a. Fetal hemoglobin has a greater affinity for oxygen as a result of
diphosphoglycerate (DPG).
b. The fetus has a different hemoglobin structure of two α- and two γ-chains rather
than two α-and two β-chains.
c. Incre
...
a. Fetal hemoglobin has a greater affinity for oxygen as a result of
diphosphoglycerate (DPG).
b. The fetus has a different hemoglobin structure of two α- and two γ-chains rather
than two α-and two β-chains.
c. Increased erythropoiesis occurs in response to the hypoxic intrauterine
environment.
d. The lungs of the fetus are undeveloped and unable to diffuse oxygen adequately to
the pulmonary capillaries.
a. The fetus does not have its own oxygen supply and must rely on oxygen from the
maternal vascular system.
b. The fetus has two γ-chains on the hemoglobin, rather than two β-chains as in the
adult.
c. Fetal hemoglobin interacts less readily with diphosphoglycerate (DPG), which
inhibits hemoglobin-oxygen binding.
d. Fetal hemoglobin production occurs in the vessels and liver rather than in the bone
marrow as in the adult.
a. Monocytes c. Neutrophils
b. Platelets d. Lymphocytes
a. Folic acid deficiency c. Hemoglobin abnormality
b. Iron deficiency d. Erythrocyte abnormality
a. HDN develops when hypoxia or dehydration causes the erythrocytes to change
shapes, which are then recognized as foreign and removed from circulation.
b. HDN is an alloimmune disease in which the mother’s immune system produces
antibodies against fetal erythrocytes, which are recognized as foreign and removed
from circulation.
c. HDN develops when the polycythemia present in fetal life continues after birth,
causing the excessive number of erythrocytes to be removed from circulation.
d. HDN is an autoimmune disease in which the fetus’s immune system produces
antibodies against fetal erythrocytes, which are recognized as foreign and removed
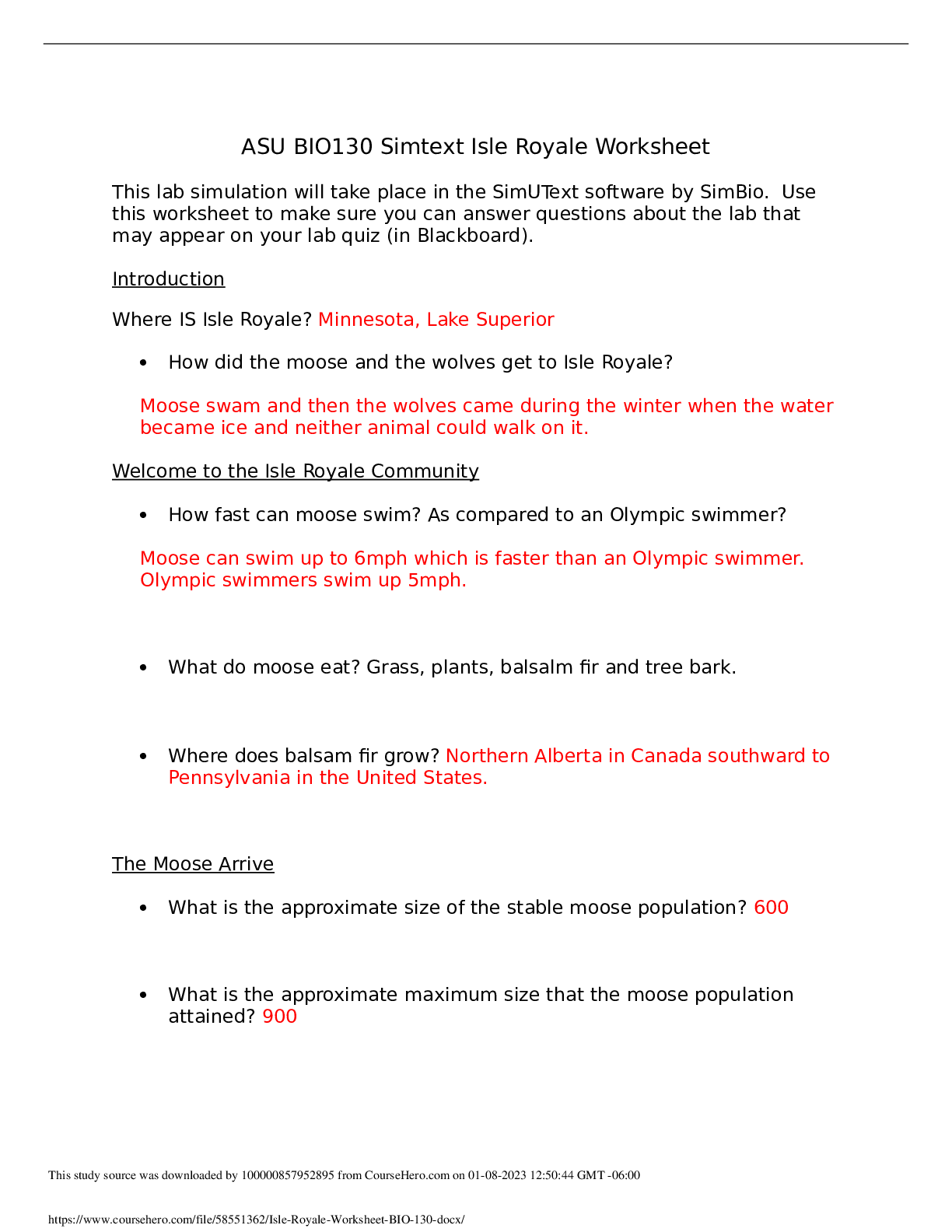
Chapter 30 Alterations of Hematologic Function in Children
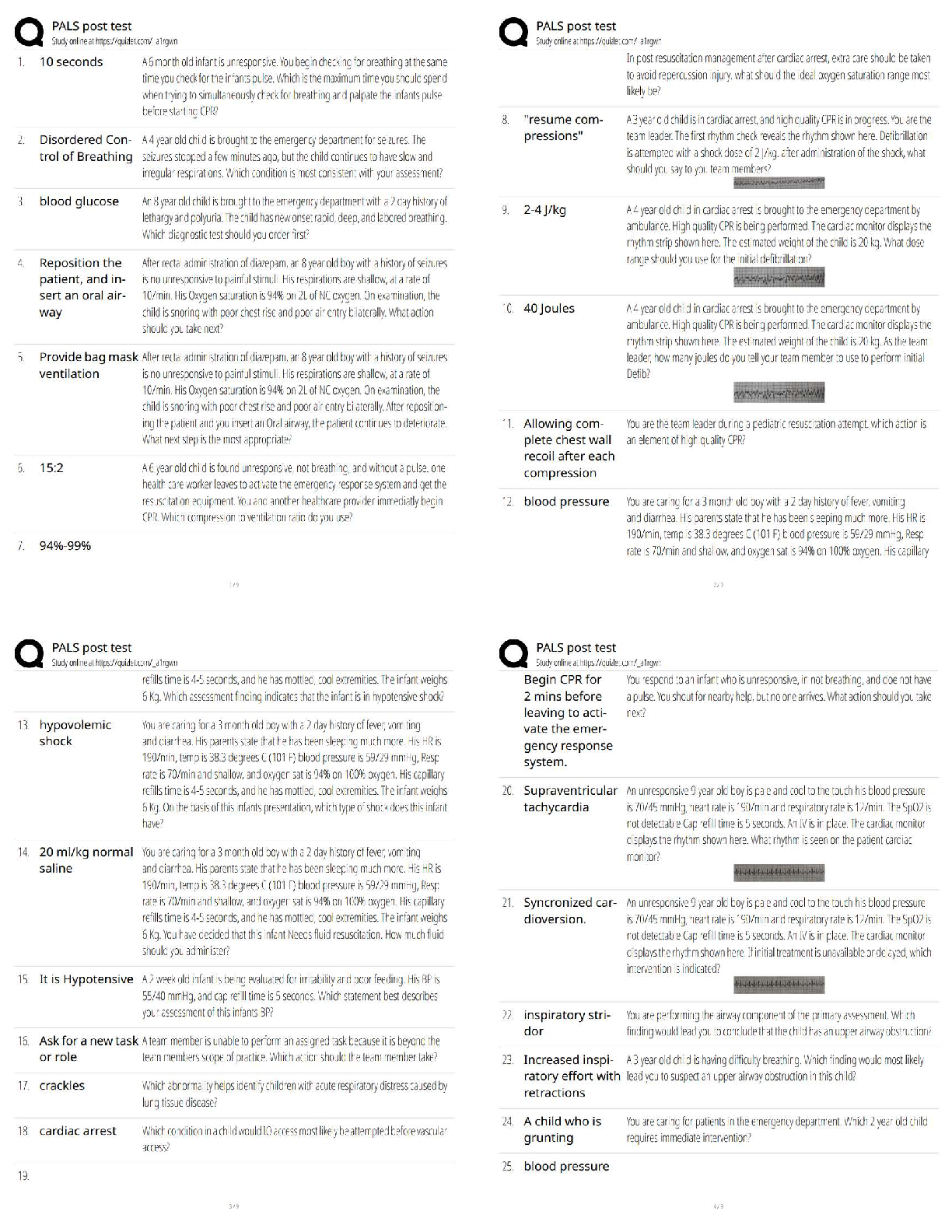
Multiple Choice
Identify the choice that best completes the statement or answers the question.
1. What is the cause of polycythemia in the fetus?
2. Why does fetal hemoglobin have a greater affinity for oxygen than adult hemoglobin?
3. Which blood cell type is elevated at birth but decreases to adult levels during the first year of life?
4. In a full-term infant, the normal erythrocyte life span is days, whereas the adult erythrocyte
life span is days.
a. 30 to 50; 80 c. 90 to 110; 140
b. 60 to 80; 120 d. 120 to 130; 150
5. What is the most common cause of insufficient erythropoiesis in children?
6. How does hemolytic disease of the newborn (HDN) cause acquired congenital hemolytic anemia?a. Allergic disease in which maternal blood and fetal blood are antigenically
incompatible
b. Alloimmune disease in which maternal blood and fetal blood are antigenically
incompatible
c. Autoimmune disease in immature nucleated cells that are released into the
bloodstream
d. Autosomal dominant hereditary disease
a. 11 c. 7
b. 9 d. 5
a. A c. C
b. B d. E
a. Is Rh-positive and the fetus is Rh-negative
b. Is Rh-negative and the fetus is Rh-positive
c. Has type A blood and the fetus has type O
d. Has type AB blood and the fetus has type B
a. Excretion of unconjugated bilirubin through the placenta into the mother’s
circulation is no longer possible.
b. Hemoglobin does not break down into bilirubin in the intrauterine environment.
c. The liver of the fetus is too immature to conjugate bilirubin from a lipid-soluble to
water-soluble form.
d. The destruction of erythrocytes producing bilirubin is greater after birth.
a. Spherocytosis c. Erythroblastosis fetalis
b. Icterus gravis neonatorum d. Hydrops fetalis
a. Kernicterus c. Jaundice
b. Icterus neonatorum d. Icterus gravis neonatorum
from circulation.
7. Erythroblastosis fetalis is defined as an:
8. An infant’s hemoglobin must fall below g/dl before signs of pallor, tachycardia, and systolic
murmurs occur.
9. Which vitamin improves the absorption of oral iron taken to treat iron deficiency anemia in
children?
10. Hemolytic disease of the newborn (HDN) can occur if the mother:
11. When diagnosed with hemolytic disease of the newborn (HDN), why does the newborn develop
hyperbilirubinemia after birth but not in utero?
12. Fetuses who do not survive anemia in utero are usually stillborn with gross edema of the entire body.
Which term is used to identify this condition?
13. What is the name of the disorder in which levels of bilirubin remain excessively high in the newborn
and are deposited in the brain?
14. What treatment prevents the development of kernicterus in an infant born with hemolytic disease of
the newborn (HDN)?
a. Administration of intravenous fluids to dilute the blooda. X-linked dominant c. Autosomal dominant
b. X-linked recessive d. Autosomal recessive
a. Inherited X-linked recessive disorder
b. Inherited autosomal recessive disorder
c. Disorder initiated by hypoxemia and acidosis
d. Disorder that is diagnosed equally in men and women
a. Deficiency in glucose 6-phosphate dehydrogenase (G6PD) that changes
hemoglobin A (HbA) to HbS.
b. Genetic mutation in which two amino acids (histidine and leucine) are missing.
c. Genetic mutation in which one amino acid (valine) is replaced by another
(glutamic acid).
d. Autoimmune response in which one amino acid (proline) is detected as an antigen
by abnormal immunoglobulin G (IgG).
a. Autosomal dominant c. X-linked dominant
b. Autosomal recessive d. X-linked recessive
a. Well-matched stem cell donors are difficult to find.
b. The child is usually too weak to survive the procedure.
c. The child’s immune system will not appropriately respond to the antirejection
medications.
d. Although effective for adults, neither procedure has been proven effective for
children.
a. Atelectasis and pneumonia
b. Edema of the hands and feet
c. Stasis ulcers of the hands, ankles, and feet
d. Splenomegaly and hepatomegaly
a. 20% c. 33%
b. 25% d. 50%
b. Replacement transfusion of new Rh-positive blood that is not contaminated with
anti-Rh antibodies
c. Performance of a splenectomy to prevent the destruction of abnormal erythrocytes
d. Replacement transfusion of Rh-negative erythrocytes
15. Glucose 6-phosphate dehydrogenase (G6PD) deficiency is what type of inherited disorder?
16. Sickle cell disease is classified as a(an):
17. Hemoglobin S (HbS) is formed in sickle cell disease as a result of which process?
18. Sickle cell disease (SCD) is what type of inherited disorder?
19. What is the reason most children diagnosed with sickle cell anemia are not candidates for either bone
marrow or stem cell transplants?
20. Which manifestations of vasoocclusive crisis are associated with sickle cell disease (SCD) in
infants?
21. What is the chance with each pregnancy that a child born to two parents with the sickle trait will
have sickle cell disease (SCD)?a. Microcytic, hypochromic c. Macrocytic, hyperchromic
b. Microcytic, normochromic d. Macrocytic, normochromic
a. The spleen prematurely destroys the precipitate-carrying cells.
b. A severe uncoupling of α- and β-chain synthesis occurs.
c. All four beta-forming genes are defective.
d. Hemoglobin H (HbH) develops when three genes are defective.
a. Autosomal recessive c. X-linked recessive
b. Autosomal dominant d. X-linked dominant
a. V c. IX
b. VIII d. X
a. Autosomal dominant c. X-linked recessive
b. Autosomal recessive d. X-linked dominant
a. Hemophilia A c. Christmas disease
b. von Willebrand disease d. Hemophilia B
a. Neutrophils c. Platelets
b. Eosinophils d. Basophils
a. Idiopathic thrombocytopenic purpura (ITP)
b. Acute lymphocytic leukemia (ALL)
c. Non-Hodgkin lymphoma (NHL)
d. Iron deficiency anemia (IDA)
a. Fourth month of gestation c. Eighth month of gestation
b. Fifth month of gestation d. At birth
a. Hemophilia A c. Hemophilia C
b. Hemophilia B d. von Willebrand disease
a. Hemophilia A c. Hemophilia C
b. Hemophilia B d. von Willebrand disease
22. Which type of anemia occurs as a result of thalassemia?
23. What is the fundamental defect that results in beta-thalassemia major?
24. The alpha- and beta-thalassemias are considered what types of inherited disorder?
25. Hemophilia B is caused by a deficiency of which clotting factor?
26. Hemophilia A is considered to be what type of inherited disorder?
27. Which disease is an autosomal dominant inherited hemorrhagic disease?
28. Idiopathic thrombocytopenic purpura (ITP) is an autoimmune process involving antibodies attacking
which type of cells?
29. Which disorder results in decreased erythrocytes and platelets with changes in leukocytes and has
clinical manifestations of pallor, fatigue, petechiae, purpura, bleeding, and fever?
30. When does fetal erythrocyte production shift from the liver to the bone marrow?
31. Which disease is caused by clotting factor VIII deficiency and is an autosomal dominant trait?
32. Which type of hemophilia affects only men?a. Hemophilia A c. Hemophilia C
b. Hemophilia B d. von Willebrand disease
a. Between 2 months and 1 year c. Between 12 months and 3 years
b. Between 6 months and 2 years d. Between 18 months and 4 years
a. Hyperdiploidy indicates a good prognosis.
b. Hyperdiploidy indicates a poor prognosis.
c. Hyperdiploidy indicates poor response to a specific treatment.
d. Hyperdiploidy indicates the achievement of remission.
a. Fever
b. Infection
c. Dehydration
d. Alkalosis
e. Exposure to the cold
33. Which hemophilia occurs equally in both men and women?
34. During childhood, when is dietary iron deficiency commonly diagnosed?
35. What is the significance of hyperdiploidy when diagnosing and treating leukemia?
Multiple Response
Identify one or more choices that best complete the statement or answer the question.
36. What are the common triggers for sickle cell crisis? (Select all that apply.)
Matching
Match each sickle cell crisis with its description. Terms may be used more than once.
A. Vasoocclusive crisis
B. Aplastic crisis
C. Sequestration crisis
D. Hyperhemolytic crisis
37. Large amounts of blood become acutely pooled in the liver and spleen.
38. Blood flow is impaired by tangled masses of rigid, sickled cells.
39. Crisis occurs in association with certain drugs or infection.
40. Compensatory erythropoiesis is compromised, thus limiting the number of erythrocytes that are
replaced.
Thought Questions
1. A woman who is Rh-negative just delivered a baby that is Rh-positive. Should she be concerned? If so,
explain why.
[Show More]











.png)
.png)
.png)