Biology > QUESTIONS & ANSWERS > Chapter 10: Immunodiagnosis of Infectious Diseases. All Answers (All)
Chapter 10: Immunodiagnosis of Infectious Diseases. All Answers
Document Content and Description Below
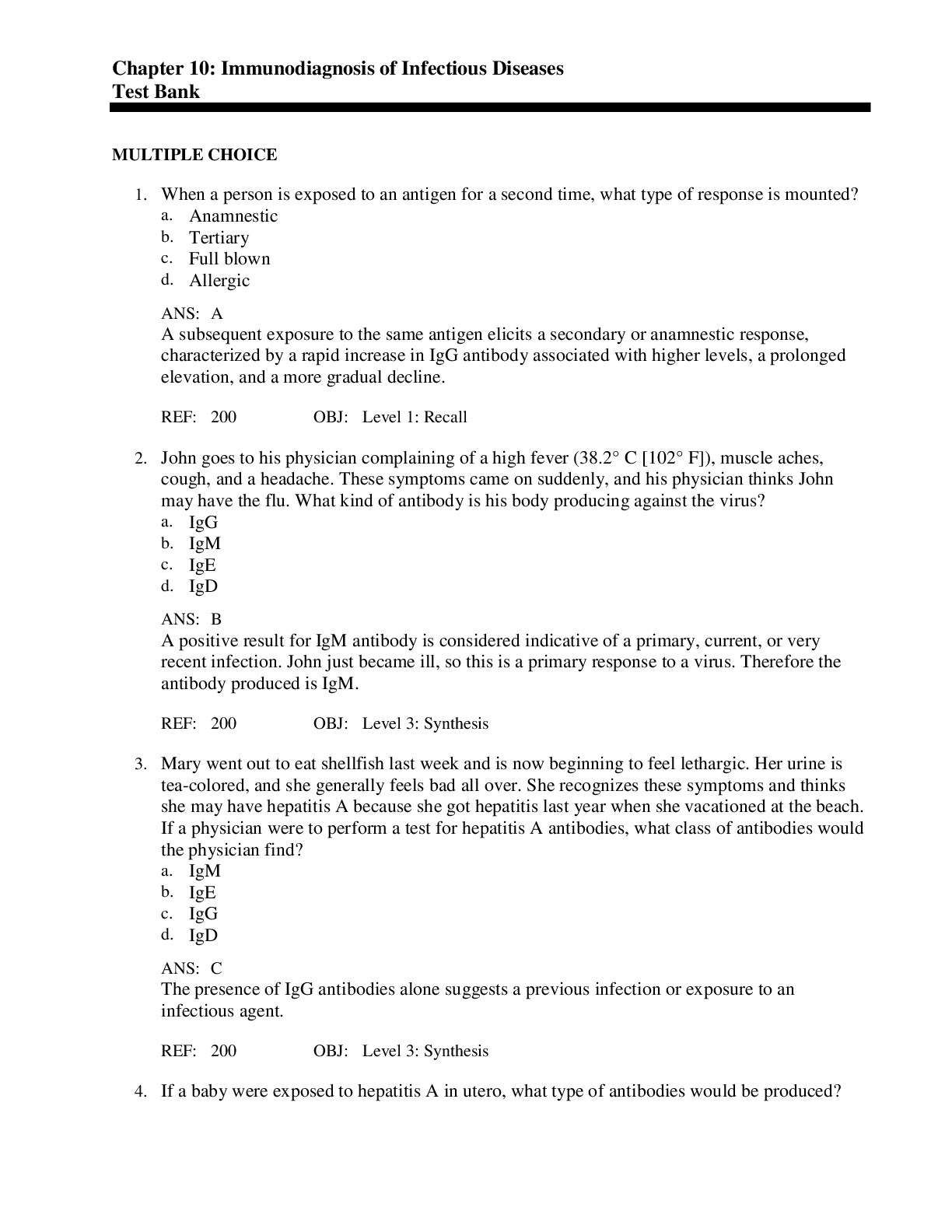
MULTIPLE CHOICE 1. When a person is exposed to an antigen for a second time, what type of response is mounted? a. Anamnestic b. Tertiary c. Full blown d. Allergic A A subsequent exposur... e to the same antigen elicits a secondary or anamnestic response, characterized by a rapid increase in IgG antibody associated with higher levels, a prolonged elevation, and a more gradual decline. REF: 200 OBJ: Level 1: Recall 2. John goes to his physician complaining of a high fever (38.2° C [102° F]), muscle aches, cough, and a headache. These symptoms came on suddenly, and his physician thinks John may have the flu. What kind of antibody is his body producing against the virus? a. IgG b. IgM c. IgE d. IgD B A positive result for IgM antibody is considered indicative of a primary, current, or very recent infection. John just became ill, so this is a primary response to a virus. Therefore the antibody produced is IgM. REF: 200 OBJ: Level 3: Synthesis 3. Mary went out to eat shellfish last week and is now beginning to feel lethargic. Her urine is tea-colored, and she generally feels bad all over. She recognizes these symptoms and thinks she may have hepatitis A because she got hepatitis last year when she vacationed at the beach. If a physician were to perform a test for hepatitis A antibodies, what class of antibodies would the physician find? a. IgM b. IgE c. IgG d. IgD C The presence of IgG antibodies alone suggests a previous infection or exposure to an infectious agent. REF: 200 OBJ: Level 3: Synthesis 4. If a baby were exposed to hepatitis A in utero, what type of antibodies would be produced? a. IgD b. IgE c. IgG d. IgM D The presence of significant levels of IgM antibodies (with or without IgG) in a newborn suggests in utero infection (IgM can be synthesized by the fetus and cannot cross the placenta), whereas IgG antibody only in the newborn is passive material transfer of antibodies. REF: 201 OBJ: Level 2: Interpretation 5. What is one of the most popular methods for physical removal of IgG? a. Miniature ion-exchange chromatography columns b. Thin-layer chromatography c. High-performance liquid chromatography (HPLC) d. Mass spectroscopy A One of the most popular methods for physical removal of IgG uses miniature ion-exchange chromatography columns to trap IgM while allowing IgG to be washed through with a buffer solution. The IgM antibody is then collected by elution from the column with a lower-pH buffer. REF: 201 OBJ: Level 1: Recall 6. How can one determine if a person has had a previous illness with an organism? a. Perform acute and convalescent IgM levels. b. Perform acute and convalescent IgG levels. c. Perform an IgM level 1 week after the symptoms start. d. Perform an IgG level 1 week after the symptoms start. B Unless a serologic test is designed to measure IgM-specific antibody for diagnosing a current infection or is being used to determine previous infections or immunization (immune status) by testing the IgG level in a single serum specimen, serodiagnosis of an infectious disease requires measurement of total antibody concentration in both acute-phase and convalescent-phase serum specimens. REF: 201 OBJ: Level 2: Interpretation 7. A significant rise in IgG detected during the convalescent phase is diagnostic for infection and is called: a. serologic adaptation. b. convalescence. c. seroconversion. d. acute phase reactant. C A significant rise in IgG detected during the convalescent (recovery phase), usually 2 weeks after onset of illness, is diagnostic for infection and is referred to as seroconversion. Although seroconversion usually occurs within 2 to 3 weeks after onset of illness, it may be delayed in certain patients or types of infection. REF: 201 OBJ: Level 1: Recall 8. A monoclonal antibody is an antibody that is derived from: a. one cell and exposed to many epitopes. b. many cells and exposed to one epitope. c. one cell and exposed to no epitopes. d. one cell initially, which has been exposed to one epitope. D This antibody is derived from one cell initially, which has been exposed to one epitope. This cell then divides and produces an antibody specific to this one epitope. Monoclonal antibodies are rarely found in nature and are usually associated with some type of abnormal immune disease process. REF: 201 OBJ: Level 1: Recall 9. Avidity means the antibodies have _____ binding kinetics to specific _____. a. strong; antigens b. weak; antigens c. strong; antibodies d. weak; antibodies A These antibodies have strong binding kinetics to specific antigens and have the ability to discriminate between closely related antigenic determinants. REF: 201 OBJ: Level 1: Recall 10. When the antigen-binding sites on the antibody molecule react with specific epitopes and not with other antigens containing different epitopes, this is antibody molecule is displaying: a. high sensitivity. b. high specificity. c. low specificity. d. low sensitivity. B Most antigen-antibody reactions show high specificity; that is, the antigen-binding sites on the antibody molecule react with specific epitopes and not with other antigens containing different epitopes. REF: 202 OBJ: Level 1: Recall 11. Heterophile antibodies are antibodies: a. produced in response to one antigen. b. that must be cleared through the thymus before going into circulation. c. produced in response to one molecule that also react against an antigen from another species. d. produced by T cells. C Antibodies produced in response to one molecule that also react against an antigen from an unrelated source are called heterophile antibodies. Because of antibody cross-reactivity, it is often best to perform a battery of serologic tests using organisms known to show cross-reactivity. REF: 202 OBJ: Level 1: Recall 12. A false-negative serologic test is defined as a: a. positive result for someone who is not infected. b. negative result for someone who does not have the disease. c. positive result for someone who does have the disease. d. negative result for a patient who really is infected. D A false-negative serologic test is defined as a negative result for a patient who really is infected. REF: 202 OBJ: Level 1: Recall 13. A false-negative test may be caused by all the following immune system-mediated reasons except: a. allergic reaction. b. no immune response. c. immunodeficiency disease. d. immunosuppression. A A false-negative serologic test result may occur because a person does not have an intact immune system and cannot mount an immune response. This might be the case in an individual with a congenital or acquired immunodeficiency disease or in a patient receiving either immunosuppressive therapy after organ transplantation or cancer chemotherapy. In addition, neonates may not always respond to an infectious agent because their immune systems are immature. REF: 203 OBJ: Level 2: Interpretation 14. What can cause a false-positive IgM serologic test? a. The presence of IgG antibodies b. The presence of rheumatoid factors c. The presence of Rh factor d. The presence of cytomegalovirus (CMV) antibodies B False-positive IgM antibody assays may also occur. These are due to the presence of rheumatoid factor activity in the serum. Rheumatoid factor is IgM antibody, produced in some individuals, that binds to the Fc region of the individual’s own IgG. IgM rheumatoid factor cannot be readily differentiated from organism-specific IgM in some serologic tests. REF: 203 OBJ: Level 2: Interpretation 15. Antibodies for many antigens can be passively acquired in: a. vaccinations. b. flu shots. c. intravenous immunoglobulin therapy. d. all of the above. C Finally, individuals receiving intravenous immunoglobulin, a product prepared by pooling large quantities of plasma from multiple volunteer donors, may show a specific antibody to a variety of infectious agents because of passive transfer, not active infection. REF: 203 OBJ: Level 1: Recall 16. Serologic tests can help epidemiologists: a. determine if people in a particular area are immune to an infectious agent. b. identify people that need to get immunizations. c. identify children that need to get immunizations. d. determine how widespread an infectious agent is in a given area. D Serologic tests for a specific infectious agent or a battery of agents may be performed to determine the percentage of individuals previously exposed or infected with the agent(s) in a geographic area. This information provides epidemiologists and public health officials with information about how widespread an infectious agent is in a given area. REF: 203 OBJ: Level 2: Interpretation 17. What tests are performed on newborns to detect congenital infections? a. TORCH b. TWAR c. CMV d. HIV A The agents most commonly tested for are the TORCH agents: Toxoplasma gondii, rubella virus, CMA and herpes simplex, and the Treponema pallidum subspecies pallidum. IgM antibody detection on neonatal serum is the method of choice for serologic diagnosis of congenital infection by one of the TORCH agents. REF: 204 OBJ: Level 1: Recall 18. What is the principle of direct antigen testing? a. A clinical specimen is mixed with an antigen, then a labeled antibody is added. If the antigen is present, a complex will form. b. It is a process by which microbial antigens are identified in patient specimens by combining specifically with antibody molecules to form stable complexes. c. A fluorescent antigen is added to a specimen, then an antibody to form sandwich complexes. d. Labeled antigen is added to a specimen, and the specimen is read for fluorescence. B Direct microbial antigen detection is the process by which microbial antigens, such as capsular polysaccharide or cell wall components, are identified in specimens obtained from an infected host. These antigens can be recognized by and can combine specifically with antibody molecules to form stable complexes. REF: 204 OBJ: Level 1: Recall 19. In precipitation assays, what is the precipitate made out of? a. Complement and protein complex b. Antibody and protein complex c. Antigen and antibody complex d. Antigen and protein complex C The precipitation reaction is found in assays involving the diffusion of soluble antigen and antibody. At a critical point, when the concentrations are optimal, a visible precipitate forms, which is composed of an insoluble complex of antigens and antibodies. REF: 204 OBJ: Level 1: Recall 20. What is the principle of the flocculation test? a. The antigen is incorporated into the agar and the test wells hold the antibody. The antibody and antigen combine at a specific concentration and produce a zone of equivalence. b. Antibodies are mixed with a labeled antigen, and a sandwich reaction occurs. c. Antibodies and antigens combine then precipitate out of a solution to the bottom of the tube. d. The antigen-antibody reaction forms a macroscopically visible clump that remains in solution. D Flocculation tests are a variation of precipitation tests that also have some properties of agglutination assays. In these tests, because of the chemical nature of the antigen (not a truly soluble antigen), the antigen-antibody reaction forms a macroscopically or microscopically visible clump or precipitate of fine particles that remain in suspension. REF: 205 OBJ: Level 1: Recall 21. Indirect agglutination is also referred to as: a. passive agglutination. b. incomplete agglutination. c. active agglutination. d. flocculation. A Indirect agglutination is also referred to as passive agglutination. The antigen or antibody is bound to a particulate carrier before forming an immune complex. REF: 206 OBJ: Level 1: Recall 22. What is the name of the test used to detect rickettsial agents? a. Levy-Jennings b. Mueller-Hinton c. Weil-Felix d. Watson-Crick C This approach is used in the Weil-Felix test to determine infection resulting from certain rickettsial agents by testing for agglutinating antibodies to various bacteria in the genus Proteus. REF: 212 OBJ: Level 1: Recall 23. All of the following controls must accompany the patient specimens in a latex agglutination test for antigen detection except _____ control. a. positive antigen b. negative antigen c. latex suspension d. positive antibody D Some important controls must accompany the patient specimens. These controls include a positive antigen control (a solution containing the known antigen of interest), a negative antigen control (a solution not containing the antigen), and a control of latex suspension to detect the presence of nonspecific agglutination reactions. REF: 206 OBJ: Level 2: Interpretation 24. Prozone occurs: a. when the relative concentration of an antibody exceeds the concentration of an antigen. b. when the relative concentration of an antigen exceeds the concentration of an antigen. c. when there are interfering substances in the specimen. d. in the equivalence zone. A Prozone occurs when the relative concentration of an antibody exceeds the concentration of an antigen. In this situation, each antigen combines with one or two antibody molecules, and cross-linking between antigen and antibody does not occur. REF: 207 OBJ: Level 1: Recall 25. The advantages of latex agglutination include all the following except: a. availability of good quality reagents in complete kit form. b. good sensitivity. c. ease of performance. d. cost of reagents. D The advantages of latex agglutination tests are the availability of good quality reagents in complete kit form, good sensitivity, relative rapidity, and ease of performance. Disadvantages include subjectivity in reading endpoints and nonspecific reactions resulting from interfering substances in clinical samples. LA tests are relatively inexpensive when compared to other methods. REF: 208 OBJ: Level 1: Recall 26. What test principle uses microbial antigens that are attached to erythrocytes after chemical treatment of the cells that promotes cross-linking of the antigens? a. Indirect hemagglutination (IHA) b. Enzyme immunoassay (EIA) c. Complement fixation (CF) d. Latex agglutination (LA) A In passive or indirect hemagglutination, microbial antigens are attached to erythrocytes after chemical treatment of the cells with tannic acid, chromic chloride, glutaraldehyde, or another substance that promotes cross-linking of the antigens. The sensitized cells can then be reacted with patient’s serum to detect an agglutinating antibody. REF: 209 OBJ: Level 2: Interpretation 27. A direct fluorescent antibody (DFA) test involves: a. an antigen-specific labeled antibody. b. an antibody-specific labeled antigen. c. a bioluminescent label. d. none of the above. A Detection techniques may be direct or indirect. In the DFA test, the clinical specimen containing the antigen of interest is fixed onto a glass slide with formalin, methanol, ethanol, or acetone. The antigen-specific labeled antibody is applied to the fixed specimen, incubated, washed, and examined with a fluorescent microscope. If the antigen was present in the clinical specimen, the labeled antibody will bind to the antigen and fluorescence will be seen. REF: 211 OBJ: Level 1: Recall 28. Enzyme immunoassay (EIA) differs from immunofluorescent tests by: a. using a different fluorescent label. b. using enzymes and a chromogenic substrate. c. being valid for direct testing only. d. all of the above. B EIA provides an alternative to immunofluorescent assays for detecting antigens and antibodies in clinical samples. Instead of labeling an antibody with a fluorochrome, EIA depends on the fact that enzyme molecules can be conjugated to specific antibodies in such a way that both enzymatic and antigen-binding activities are preserved. REF: 212 OBJ: Level 2: Interpretation 29. What is the advantage of using an indirect sandwich assay for EIA? a. One enzyme conjugated antiimmune antibody can be used for several tests. b. It is much more specific than direct sandwich EIA. c. It is much more sensitive than direct sandwich EIA. d. The lower detection limit is superior to any other EIA test. A The advantage of the indirect sandwich immunoassay is the need for only one enzyme conjugated antiimmunoglobulin antibody (third antibody) that can be used in different assays to detect a variety of antigens. REF: 213 OBJ: Level 2: Interpretation 30. What test has its results reported as the relative amount of a signal generated by the patient’s serum when compared with that of a known weakly positive serum? a. Enzyme immunoassay (EIA) b. Enzyme-linked immunosorbent assay (ELISA) c. Radioimmunoassay (RIA) d. Solid phase immunobead assay (SPIA) B Many laboratories are using some form of ELISA testing for antibody detection. In this test, results are reported not as antibody titer but as they relate to the relative amount of signal generated by the patient’s serum when compared with that of a known weakly positive serum. Results are usually reported either as relative units with a numerical reference range (units/mL) or as a ratio of results in the sample to the low positive control. REF: 215 OBJ: Level 2: Interpretation 31. What are the benefits of using membranes to perform enzyme immunoassay (EIA) reactions? a. They improve specificity and signal strength. b. They enhance speed and signal strength. c. They enhance speed and sensitivity. d. They improve specificity and sensitivity. C The flow-through and large surface area characteristics of nitrocellulose, nylon, or other membranes have been demonstrated to enhance the speed and sensitivity of EIA reactions. The improvements associated with membrane-bound EIAs are largely the result of immobilizing antibody onto the surface of porous membranes. REF: 216 OBJ: Level 2: Interpretation 32. What is used as the indicator in a complement fixation (CF) test? a. Latex particles b. Horse red blood cells c. Rabbit red blood cells d. Sheep red blood cells D The CF test is performed as a two-step procedure. The patient’s serum is serially diluted in test tubes, and each dilution is mixed with a known amount of antigen. A fixed amount of complement is then added to each tube, and the mixture is incubated. Next, the sheep erythrocytes and rabbit antibody are added to each tube, and the tubes are incubated again. REF: 218 OBJ: Level 1: Recall 33. What is one of the biggest uses for Western blot tests in the laboratory today? a. Confirming antibodies to HIV b. Confirming antibodies to cytomegalovirus (CMV) c. Confirming antibodies to rubella d. DNA sequencing from herpes A Western blotting has gained importance and is extensively used to confirm antibodies to HIV type 1 in patients whose sera have been repeatedly reactive in enzyme immunoassay (EIA) tests. REF: 218 OBJ: Level 1: Recall 34. The difference between dot blots and Western blots is that in dot blot testing: a. proteins are blotted to specific areas. b. proteins are purified and directly blotted to specific locations on the solid surface. c. DNA is purified and directly blotted to specific locations on the solid surface. d. RNA is purified and directly blotted to specific locations on the solid surface. B Immunoblots, or dot blots, are similar to Western blots, except the protein antigens are not electrophoretically separated and transferred to a solid surface. Instead, the proteins are purified and directly applied (blotted) to specific locations on the solid surface. REF: 219 OBJ: Level 2: Interpretation 35. Confirmatory tests for syphilis include all the following except: a. FTA-ABS. b. TP-PA. c. RPR. d. MHA-TP. C Examples of confirmatory tests for syphilis include the fluorescent treponema antibody absorbance (FTA-ABS) test and the Treponema pallidum particle agglutination (TP-PA) test, which has generally replaced the microhemagglutination assay for the Treponema pallidum (MHA-TP) test. Nontreponemal antigen tests are technically easier and more rapid to perform; therefore they are the tests of choice for syphilis screening. The most commonly used nontreponemal tests today are the Venereal Disease Research Laboratory (VDRL) and the rapid plasma reagin (RPR) tests. REF: 219 OBJ: Level 1: Recall 36. What is ASO used for? a. To demonstrate serologic response to streptococcal antigen b. To determine if a strep has been lysogenized c. To determine if a strep produces a hemolysin d. To demonstrate serologic response to Streptococcus pyogenes D The antistreptolysin-O, or ASO, antibody test is commonly used to demonstrate serologic response to S. pyogenes. REF: 220 OBJ: Level 1: Recall 37. Streptozyme detects all of the following except: a. streptokinase. b. hyaluronidase. c. streptolysin-O. d. hippurate hydrolysis. D As mentioned earlier, the streptozyme test is an indirect hemagglutination antibody (IHA) assay detecting antibodies to five different streptococcal proteins: streptolysin-O (ASO), deoxyribonuclease (DNase)-B, hyaluronidase, streptokinase, and nicotinamide adenine dinucleotidase (NADase). REF: 220 OBJ: Level 1: Recall 38. All of the following are congenital defects produced by rubella except: a. deafness. b. blindness. c. cataracts. d. congenital heart disease. B Rubella is normally insignificant except in pregnant women. This disease may cause a miscarriage, or it may cause congenital heart disease, cataracts, deafness, and brain damage in the unborn fetus. REF: 220 OBJ: Level 1: Recall 39. What test is used to diagnose an Epstein-Barr virus (EBV) infection? a. ASO b. EBV antibody c. Heterophile antibody d. Cold agglutinin C The heterophile antibody titer is one of the tests used to diagnose EBV infection, the causative agent of infectious mononucleosis. Recall that heterophile antibody refers to an antibody with an affinity to an antigen from more than one group or species. REF: 220 OBJ: Level 1: Recall 40. Infection with cytomegalovirus (CMV) in nonimmune pregnant women can cause: a. misshapen limbs. b. congenital heart defects. c. liver problems. d. microencephalopathy. D CMV, a herpesvirus, can be found in almost all body fluids. The virus can cross the placenta and may be transfused in blood and blood products. Nonpregnant women should be concerned about potential damage to the fetus, such as cerebral malformation (microencephalopathy) and necrosis of brain tissue. REF: 203 OBJ: Level 1: Recall 41. What patients are highly susceptible to cytomegalovirus (CMV) infections? a. Immunosuppressed b. Immunocompetent c. Males d. Females A Patients who are immunosuppressed are highly susceptible to CMV infection. Acquired immunodeficiency syndrome (AIDS) patients acquiring an acute infection with CMV may have eye damage and blindness as well as cerebral damage. REF: 223 OBJ: Level 1: Recall 42. How is hepatitis B transmitted? a. Contaminated food and water b. Blood and body fluids c. Respiratory droplets d. Airborne B The hepatitis B virus was discovered as early as 1965 and was originally named Australian antigen, because it was first diagnosed in an Australian man. The blood of an infected patient is infectious; the disease can also be sexually transmitted. REF: 221 OBJ: Level 1: Recall 43. What is the earliest serologic marker detected in hepatitis B? a. HAV b. HBsAg c. HBcAg d. HBeAg B One of the earliest markers detected in infections is the hepatitis B surface antigen (HBsAg). REF: 221 OBJ: Level 1: Recall 44. All of the following are antigens present in a hepatitis B infection except: a. HBsAg. b. HBcAg. c. HBeAg. d. VCNA. D VCNA is from Epstein-Barr virus. Additional antigen assays include detection of hepatitis B core antigen (HBcAg) and hepatitis B early antigen (HBeAg). REF: 221 OBJ: Level 2: Interpretation 45. All of the following are hepatitis antibodies except: a. EBNA. b. HBsAg. c. HBcAg. d. HBeAg. A EBNA is from the Epstein-Barr virus. The laboratory can also test for antibodies to the various antigens: anti-HBs antibody, anti-HBc antibody, and anti-HBe antibody. REF: 221 OBJ: Level 2: Interpretation 46. Which hepatitis virus is spread by the fecal/oral route? a. Hepatitis B b. Hepatitis A c. Hepatitis C d. Hepatitis D B The hepatitis A virus is generally spread by the fecal-oral route and by food handlers and children. REF: 221 OBJ: Level 1: Recall 47. Which hepatitis virus commonly leads to chronic hepatitis and cirrhosis, often requiring a liver transplant, and causes a high risk for development of liver cancer? a. Hepatitis A b. Hepatitis D c. Hepatitis C d. Hepatitis E C Many patients with hepatitis C virus infection are asymptomatic. However, even asymptomatic cases can progress to chronic hepatitis and cirrhosis, ultimately requiring a liver transplant. Both hepatitis B and hepatitis C viruses have been associated with liver cancer. REF: 221 OBJ: Level 2: Interpretation 48. Which test is a confirmatory test of enzyme-linked immunosorbent assay (ELISA) HIV? a. Enzyme immunoassay (EIA) b. Northern blot c. Southern blot d. Western blot D The detection of antihuman HIV antibodies has generally used two tests: ELISA for screening and the Western blot for confirmation. The Western blot test is highly sensitive and specific and remains the standard confirmatory test for HIV infection. REF: 221 OBJ: Level 1: Recall 49. What two methods are used to diagnose histoplasmosis and coccidioidomycosis? a. Complement fixation and immunodiffusion b. Enzyme immunoassay (EIA) and immunodiffusion c. Complement fixation and hemagglutination inhibition (HAI) d. Agglutination and precipitation A The laboratory can identify antibodies that occur in response to fungal disease by the use of complement fixation or immunodiffusion techniques. The primary fungi diagnosed by these means are histoplasmosis and coccidioidomycosis. REF: 221 OBJ: Level 1: Recall 50. What is one of the most widely used applications of the direct antigen test? a. HIV in saliva b. Group A strep in throat swabs c. Epstein-Barr virus (EBV) in urine d. Cytomegalovirus (CMV) in hair follicles B One of the most widely used applications of direct antigen tests, popularized in the 1980s, is for the detection of group A strep in throat swab specimens for the diagnosis of streptococcal pharyngitis. REF: 221 OBJ: Level 1: Recall 51. For which organism is DFA used for detection, despite the test having a low sensitivity (25% to 75%)? a. Neisseria b. Streptococcus c. Legionella d. Klebsiella C A variety of antigen detection methods for Legionella have been evaluated and compared with culture isolation. The DFA is commonly performed on respiratory specimens, although the sensitivity (25% to 75%) is much lower than culture. REF: 211 OBJ: Level 1: Recall 52. Which organism can cause hospitalization in young children and is detected using fluorescent antibodies? a. Bordetella b. Klebsiella c. Streptococcus d. Respiratory syncytial virus (RSV) D Of particular importance is the direct detection of RSV by fluorescent antibody or membrane-bound enzyme immunoassay (EIA) in nasopharyngeal samples. Rapid direct detection is important because RSV causes serious lower respiratory disease (bronchiolitis and pneumonia) in young children, often requiring hospitalization. REF: 222 OBJ: Level 2: Interpretation 53. Latex agglutination kits are currently available for all the following bacterial antigens except: a. Cryptococcus neoformans. b. Neisseria meningitidis. c. Haemophilus influenzae. d. Streptococcus pneumoniae. A Cryptococcus neoformans is a yeast, not a bacterial organism. Today, clinical laboratories typically use latex agglutination when performing rapid antigen testing for bacterial meningitis. The bacterial agents detected in commercially available kits include H. influenzae type b, N. meningitidis, S. pneumoniae, and S. agalactiae. REF: 222 OBJ: Level 1: Recall 54. All of the following are important pulmonary pathogens in transplant, cancer, and AIDS patients except: a. Cryptococcus. b. Group A Streptococcus. c. Pneumocystis. d. Cytomegalovirus (CMV). B Cryptococcus neoformans, CMV, and Pneumocystis (carinii) jirovecii are important pulmonary pathogens in transplant, cancer, and AIDS patients. REF: 223 OBJ: Level 1: Recall 55. How does Clostridium difficile produce pseudomembranous colitis and antibiotic-associated diarrhea? a. Endotoxin b. Hyaluronidase c. Toxin A and toxin B (exotoxins) d. Protease C C. difficile, an anaerobic gram-positive rod, causes pseudomembranous colitis and antibiotic-associated diarrhea. These diseases typically occur in hospitalized patients who are receiving antibiotics or other chemotherapeutic agents that alter bowel flora. The organism produces two exotoxins, toxins A and B, which are involved in pathogenesis. REF: 216 OBJ: Level 2: Interpretation 56. All of the following are identifiable viral agents of gastroenteritis except: a. Norwalk. b. rotavirus. c. enteric adenoviruses. d. cytomegalovirus (CMV). D The most important identifiable agents of viral gastroenteritis are human rotaviruses, enteric adenoviruses, caliciviruses, Norwalk virus, and Norwalk-like viruses. REF: 222 OBJ: Level 1: Recall [Show More]
Last updated: 2 years ago
Preview 1 out of 16 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$6.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jan 23, 2020
Number of pages
16
Written in
Additional information
This document has been written for:
Uploaded
Jan 23, 2020
Downloads
0
Views
84


.png)
.png)
.png)
.png)
.png)
.png)
.png)