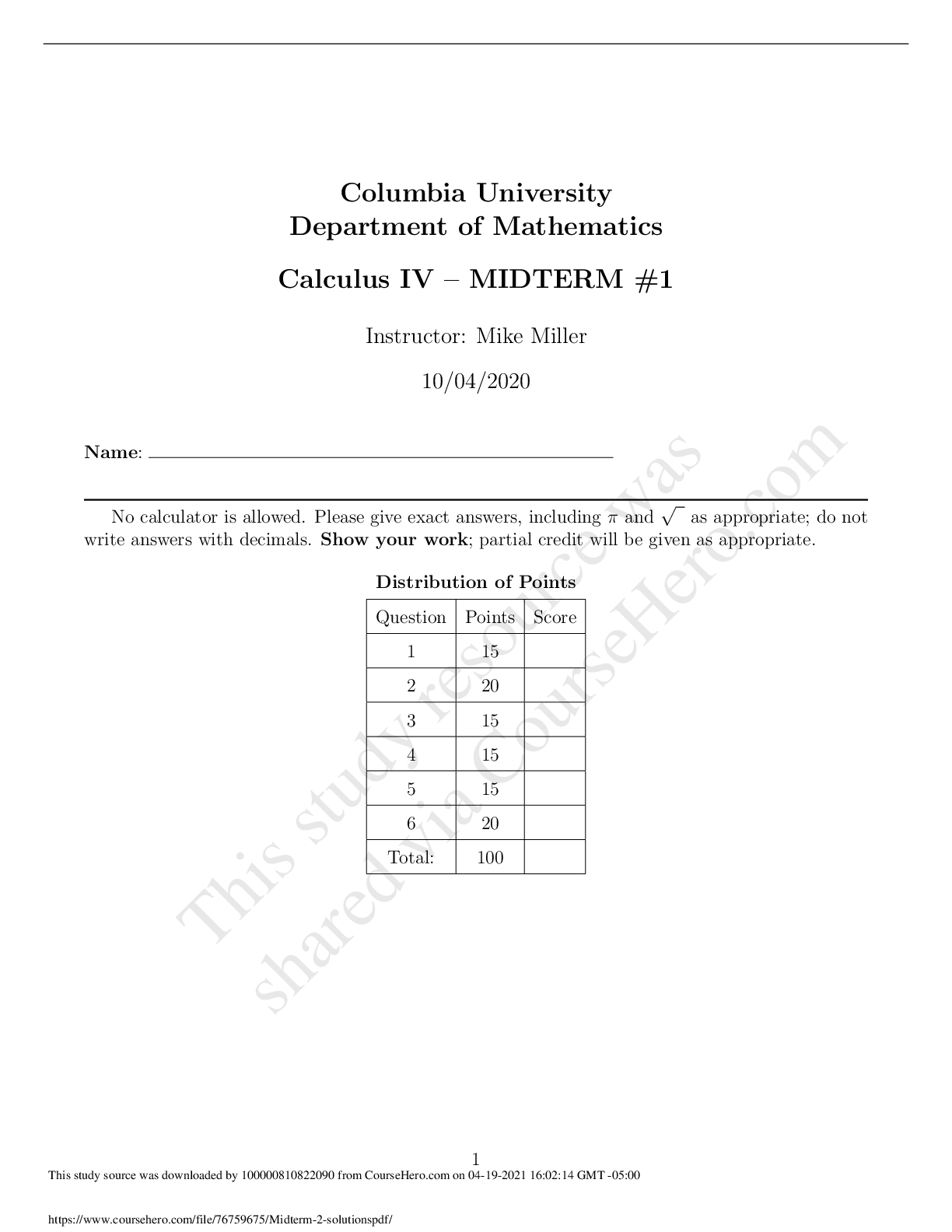
Exam 3 unit tests. Questions and Answer
Document Content and Description Below
Both men and women experience bone loss with aging. The bones most likely to demonstrate significant loss are:
A.
Cortical bone
B.
Femoral neck
C.
Cervical vertebrae
D.
Pelvic bones
Bisphos
...
phonates treat or prevent osteoporosis by:
A.
Inhibiting osteoclastic activity
B.
Fostering bone resorption
C.
Enhancing calcium uptake in bone
D.
Strengthening the osteoclastic proton pump
Prophylactic use of bisphosphonates is recommended for patients with early osteopenia related to long-term use of which of the following drugs?
A.
Selective estrogen receptor modulators
B.
Aspirin
C.
Glucocorticoids
D.
Calcium supplements
Patients with cystic fibrosis are often prescribed enzyme replacement for pancreatic secretions. Each replacement drug has lipase, protease, and amylase components, but the drug is prescribed in units of:
A.
Lipase
B.
Protease
C.
Amylase
D.
Pancreatin
Brands of pancreatic enzyme replacement drugs are:
A.
Bioequivalent
B.
About the same in cost per unit of lipase across brands
C.
Able to be interchanged between generic and brand-name products to reduce cost
D.
None of the above
When given subcutaneously, NPH insulin begins to take effect (onset of action):
A.
15 to 30 minutes after administration
B.
60 to 90 minutes after administration
C.
3 to 4 hours after administration
D.
6 to 8 hours after administration
Hypoglycemia can result from the action of either insulin or an oral hypoglycemic. Signs and symptoms of hypoglycemia include:
A.
“Fruity” breath odor and rapid respiration
B.
Diarrhea, abdominal pain, weight loss, and hypertension
C.
Dizziness, confusion, diaphoresis, and tachycardia
D.
Easy bruising, palpitations, cardiac dysrhythmias, and coma
Nonselective beta blockers and alcohol create serious drug interactions with insulin because they:
A.
Increase blood glucose levels
B.
Produce unexplained diaphoresis
C.
Interfere with the ability of the body to metabolize glucose
D.
Mask the signs and symptoms of altered glucose levels
Lipro is an insulin analogue produced by recombinant DNA technology. Which of the following statements about this form of insulin is NOT true?
A.
Optimal time of preprandial injection is 15 minutes.
B.
Duration of action is increased when the dose is increased.
C.
It is compatible with NPH insulin.
D.
It has no pronounced peak.
The decision may be made to switch from BID NPH insulin to insulin glargine to improve glycemia control throughout the day. If this is done:
A.
The initial dose of glargine is reduced by 20% to avoid hypoglycemia
B.
The initial dose of glargine is 2 to 10 Units per day
C.
Patients who have been on high doses of NPH will need tests for insulin antibodies
D.
Obese patients may require more than 100 Units per day
When blood glucose levels are difficult to control in Type 2 diabetes some form of insulin may be added to the treatment regimen to control blood glucose and limit complications risks. Which of the following statements are accurate based on research?
A.
Premixed insulin analogues are better at lowering HbA1C and have less risk for hypoglycemia.
B.
Premixed insulin analogues and the newer premixed insulins are associated with more weight gain than the oral antidiabetic agents.
C.
Newer premixed insulins are better at lowering HbA1C and post-prandial glucose levels than are long-acting insulins.
D.
Patients who are not controlled on oral agents and have post-prandial hyperglycemia can have NPH insulin added at bedtime.
C.
Newer premixed insulins are better at lowering HbA1C and post-prandial glucose levels than are long-acting insulins.
Metformin is a primary choice of drug to treat hyperglycemia in Type 2 diabetes because it:
A.
Substitutes for insulin usually secreted by the pancreas
B.
Decreases glycogenolysis by the liver
C.
Increases the release of insulin from beta cells
D.
Decreases peripheral glucose utilization
Prior to prescribing metformin, the provider should:
A.
Draw a serum creatinine to assess renal function
B.
Try the patient on insulin
C.
Tell the patient to increase iodine intake
D.
Have the patient stop taking any sulfonylurea to avoid dangerous drug interactions
The action of “gliptins” is different from other antidiabetic agents because they:
A.
Have a low risk for hypoglycemia
B.
Are not associated with weight gain
C.
Close ATP-dependent potassium channels in the beta cell
D.
Act on the incretin system to indirectly increase insulin production
Sitagliptin has been approved for:
A.
Monotherapy in once daily doses
B.
Combination therapy with metformin
C.
Both A and B
D.
Neither A nor B
GLP-1 agonists:
A.
Directly bind to a receptor in the pancreatic beta cell
B.
Have been approved for monotherapy
C.
Speed gastric emptying to decrease appetite
D.
Can be given orally once daily
Avoid concurrent administration of exenatide with which of the following drugs?
A.
Digoxin
B.
Warfarin
C.
Lovastatin
D.
All of the above
Administration of exenatide is by subcutaneous injection:
A.
30 minutes prior to the morning meal
B.
60 minutes prior to the morning and evening meal
C.
15 minutes after the evening meal
D.
60 minutes before each meal daily
Potentially fatal granulocytopenia has been associated with treatment of hyperthyroidism with propylthiouracil. Patients should be taught to report:
A.
Tinnitus and decreased salivation
B.
Fever and sore throat
C.
Hypocalcemia and osteoporosis
D.
Laryngeal edema and difficulty swallowing
Elderly patients who are started on levothyroxine for thyroid replacement should be monitored for:
A.
Excessive sedation
B.
Tachycardia and angina
C.
Weight gain
D.
Cold intolerance
ACE inhibitors are a central part of the treatment of heart failure because they have more than one action to address the pathological changes in this disorder. Which of the following pathological changes in heart failure is NOT addressed by ACE inhibitors?
A.
Changes in the structure of the left ventricle so that it dilates, hypertrophies, and uses energy less efficiently.
B.
Reduced formation of cross-bridges so that contractile force decreases.
C.
Activation of the sympathetic nervous system that increases heart rate and preload.
D.
Decreased renal blood flow that decreases oxygen supply to the kidneys.
One of the three types of heart failure involves systolic dysfunction. Potential causes of this most common form of heart failure include:
A.
Myocardial ischemia and injury secondary to myocardial infarction
B.
Inadequate relaxation and loss of muscle fiber secondary to valvular dysfunction
C.
Increased demands of the heart beyond its ability to adapt secondary to anemia
D.
Slower filling rate and elevated systolic pressures secondary to uncontrolled hypertension
The American Heart Association and the American College of Cardiology have devised a classification system for heart failure that can be used to direct treatment. Patients with symptoms and underlying disease are classified as:
A.
Stage A
B.
Stage B
C.
Stage C
D.
Stage D
Diagnosis of heart failure cannot be made by symptoms alone since many disorders share the same symptoms. The most specific and sensitive diagnostic test for heart failure is:
A.
Chest x-rays that show cephalization and measure heart size
B.
Two-dimensional echocardiograms that identify structural anomalies and cardiac dysfunction
C.
Complete blood count, BUN, and serum electrolytes that facilitate staging for end-organ damage
D.
Two-dimensional echocardiograms that identify structural anomalies and cardiac dysfunction
Treatments for heart failure, including drug therapy, are based on the stages developed by the ACC/AHA. Stage A patients are treated with:
A.
Drugs for hypertension and hyperlipidemia, if they exist
B.
Lifestyle management including diet, exercise, and smoking cessation only
C.
ACE inhibitors to directly affect the heart failure only
D.
No drugs are used in this early stage
Class I recommendations for Stage A heart failure include:
A.
Aerobic exercise within tolerance levels to prevent the development of heart failure
B.
Reduction of sodium intake to less than 2,000 mg/day to prevent fluid retention
C.
Beta blockers for all patients regardless of cardiac history
D.
Treatment of thyroid disorders, especially if they are associated with tachyarrhythmias
Stage B patients should have beta blockers added to their heart failure treatment regimen when:
A.
They have an ejection fraction less than 40%
B.
They have had a recent MI
C.
Both A and B
D.
Neither A nor B
C.
Both A and B
Increased life expectancy for patients with heart failure has been associated with the use of:
A.
ACE inhibitors, especially when started early in the disease process
B.
All beta blockers regardless of selectivity
C.
Thiazide and Loop diuretics
D.
Cardiac glycosides
A.
ACE inhibitors, especially when started early in the disease process
Stage C patients usually require a combination of three to four drugs to manage their heart failure. In addition to ACE inhibitors and beta blockers, diuretics may be added. Which of the following statements about diuretics is NOT true?
A.
Diuretics reduce preload associated with fluid retention.
B.
Diuretics can be used earlier than Stage C when the goal is control of hypertension.
C.
Diuretics may produce problems with electrolyte imbalances and abnormal glucose and lipid metabolism.
D.
Diuretics from the potassium-sparing class should be used when using an ARB.
D.
Diuretics from the potassium-sparing class should be used when using an ARB.
Digoxin has a very limited role in treatment of heart failure. It is used mainly for patients with:
A.
Ejection fractions above 40%
B.
An audible S3
C.
Mitral stenosis as a primary cause for heart failure
D.
Renal insufficiency
B.
An audible S3
Which of the following classes of drugs is contraindicated in heart failure?
A.
Nitrates
B.
Long-acting dihydropyridines
C.
Calcium channel blockers
D.
Alpha-beta blockers
C.
Calcium channel blockers
Heart failure is a leading cause of death and hospitalization in older adults (greater than 65 years old). The drug of choice for this population is:
A.
Aldosterone antagonists
B.
Eplerenone
C.
ACE inhibitors
D.
ARBs
C.
ACE inhibitors
ACE inhibitors are contraindicated in pregnancy. While treatment of heart failure during pregnancy is best done by a specialist, which of the following drug classes are considered to be safe, at least in the later parts of pregnancy?
A.
Diuretics
B.
ARBs
C.
Beta blockers
D.
Nitrates
C.
Beta blockers
Heart failure is a chronic condition that can be adequately managed in primary care. However, consultation with or referral to a cardiologist is appropriate when:
A.
Symptoms markedly worsen or the patient becomes hypotensive and has syncope
B.
There is evidence of progressive renal insufficiency or failure
C.
The patient remains symptomatic on optimal doses of an ACE inhibitor, a beta blocker, and a diuretic
D.
Any of the above
D.
Any of the above
Digoxin levels need to be monitored closely when the following medication is started:
A.
Loratadine
B.
Diphenhydramine
C.
Ipratropium
D.
Albuterol
D.
Albuterol
Patients with pheochromocytoma should avoid which of the following classes of drugs due to the possibility of developing hypertensive crisis?
A.
Expectorants
B.
Beta-2-agonists
C.
Antitussives
D.
Antihistamines
B.
Beta-2-agonists
Harold, a 42-year-old African American, has moderate persistent asthma. Which of the following asthma medications should be used cautiously, if at all?
A.
Betamethasone, an inhaled corticosteroid
B.
Salmeterol, an inhaled long-acting beta-agonist
C.
Albuterol, a short-acting beta-agonist
D.
Montelukast, a leukotriene modifier
B.
Salmeterol, an inhaled long-acting beta-agonist
Long-acting beta-agonists (LTBAs) received a Black Box warning from the U.S. Food and Drug Administration due to the:
A.
Risk of life-threatening dermatological reactions
B.
Increased incidence of cardiac events when LTBAs are used
C.
Increased risk of asthma-related deaths when LTBAs are used
D.
Risk for life-threatening alterations in electrolytes
C.
Increased risk of asthma-related deaths when LTBAs are used
The bronchodilator of choice for patients taking propranolol is:
A.
Albuterol
B.
Pirbuterol
C.
Formoterol
D.
Ipratropium
D.
Ipratropium
James is a 52-year-old overweight smoker taking theophylline for his persistent asthma. He tells his provider he is going to start the Atkin’s diet for weight loss. The appropriate response would be:
A.
Congratulate him on making a positive change in his life
B.
Recommend he try stopping smoking instead of the Atkin’s diet
C.
Schedule him for regular serum theophylline levels during his diet due to increased excretion of theophylline
D.
Decrease his theophylline dose because a high-protein diet may lead to elevated theophylline levels
C.
Schedule him for regular serum theophylline levels during his diet due to increased excretion of theophylline
i takes theophylline for his persistent asthma and calls the office with a complaint of nausea, vomiting, and headache. The best advice for him would be to:
A.
Reassure him this is probably a viral infection and should be better soon
B.
Have him seen the same day for an assessment and theophylline level
C.
Schedule him for an appointment in 2 to 3 days, which he can cancel if he is better
D.
Order a theophylline level at the lab for him
B.
Have him seen the same day for an assessment and theophylline level
Tiotropium bromide (Spiriva) is an inhaled anticholinergic:
A.
Used for the treatment of COPD
B.
Used in the treatment of asthma
C.
Combined with albuterol for treatment of asthma exacerbations
D.
Combined with fluticasone for the treatment of persistent asthma
A.
Used for the treatment of COPD
Christy has exercise and mild persistent asthma and is prescribed two puffs of albuterol 15 minutes before exercise and as needed for wheezing. One puff per day of beclomethasone (QVAR) is also prescribed. Teaching regarding her inhalers includes:
A.
Use one to two puffs of albuterol per day to prevent an attack with no more than eight puffs per day
B.
Beclomethasone needs to be used every day to treat her asthma
C.
Report any systemic side effects she is experiencing, such as weight gain
D.
Use the albuterol MDI immediately after her corticosteroid MDI to facilitate bronchodilation
B.
Beclomethasone needs to be used every day to treat her asthma
When prescribing montelukast (Singulair) for asthma, patients or parents of patients should be instructed:
A.
Montelukast twice a day is started when there is an asthma exacerbation
B.
Patients may experience weight gain on montelukast
C.
Aggression, anxiety, depression, and/or suicidal thoughts may occur when taking montelukast
D.
Lethargy and hypersomnia may occur when taking montelukast
C.
Aggression, anxiety, depression, and/or suicidal thoughts may occur when taking montelukast
Montelukast (Singulair) may be prescribed for:
A.
A 6 year old with exercise-induced asthma
B.
A 2 year old with moderate persistent asthma
C.
An 18 month old with seasonal allergic rhinitis
D.
None of the above; montelukast is not approved for use in children
B.
A 2 year old with moderate persistent asthma
The known drug interactions with the inhaled corticosteroid beclomethasone (QVAR) include:
A.
Albuterol
B.
MMR vaccine
C.
Insulin
D.
None of the above
D.
None of the above
When educating patients who are starting on inhaled corticosteroids, the provider should include:
A.
They need to get any live vaccines before starting the medication.
B.
Inhaled corticosteroids need to be used daily during asthma exacerbations to be effective.
C.
Patients should rinse their mouths out after using the inhaled corticosteroid to prevent thrush.
D.
They can triple the dose number of inhalations of medication during colds to prevent needing systemic steroids.
C.
Patients should rinse their mouths out after using the inhaled corticosteroid to prevent thrush
Patients with allergic rhinitis may benefit from a prescription of:
A.
Fluticasone (Flonase)
B.
Cetirizine (Zyrtec)
C.
OTC cromolyn nasal spray (Nasalcrom)
D.
Any of the above
D.
Any of the above
____15.Howard is a 72-year-old male who occasionally takes diphenhydramine for his seasonal allergies. Monitoring for this patient taking diphenhydramine would include assessing for:
A.
Urinary retention
B.
Cardiac output
C.
Peripheral edema
D.
Skin for rash
A.
Urinary retention
First generation antihistamines such as loratadine (Claritin) are prescribed for seasonal allergies because they are:
A.
More effective than first generation antihistamines
B.
Less sedating than the first generation antihistamines
C.
Prescription products, therefore are covered by insurance
D.
Able to be taken with CNS sedatives, such as alcohol
B.
Less sedating than the first generation antihistamines
When recommending dimenhydrinate (Dramamine) to treat motion sickness, patients should be instructed to:
A.
Take the dimenhydrinate after they get nauseated
B.
Drink lots of water while taking the dimenhydrinate
C.
Take the dimenhydrinate 15 minutes before it is needed
D.
Double the dose if one tablet is not effective
C.
Take the dimenhydrinate 15 minutes before it is needed
Decongestants such as pseudoephedrine (Sudafed):
A.
Are Schedule III drugs in all states
B.
Should not be prescribed or recommended for children under 4 years of age
C.
Are effective in treating the congestion children experience with the common cold
D.
May cause drowsiness in patients of all ages
B.
Should not be prescribed or recommended for children under 4 years of age
Cough and cold medications that contain a sympathomimetic decongestant such as phenylephrine should be used cautiously in what population:
A.
Older adults
B.
Hypertensive patients
C.
Infants
D.
All of the above
D.
All of the above
Martin is a 60 year old with hypertension. The first-line decongestant to prescribe would be:
A.
Oral pseudoephedrine
B.
Oral phenylephrine
C.
Nasal oxymetazoline
D.
Nasal azelastine
C.
Nasal oxymetazoline
The first-line treatment for cough related to a URI in a 5 year old is:
A.
Fluids and symptomatic care
B.
Dextromethorphan and guaifenesin syrup (Robitussin DM for Kids)
C.
Guaifenesin and codeine syrup (Tussin AC)
D.
Chlorpheniramine and dextromethorphan syrup (Nyquil for Kids)
A.
Fluids and symptomatic care
Prior to developing a plan for the treatment of asthma, the patient’s asthma should be classified according to the NHLBI Expert Panel 3 guidelines. In adults mild-persistent asthma is classified as asthma symptoms that occur:
A.
Daily
B.
Daily and limit physical activity
C.
Less than twice a week
D.
More than twice a week and less than once a day
D.
More than twice a week and less than once a day
In children age 5 to 11 years mild-persistent asthma is diagnosed when asthma symptoms occur:
A.
At nighttime one to two times a month
B.
At nighttime three to four times a month
C.
Less than twice a week
D.
Daily
B.
At nighttime three to four times a month
One goal of asthma therapy outlined by the NHLBI Expert Panel 3 guidelines is:
A.
Ability to use albuterol daily to control symptoms
B.
Minimize exacerbations to once a month
C.
Keep nighttime symptoms at a maximum of twice a week
D.
Require infrequent use of beta 2 agonists (albuterol) for relief of symptoms
D.
Require infrequent use of beta 2 agonists (albuterol) for relief of symptoms
A stepwise approach to the pharmacologic management of asthma:
A.
Begins with determining the severity of asthma and assessing asthma control
B.
Is used when asthma is severe and requires daily steroids
C.
Allows for each provider to determine their personal approach to the care of asthmatic patients
D.
Provides a framework for the management of severe asthmatics, but is not as helpful when patients have intermittent asthma
A.
Begins with determining the severity of asthma and assessing asthma control
Treatment for mild intermittent asthma is:
A.
Daily inhaled medium dose corticosteroids
B.
Short-acting beta-2-agonists (albuterol) as needed
C.
Long-acting beta-2-agonists every morning as a preventative
D.
Montelukast (Singulair) daily
B.
Short-acting beta-2-agonists (albuterol) as needed
The first-line therapy for mild-persistent asthma is:
A.
High-dose montelukast
B.
Theophylline
C.
Low-dose inhaled corticosteroids
D.
Long-acting beta-2-agonists
C.
Low-dose inhaled corticosteroids
Monitoring a patient with persistent asthma includes:
A.
Monitoring how frequently the patient has a URI during treatment
B.
Monthly in-office spirometry testing
C.
Determining if the patient has increased use of his or her long-acting beta-2-agonist due to exacerbations
D.
Evaluating the patient every 1 to 6 months to determine if the patient needs to step up or down in their therapy
D.
Evaluating the patient every 1 to 6 months to determine if the patient needs to step up or down in their therapy
Asthma exacerbations at home are managed by the patient by:
A.
Increasing frequency of beta-2-agonists and contacting their provider
B.
Doubling inhaled corticosteroid dose
C.
Increasing frequency of beta-2-agonists
D.
Starting montelukast (Singulair)
A.
Increasing frequency of beta-2-agonists and contacting their provider
Patients who are at risk of a fatal asthma attack include patients:
A.
With moderate persistent asthma
B.
With a history of requiring intubation or ICU admission for asthma
C.
Who are on daily inhaled corticosteroid therapy
D.
Who are pregnant
B.
With a history of requiring intubation or ICU admission for asthma
Pregnant patients with asthma may safely use ____ throughout their pregnancy.
A.
Oral terbutaline
B.
Prednisone
C.
Inhaled corticosteroids (budesonide)
D.
Montelukast (Singulair)
C.
Inhaled corticosteroids (budesonide)
One goal of asthma management in children is:
A.
They independently manage their asthma
B.
Participation in school and sports activities
C.
No exacerbations
D.
Minimal use of inhaled corticosteroids
B.
Participation in school and sports activities
Medications used in the management of patients with COPD include:
A.
Inhaled beta-2-agonists
B.
Inhaled anticholinergics (ipratropium)
C.
Inhaled corticosteroids
D.
All of the above
D.
All of the above
Patients with a COPD exacerbation may require:
A.
Doubling of inhaled corticosteroid dose
B.
Systemic corticosteroid burst
C.
Continuous inhaled beta-2-agonists
D.
Leukotriene therapy
B.
Systemic corticosteroid burst
Patients with COPD require monitoring of:
A.
Beta-2-agonist use
B.
Serum electrolytes
C.
Blood pressure
D.
All of the above
A.
Beta-2-agonist use
Education of patients with COPD who use inhaled corticosteroids includes:
A.
Doubling dose at the first sign of a URI
B.
Use their inhaled corticosteroid first and then their bronchodilator
C.
Rinsing mouth after use
D.
They should not smoke for at least 30 minutes after using
C.
Rinsing mouth after use
Type 1 diabetes results from autoimmune destruction of the beta cells. Eighty-five to 90 percent of Type 1 diabetics have:
A.
Autoantibodies to two tyrosine phosphatases
B.
Mutation of the hepatic transcription factor on chromosome 12
C.
A defective glucokinase molecule due to a defective gene on chromosome 7p
D.
Mutation of the insulin promoter factor
A.
Autoantibodies to two tyrosine phosphatases
Type 2 diabetes is a complex disorder involving:
A.
Absence of insulin production by the beta cells
B.
A suboptimal response of insulin-sensitive tissues in the liver
C.
Increased levels of glucagon-like peptide in the post-prandial period
D.
Too much fat uptake in the intestine
B.
A suboptimal response of insulin-sensitive tissues in the liver
Diagnostic criteria for diabetes include:
A.
Fasting blood glucose greater than 140 mg/dl on two occasions
B.
Post-prandial blood glucose greater than 140 mg/dl
C.
Fasting blood glucose 100 to 125 mg/dl on two occasions
D.
Symptoms of diabetes plus a casual blood glucose greater than 200 mg/dl
D.
Symptoms of diabetes plus a casual blood glucose greater than 200 mg/dl
Routine screening of asymptomatic adults for diabetes is appropriate for:
A.
Individuals who are older than 45 and have a BMI less than 25 kg/m2
B.
Native Americans, African Americans, and Hispanics
C.
Persons with HDL cholesterol greater than 100 mg/dl
D.
Persons with pre-diabetes confirmed on at least two occasions
B.
Native Americans, African Americans, and Hispanics
Screening criteria for children who meet the following criteria should begin at age 10 and occur every 3 years thereafter:
A.BMI above the 85th percentile for age and sex
B.Family history of diabetes in first- or second-degree relative
C.Hypertension based on criteria for children
D.Any of the above
D.Any of the above
Insulin is used to treat both types of diabetes. It acts by:
A.
Increasing beta cell response to low blood glucose levels
B.
Stimulating hepatic glucose production
C.
Increasing peripheral glucose uptake by skeletal muscle and fat
D.
Improving the circulation of free fatty acids
C.
Increasing peripheral glucose uptake by skeletal muscle and fat
Adam has Type 1 diabetes and plays tennis for his university. He exhibits a Knowledge deficit about his insulin and his diagnosis. He should be taught that:
A.
He should increase his CHO intake during times of exercise
B.
Each brand of insulin is equal in bioavailability, so buy the least expensive
C.
Alcohol produces hypoglycemia and can help control his diabetes when taken in small amounts
D.
If he does not want to learn to give himself injections, he may substitute an oral hypoglycemic to control his diabetes
A.
He should increase his CHO intake during times of exercise
Insulin preparations are divided into categories based on onset, duration, and intensity of action following subcutaneous inject. Which of the following insulin preparations has the shortest onset and duration of action?
A.
Insulin lispro
B.
Insulin glulisine
C.
Insulin glargine
D.
Insulin detemir
B.
Insulin glulisine
The drug of choice for Type 2 diabetics is metformin. Metformin:
A.
Decreases glycogenolysis by the liver
B.
Increases the release of insulin from beta cells
C.
Increases intestinal uptake of glucose
D.
Prevents weight gain associated with hyperglycemia
A.
Decreases glycogenolysis by the liver
Before prescribing metformin, the provider should:
A.
Draw a serum creatinine level to assess renal function
B.
Try the patient on insulin
C.
Prescribe a thyroid preparation if the patient needs to lose weight
D.
All of the above
A.
Draw a serum creatinine level to assess renal function
Sulfonylureas may be added to a treatment regimen for Type 2 diabetics when lifestyle modifications and metformin are insufficient to achieve target glucose levels. Sulfonylureas have been moved to Step 2 therapy because they:
A.
Increase endogenous insulin secretion
B.
Have a significant risk for hypoglycemia
C.
Address the insulin resistance found in Type 2 diabetics
D.
Improve insulin binding to receptors
B.
Have a significant risk for hypoglycemia
Dipeptidyl peptidase-4 inhibitors (gliptins) act on the incretin system to improve glycemic control. Advantages of these drugs include:
A.
Better reduction in glucose levels than other classes
B.
Less weight gain than sulfonylureas
C.
Low risk for hypoglycemia
D.
Can be given twice daily
C.
Low risk for hypoglycemia
Control targets for patients with diabetes include:
A.
HbA1C between 7 and 8
B.
Fasting blood glucose levels between 100 and 120 mg/dl
C.
Blood pressure less than 130/80 mm Hg
D.
LDL lipids less than 130 mg/dl
C.
Blood pressure less than 130/80 mm Hg
Establishing glycemic targets is the first step in treatment of both types of diabetes. For Type 1 diabetes:
A.
Tight control/intensive therapy can be given to adults who are willing to test their blood glucose at least twice daily
B.
Tight control is acceptable for older adults if they are without complications
C.
Plasma glucose levels are the same for children as adults
D.
Conventional therapy has a fasting plasma glucose target between 120 and 150 mg/dl
D.
Conventional therapy has a fasting plasma glucose target between 120 and 150 mg/dl
Treatment with insulin for Type 1 diabetics:
A.
Starts with a total daily dose of 0.2 to 0.4 units per kg of body weight
B.
Divides the total doses into three injections based on meal size
C.
Uses a total daily dose of insulin glargine given once daily with no other insulin required
D.
Is based on the level of blood glucose
A.
Starts with a total daily dose of 0.2 to 0.4 units per kg of body weight
When the total daily insulin dose is split and given twice daily, which of the following rules may be followed?
A.
Give two-thirds of the total dose in the morning and one-third in the evening.
B.
Give 0.3 units per kg of premixed 70/30 insulin with one-third in the morning and two-thirds in the evening.
C.
Give 50% of an insulin glargine dose in the morning and 50% in the evening.
D.
Give long-acting insulin in the morning and short-acting insulin at bedtime.
A.
Give two-thirds of the total dose in the morning and one-third in the evening.
Studies have shown that control targets that reduce the HbA1C to less than 7% are associated with fewer long-term complications of diabetes. Patients who should have such a target include:
A.
Those with long-standing diabetes
B.
Older adults
C.
Those with no significant cardiovascular disease
D.
Young children who are early in their disease
C.
Those with no significant cardiovascular disease
Prevention of conversion from pre-diabetes to diabetes in young children must take highest priority and should focus on:
A.
Aggressive dietary manipulation to prevent obesity
B.
Fostering LDL levels less than 100 mg/dl and total cholesterol less than 170 mg/dl to prevent cardiovascular disease
C.
Maintaining a blood pressure that is less than 80% based on weight and height to prevent hypertension
D.
All of the above
B.
Fostering LDL levels less than 100 mg/dl and total cholesterol less than 170 mg/dl to prevent cardiovascular disease
The drugs recommended by the American Academy of Pediatrics for use in children with diabetes (depending upon type of diabetes) are:
A.
Metformin and insulin
B.
Sulfonylureas and insulin glargine
C.
Split-mixed dose insulin and GPL-1 agonists
D.
Biguanides and insulin lispro
A.
Metformin and insulin
Unlike most Type 2 diabetics where obesity is a major issue, older adults with low body weight have higher risks for morbidity and mortality. The most reliable indicator of poor nutritional status in older adults is:
A.
Weight loss in previously overweight persons
B.
Involuntary loss of 10% of body weight in less than 6 months
C.
Decline in lean body mass over a 12-month period
D.
Increase in central versus peripheral body adiposity
B.
Involuntary loss of 10% of body weight in less than 6 months
The drugs recommended for older adults with Type 2 diabetes include:
A.
Second generation sulfonylureas
B.
Metformin
C.
Pioglitazone
D.
Third generation sulfonylureas
D.
Third generation sulfonylureas
Ethnic groups differ in their risk for and presentation of diabetes. Hispanics:
A.
Have a high incidence of obesity, elevated triglycerides, and hypertension
B.
Do best with drugs that foster weight loss, such as metformin
C.
Both A and B
D.
Neither A nor B
C.
Both A and B
The American Heart Association states that people with diabetes have a 2- to 4-fold increase in the risk of dying from cardiovascular disease. Treatments and targets that do not appear to decrease risk for micro- and macro-vascular complications include:
A.
Glycemic targets between 7% and 7.5%
B.
Use of insulin in Type 2 diabetics
C.
Control of hypertension and hyperlipidemia
D.
Stopping smoking
A.
Glycemic targets between 7% and 7.5%
All diabetic patients with known cardiovascular disease should be treated with:
A.
Beta blockers to prevent MIs
B.
ACE inhibitors and aspirin to reduce risk of cardiovascular events
C.
Sulfonylureas to decrease cardiovascular mortality
D.
Pioglitazone to decrease atherosclerotic plaque buildup
B.
ACE inhibitors and aspirin to reduce risk of cardiovascular events
All diabetic patients with hyperlipidemia should be treated with:
A.
HMG-CoA reductase inhibitors
B.
Fibric acid derivatives
C.
Nicotinic acid
D.
Colestipol
A.
HMG-CoA reductase inhibitors
Both ACE inhibitors and some Angiotensin-II receptor blockers have been approved in treating:
A.
Hypertension in diabetic patients
B.
Diabetic nephropathy
C.
Both A and B
D.
Neither A nor B
C.
Both A and B
Protein restriction helps slow the progression of albuminuria, GFR decline, and ESRD is some patients with diabetes. It is useful for patients who:
A.
Cannot tolerate ACE inhibitors or ARBs
B.
Have uncontrolled hypertension
C.
Have HbA1C levels above 7%
D.
Show progression of diabetic nephropathy despite optimal glucose and blood pressure control
D.
Show progression of diabetic nephropathy despite optimal glucose and blood pressure control
Diabetic autonomic neuropathy (DAN) is the earliest and most common complication of diabetes. Symptoms associated with DAN include:
A. Resting tachycardia, exercise intolerance, and orthostatic hypotension
B. Gastroparesis, cold intolerance, and moist skin
C. Hyperglycemia, erectile dysfunction, and deficiency of free fatty acids
D. Pain, loss of sensation, and muscle weaknes
A. Resting tachycardia, exercise intolerance, and orthostatic hypotension
Drugs used to treat diabetic peripheral neuropathy include:
A. Metoclopramide
B. Cholinergic agonists
C. Cardioselective beta blockers
D. Gabapentin
D. Gabapentin
The American Diabetic Association has recommended which of the following tests for ongoing management of diabetes?
A. Fasting blood glucose
B. HbA1C
C. Thyroid function tests
D. Electrocardiograms
B. HbA1C
Angina is produced by an imbalance between oxygen supply (MOS) and demand (MOD) in the myocardium. Which of the following drugs help to correct this imbalance by increasing MOS?
A. Calcium channel blockers
B. Beta blockers
C. ACE inhibitors
D. Aspirin
C. ACE inhibitors
Not all chest pain is caused by myocardial ischemia. Non-cardiac causes of chest pain include:
A. Pulmonary embolism
B. Pneumonia
C. Gastroesophageal reflux
D. All of the above
D. All of the above
The New York Heart Association and the Canadian Cardiovascular Society have described grading criteria for levels of angina. Angina that occurs with unusually strenuous activity or on walking or climbing stair after meals is:
A.
Class I
B.
Class II
C.
Class III
D.
Class IV
B.
Class II
Patients at high risk for developing significant coronary heart disease are those with:
A.
LDL values between 100 and 130
B.
Systolic blood pressure between 120 and 130
C.
Class III angina
D.
Obesity
C.
Class III angina
To reduce mortality, all patients with angina, regardless of Class, should be on:
A.
Aspirin 81 to 325 mg/d
B.
Nitroglycerin sublingually for chest pain
C.
ACE inhibitors or ARBs
D.
Digoxin
A.
Aspirin 81 to 325 mg/d
Patients who have angina, regardless of Class, who are also diabetic, should be on:
A.
Nitrates
B.
Beta blockers
C.
ACE inhibitors
D.
Calcium channel blockers
C.
ACE inhibitors
Management of all types and grades of angina includes the use of lifestyle modification to reduce risk factors. Which of these modifications are appropriate for which reason? Both the modification and the reason for it must be true for the answer to be correct.
A.
Lose at least 10 pounds of body weight. Excessive weight increases cardiac workload.
B.
Reduce sodium intake to no more than 2,400 mg of sodium. Sodium increases blood volume and cardiac workload.
C.
Increase potassium intake to at least 100 mEq/d. The heart needs higher levels of potassium to improve contractility and oxygen supply.
D.
Intake a moderate amount of alcohol. Moderate intake has been shown by research to improve cardiac function.
B.
Reduce sodium intake to no more than 2,400 mg of sodium. Sodium increases blood volume and cardiac workload.
Nitrates are especially helpful for patients with angina who also have:
A.
Heart failure
B.
Hypertension
C.
Both A and B
D.
Neither A nor B
C.
Both A and B
Beta blockers are especially helpful for patients with exertional angina who also have:
A.
Arrhythmias
B.
Hypothyroidism
C.
Hyperlipidemia
D.
Atherosclerosis
A.
Arrhythmias
Rapid-acting nitrates are important for all angina patients. Which of the following are true statements about their use?
A.
These drugs are useful for immediate symptom relief when the patient is certain it is angina.
B.
The dose is one sublingual tablet or spray every 5 minutes until the chest pain goes away.
C.
Take one nitroglycerine tablet or spray at the first sign of angina; repeat every 5 minutes for no more than three doses. If chest pain is still not relieved, go to the hospital.
D.
All of the above
C.
Take one nitroglycerine tablet or spray at the first sign of angina; repeat every 5 minutes for no more than three doses. If chest pain is still not relieved, go to the hospital.
Isosorbide dinitrate is a long-acting nitrate given BID. The schedule for administration is 7 AM and 2 PM because:
A.
Long-acting forms have a higher risk for toxicity
B.
Orthostatic hypotension is a common adverse effect
C.
It must be taken with milk or food
D.
Nitrate tolerance can develop
D.
Nitrate tolerance can develop
Combinations of a long-acting nitrate and a beta blocker are especially effective in treating angina because:
A.
Nitrates increase MOS and beta blockers increase MOD
B.
Their additive affects permit lower doses of both drugs and their adverse reactions cancel each other out.
C.
They address the pathology of patients with exertional angina who have fixed atherosclerotic coronary heart disease
D.
All of the above
B.
Their additive affects permit lower doses of both drugs and their adverse reactions cancel each other out.
Although they are often described as helpful in the lay media, which of the following therapies have not been shown to be helpful based on clinical evidence?
A.
Vitamins C and E
B.
Co-enzyme Q10
C.
Folic acid
D.
All of the above
D.
All of the above
Drug choices to treat angina in older adults differ from those of younger adults only in:
A.Consideration of risk factors for diseases associated with and increased in aging
B.The placement of drug therapy as a treatment choice before lifestyle changes are tried
C.The need for at least three drugs in the treatment regimen because of the complexity of angina in the older adult
D.Those with higher risk for silent myocardial infarction (MI)
A.
Consideration of risk factors for diseases associated with and increased in aging
Which of the following drugs has been associated with increased risk for myocardial infarction (MI) in women?
A.
Aspirin
B.
Beta blockers
C.
Estrogen replacement
D.
Lipid-lowering agents
C.
Estrogen replacement
Cost of antianginal drug therapy should be considered in drug selection because of all of the following EXCEPT:
A.
Patients often require multiple drugs
B.
A large number of angina patients are older adults on fixed incomes
C.
Generic formulations may be cheaper but are rarely bioequivalent
D.
Lack of drug selectivity may result in increased adverse reactions
C.
Generic formulations may be cheaper but are rarely bioequivalent
Five questions should be asked during the follow up of any angina patient. They include:
A.
Have there been any changes in lab data since the last visit?
B.
Has the level of physical activity associated with the angina changed since the last visit?
C.
Have new risk factors come to light in producing the angina?
D.
Is the patient filling prescriptions and taking the drugs as prescribed?
B.
Has the level of physical activity associated with the angina changed since the last visit?
Situations that suggest referral to a specialist is appropriate include:
A.
When chronic stable angina becomes unpredictable in its characteristics and precipitating factors
B.
When a post-MI patient develops new-onset angina
C.
When standard therapy is not successful in improving exercise tolerance or reducing the incidence of angina
D.
All of the above
D.
All of the above
Ray has been diagnosed with hypertension and an ACE inhibitor is determined to be needed. Prior to prescribing this drug, the NP should assess for:
A.
Hypokalemia
B.
Impotence
C.
Decreased renal function
D.
Inability to concentrate
C.
Decreased renal function
ACE inhibitors are the drug of choice in treating hypertension in diabetic patients because they:
A.
Improve insulin sensitivity
B.
Improve renal hemodynamics
C.
Reduce the production of angiotensin II
D.
All of the above
D.
All of the above
A potentially life-threatening adverse response to ACE inhibitors is angioedema. Which of the following statements is true about this adverse response?
A.
Swelling of the tongue or hoarseness are the most common symptoms.
B.
It appears to be related to the decrease in aldosterone production.
C.
Presence of a dry, hacky cough indicates a high risk for this adverse response.
D.
Because it takes time to build up a blood level, it occurs after being on the drug for about 1 week.
A.
Swelling of the tongue or hoarseness are the most common symptoms.
ACE inhibitors are useful in a variety of disorders. Which of the following statements are true about both its usefulness in the disorder and the reason for its use?
A.
Stable angina because it decreases the thickening of vascular walls to decreased MOD.
B.
Heart failure because it reduces remodeling of injured myocardial tissues.
C.
Both A and B are true and the reasons are correct
D.
Both A and B are true but the reasons are wrong
E.
Neither A nor B are true
C.
Both A and B are true and the reasons are correct
Despite good blood pressure control, a NP might change a patient’s drug from an ACEI to an angiotensin II receptor blocker (ARB) because the ARB:
A.
Is stronger than the ACEI
B.
Does not produce a dry, hacky cough
C.
Has no effect on the renal system
D.
Reduces sodium and water retention
B.
Does not produce a dry, hacky cough
While taken an ARB, patients need to avoid certain over-the-counter drugs without first consulting the provider because:
A.
Cimetidine is metabolized by the CYP 3A4 isoenzymes
B.
Nonsteroidal anti-inflammatory drugs reduce prostaglandin levels
C.
Both A and B
D.
Neither A nor B
C.
Both A and B
Laboratory monitoring for patients on ACEIs or ARBs should include:
A.
White blood cells counts with the drug dose increased for elevations above 10,000
B.
Liver function tests with the drug dose stopped for ALT values 2× normal
C.
Serum creatinine levels with the drug dose reduced for values above 2.5 mg/dL
D.
Serum glucose levels with the drug dose increased for levels above 120 mg/dL
C.
Serum creatinine levels with the drug dose reduced for values above 2.5 mg/dL
Jacob has hypertension for which a calcium channel blocker has been prescribed. This drug helps control blood pressure because it:
A.
Decreases the amount of calcium inside the cell
B.
Reduces stroke volume
C.
Increases the activity of the Na+/K+/ATPase pump indirectly
D.
Decreases heart rate
A.
Decreases the amount of calcium inside the cell
Which of the following adverse effects may occur due to a dihydropyridine-type calcium channel blocker?
A.
Bradycardia
B.
Hepatic impairment
C.
Increased contractility
D.
Edema of the hands and feet
D.
Edema of the hands and feet
Patient teaching related to amlodipine includes:
A.
Increase calcium intake to prevent osteoporosis from calcium blockade.
B.
Do not crush the tablet; it must be given in liquid form if the patient has trouble swallowing it.
C.
Avoid grapefruit juice as it affects the metabolism of this drug.
D.
Rise slowly from a supine position to reduce orthostatic hypotension.
C.
Avoid grapefruit juice as it affects the metabolism of this drug.
Vera, age 70, has isolated systolic hypertension. Calcium channel blocker doses for her should be:
A.
Started at about half the usual dose
B.
Not raised above the usual dose for an adult
C.
Given once daily due to memory issues in the older adult
D.
Withheld if she experiences gastroesophageal reflux
A.
Started at about half the usual dose
Larry has heart failure which is being treated with digoxin because it exhibits:
A.
Negative inotropism
B.
Positive chronotropism
C.
Both A and B
D.
Neither A nor B
D.
Neither A nor B
Furosemide is added to a treatment regimen for heart failure which includes digoxin. Monitoring for this combination includes:
A.
Hemoglobin
B.
Serum potassium
C.
Blood urea nitrogen
D.
Serum glucose
B.
Serum potassium
Which of the following create higher risk for digoxin toxicity? Both the cause and the reason for it must be correct.
A.
Older adults due to reduced renal function
B.
Administration of aldosterone antagonist diuretics due to decreased potassium levels
C.
Taking an antacid for GERD because it increases the absorption of digoxin
D.
Doses between 0.25 and 0.5 mg/day
A.
Older adults due to reduced renal function
Serum digoxin levels are monitored for potential toxicity. Monitoring should occur:
A.
Within 6 hours of the last dose
B.
Because a reference point is needed in adjusting a dose
C.
After three half-lives from the starting of the drug
D.
When a patient has stable renal function
B.
Because a reference point is needed in adjusting a dose
Rodrigo has been prescribed procainamide after a myocardial infarction. He is monitored for dyspnea, jugular venous distention, and peripheral edema because they may indicate:
A.
Widening of the area of infarction
B.
Onset of congestive heart failure
C.
An electrolyte imbalance involving potassium
D.
Renal dysfunction
B.
Onset of congestive heart failure
Which of the following is true about procainamide and its dosing schedule?
A.
It produces bradycardia and should be used cautiously in patients with cardiac conditions that a slower heart rate might worsen.
B.
Gastrointestinal adverse effects are common so the drug should be taken with food.
C.
Adherence can be improved by using a sustained release formulation that can be given once daily.
D.
Doses of this drug should be taken evenly spaced around the clock to keep an even blood level.
D.
Doses of this drug should be taken evenly spaced around the clock to keep an even blood level.
Amiodarone has been prescribed in a patient with a supraventricular dysrhythmia. Patient teaching should include all of the following EXCEPT:
A.
Notify your health-care provider immediately if you have visual change
B.
Monitor your own blood pressure and pulse daily
C.
Take a hot shower or bath if you feel dizzy
D.
Use a sunscreen on exposed body surfaces
C.
Take a hot shower or bath if you feel dizzy
The NP orders a thyroid panel for a patient on amiodarone. The patient tells the NP that he does not have thyroid disease and wants to know why the test is ordered. Which is a correct response?
A.
“Amiodarone inhibits an enzyme that is important in making thyroid hormone and can cause hypothyroidism.”
B.
“Amiodarone damages the thyroid gland and can result in inflammation of that gland causing hyperthyroidism.”
C.
“Amiodarone is a broad spectrum drug with many adverse effects. Many different tests need to be done before it is given.”
D.
“Amiodarone can cause corneal deposits in up to 25% of patients.”
A.
“Amiodarone inhibits an enzyme that is important in making thyroid hormone and can cause hypothyroidism.”
Isosorbide dinitrate is prescribed for a patient with chronic stable angina. This drug is administered twice daily, but the schedule is 7 AM and 2 PM because:
A.
It is a long-acting drug with potential for toxicity
B.
Nitrate tolerance can develop
C.
Orthostatic hypotension is a common adverse effect
D.
It must be taken with milk or food
B.
Nitrate tolerance can develop
Art is a 55-year-old smoker who has been diagnosed with angina and placed on nitrates. He complains of headaches after using his nitrate. An appropriate reply might be:
A.
“This is a parasympathetic response to the vasodilating effects of the drug.”
B.
“Headaches are common side effects with these drugs. How severe are they?”
C.
“This is associated with your smoking. Let’s work on having you stop smoking.”
D.
“This is not related to your medication. Are you under a lot of stress?”
B.
“Headaches are common side effects with these drugs. How severe are they?”
In teaching about the use of sublingual nitroglycerine, the patient should be instructed:
A.
To swallow the tablet with a full glass of water
B.
To place one tablet under the tongue if chest pain occurs and allow it to dissolve
C.
To take one tablet every 5 minutes until the chest pain goes away
D.
That it should “burn” when placed under the tongue or it is no longer effective
B.
To place one tablet under the tongue if chest pain occurs and allow it to dissolve
Donald has been diagnosed with hyperlipidemia. Based on his lipid profile, atorvastatin is prescribed. Rhabdomyolysis is a rare but serious adverse response to this drug. Donald should be told to:
A.
Become a vegetarian since this disorder is associated with eating red meat
B.
Stop taking the drug if abdominal cramps and diarrhea develop
C.
Report muscle weakness or tenderness and dark urine to his provider immediately
D.
Expect “hot flash” sensations during the first 2 weeks of therapy
C.
Report muscle weakness or tenderness and dark urine to his provider immediately
Which of the following diagnostic studies would NOT indicate a problem related to a reductase inhibitor?
A.
Elevated serum transaminase
B.
Increased serum creatinine
C.
Elevated creatinine kinase
D.
Increased white blood cells counts
D.
Increased white blood cells counts
Because of the pattern of cholesterol synthesis, reductase inhibitors are given:
A.
In the evening in a single daily dose
B.
Twice daily in the morning and the evening
C.
With each meal and at bedtime
D.
In the morning before eating
A.
In the evening in a single daily dose
Janice has elevated LDL, VLDL, and triglyceride levels. Niaspan, an extended-release form of niacin, is chosen to treat her hyperlipidemia. Due to its metabolism and excretion, which of the following labs should be monitored?
A.
Serum alanine aminotransferase
B.
Serum amylase
C.
Serum creatinine
D.
Phenylketonuria
C.
Serum creatinine
Niaspan is less likely to cause which side effect that is common to niacin?
A.
Gastrointestinal irritation
B.
Cutaneous flushing
C.
Dehydration
D.
Headaches
B.
Cutaneous flushing
Which of the following statements is true?
A.
Niacin is a B-complex vitamin and taking double the dose of the over-the-counter vitamin will lower LDL and save money.
B.
Niacin has been shown to reduce all-cause mortality for patients with CAD if taken in prescription strength.
C.
Niacin should be given on an empty stomach to avoid GI irritation.
D.
All of the above
B.
Niacin has been shown to reduce all-cause mortality for patients with CAD if taken in prescription strength.
Dulcea has type 2 diabetes and a high triglyceride level. She has gemfibrozil prescribed to treat her hypertriglyceridemia. A history of which of the following might contraindicate the use of this drug?
A.
Reactive airway disease/asthma
B.
Inflammatory bowel disease
C.
Allergy to aspirin
D.
Gallbladder disease
D.
Gallbladder disease
Many patients with hyperlipidemia are treated with more than one drug. Combining a fibric acid derivative such as gemfibrozil with which of the following is not recommended? The drug and the reason must both be correct for the answer to be correct.
A.
Reductase inhibitors, due to an increased risk for rhabdomyolysis
B.
Bile-acid sequestering resins, due to interference with folic acid absorption
C.
Grapefruit juice, due to interference with metabolism
D.
Niacin, due to decreased gemfibrozil activity
A.
Reductase inhibitors, due to an increased risk for rhabdomyolysis
Felicity has been prescribed colestipol to treat her hyperlipidemia. Unlike other anti-lipidemics, this drug:
A.
Blocks synthesis of cholesterol in the liver
B.
Exchanges chloride ions for negatively charged acids in the bowel
C.
Increases HDL levels the most among the classes
D.
Blocks the lipoprotein lipase pathway
B.
Exchanges chloride ions for negatively charged acids in the bowel
Because of their site of action, bile acid sequestering resins:
A.
Should be administered separated from other drugs by at least 4 hours
B.
May increase the risk for bleeding
C.
Both A and B
D.
Neither A nor B
A.
Should be administered separated from other drugs by at least 4 hours
Colestipol comes in a powdered form. The patient is taught to:
A.
Take the powder dry and follow it with at least 8 ounces of water
B.
Take it with a meal to enhance its action on fatty food
C.
Mix the powder with 4 to 6 ounces of milk or fruit juice
D.
Take after the evening meal to coincide with cholesterol synthesis
C.
Mix the powder with 4 to 6 ounces of milk or fruit juice
The choice of diuretic to use in treating hypertension is based on:
A.
Presence of diabetes with loop diuretics being used for these patients
B.
Level of kidney function with a thiazide diuretic being used for an estimated glomerular filtration rate higher than the mid-40 mL/min range
C.
Ethnicity with aldosterone antagonists best for African Americans and older adults
D.
Presence of hyperlipidemia with higher doses needed for patients with LDL above 130 mg/dL
B.
Level of kidney function with a thiazide diuretic being used for an estimated glomerular filtration rate higher than the mid-40 mL/min range
[Show More]
Last updated: 3 years ago
Preview 1 out of 30 pages









.png)
.png)
.png)
.png)
.png)