is soft, firm, or hard • Movable: is lump freely movable or fixed when you try to slide it over chest wall? • Distinctness: is lump solitary or multiple? • Nipple: is it displaced or retracted? • Note skin over lump: is it erythematous, dimpled, or retracted? • Tenderness: is lump tender to palpation? • Lymphadenopathy: are any regional lymph nodes palpable? • Teaching Breast Self-Exam (BSE) o Help each woman establish regular schedule of self-care o The best time to conduct BSE is right after menstrual period, when breasts are smallest and least congested o Advise pregnant or menopausal woman not having menstrual periods to select a familiar date to examine her breasts each month o Stress that self-examination will familiarize woman with her own breasts and their normal variation; emphasize absence of lumps (not the presence of them) o Encourage her to report any unusual finding promptly o Focus on positive aspects of BSE o Avoid citing frightening mortality statistics about breast cancer and generating excessive fear and denial that actually obstructs a woman’s self-care action o Majority of women will never get breast cancer o Great majority of breast lumps are benign o Early detection of breast cancer is important; if cancer is not invasive, survival rate close to 98% o Keep teaching simple (more likely to comply) o Describe correct technique and rationale and expected findings to note as woman inspects her own breasts o Teach woman to do this in front of a mirror while she is disrobed to waist o At home, she can start palpation in shower, where soap and water assist palpation o Then palpation should be performed while lying supine o Encourage woman to palpate her own breasts while you monitor her technique • Objective data: male breast o Examination of male breast can be abbreviated, but do not omit it o Combine breast exam with that of anterior thorax o Inspect chest wall, noting skin surface and any lumps or swelling o Palpate nipple area for any lump or tissue enlargement; it should feel even, with no nodules o Palpate axillary lymph nodes • Objective data: infants and adolescents o In neonate, breasts may be enlarged and visible due to maternal estrogen crossing placenta o May secrete a clear or white fluid, called “witch’s milk” o Breast development usually begins on an average between 8 and 10 years o Teach BSE now, so that technique will become a natural, comfortable habit by time girl becomes an adult Male & Female Genitailia: Anus, Rectum, Prostate • • • Developmental considerations o Infancy- undescended testes o Adolescents- Puberty begins between 9 to 13 years of age, development completed on average 3 years • Tanner stages of development o • Aging o No definite end to fertility, though will see decrease in sperm production o Pubic hair decreases & grey o Penis size decreases o Scrotum hangs lower • Cultural considerations o Circumcision- remove all/ part of foreskin o AAP- Health benefits outweigh risks o Risk for minor complications • Subjective Data: Health History Questions o Frequency, urgency, and nocturia o Dysuria o Hesitancy and straining o Urine color o Past genitourinary history o Penis o Scrotum o Sexual activity and contraceptive use o STD contact • Objective Data: Physical Exam o Preparation ▪ Position ▪ Apprehension regarding exam- Patient? RN? Both? o Equipment needed for RN exam ▪ Gloves ▪ Flashlight o Inspecting: penis ▪ Inspect, then palpate • Skin • Glans- smooth without lesions • Urethral meatus- central • Pubic hair- free of “pests” • Urethral discharge- lab analysis if any present • Shaft- smooth, firm, non-tender • Squeeze- checking for discharge o Scrotum ▪ Inspect, then palpate • Skin- swelling or lesions • Testis- gently palpate, oval shaped, bilateral • Epididymis- softer than the testes, smooth, nontender • Spermatic cord- smooth, nontender • Any mass • Note characteristics- tenderness, reduce when laying down • Transillumination- normally scrotal contents do not illuminate ▪ o Hernia ▪ Check for hernia—inspect, then palpate • Person standing and straining down • Palpation technique- palpate up the length of the spermatic cord, palpate for a bulge, does it easily reduce • Normal- feels nothing! ▪ Inguinal lymph nodes • Along the inguinal ligament • Vertical chain along the upper inner thigh • Testicular cancer o Most common cancer in young men 15 to 35 years o Early detection, almost 100% cure rate o No early symptoms o Important for patient to know what the body feels like o TSE (timing, shower, exam) • Subjective o Urinates times per day. Color is . No nocturia, dysuria, or hesitancy. No pain, lesions or discharge from penis. Does not perform TSE. No history of genitourinary-related disease. Sexually active with one partner x 5 years. States sexual life is satisfactory. Partner takes oral contraceptives. No known STI contacts. • Objective o No lesions, inflammation, or discharge from penis. Scrotum with descended testes that are symmetric. No palpable masses • Anus, rectum, prostate o o Structure and function: prostate ▪ Prostate gland • 2.5 cm long by 4 cm in diameter. • The gland lies in front of the anterior wall of the rectum and 2 cm behind the symphysis pubis • Surrounds the bladder neck • Secretes fluid that helps sperm viability o Developmental considerations ▪ Infants • Meconium • Nerves of the rectal area become myelinated at between 1½ and 2 years • Voluntary control of sphincter control at 18 mos. to 2 yrs.-”Potty training” can begin! ▪ Puberty • Prostate gland undergoes rapid increase in size and remains constant ▪ Middle Adult • Prostate starts to enlarge • PSA starting age 50 o Abnormalities ▪ o Subjective Data: Health History Questions ▪ Usual bowel routine ▪ Change in bowel habits ▪ Rectal bleeding or blood in the stool ▪ Medications ▪ Rectal conditions ▪ Family history ▪ Self-care behaviors o Objective Data: exam ▪ Preparation • Position: left lateral (male) • Female- supine, knees flexed (lithotomy) ▪ Equipment needed • Penlight • Lubricating jelly • Glove • Guaiac test container ▪ Inspection • Inspection of the perianal area o Skin- inflammation, lesions, scars o Anal opening- lesions, hemorrhoids, fissures o Valsalva maneuver- no break in skin integrity or protrusion through the anal opening • Palpation of the Anus and Rectum o Lubricant! o Palpation technique- ask patient to exhale, feel the sphincter tighten then relax, slowly insert- no jabbing! o Canal wall- smooth and even o Rectal wall- smooth and no nodularity ▪ Examine for occult blood o Fecal impaction ▪ Decreased bowel motility ▪ Constipation with diarrhea around the impaction o Documentation (subjective) ▪ BM per day (or per week). Soft, brown, no pain, no change in pattern. Takes no related medications. No history of pruritus, hemorrhoids, or fissure. Eats 1 serving of fruits and vegetables per day. No whole grains ▪ Objective • No hemorrhoids, fissure, or skin irritation in perianal area. Sphincter tone good. No prolapse. Rectal walls smooth. Prostate not enlarged. No masses or tenderness. Hematest negative • Female genitalia o o o o Structure and function ▪ Internal Genitalia • Vagina • Cervix • Uterus • Fallopian tubes • Ovaries ▪ Function of reproductive system • Manufactures ova for fertilization • Transports the fertilized ovum for implantation • Protects the fertilized embryo during development • Regulates hormone production • Serves as the female organ of copulation • Birth canal • Channel for the exit of menstrual flow o Puberty ▪ Estrogens stimulate the growth of cells in the reproductive tract and the development of secondary sex characteristics. ▪ First signs of puberty are breast and pubic hair development, beginning between the ages of 8½ to 13 years. ▪ Menarche occurs during the latter half of this sequence. ▪ Tanner’s table on the five stages of pubic hair development is helpful in teaching girls the expected sequence of sexual development.. • o Perimenopause- menopause ▪ Ages 35 to 60 years ▪ Ovarian function declines; the menses become farther apart and produce a lighter flow than usual. ▪ Uterus shrinks, ovaries atrophy (not able to palpate), uterus droops due to muscle weakness ▪ Cervix paler; vagina shorter and less elastic with pH more alkaline with fragile mucosa; vaginal dryness ▪ Pubic hair thin and sparse o Subjective Data: Health History Questions ▪ Menstrual history ▪ Obstetric history ▪ Menopause ▪ Self-care behaviors ▪ Urinary symptoms ▪ Vaginal discharge ▪ Past history ▪ Sexual activity ▪ Contraceptives ▪ STD’s o Objective Data: exam ▪ Preparation • Lithotomy position and draping • Measures to enhance comfort during exam ▪ Equipment • Gloves • Protective clothing for examiner • Goose-necked lamp with a strong light • Vaginal speculum of appropriate size • Large cotton-tipped applicators (rectal swabs) • Materials for cytologic study • Lubricant ▪ Internal Genitalia- bimanual examination • Palpation technique • Cervix • Consistency • Contour • Mobility • Uterus • Rectovaginal o Inspection ▪ o Palpation ▪ o Screenings ▪ Pap smear • cervical swab (checks for cancer) • Diseases o HPV (human papilloma virus) ▪ Painless warty growths, pink, flesh colored, may go unnoticed, occur around the vulva, anus, cervix, entrance of vagina ▪ Sexually active women • Charting o Subjective ▪ Menarche age 12, cycle lasts 30 days, duration 7 days, flow moderate, no dysmenorrhea. LMP January 5. G2/P2/Ab0. Last pap 1 year ago, negative. No urinary concerns, no foul-smelling vaginal discharge, no sores or lesions, no history of STDs. Takes oral contraceptives. Not aware of any exposure to STDs o Objective ▪ External genitalia: No swelling, lesions, or discharge ▪ Rectal: No hemorrhoids, fissures or lesions. Stool brown with guaiac negative stool ▪ Additional documentation may be needed according to extent of exam (p. 762) [Show More]
Last updated: 2 years ago
Preview 1 out of 53 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jul 13, 2021
Number of pages
53
Written in
Additional information
This document has been written for:
Uploaded
Jul 13, 2021
Downloads
0
Views
133