Food and Nutrition > PROJECT FINAL > Food Environments and Obesity: Household Diet Expenditure Versus Food Deserts. (All)
Food Environments and Obesity: Household Diet Expenditure Versus Food Deserts.
Document Content and Description Below
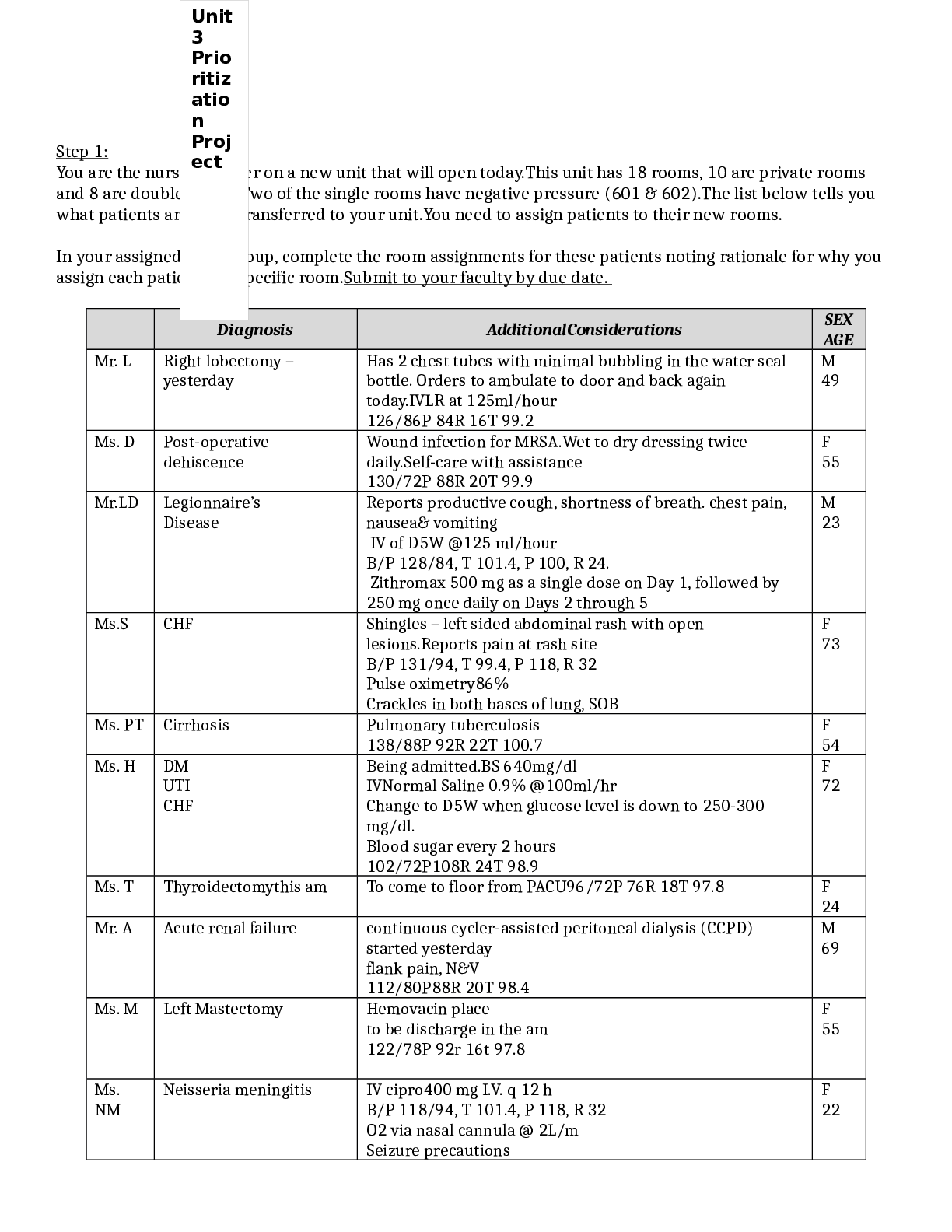
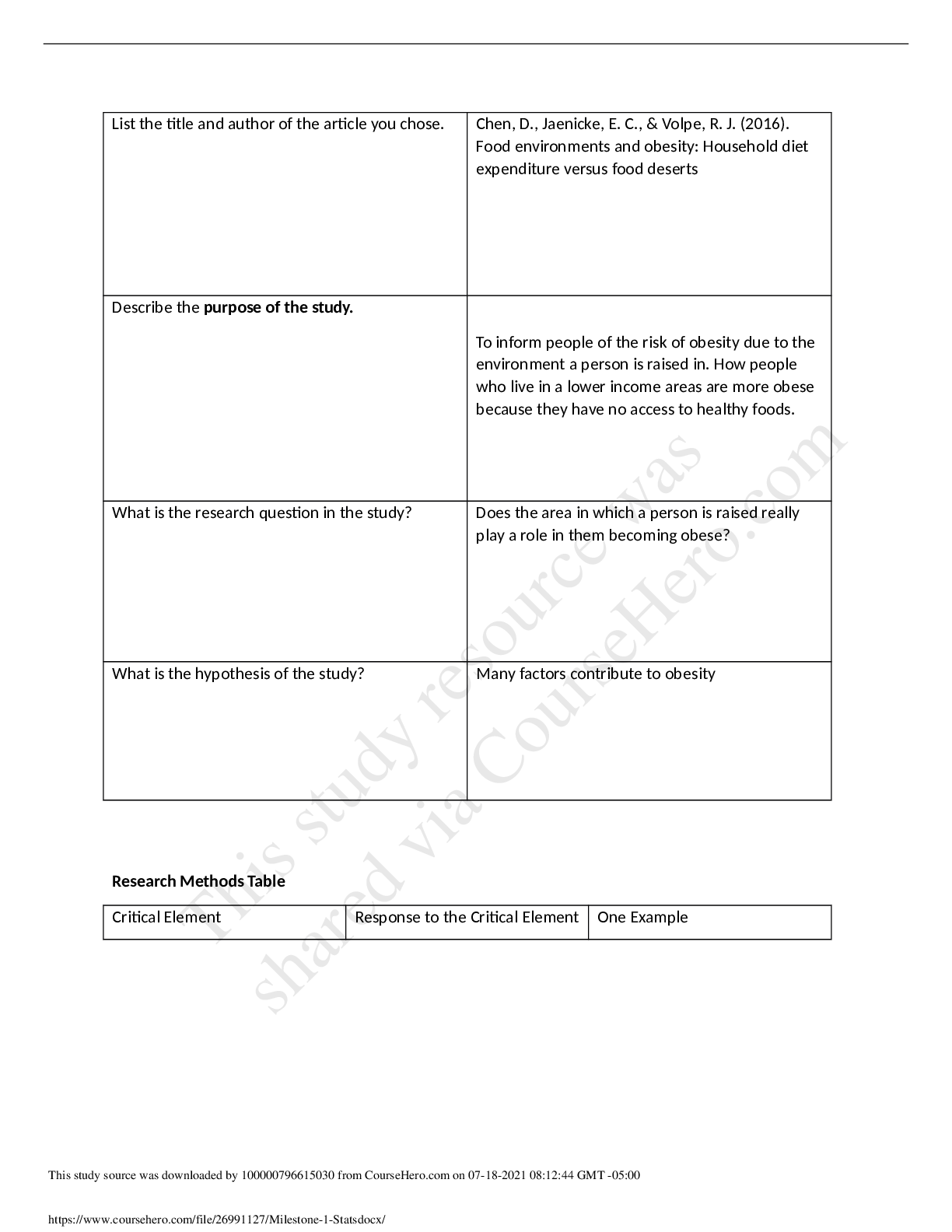
Authors: Danhong Chen; Jaenicke, Edward C.; Volpe, Richard J. Affiliation: Department of Agricultural Economics and Agribusiness, University of Arkansas, Fayetteville Department of Agricultural Ec... onomics, Sociology, and Education, Pennsylvania State University, University Park Agribusiness Department, California Polytechnic State University,San Luis Obispo Source: American Journal of Public Health (AM J PUBLIC HEALTH), May2016; 106(5): 881-888. (8p) Publication Type: Article Language: English Major Subjects: Obesity -- Psychosocial Factors Food -- Classification Diet Home Environment Residence Characteristics United States Department of Agriculture -- Standards Socioeconomic Factors Minor Subjects: Human; Descriptive Statistics; Body Mass Index; Factor Analysis; Data Analysis Software; Female; Male; Odds Ratio; Confidence Intervals;Pearson's Correlation Coefficient; Funding Source; Child, Preschool; Child; Adolescence; Young Adult; Adult; Middle Age; Aged; Aged, 80 and Over Abstract: Objectives. To examine the associations between obesity and multiple aspects of the food environments, at home and in the neighborhood. Methods. Our study included 38 650 individuals nested in 18 381 households located in 2104 US counties. Our novel home food environment measure, USDAScore, evaluated the adherence of a household's monthly expenditure shares of 24 aggregated food categories to the recommended values based on US Department of Agriculture food plans. The US Census Bureau's County Business Patterns (2008), the detailed food purchase information in the IRi Consumer Panel scanner data (2008-2012), and its associated MedProfiler data set (2012) constituted the main sources for neighborhood-, household-, and individual-level data, respectively. Results. After we controlled for a number of confounders at the individual, household, and neighborhood levels,USDAScore was negatively linked with obesity status, and a census tract-level indicator of food desert status was positively associated with obesity status. Conclusions. Neighborhood food environment factors, such as food desert status, were associated with obesity status even after we controlled for home food environment factors. Journal Subset: Biomedical; Core Nursing; Double Blind Peer Reviewed; Nursing; Peer Reviewed; Public Health; USA ISSN: 0090-0036 MEDLINE Info: NLM UID: 1254074 Grant Information: This research was partially funded by the US Department of Agriculture’s Economic Research Service. Entry Date: 20160511 Revision Date: 20160518 DOI: http://dx.doi.org.ezproxy.snhu.edu/10.2105/AJPH.2016.303048 Accession Number: 114349479 Database: CINAHL Complete Food Environments and Obesity: Household Diet Expenditure Versus Food Deserts Danhong ChenPhD, Edward C. JaenickePhD, and Richard J. VolpePhDAuthor affiliations, information, and correspondence details Accepted: December 20, 2015 Published Online: April 06, 2016 Objectives. To examine the associations between obesity and multiple aspects of the food environments, at home and in the neighborhood. Methods. Our study included 38 650 individuals nested in 18 381 households located in 2104 US counties. Our novel home food environment measure, USDAScore, evaluated the adherence of a household’s monthly expenditure shares of 24 aggregated food categories to the recommended values based on US Department of Agriculture food plans. The US Census Bureau’s County Business Patterns (2008), the detailed food purchase information in the IRi Consumer Panel scanner data (2008–2012), and its associated MedProfiler data set (2012) constituted the main sources for neighborhood-, household-, and individual-level data, respectively. Results. After we controlled for a number of confounders at the individual, household, and neighborhood levels, USDAScore was negatively linked with obesity status, and a census tract– level indicator of food desert status was positively associated with obesity status. Conclusions. Neighborhood food environment factors, such as food desert status, were associated with obesity status even after we controlled for home food environment factors. A number of recent studies have uncovered significant associations between the neighborhood food environment and health outcomes, particularly obesity status.1–6 Other studies, however, have found no such statistically significant relationships.7–10 Among those studies finding significant associations, it is most common to find obesity status or weight negatively related to supermarket counts,3–5 less common to find convenience store counts positively related,3 and rarer still to find club stores or supercenters positively related, with Courtemanche and Carden2 being one of the few studies that link supercenters to obesity. Finally, at least 1 study investigated the link between county-level obesity rates and the percentage of the county’s population living in food desert tracts, but it did not find a significant association.11 One explanati on for these mixed results centers on data measurement issues, with researchers’ measures of the built environment varying widely. Different measures include the number of food outlets within a predetermined area, 12–15 distance to the nearest food outlet, 9,16 and densiti es of food outlets in various forms. 8,17–21 Whereas some studies employed only 1 of these measures, others examined multi ple measures to investi gate the consistency of effects. 22–24 A second explanation for the mixed results centers on particular covariates included or missing from the analysis. Although 1 line of research focuses on the home food environment, few studies that focused on the neighborhood food environment also included covariates that described the home food environment. If covariates that accurately describe the home food environment are not accounted for, behavioral choices may possibly mask or confound associations between obesity and neighborhood food environment measures. Two reviews concluded that commonly used measures of food availability at home (which the reviews discussed in detail) had various limitations.25,26 Although open inventories examined by researchers can capture any type of food available at home, they are labor intensive and constrained by the time points of data collection.25 Other measures, such as predefined inventory checklists, food frequency questionnaires, and self-reported checklists, include a limited number of items, most of which focus on fruits and vegetables.25,26 In addition, a biomarker-based observational study27 indicated that both food frequency questionnaires and 24-hour recalls are subject to considerable measurement errors, and the bias is larger for food frequency questionnaires. The availability of household-level scanner data in multiple years enabled us to generate a comprehensive home food environment measure with an extended period of time and potentially less bias. This measure indicates households’ compliance with the US Department of Agriculture’s (USDA) recommended food purchase shares by food category, which are designed for households that would like to meet the Dietary Guidelines for Americans for at-home food consumption, even on a limited budget.28 In this sense, it is related to a substantial body of literature that examines the association between overall dietary patterns and various health outcomes. These studies’ findings are summarized in a number of review articles.29–33 A broader review of studies found that there is an inverse relationship between compliance with the Dietary Guidelines for Americans and obesity.34–36 By including a novel home food environment variable, as well as rich measures of the neighborhood food environment, our study addressed some of these confounding issues and other deficiencies in the literature. Following a number of related studies and research recommendations,1,37 our research was premised on the social environmental approach to health and health interventions, which places emphasis on how the health of individuals is influenced not only by biological and genetic functioning and predisposition, but also by social and familial relationships, environmental contingencies, and broader social and economic trends.38(p150) Our research, therefore, investigated how obesity and overweight status was influenced by (1) individual-level factors, including age, gender, and several self-reported behavior responses; (2) household-level factors, including race, ethnicity, education, income, and a home food environment measure that indicated the overall healthfulness of a household’s aggregate food-athome purchases; and (3) neighborhood-level factors, including county-level densities of various food store types, poverty rates, metro status, and a census tract–level indicator of food desert status as defined by the USDA. METHODS Section: We compiled a multilevel data set from several sources. Individual- and household-level data came from the IRi Consumer Panel and the IRi MedProfiler data. The Consumer Panel data reflected all food purchases from 2008 to 2012 by a representative set of US households that Choose recorded all their retail food purchases with a home-scanning device. Additionally, the IRi data contained a rich set of household-level demographics. The companion MedProfiler data set for 2012 contained self-reported responses on height, weight, health outcomes, and various behavioral questions for individuals in the IRi households matched by household ID. Neighborhood-level data came from various public sources. From the US Census Bureau’s County Business Patterns, we collected food store and restaurant establishment numbers at the county level. From the Census Bureau’s American Community Survey (2010–2012), we extracted population and poverty rate data. From the USDA, we collected county-level 2013 Rural–Urban Continuum Codes and census tract–level food desert information. Our full data set contained 38 650 individuals nested in 18 381 households located in 2104 counties of the United States. The actual sample size for analysis was slightly less because of missing observations for some of the variables. Obesity and Overweight Status Outcomes We calculated individuals’ body mass indexes (BMIs; defined as weight in kilograms divided by the square of height in meters) on the basis of IRi household members’ self-reported weights and heights ([weight in pounds/(height in inches)2 ] × 703). On the basis of our BMI calculations, we constructed indicator variables for obesity and overweight status using different criteria for adults and children. For adults aged 18 years and older, overweight status was a binary variable, with 1 indicating overweight status (25 ≤ BMI < 30) and 0 indicating underweight or normal- weight status (BMI < 25). Similarly, obesity status was a binary variable, with 1 indicating obesity (BMI ≥ 30) and 0 indicating underweight or normal-weight status (BMI < 25). For children aged 2 to 17 years, we obtained age- and gender-specific BMI percentile values from the Centers for Disease Control and Prevention.39 We categorized children with BMIs lower than the 85th percentile for their age and gender as being underweight or normal weight, those with BMIs greater than or equal to the 85th percentile but lower than the 95th percentile as overweight, and those with BMIs greater than or equal to the 95th percentile as obese.40 Individual-Level Variables “Diet feature” was a factor analysis score constructed from 7 MedProfiler questions related to special diets, including high-fiber, high-protein, low-calorie, low-carbohydrate, low-fat, low-salt, and low-sugar diets. All responses to these dietary features were either yes (coded as 1) or no (0). Additional covariates included individuals’ age, gender, whether they ate at a fast-food restaurant on most days of a week (“fast food”), and whether they exercised for at least 20 minutes per day on most days of a week (“exercise”). Household-Level Variables Household-level demographic characteristics, including race/ethnicity, household size, income, education, and marital status, were available directly from the IRi Consumer Panel. One of the main household-level measures in our analysis, USDAScore, reflected the home food environment and was constructed from the detailed food purchase information in the IRi Consumer Panel. Following Volpe and Okrent,28 USDAScore measured adherence of a household’s monthly expenditure shares of 24 aggregated food categories—defined by the USDA’s Center for Nutrition Policy and Promotion (CNPP)—to the recommended values based on USDA food plans. We calculated the USDAScore by a squared-error loss function: where is the recommended household-specific food expenditure share for household j in CNPP food category f and is household j’s actual expenditure share in category f in month m. The recommended shares varied across households depending on household demographics, which included the age of male household head, age of female household head, and presence and age of children. Table 1 lists the 24 food categories and shows how the expenditure shares based on USDA food plan recommendations for each category compared with observed average expenditures in the sample. Further explanation of this score can be found in Volpe and Okrent.28 In this study, we used the 5-year average of the monthly scores (USDAScore) for households that stayed in the IRi panel from 2008 to 2012, thus emphasizing the long-term impact that the at-home food environment might have on obesity. TABLE 1—USDA Recommended Expenditure Shares for 24 Aggregated Food Categories, and Average Expenditure Shares in the IRi Consumer Panel (2008–2012): United States TABLE 1—USDA Recommended Expenditure Shares for 24 Aggregated Food Categories, and Average Expenditure Shares in the IRi Consumer Panel (2008–2012): United States Food Category DGA Recommended or Recommended With Limited Consumption USDA Recommended Expenditure Sharesa Mean Monthly Expenditure Shares per Householdb Grains Wholegrain productsc Recommended 10.09 2.82 Non– whole-grain productsd Limited 6.10 20.61 Food Category DGA Recommended or Recommended With Limited Consumption USDA Recommended Expenditure Sharesa Mean Monthly Expenditure Shares per Householdb Vegetables All potato products Recommended 1.77 1.85 Dark-green vegetables Recommended 5.59 0.50 Orange vegetables Recommended 2.61 0.06 Canned and dry beans, lentils, and peas (legumes) Recommended 8.32 0.99 Other vegetables Recommended 8.66 2.71 Fruits Whole fruits Recommended 16.49 1.50 Fruit juices Recommended 1.86 2.26 Milk products Wholemilk productse Limited 0.86 5.38 Lower fat and skim milk and low-fat yogurt Recommended 8.77 5.46 All cheese (including cheese soup and sauce) Limited 0.60 4.85 Food Category DGA Recommended or Recommended With Limited Consumption USDA Recommended Expenditure Sharesa Mean Monthly Expenditure Shares per Householdb Meat and beans Beef, pork, veal, lamb, and game Limited 5.31 0.48 Chicken, turkey, and game birds Recommended 2.69 1.69 Fish and fish products Recommended 11.92 2.06 Bacon, sausages, and luncheon meats (including spreads) Limited 0.91 5.29 Nuts, nut butters, and seeds Recommended 3.16 2.77 Eggs and egg mixtures Recommended 0.12 1.40 Other foods Fats and condimentsf Limited 1.79 7.86 Coffee and tea Recommended 0.02 3.71 Soft drinks, sodas, fruit drinks, and ades (including rice Limited 1.33 6.46 Food Category DGA Recommended or Recommended With Limited Consumption USDA Recommended Expenditure Sharesa Mean Monthly Expenditure Shares per Householdb beverages) Sugars, sweets, and candies Limited 0.41 8.10 Soups (ready-toserve and condensed soups, dry soups) Limited 0.51 2.17 Frozen or refrigerated entrees (including pizza, fish sticks, and frozen meals) Limited 0.18 9.02 Note. DGA = Dietary Guidelines for Americans; USDA = US Department of Agriculture. aThe USDA recommended shares are based on the recommended dollar costs of feeding a representative family consisting of 1 male and 1 female aged 19–50 years, 1 child aged 9–11 years, and 1 child aged 6–8 years, according to the Liberal Food Plan.28 bAverage expenditure shares were calculated on the basis of all the households (n = 18 381) included in this study. c Includes whole-grain breads, rice, pasta, and pastries (including whole-grain flours); wholegrain cereals (including hot cereal mixes); and popcorn and other whole-grain snacks. d Includes non–whole-grain breads, cereals, rice, pasta, pies, pastries, snacks, and flours. e Includes whole milk, yogurt, cream, milk drinks, and milk desserts. f Includes table fats, oils, salad dressings, gravies, sauces, condiments, and spices. Neighborhood-Level Variables We collected data on the average number of food stores or restaurants per 10 000 county residents. Definitions and specific examples of each category can be found in Morland et al.41 We extracted numbers of establishments from the 2008 County Business Patt [Show More]
Last updated: 2 years ago
Preview 1 out of 24 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$7.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jul 18, 2021
Number of pages
24
Written in
Additional information
This document has been written for:
Uploaded
Jul 18, 2021
Downloads
0
Views
167