*NURSING > QUESTIONS & ANSWERS > Pathophysiology Questions and Answers. All of them are here. 100%. Chapter 1to 50. (All)
Pathophysiology Questions and Answers. All of them are here. 100%. Chapter 1to 50.
Document Content and Description Below
Chapter 1: Cellular Biology MULTIPLE CHOICE 1. Which statement best describes the cellular function of metabolic absorption? 2. Most of a cell’s genetic information, including RNA and DN ... A, is contained in the: 3. Which component of the cell prodNuUceRsSIhNyGdTroBg.CenOMperoxide (H2O2) by using oxygen to remove hydrogen atoms from specific substrates in an oxidative reaction? 4. Which cell component is capable of cellular autodigestion when it is released during cell injury? 5. What is the sequence of steps in the development of a digestive enzyme by the pancreas cells from the initial transcription to the release from the cell? 6. During which phase of the cell cycle is DNA synthesized? 7. What organic compound facilitates transportation across cell membranes by acting as receptors, transport channels for electrolytes, and enzymes to drive active pumps? 8. Understanding the various steps of proteolytic cascades, such as caspase-mediated apoptosis and complement cascades, may be useful in designing drug therapy for which human diseases? 9. Which structure prevents water-soluble molecules from entering cells across the plasma membrane? 10. The fluid mosaic model explains: 11. Which form of cell communication is used to communicate within the cell itself and with other cells in direct physical contact? 12. Which mode of chemical signaling uses blood to transport communication to cells some distance away? 13. Which mode of chemical signaling uses local chemical mediators that are quickly taken up, destroyed, or immobilized? 14. Neurotransmitters affect the postsynaptic membrane by binding to: 15. How do cells receive communication from the extracellular fluid surrounding them? 16. When a second message is necessary for extracellular communication to be activated, it is provided by which one? 17. Under anaerobic conditions, what process provides energy for the cell? 18. What is the mechanism by which the energy produced from carbohydrates, proteins, and lipids is transferred to adenosine triphosphate (ATP)? 19. Passive transport is best described with which statement? 20. Active transport occurs across which type of membranes? 21. Which method of transport uses transmembrane proteins with receptors with a high degree 22. The movement of fluid across the arterial end of capillary membranes into the interstitial 23. Why is osmolality preferred over osmolarity as the measurement of osmotic activity in the clinical assessment of individuals? 24. A patient who has diarrhea receives a 3% saline solution intravenously to replace the sodium and chloride lost in the stoNoUl.RWSINhaGtTeBf.fCeOctMwill this fluid replacement have on cells? 25. The transport of glucose from the blood to the cell is accomplished by which process? 26. Potassium and sodium are transported across plasma membranes by: 27. What occurs during exocytosis? 28. Why is it possible for potassium to diffuse easily into and out of cells? 29. The cellular uptake of the nutrient cholesterol depends on which process? 30. What causes the rapid change in the resting membrane potential to initiate an action potential? 31. The action of platelet-derived growth factor is to stimulate the production of which cells? a. Platelets c. Connective tissue cells b. Epidermal cells d. Fibroblast cells 32. The role of cytokines in cell reproduction is that they: 33. What is the process of cellular reproduction? 34. Which statement is true about eukaryotic cells? 35. Which statement is true about phagocytosis? 36. A muscle cell possesses which specialized function? 37. When a mucous gland cell creates a new substance from previously absorbed material, this process is known as which specialized cellular function? 38. All cells are capable of what process? MULTIPLE RESPONSE 39. What are the major chemical components of the cell membranes? (Select all that apply.) 40. Which cells lose their ability to replicate and divide? (Select all that apply.) 41. Which statements are true concerning the process of facilitated diffusion? (Select all that apply). 42. Passive transport is dependent on: (Select all that apply.) 43. What is the primary function of proteins? (Select all that apply.) a. Proteins are binding units. MATCHING Match the structure with its function. Answers may be used more than once. A. Endoplasmic reticulum B. Ribosome C. Secretory vesicle D. Lysosomes 44. Packages and transports proteins. 45. Fuses with the plasma membrane to release contents from the cell. 46. Synthesizes and transports lipids. 47. Provides energy to digest proteins into amino acids. .Match the structure with its functiNoUn.RASInNsGwTeBrs.CmOaMy be used more than once. A. Passive-mediated transport B. Active-mediated transport C. Osmosis 44. Movement of water 45. Protein carrier 46. Facilitated diffusion 48. ANS: C PTS: 1 REF: Page 30 MSC: Osmosis is the movement of water down a concentration gradient; that is, across a semipermeable membrane from a region of higher water concentration to a lower water concentration. 49. ANS: B PTS: 1 REF: Page 32 MSC: In active-mediated transport, also called active transport, the protein transporter moves molecules against, or up, the concentration gradient. Unlike passive-mediated transport, active-mediated transport requires the expenditure of energy. 50. ANS: A PTS: 1 REF: Pages 31-32 MSC: In passive-mediated transport, also called facilitated diffusion, the protein transporter moves solute molecules through cellular membranes without expending metabolic energy. Chapter 2: Altered Cellular and Tissue Biology MULTIPLE CHOICE 1. Which type of cell adaptation occurs when normal columnar ciliated epithelial cells of the bronchial lining have been replaced by stratified squamous epithelial cells? 2. The loss of the adenosine triphosphate (ATP) during ischemia causes cells to: 3. The mammary glands enlarge during pregnancy primarily as a consequence of hormonal: 4. Free radicals play a major role in the initiation and progression of which diseases? 5. Free radicals cause cell damage by: 6. What is a consequence of plasma membrane damage to the mitochondria? 7. What is a consequence of leakage of lysosomal enzymes during chemical injury? 8. Lead causes damage within the cell by interfering with the action of: 9. Which statement is a description of the characteristics of apoptosis? 10. Lead poisoning affects the nervous system by: 11. Carbon monoxide causes tissue damage by: 12. Acute alcoholism mainly affects which body system? 13. During cell injury caused by hypoxia, an increase in the osmotic pressure occurs within the 14. Which statement is true regarding the difference between subdural hematoma and epidural hematoma? 15. What physiologic change occurs during heat exhaustion? 16. In hypoxic injury, sodium enters the cell and causes swelling because: 17. What is the most common site of lipid accumulation? 18. What mechanisms occur in the liver cells as a result of lipid accumulation? 19. Hemoprotein accumulations are a result of the excessive storage of: NURSINGTB.COM 20. Hemosiderosis is a condition that results in the excess of what substance being stored as hemosiderin in cells of many organs and tissues? 21. What is the cause of free calcium in the cytosol that damages cell membranes by uncontrolled enzyme activation? PTS: 1 REF: Pages 57-58 | Page 87 | Figure 2-24 22. What two types of hearing loss are associated with noise? 23. What type of necrosis results from ischemia of neurons and glial cells? 24. What type of necrosis is often associated with pulmonary tuberculosis? 25. What type of necrosis is associated with wet gangrene? 26. Current research supports the believe that, after heart muscle injury, the damage: 27. After ovulation, the uterine endometrial cells divide under the influence of estrogen. This process is an example of hormonal: 28. The abnormal proliferation of cells in response to excessive hormonal stimulation is called: 29. Removal of part of the liver leads to the remaining liver cells undergoing compensatory: 30. What is the single most common cause of cellular injury? 31. During cell injury caused by hypoxia, sodium and water move into the cell because: 32. In decompression sickness, emboli are formed by bubbles of: 33. Which is an effect of ionizing radiation exposure? 34. What is an example of compensatory hyperplasia? 35. It is true that nondividing cells are: 36. Dysplasia refers to a(n): 37. Current research has determined that chemical-induced cellular injury: MULTIPLE RESPONSE 38. Which organs are affected by lead consumption? (Select all that apply.) 39. What effect does fetal alcohol syndrome have on newborns? (Select all that apply.) 40. What organs are affected by the type of necrosis that results from either severe ischemia or chemical injury? (Select all that apply.) 41. It is true that melanin is: (Select all that apply.) 42. Examples of adaptive cellular responses include: (Select all that apply.) 43. Blunt force injuries would include a: (Select all that apply.) 44. Which statements are true regarding the effects of marijuana use? (Select all that apply.) Chapter 3: The Cellular Environment: Fluids and Electrolytes, Acids and Bases MULTIPLE CHOICE 1. Infants are most susceptible to significant losses in total body water because of an infant’s: 2. Obesity creates a greater risk for dehydration in people because: 3. A patient’s blood gases reveal the following findings: pH, 7.3; bicarbonate (HCO3) 27 mEq/L; carbon dioxide (CO2), 58 mm Hg. What is the interpretation of these gases? 4. Water movement between the intracellular fluid (ICF) compartment and the extracellular fluid (ECF) compartment is primarily a function of: 5. In addition to osmosis, what force is involved in the movement of water between the plasma and interstitial fluid spaces? 6. Venous obstruction is a cause of edema because of an increase in which pressure? 7. At the arterial end of capillaries, fluid moves from the intravascular space into the interstitial space because the: 8. Low plasma albumin causes edema as a result of a reduction in which pressure? 9. Secretion of antidiuretic hormone (ADH) and the perception of thirst are stimulated by a(n): 10. Thirst activates osmoreceptors by an increase in which blood plasma? 11. It is true that natriuretic peptides: 12. When changes in total body water are accompanied by proportional changes in electrolytes, what type of alteration occurs? 13. Which enzyme is secreted by the juxtaglomerular cells of the kidney when circulating blood volume is reduced? 14. What mechanism can cause hypernatremia? 15. What causes the clinical manifestations of confusion, convulsions, cerebral hemorrhage, and coma in hypernatremia? 16. Vomiting-induced metabolic alkalosis, resulting in the loss of chloride, causes: 17. The pathophysiologic process of edema is related to which mechanism? 18. Insulin is used to treat hyperkalemia because it: 19. A major determinant of the resting membrane potential necessary for the transmission of nerve impulses is the ratio between: 20. During acidosis, the body compensates for the increase in serum hydrogen ions by shifting hydrogen ions into the cell in exchange for which electrolyte? NURSINGTB.COM 21. Causes of hyperkalemia include: 22. In hyperkalemia, what change occurs to the cells’ resting membrane potential? 23. The calcium and phosphate balance is influenced by which three substances? 24. It is true that Kussmaul respirations indicate: 25. An excessive use of magnesium-containing antacids and aluminum-containing antacids can result in: 26. The most common cause of hypermagnesemia is: a. 27. Physiologic pH is maintained at approximately 7.4 because bicarbonate (HCO3) and carbonic acid (H2CO3) exist in a ratio of: 28. Which arterial pH will initiate the formation of ammonium (NH4) from ammonia (NH3), referred to as academia, in the tubular lumen of the kidney? 29. Two thirds of the body’s water is found in its: 30. It is true that when insulin is administered: 31. Increased capillary hydrostatic pressure results in edema because of: 32. The existence of hyperkalemia is likely to result in which changes to a person’s electrocardiogram (ECG)? MULTIPLE RESPONSE 33. Which groups are at risk for fluid imbalance? (Select all that apply.) 34. Dehydration can cause which result? (Select all that apply.) 35. Causes of hypocalcemia include: (Select all that apply.) 36. The electrolyte imbalance called hyponatremia exhibits which clinical manifestations? (Select all that apply.) 37. The electrolyte imbalance hypercalcemia exhibits which clinical manifestations? (Select all that apply.) , D, E Fatigue, weakness, lethargy, anorexia, nausea, and constipation are common. Behavioral changes may occur. Impaired renal function frequently develops, and kidney stones form 38. The electrolyte imbalance hypokalemia exhibits which clinical manifestations? (Select all that apply.) 39. A third of the body’s fluid is contained in the extracellular interstitial fluid spaces that include: (Select all that apply.) 40. An imbalance of potassium can produce which dysfunctions? (Select all that apply.) 41. Which statements regarding total body water (TBW) are true? (Select all that apply.) a. During childhood, TBW slowly decreases in relationship to body weight. MATCHING Match the electrolytes with the corresponding descriptions. Terms may be used more than once. A. Sodium B. Chloride C. Potassium D. Magnesium E. Phosphate 42. Regulates osmolality in the extracellular fluid (ECF) space. 43. Is inversely related to HCO3 concentration. 44. Is a major determinant of resting membrane potential. 45. An intracellular metabolic form is adenosine triphosphate (ATP). 46. Changes in hydrogen ion concentration affect this electrolyte. Chapter 4: Genes and Genetic Diseases MULTIPLE CHOICE 1. Inserting bone marrow cells into an individual who produces abnormal erythrocytes is an example of what type of therapy? 2. DNA replication requires the enzyme DNA polymerase to: 3. Transcription is best defined as a process by which: 4. The purpose of a staining technique of chromosomes such as Giemsa is to: 5. An amniocentesis indicates a neural tube defect when an increase in which protein is evident? 6. An amniocentesis is recommended for pregnant women who: 7. The most clinically useful technique for prenatal diagnosis of chromosomal abnormalities at 3 months’ (12 weeks’) gestation is: 8. The term for an error in which homologous chromosomes fail to separate during meiosis or mitosis is: 9. Which clinical manifestations would be expected for a child who has complete trisomy of the twenty-first chromosome? 10. What is the most common cause of Down syndrome? 11. What syndrome, characterized by an absent homologous X chromosome with only a single X chromosome, exhibits features that include a short stature, widely spaced nipples, and webbed neck? 12. A person with 47, XXY karyotype has the genetic disorder resulting in which syndrome? 13. What is the chromosomal variation that causes Klinefelter syndrome? 14. What is the second most commonly recognized genetic cause of mental retardation? 15. What is the blood type of a person who is heterozygous, having A and B alleles as codominant? 16. A couple has two children diagnosed with an autosomal dominant genetic disease. What is the probability that the next child will have the same genetic disease? 17. When a child inherits a disease that is autosomal recessive, it is inherited from: 18. People diagnosed with neurofibromatosis have varying degrees of the condition because of the genetic principle of: a. Penetrance c. Dominance b. Expressivity d. Recessiveness 19. Which genetic disease has been linked to a mutation of the tumor-suppressor gene? 20. Cystic fibrosis is caused by what type of gene? 21. Which is an important criterion for discerning autosomal recessive inheritance? 22. Consanguinity refers to the mating of persons: 23. Males, having only one X chromosome (as is expected), are said to be: 24. Males are more often affected by which type of genetic disease? 25. An X-linked recessive disease can skip generations because: 26. The presence of a zygote having one chromosome with the normal complement of genes and one with a missing gene is characteristic of which genetic disorder? 27. A child with which genetic disorder has a characteristic cry? 28. Which statement is true regarding X-linked recessive conditions? 29. DNA formation occurs in which of the cell’s structures? 30. What is the risk for the recurrence of autosomal dominant diseases? 31. An individual’s genetic makeup is referred to as his or her: MULTIPLE RESPONSE 32. Which disorders have similar modes of inheritance? (Select all that apply.) 33. The key to accurate DNA replication depends on which complementary base pairs? (Select all that apply.) 34. Chromosomal abnormalities are the leading known cause of: (Select all that apply.) 35. Examples of prenatal diagnostic studies include: (Select all that apply.) 36. The advantage derived from human genome sequencing on genetic disorders focuses on: (Select all that apply.) MATCHING Match the genetic terms with the corresponding diseases. Terms may be used more than once. A. Autosomal dominant B. Autosomal recessive C. X-linked dominant D. X-linked recessive 37. Cystic fibrosis 38. Duchenne muscular dystrophy 39. Sickle cell disease 40. Huntington disease Chapter 5: Genes, Environment-Lifestyle, and Common Diseases MULTIPLE CHOICE 1. The data reporting that sickle cell disease affects approximately 1 in 600 American blacks is an example of which concept? 2. The ratio of the disease among the exposed population to the disease rate in an unexposed population is referred to as what type of risk? a. Attributable c. Causal b. Contingency d. Relative 3. Empirical risks for most multifactorial diseases are based on: 4. What is the cause of familial hypercholesterolemia (FH)? 5. Which risk factor for hypertension is influenced by genetic factors and lifestyle? 6. What percentage of all cases of breast cancer are identified as an autosomal dominant form? 7. When a woman has one first-degree relative with breast cancer, her risk of developing breast cancer is how many times greater? 8. Adoption studies have shown that the offspring of an alcoholic parent when raised by nonalcoholic parents have what amount of an increased risk of developing alcoholism? 9. Studies have identified several genes that play a role in the prevention of obesity by affecting what? 10. The BRCA1 and BRCA2 mutations increase the risk of which cancer in women? 11. Blood pressure variations are assoNcUiaRteSdINwGiTthB:.COM 12. The two most important risk factors for type 2 diabetes are: 13. A major characteristic of type 1 diabetes mellitus is that there is: 14. Obesity acts as an important risk factor for type 2 diabetes mellitus by: 15. Traits caused by the combined effects of multiple genes are referred to by which term? 16. Regarding type 2 diabetes, obesity is considered to be what type of risk? 17. Which disease form is identified on the basis of empirical risk observation? 18. The number of persons living with a specific disease at a specific point in time is referred to by which term? 19. Which type of cancer is said to aggregate among families? 20. Which dietary lifestyle choice has been associated with a decreased risk for developing colon cancer? 21. It is currently believed that the risk for developing Alzheimer disease: 22. The number of new cases of a disease reported during a specific period divided by the number of individuals in the population is defined as which characteristic of a disease? MULTIPLE RESPONSE 23. Cancers that cluster strongly in families include: (Select all that apply.) a. Breast 24. dominant form of breast cancer? (Select all that apply.) a. LCAT b. CHK1 c. CHK2 d. BRCA1 e. BRCA2 25. Lifestyle modifications that affect health-related risk factors include: (Select all that apply.) a. Diet b. Exercise 26. What factors are typically considered when assessing an individual’s risk for developing such common diseases as hypertension? (Select all that apply.) a. Age b. Diet c. Exercise habits 27. Examples of multifactorial diseases associated with adults include: (Select all that apply.) MATCHING Match the terms with the corresponding descriptions. A. Incidence rate effect of multiple genes B. Gene-environment interaction C. Prevalence rate at which some diseases occur D. Obesity E. Polygenic F. Empirical risk G. Relative risk 28. Traits caused by the combined effects of multiple genes 29. Number of persons living with the disease 30. Yields an increased risk for some diseases 31. Modifiable risk factor for many diseases 32. Number of new cases (persons) detected with the disease 33. Measure of the effect of a specific risk factor 34. Risks based on direct observation of data Chapter 6: Epigenetics and Disease MULTIPLE CHOICE 1. What genetic process is likely responsible for the occurrence of asthma in only one of a pair of identical twins? 2. Prader-Willi syndrome causes a chromosomal defect that is: 3. A malfunction in DNA methylation can lead to: 4. Which statement is true regarding the embryonic development of stem cells? 5. When microRNA (miRNA) are methylated their messenger RNA (mRNA) targets are over-expressed, the resulting effect on existing cancer would be: 6. The difference between DNA sequence mutations and epigenetic modifications is: 7. Which term refers to the silenced gene of a gene pair? 8. The shape of the face of a child diagnosed with Russell-Silver syndrome is likely to be: 9. Genes responsible for the maintenance of all cells are referred to as: 10. What is the belief regarding twins who adopt dramatically different lifestyles? 11. Hypomethylation and the resulting effect on oncogenes result in a(an): 12. When a chromosome lacking 4 Mb is inherited from the mother, the child is at risk for developing which syndrome? MULTIPLE RESPONSE 13. A child’s diagnosis of Beckwith-Wiedemann syndrome is supported by the presence of: (Select all that apply.) a. An omphalocele 14. A diagnosis of Angelman syndrome in a child is supported by which assessment findings? (Select all that apply.) a. Small feet and hands b. Profound cognitive dysfunction Chapter 7: Innate Immunity: Inflammation MULTIPLE CHOICE 1. Which action is a purpose of the inflammatory process? 2. How do surfactant proteins A through D provide innate resistance? 3. Which secretion is a first line of defense against pathogen invasion that involves antibacterial and antifungal fatty acids, as well as lactic acid? 4. Which bacterium grows in the intestines after prolonged antibiotic therapy? 5. What causes the edema that occurs during the inflammatory process? 6. What process causes heat and redness to occur during the inflammatory process? 7. Activation of the classical pathway begins with: 8. What plasma protein system forms a fibrinous meshwork at an inflamed site? 9. Which component of the plasma protein system tags pathogenic microorganisms for destruction by neutrophils and macrophages? 10. What is the vascular effect of histamine released from mast cells? 11. What is an outcome of the compleNmUeRnStINcaGsTcBad.CeO?M 12. The function of opsonization related to the complement cascade is to: 13. In the coagulation (clotting) cascade, the intrinsic and the extrinsic pathways converge at which factor? 14. Which chemical interacts among all plasma protein systems by degrading blood clots, activating complement, and activating the Hageman factor? 15. The chemotactic factor affects the inflammatory process by: 16. What affect does the process of histamine binding to the histamine-2 (H2) receptor have on inflammation? 17. Frequently when H1 and H2 receptors are located on the same cells, they act in what fashion? 18. Some older adults have impaired inflammation and wound healing because of which problem? 19. Which chemical mediator derived from mast cells retracts endothelial cells to increase vascular permeability and to cause leukocyte adhesion to endothelial cells? a. Leukotrienes c. Platelet-activating factor b. Prostaglandin E d. Bradykinin 20. What is the inflammatory effect of nitric oxide (NO)? 21. What is the correct sequence in phagocytosis? 22. When considering white blood celNlUdRifSfIeNreGnTtBia.lCsO, aMcute inflammatory reactions are related to elevations of which leukocyte? 23. In the later stages of an inflammatory response, which phagocytic cell is predominant? 24. In regulating vascular mediators released from mast cells, the role of eosinophils is to release: 25. What is the role of a natural killer (NK) cells? 26. Which cytokine is produced and rNelUeRasSeINd GfrToBm.CvOiMrally infected host cells? 27. IFN- is secreted from which cells? 28. Which manifestation of inflammation is systemic? 29. The acute inflammatory response is characterized by fever that is produced by the hypothalamus being affected by: 30. What occurs during the process of repair after tissue damage? a. Nonfunctioning scar tissue replaces destroyed tissue. b. Regeneration occurs; the original tissue is replaced. c. Resolution occurs; tissue is regenerated. 31. The role of fibroblasts during the reconstructive phase of wound healing is to: 32. A keloid is the result of which dysfunctional wound healing response? 33. Which solution is best to use when cleaning a wound that is healing by epithelialization? 34. Many neonates have a transient depressed inflammatory response as a result of which condition? 35. During phagocytosis, what is occurring during the step referred to as opsonization? 36. Fusion is the step in phagocytosis during which: 37. During the process of endocytosis, the phagosome step results in: 38. When cellular damage occurs and regeneration is minor with no significant complications, 39. Newborns often have deficiencies in collectin-like proteins, making them more susceptible to what type of infection? 40. Which cell is the body’s primary defense against parasite invasion? MULTIPLE RESPONSE 41. Which chemical mediators induce pain during an inflammatory response? (Select all that apply.) a. Prostaglandins 42. Sebaceous glands protect the bodyNUfrRoSmINinGfTeBc.tCioOnMby secreting: (Select all that apply.) 43. Which body fluid has the ability to attack the cell walls of gram-positive bacteria? (Select all that apply.) 44. The main function of NK cells includes: (Select all that apply.) a. Recognizing virus-infected cells 45. Normal bacterial flora found in the intestines produce vitamin K to assist in the absorption of which of the following? (Select all that apply.) a. Calcium 46. An individual’s acquired immunity is dependent on the function of which cells? (Select all that apply.) a. T lymphocytes 47. An example of a pathogen capable of surviving and even multiplying inside a macrophage is known as: (Select all that apply.) 48. An older adult is particularly susceptible to infections of which body parts? (Select all that apply.) MATCHING NURSINGTB.COM Match each step of phagocytosis with its function. A. Opsonization B. Engulfment C. Phagosome D. Fusion E. Destruction 49. Microorganisms are ingested. 50. Microorganisms are killed and digested. 51. Phagocytes gain enhanced recognition and adherence of bacteria. 52. Lysosomal granules enter the phagocyte. 53. Intracellular phagocytic vacuole is formed. NURSINGTB.COM Chapter 8: Adaptive Immunity MULTIPLE CHOICE 1. Which primary characteristic is unique for the immune response? 2. In which structure does B lymphocytes mature and undergo changes that commit them to becoming B cells? 3. What is the term for the process during which lymphoid stem cells migrate and change into either immunocompetent T cells or immunocompetent B cells? 4. Which type of immunity is produced by an individual after either natural exposure to the antigen or after immunization against the antigen? 5. What type of immunity is produced when an immunoglobulin crosses the placenta? 6. The portion of the antigen that is configured for recognition and binding is referred to as what type of determinant? 7. Which characteristic is the most important determinant of immunogenicity when considering the antigen? 8. When antigens are administered to produce immunity, why are different routes of administration considered? 9. The functions of the major histocompatibility complex (MHC) and CD1 molecules are alike because both: 10. Where are antibodies produced? 11. Which immunoglobulin is present in blood, saliva, breast milk, and respiratory secretions? 12. Which antibody initially indicates a typical primary immune response? 13. An individual is more susceptible to infections of mucous membranes when he or she has a seriously low level of which immunoglobulin antibody? 14. The B-cell receptor (BCR) complex functions uniquely by: 15. The generation of clonal diversity occurs primarily during which phase of life? 16. The generation of clonal diversity includes a process that: 17. Which statement is true concerning clonal selection? a. Clonal selection is driven by hormones and does not require foreign antigens. b. This theory involves antigens that select those lymphocytes with compatible receptors. c. Clonal selection takes place in the primary (central) lymphoid organs. d. This process generates immature but immunocompetent T and B cells with receptors. 18. Which is an example of an endogenous antigen? 19. Which cytokine is needed for the maturation of a functional helper T cell? 20. Th2 cells produce IL-4 and suppress which cells? 21. Which statement is believed to be true concerning Th1 cells? 22. Which statement is believed to be true concerning Th2 cells? 23. When a person is exposed to most antigens, antibodies can be usually detected in his or her circulation within: 24. Vaccinations are able to provide protection against certain microorganisms because of the: 25. Why is the herpes virus inaccessible to antibodies after the initial infection? 26. Increased age may cause which change in lymphocyte function? 27. How do antibodies protect the host from bacterial toxins? 28. Which T cell controls or limits the immune response to protect the host’s own tissues against an autoimmune response? 29. Evaluation of umbilical cord blood can confirm that which immunoglobulin level is near adult levels? 30. Which statement is true concerning the IgM? 31. Which cell has the ability to recognize antigens presented by the MHC class I molecules? 32. Which cell has a role in developing cell-mediated immunity? 33. How does the aging process of the T-cell activity affect older adults? 34. Which statement is true regarding maternal antibodies provided to the neonate? 35. Antibodies that are associated with mucosal immune system, such as immunoglobulins, function to prevent which type of infections? 36. Cytokines are vital to a cell’s ability to do which function? MULTIPLE RESPONSE 37. Which is an example of a bacterial toxin that has been inactivated but still retains its immunogenicity to protect the person? (Select all that apply.) a. Poliomyelitis b. Measles 38. Which statements are true concerning the humoral immune response? (Select all that apply.) 39. CD4 is a characteristic surface marker and a result of which of the following? (Select all that apply.) 40. What are the necessary components of an adaptive immune response? (Select all that apply.) MATCHING Match each immunoglobulin with its characteristic or function. Each immunoglobulin can be used only once. A. IgA B. IgE C. IgG 41. Crosses the placenta. 42. Is predominantly found in the blood and body secretions. 43. Mediates many common allergic responses Chapter 9: Alterations in Immunity and Inflammation MULTIPLE CHOICE 1. Hypersensitivity is best defined as a(an): 2. A hypersensitivity reaction that produces an allergic response is called: 3. The common hay fever allergy is NexUpRrSeIsNseGdTBth.CroOuMgh a reaction that is mediated by which class of immunoglobulins? 4. Which type of antibody is involved in type I hypersensitivity reaction? 5. Blood transfusion reactions are an example of: 6. During an IgE-mediated hypersensitivity reaction, which leukocyte is activated? 7. During an IgE-mediated hypersensitivity reaction, what causes bronchospasm? 8. During an IgE-mediated hypersensitivity reaction, the degranulation of mast cells is a result of which receptor action? 9. What characteristic do atopic individuals have that make them genetically predisposed to develop allergies? 10. What is the mechanism that results in type II hypersensitivity reactions? 11. When mismatched blood is administered causing an ABO incompatibility, the erythrocytes are destroyed by: 12. When antibodies are formed against red blood cell antigens of the Rh system, the blood cells are destroyed by: 13. When soluble antigens from infectious agents enter circulation, tissue damage is a result of: 14. How are target cells destroyed in a type II hypersensitivity reaction? a. Complement-mediated cell lysis 15. Graves disease (hyperthyroidism) is an example of which type II hypersensitivity reaction? a. Modulation 16. Type III hypersensitivity reactions are a result of which of the following? 17. A type IV hypersensitivity reaction causes which result? 18. In a type III hypersensitivity reaction, the harmful effects after the immune complexes that are deposited in tissues are a result of: 19. Raynaud phenomenon is classified as a type III hypersensitivity reaction and is due to: 20. Deficiencies in which element can produce depression of both B- and T-cell function? 21. When the maternal immune system becomes sensitized against antigens expressed by the fetus, what reaction occurs? 22. Tissue damage caused by the deposition of circulating immune complexes containing an antibody against the host DNA is the cause of which disease? 23. Why does tissue damage occurs in acute rejection after organ transplantation? 24. Which blood cell carries the carbohydrate antigens for blood type? 25. A person with type O blood is likely to have high titers of which anti-antibodies? 26. Which class of immunoglobulins forms isohemagglutinins? NURSINGTB.COM 27. Which component of the immune system is deficient in individuals with infections caused by viruses, fungi, or yeast? 28. In which primary immune deficiency is there a partial-to-complete absence of T-cell immunity? 29. How many months does it take for the newborn to be sufficiently protected by antibodies produced by its own B cells? 30. Considering the effects of nutritional deficiencies on the immune system, severe deficits in calories and protein lead to deficiencies in the formation of which immune cells? 31. Urticaria are a manifestation of a which type of hypersensitivity reaction? 32. Graves disease is a result of: 33. Raynaud phenomenon is an example of which type of hypersensitivity? 34. Which statement is true concerning an atopic individual? 35. Which statement is true regarding immunodeficiency? .COM 36. A person with type O blood is considered to be the universal blood donor because type O blood contains which of the following? 37. Immunoglobulin E (IgE) is associated with which type of hypersensitivity reaction? 38. Graves disease is an autoimmune disease that results in which maternal antibody? MULTIPLE RESPONSE 39. When a tuberculin skin test is positive, the hard center and erythema surrounding the induration are a result of which of the following? (Select all that apply.) 40. Exposure to which of the following could result in a type IV hypersensitivity reaction? (Select all that apply.) 41. Which disorders are considered autoimmune? (Select all that apply.) 42. Which statements best define acute rejection? (Select all that apply.) NURSINGTB.COM Chapter 10: Infection MULTIPLE CHOICE 1. What is a significant cause of morbidity and mortality worldwide? 2. What is the first stage in the infectious process? 3. Which type of microorganism repNroUdRuScIeNsGoTnBt.CheOMskin? 4. Phagocytosis involves neutrophils actively attacking, engulfing, and destroying which microorganisms? 5. Once they have penetrated the first line of defense, which microorganisms do natural killer (NK) cells actively attack? 6. Which statement concerning exotoxins is true? 7. Which statement is true concerning a fungal infection? 8. Cytokines are thought to cause fevers by stimulating the synthesis of which chemical mediator? 9. Considering the hypothalamus, a fever is produced by: 10. Which statement about vaccines is true? 11. Vaccines against viruses are created from: 12. Which statement is a characteristic of HIV? 13. What is the role of reverse transcriptase in HIV infection? 14. After sexual transmission of HIV, a person can be infected yet seronegative for how many months? 15. Which cells are primary targets for HIV? 16. What area in the body may act as a reservoir in which HIV can be relatively protected from antiviral drugs? 17. AIDS produces a striking decrease in the number of which cells? 18. HIV antibodies appear within how many weeks after infection through blood products? 19. What is the final stage of the infectious process? 20. Toxigenicity is defined as the: 21. The ability of the pathogen to invade and multiply in the host is referred to as: 22. Some bacterial surface proteins bind with the crystalline fragment (Fc) portion of an antibody to: 23. Which organism is a common sexually transmitted bacterial infection? 24. Which disease is an example of a rickettsial infection? MULTIPLE RESPONSE 25. Which secretion transmits HIV? (Select all that apply.) a. Semen 26. Which infection is fungal? (Select all that apply.) 27. Which statement is true regarding the development of HIV symptoms? (Select all that apply.) 28. Which statements are true regarding endotoxins? (Select all that apply.) 29. Which statements are true regarding viruses? (Select all that apply.) 30. Which of the following play a role in the control of fungal infections? (Select all that apply.) 31. Complications of AIDS include: (Select all that apply.) a. Kaposi sarcoma MATCHING Match each term with its definition. A. Toxigenicity B. Infectivity C. Pathogenicity D. Virulence 32. Ability of the pathogen to invade and multiply in the host 33. Capacity of a pathogen to cause severe disease 34. An important factor in determining a pathogen’s ability to produce disease by the production of a soluble toxin 35. Ability of an agent to produce disease NURSINGTB.COM Chapter 11: Stress and Disease MULTIPLE CHOICE 1. Exhaustion occurs if stress continues when which stage of the general adaptation syndrome is not successful? 2. Which organ is stimulated during the alarm phase of the general adaptation syndrome (GAS)? 3. During an anticipatory response to stress, the reaction from the limbic system is stimulated by the: 4. Which hormone prompts increased anxiety, vigilance, and arousal during a stress response? 5. Perceived stress elicits an emotional, anticipatory response that begins where? 6. During a stress response, the helper T (Th) 1 response is suppress by which hormone? 7. What is the effect that low-serum albumin has on the central stress response? 8. Stress-age syndrome directly results in depressed function of which system? 9. Stress-induced sympathetic stimulation of the adrenal medulla causes the secretion of: 10. Stress-induced norepinephrine results in: 11. Released stress-induced cortisol results in the stimulation of gluconeogenesis by affecting which structure? 12. What is the effect of increased secretions of epinephrine, glucagon, and growth hormone? 13. Which hormone increases the formation of glucose from amino acids and free fatty acids? 14. What effect do androgens have on lymphocytes? 15. Which gland regulates the immune response and mediates the apparent effects of circadian rhythms on immunity? 16. Which cytokines initiate the production of corticotropin-releasing hormone (CRH)? 17. The release of which cytokines is triggered by bacterial or viral infections, cancer, and tissue injury that, in turn, initiate a stress response? 18. The action of which hormone helps explain increases in affective anxiety and eating disorders, mood cycles, and vulnerability to autoimmune and inflammatory diseases in women as a result of stimulation of the CRH gene promoter and central norepinephrine system? 19. What effect does estrogen have on lymphocytes? 20. Which statement is true concerning the differences between stress-induced hormonal alterations of men and women? 21. Diagnostic blood work on individuals who perceive themselves to be in a chronic stress state will likely demonstrate: 22. What are the signs that a patient is in the adaptive stage of the general adaptation syndrome? 23. The most influential factor in whether a person will experience a stress reaction is his or her: 24. A reduction is an individual’s number of natural killer (NK) cells appears to correlate with an increased risk for the development of: 25. A nurse is providing care to a terminally ill adult who has been with his life partner for over 56 years. Research supports the nurse’s assessment of the life partner for signs of: MULTIPLE RESPONSE 26. The effect epinephrine has on the immune system during the stress response is to increase which cells? (Select all that apply.) a. NK cells 27. Which immune cells are suppressed by the corticotropin-releasing hormone (CRH)? (Select all that apply.) a. Monocyte-macrophage cells 28. The increased production of proinflammatory cytokines is associated with which considerations? (Select all that apply.) 29. Which statements are true regarding lymphocytes? (Select all that apply.) a. Lymphocytes are involved in the production of the human growth hormone. MATCHING Match the hormone with its effects during a stress response. Hormones may be used more than once. A. Epinephrine B. Norepinephrine C. Cortisol 30. Constricts peripheral vessels to increase blood pressure. 31. Increases cardiac output by increasing heart rate and myocardial contractility. 32. Increases gastric secretions. Chapter 12: Cancer Biology MULTIPLE CHOICE 1. Which cancer originates from connective tissue? 2. Carcinoma refers to abnormal cell proliferation originating from which tissue origin? 3. Carcinoma in situ is characterized by which changes? 4. Which term is used to describe a muscle cell showing a reduced ability to form new muscle while appearing highly disorganized? 5. What are tumor cell markers? 6. The function of the tumor cell marker is to: NURSINGTB.COM 7. Which statement supports the hypothesis that intestinal polyps are benign neoplasms and the first stage in the development of colon cancer? 8. Autocrine stimulation is the ability of cancer cells to: 9. Apoptosis is a(an): a. Normal mechanism for cells to self-destruct when growth is excessive 10. Many cancers create a mutation of ras. ras is a(an): a. Tumor-suppressor gene 11. Oncogenes are genes that are capable of: a. Undergoing mutation that directs the synthesis of proteins to accelerate the rate of 12. Burkitt lymphomas designate a chromosome that has a piece of chromosome 8 fused to a piece of chromosome 14. This is an example of which mutation of normal genes to oncogenes? 13. In childhood neuroblastoma, the N-myc oncogene undergoes which type of mutation of normal gene to oncogene? a. Point mutation c. Gene amplification b. Chromosome fusion d. Chromosome translocation 14. What aberrant change causes the abnormal growth in retinoblastoma? 15. Two “hits” are required to inactivate tumor-suppressor genes because: 16. The ras gene converts from a proto-oncogene to an oncogene by: 17. How do cancer cells use the enzyme telomerase? 18. What are characteristics of benign tumors? 19. Which terms represent the correct nomenclature for benign and malignant tumors of adipose tissue, respectively? 20. What is the major virus involved in the development of cervical cancer? 21. The Papanicolaou (Pap) test is used to screen for which cancer? 22. What is the skin-related health risk induced by some types of chemotherapy? 23. Which cancers are all associated with chronic inflammation? 24. Chronic inflammation causes cancer by: 25. Inherited mutations that predispose to cancer are almost invariably what kind of gene? 26. What is the consequence for cells when the functioning TP53 gene is lost as a result of mutation? 27. Which gastrointestinal tract condition can be an outcome of both chemotherapy and radiation therapy? 28. What is the role of vascular endothelial growth factor (VEGF) and basic fibroblast growth factor (bFGF) in cell metastasis? 29. It has been determined that a tumor is in stage 2. What is the meaning of this finding? 30. Which statement is true regarding pain and cancer? 31. Which cancer may be treated with radiation delivered by brachytherapy? 32. The survival rate for stage IV Hodgkin disease can be as high as: 33. What is the cause of anemia in a patient diagnosed with pancreatic cancer? 34. By what process do cancer cells multiply in the absence of external growth signals? 35. What is the role of caretaker genes? 36. In a normal, nonmutant state, an oncogene is referred to as a: 37. Which statement is true regarding pleomorphic cells? 38. What is the most commonly reported symptom of cancer treatment? 39. The most common site of metastasis for a patient diagnosed with prostate cancer is which location? 40. Which statement concerning benign tumors is true? MULTIPLE RESPONSE 41. Normally, which cells are considered immortal (never die)? (Select all that apply.) a. Germ b. Stem 42. What is the most common route for distant metastasis? (Select all that apply.) a. Seeding b. Blood 43. What cellular characteristics are affected by anaplasia? (Select all that apply.) a. Size b. Ability to differentiate 44. What are the most common causes of nosocomial infections among patients with cancer? (Select all that apply.) 45. Which statements concerning aging and the occurrence of cancer are true? (Select all that apply.) a. Decline in immunologic functions MATCHING Match the phrases with the corresponding terms. A. Is the process of cancer cell growth. B. Is used to kill cancer cells while minimizing damage to normal structures. C. Is guided by molecular analysis in specific diseases. D. Takes advantage of specific vulnerabilities in specific cancer cells. E. Provides a framework to determine treatment. 46. Chemotherapy 47. Radiation 48. Staging 49. Angiogenesis 50. Target agent MICS: The newest highly targeted agents that are used to treat cancer exploit specific vulnerabilities uncovered by molecular analysis in specific diseases. Match the organism factor with the cancer it causes. A. HPV B. Human herpesvirus (HHV) 8 C. Hepatis B virus (HBV) D. Helicobacter pylori 51. Cervical cancer 52. Kaposi sarcoma 53. Liver cancer 54. Stomach cancer NURSINGTB.COM Chapter 13: Cancer Epidemiology MULTIPLE CHOICE 1. Which characteristic among women correlates with a high morbidity of cancer of the colon, uterus, and kidney? 2. Which substance has been shown to increase the risk of cancer when used in combination with tobacco smoking? 3. Which cancers pose the highest risk for radiologists? 4. Research has shown a link between cancer and which sexually transmitted disease? 5. Research has supported that alcohol consumption has a convincing impact on increasing the risk of which cancer? 6. Research supports the premise that exercise has a probable impact on reducing the risk of which cancer? 7. The World Health Organization (WNUHROSI)NdGeTfiBn.eCsOgMrade 1 (overweight) as a BMI of: MULTIPLE RESPONSE 8. Tobacco smoking is associated with which cancers? (Select all that apply) a. Lung b. Skin 9. The significant risk factors associated with the development of basal cell carcinoma include: (Select all that apply.) a. Light-colored hair 10. Which environmental factors have been shown to have greatest significant effect on the frequency of genetic mutations in humans? (Select all that apply.) 11. Research data support the relationship between the exposure of ultraviolet light (UVL) and the development of: (Select all that apply.) a. Basal cell carcinoma 12. Alcohol consumption has been proven to be a consistent risk factor in the development of which major cancer? (Select all that apply.) a. Colorectal 13. Nutritional counseling regarding cancer stem cell repopulation must stress the importance of including sufficient quantities of what in a daily diet? (Select all that apply.) a. Vitamin A 14. Which personal lifestyle choices will likely have a positive impact on reducing an individual’s risk for developing cancer? (Select all that apply.) a. Avoiding crowds 15. Which individual is at risk for developing lung and respiratory tract cancers because of exposure to known cancer-inducing environmental factors? (Select all that apply.) a. A patient whose partner smokes 1 1/2 packs of cigarettes a day 16. Which primary prevention strategy has a substantial likelihood of reducing the risk of developing cancer? (Select all that apply.) a. Offering free smoking cessation classes to college students 17. When considering topics for a series of community discussions related to cancer prevention strategies, the nurse will include: (Select all that apply.) a. Healthy eating NURSINGTB.COM Chapter 14: Cancer in Children MULTIPLE CHOICE 1. What congenital malformation is commonly linked to acute leukemia in children? 2. When are childhood cancers most often diagnosed? NURSINGTB.COM 3. Prenatal exposure to diethylstilbestrol (DES) can result in which type of cancer? 4. Currently, what percentage of children with cancer can be cured? 5. Most childhood cancers arise from the: 6. Which form of cancer is linked to congenital malformation syndromes? 7. Research data support a carcinogenic relationship in children resulting from exposure to which virus? 8. A child diagnosed with acquired immunodeficiency syndrome (AIDS) has an increased risk of developing: 9. Which intervention has the greatest affect on a child’s mortality rate when diagnosed with cancer? 10. Which statement is likely true regarding children being treated for cancer with radiation therapy? 11. How should the nurse reply when a parent questions why a computed tomographic (CT) scan of the head was not ordered for their 5-year-old child after a minor fall? MULTIPLE RESPONSE 12. Childhood exposure to which risk factors increases the susceptibility for developing cancers? (Select all that apply.) 13. Which statement is true concerning the difference between adult and childhood cancers? (Select all that apply.) 14. Most childhood cancers originate from the mesodermal germ layer that ultimately produces which of the following? (Select all that apply.) a. Connective tissue 15. Which statements are true regarding cancers that develop in children? (Select all that apply.) 16. The nurse is preparing a discussion on cancer and its occurrence among college-aged students. Which cancers will the nurse include in the discussion? (Select all that apply.) a. Colorectal Chapter 15: Structure and Function of the Neurologic System MULTIPLE CHOICE 1. Which pathway carries sensory information toward the central nervous system (CNS)? 2. Which type of axon transmits a nerve impulse at the highest rate? 3. Which nerves are capable of regeneration? 4. The neurotransmitter, norepinephrine, is secreted in the: 5. Both oligodendroglia and Schwann cells share the ability to: 6. During a synapse, what change occurs after the neurotransmitter binds to the receptor? 7. What name is given to a large network of neurons within the brainstem that is essential for maintaining wakefulness? 8. Thought and goal-oriented behaviors are functions of which area of the brain? 9. The region responsible for the motor aspects of speech is located in the: Broca speech area is the only region responsible for the motor aspects of speech. 10. Parkinson and Huntington diseases are associated with defects in which area of the brain? 11. Maintenance of a constant internal environment and the implementation of behavioral patterns are main functions of which area of the brain? 12. The ability of the eyes to track moving objects through a visual field is primarily a function of which colliculi? NURSINGTB.COM 13. What parts of the brain mediate the expression of affect, both emotional and behavioral states? 14. Reflex activities concerned with heart rate, blood pressure, respirations, sneezing, swallowing, and coughing are controlled by which area of the brain? 15. From which part of the midbrain do cranial nerves V to VIII emerge? 16. From which part of the midbrain do cranial nerves IX to XII emerge? 17. for conscious and unconscious muscle synergy and for maintaining balance and posture? 18. Which statement is true regarding upper motor neurons? 19. The membrane that separates the brain’s cerebellum from its cerebrum is the: 20. The function of arachnoid villi is to: 21. Where is the cerebrospinal fluid pNroUdRuScIeNdG?TB.COM 22. Which of the meninges closely adheres to the surface of the brain and spinal cord and follows the sulci and fissures? 23. Norepinephrine produces what primary response? 24. What is an effect of the sympathetic nervous system? 25. The brain receives approximately what percentage of the cardiac output? 26. The collateral blood flow to the brain is provided by the: 27. The nurse recognizes that a patient’s diagnosis of a viral infection of the brain’s meningeal layer is supported by which diagnostic laboratory result? MULTIPLE RESPONSE 28. Which cranial nerves contain parasympathetic nerves? (Select all that apply.) 29. The sympathetic nervous system primarily serves to protect an individual by doing which of the following? (Select all that apply.) NURSINGTB.COM 30. The aging process brings about what changes to human cells? (Select all that apply.) 31. Which statement is true regarding the blood-brain barrier (BBB)? (Select all that apply.) 32. A nurse caring for an older adult patient would expect which functional changes to occur? 33. What evidence does the nurse expect to see when a patient experiences trauma to the hypothalamus? (Select all that apply.) 34. A Schwann cell: (Select all that apply.) a. Can form the myelin sheath. b. Is also referred to as a neurolemmocyte. MATCHING Match the function with the appropriate cranial nerve. A. Fibers emerge from the posterior midbrain and exit from the skull to run to the eye. B. Provides motor and sensory functions to the face, mouth, nose, and eyes. C. Fibers emerge from the midbrain, exit from the skull, and extend to the eye. D. Controls motor functions to the pharynx and salivary glands and sensory functions from the pharynx and tongue. E. Innervates muscles that move the eye laterally. F. Affects control over the motor fibers to the muscles of tongue and sensory impulses from the tongue to the brain. G. Is purely sensory and carries impulses for the sense of smell. H. Is made up of parasympathetic motor fibers that supply the smooth muscles of the abdominal oNrgUaRnSsI.NGTB.COM I. Transmits impulses for the sense of hearing. J. Carries sensory and motor fibers to the pharynx and larynx. 35. Glossopharyngeal nerve 36. Oculomotor nerve 37. Trochlear nerve 38. Abducens nerve 39. Trigeminal nerve 40. Hypoglossal nerve 41. Vagus nerve 42. Spinal accessory nerve 43. Olfactory nerve 44. Vestibulocochlear nerve Chapter 16: Pain, Temperature Regulation, Sleep, and Sensory Function MULTIPLE CHOICE 1. Pricking one’s finger with a needle would cause minimal pain, whereas experiencing abdominal surgery would produce more pain. This distinction is an example of which pain theory? 2. Which pain theory proposes that a balance of impulses conducted from the spinal cord to the higher centers in the central nervous system (CNS) modulates the transmission of pain? 3. Which type of nerve fibers transmits pain impulses? 4. Where are the primary-order pain transmitting neurons located within the spinal cord? 5. The gate in the GCT of pain is located in the: 6. Which spinal tract carries the most nociceptive information? 7. The major relay station of sensory information is located in the: 8. Where in the CNS does a person’s learned pain response occur? 9. Massage therapy relieves pain by closing the pain gate with the stimulation which fibers? 10. What part of the brain provides the emotional response to pain? 11. Which neurotransmitters inhibit pain in the medulla and pons? a. Norepinephrine and serotonin 12. Which endogenous opioid is located in the hypothalamus and pituitary and is a strong -receptor agonist? 13. What is the term that denotes the duration of time or the intensity of pain that a person will endure before outwardly responding? 14. Pain that warns of actual or impending tissue injury is referred to as what? 15. Which description characterizes visceral pain? 16. When caring for a person who has experienced pain for 3 days, anxiety is likely to produce which physical signs that a nurse would expect to find? PTS: 1 REF: Pages 491-492 17. Enkephalins and endorphins act to relieve pain by which process? 18. What is a long-term complication of rewarming as a treatment for hypothermia? 19. How does the release (increase) of epinephrine raise body temperature? 20. Using a fan to reduce body temperature is an example of which mechanism of heat loss? 21. Up to how many liters of fluid per hour may be lost by sweating? 22. Heat loss from the body via radiation occurs by: 23. Which cytokines are endogenous pyrogens? 24. Which hormones help diminish the febrile response? 25. Prolonged high environmental temperatures that produce dehydration, decreased plasma volumes, hypotension, decreased cardiac output, and tachycardia cause which disorder of temperature regulation? 26. In acute hypothermia, what physiologic change shunts blood away from the colder skin to the body core in an effort to decrease heat loss? Tissue hypothermia slows the rate of chemical reactions (tissue metabolism), increases the viscosity of the blood, slows blood flow through microcirculation, facilitates blood coagulation, and stimulates profound vasoconstriction. The remaining options do not fulfill this objective. 27. A heat stroke is characterized by: 28. Which medication is used to reverse the effects of malignant hyperthermia? 29. The major sleep center is located in which section of the brain? 30. Which neuropeptide promotes wakefulness? 31. Which term is also used to refer to paradoxic sleep? 32. The sudden apparent arousal in which a child expresses intense fear or another strong emotion while still in a sleep state characterizes which sleep disorder? 33. Coronary artery disease is most affected by which component of sleep? 34. Rapid eye movement (REM) sleep occurs in cycles approximately every: 35. Loud snoring, a decrease in oxygen saturation, fragmented sleep, chronic daytime sleepiness, and fatigue are clinical manifestations of which sleep disorder? 36. What are the expected changes in sleep patterns of older adults? a. Older adults experience difficulty falling asleep with less time spent in REM sleep. 37. Pinkeye is characterized by inflammation of which structure? 38. Open-angle glaucoma occurs because of: 39. How can glaucoma cause blindness? 40. When comparing the effects of acute and chronic pain on an individual, chronic pain is more often: 41. When considering the risk factors for the development of phantom limb pain, the nurse recognizes which as a primary contributing factor? 42. Based on an understanding of the physiologic process of nociceptors, the nurse expects which surgical procedure to create more pain? 43. The basis of the specificity theory of pain is that: 44. Which statement is true regarding the gate control theory (GCT) of pain? MULTIPLE RESPONSE 45. Which factors contribute to sensorineural hearing loss? (Select all that apply.) a. Ménière disease 46. Why are children more susceptible to heat stroke than are adults? (Select all that apply.) a. Children produce more metabolic heat when exercising. 47. Heat exhaustion results in: (Select all that apply.) 48. It is true that a fever: (Select all that apply.) MATCHING Match the types of chronic pain with its description. Types of pain may be used more than once. A. Myofascial pain syndrome B. Neuropathic pain C. Deafferentation pain D. Sympathetically maintained pain 49. Pain that results from tumor infiltration of nerve tissue, from trauma or chemical injury to the nerve, or from damage from radiation, chemotherapy, or surgical sectioning of the nerve 50. Pain that is thought to be caused by trauma or disease of nerves and leads to abnormal processing of sensory information by the peripheral and central nervous systems 51. Pain that occurs after peripheral nerve injury and is described as continuous with severe sensations and a burning quality 52. Pain that is the result of muscle spasms, tenderness, and stiffness and leads to muscle guarding that limits muscle motion NURSINGTB.COM Chapter 17: Alterations in Cognitive Systems, Cerebral Hemodynamics, and Motor Function MULTIPLE CHOICE 1. Cognitive operations cannot occur without the effective functioning of the brain’s: 2. Which intracerebral disease process is capable of producing diffuse dysfunction? empyema (accumulation of pus), can cause similar dysfunction. 3. What is the most common infratentorial brain disease process that results in the direct destruction of the reticulating activation system (RAS)? 4. What stimulus causes posthyperventilation apnea (PHVA)? 5. Posthyperventilation apnea (PHVA) ceases and rhythmic breathing is resumed when levels of arterial: 6. Cheyne-Stokes respirations are described as a: 7. Vomiting is associated with central nervous system (CNS) injuries that compress which of the brain’s anatomic locations? 8. Which midbrain dysfunction causes pupils to be pinpoint size and fixed in position? 9. What characteristic is a medical criterion of brain death? 10. A clinical manifestation caused by damage to the lower pons includes an abnormal: 11. Which person is at the greatest risk for developing delirium? 12. A sudden, explosive, disorderly discharge of cerebral neurons is termed: 13. A complex partial seizure is described as: 14. Status epilepticus is considered a medical emergency because of the: 15. The most critical aspect in correctNlyUdRiSaIgNnGoTsBin.CgOaMseizure disorder and establishing its cause is: 16. What type of seizure starts in the fingers and progressively spreads up the arm and extends to the leg? 17. What area of the brain mediates the executive attention functions? 18. What term describes the loss of the comprehension or production of language? 19. With receptive dysphasia (fluent), the individual is able to: 20. What is the normal intracranial pressure (in mm Hg)? 21. Cerebral edema is an increase in the fluid content of the brain’s: 22. What type of cerebral edema occurs when permeability of the capillary endothelium increases after injury to the vascular structure? 23. A communicating hydrocephalus is caused by an impairment of the: 24. Which edema is most often observed with noncommunicating hydrocephalus? 25. Which dyskinesia involves involuntary movements of the face, trunk, and extremities? 26. Antipsychotic drugs cause tardive dyskinesia by mimicking the effects of increased: 27. The existence of regular, deep, and rapid respirations after a severe closed head injury is indicative of neurologic injury to the: 28. What type of posturing exists when a person with a severe closed head injury has all four extremities in rigid extension with the forearms in hyperpronation and the legs in plantar extension? 29. Since his cerebrovascular accident, a man has been denying his left hemiplegia. What term is used to describe this finding? 30. After a cerebrovascular accident, a man is unable to either feel or identify a comb with his eyes closed. This is an example of: 31. Most dysphasias are associated with cerebrovascular accidents involving which artery? 32. Tactile agnosia is related to injury of which area of the brain? 33. Neurofibrillary tangles characterize which neurologic disorder? 34. The body compensates for a rise in intracranial pressure by first displacing the: 35. Stage 1 intracranial hypertension is caused by the: 36. Dilated and sluggish pupils, widening pulse pressure, and bradycardia are clinical findings evident of which stage of intracranial hypertension? 37. Dilation of the ipsilateral pupil, following uncal herniation, is the result of pressure on which cranial nerve (CN)? 38. Which characteristic is the most critical index of nervous system dysfunction? 39. Diagnostic criteria for a persistent vegetative state include: 40. Uncal herniation occurs when: 41. Which assessment finding marks the end of spinal shock? 42. Characteristics of primary motor neuron atrophy include: 43. The weakness resulting from the segmental paresis and paralysis characteristic of anterior horn cell injury is difficult to recognize because: 44. Parkinson disease is a degenerative disorder of the brain’s: 45. Clinical manifestations of Parkinson disease are caused by a deficit in which of the brain’s neurotransmitters? 46. Tremors at rest, rigidity, akinesia, and postural abnormalities are a result of the atrophy of neurons in the brain’s: MULTIPLE RESPONSE 47. Dementia is commonly characterized by the deterioration in which abilities? (Select all that apply.) a. Sociability 48. The clinical manifestations of Parkinson disease include: (Select all that apply.) a. Fragmented sleep 49. In Parkinson disease the basal ganglia influence the hypothalamic function to produce which clinical manifestations? (Select all that apply.) a. Inappropriate diaphoresis Chapter 18: Disorders of the Central and Peripheral Nervous Systems and the Neuromuscular Junction MULTIPLE CHOICE 1. Diffuse axonal injuries (DAIs) of the brain often result in: 2. What event is most likely to occur to the brain in a classic cerebral concussion? 3. Which disorder has clinical manifestations that include decreased consciousness for up to 4. What group is most at risk of spinal cord injury from minor trauma? 5. The edema of the upper cervical cord after spinal cord injury is considered life threatening because of which possible outcome? 6. What indicates that spinal shock is terminating? 7. What term is used to describe the complication that can result from a spinal cord injury above T6 that is producing paroxysmal hypertension, as well as piloerection and sweating above the spinal cord lesion? 8. Why does a person who has a spinal cord injury experience faulty control of sweating? 9. Autonomic hyperreflexia–induced bradycardia is a result of stimulation of the: 10. A herniation of which disk will likely result in motor and sensory changes of the lateral lower legs and soles of the feet? 11. Which condition poses the highest risk for a cerebrovascular accident (CVA)? 12. A right hemisphere embolic CVA has resulted in left-sided paralysis and reduced sensation of the left foot and leg. Which cerebral artery is most likely affected by the emboli? 13. Atrial fibrillation, rheumatic heart disease, and valvular prosthetics are risk factors for which type of stroke? NURSINGTB.COM 14. Microinfarcts resulting in pure motor or pure sensory deficits are the result of which type of stroke? 15. Which vascular malformation is characterized by arteries that feed directly into veins through vascular tangles of abnormal vessels? 16. Which clinical finding is considered a diagnostic indicator for an arteriovenous malformation (AVM)? 17. Which cerebral vascular hemorrhage causes meningeal irritation, photophobia, and positive Kernig and Brudzinski signs? 18. In adults, most intracranial tumors are located: 19. In children, most intracranial tumors are located: 20. The most common primary central nervous system (CNS) tumor is the: 21. Meningiomas characteristically compress from: 22. What is the central component of the pathogenic model of multiple sclerosis? 23. A blunt force injury to the forehead would result in a coup injury to which region of the brain? 24. A blunt force injury to the forehead would result in a contrecoup injury to which region of the brain? 25. Spinal cord injuries most likely occur in which region? 26. The most likely rationale for body temperature fluctuations after cervical spinal cord injury is that the person has: 27. A man who sustained a cervical spinal cord injury 2 days ago suddenly develops severe hypertension and bradycardia. He reports severe head pain and blurred vision. The most likely explanation for these clinical manifestations is that he is: 28. The type of vascular malformation that most often results in hemorrhage is: 29. Atheromatous plaques are most commonly found: 30. Multiple sclerosis is best described as a(an): 31. What is the most common opportunistic infection associated with acquired immunodeficiency syndrome (AIDS)? 32. It is true that Guillain-Barré syndrome (GBS): 33. It is true that myasthenia gravis: 34. In which disorder are acetylcholine receptor antibodies (IgG antibodies) produced against acetylcholine receptors? 35. Multiple sclerosis and Guillain-Barré syndrome are similar in that they both: MULTIPLE RESPONSE 36. Which clinical manifestation is characteristic of cluster headaches? (Select all that apply.) 37. What are the initial clinical manifestations immediately noted after a spinal cord injury? (Select all that apply.) MATCHING Match the terms with the corresponding descriptions. A. Complication of mastoiditis B. Opportunistic infection C. CNS manifestation of tuberculosis D. Mosquito-borne viral infection E. Tick-borne bacterial infection 38. Meningitis 39. Encephalitis 40. Cryptococcus neoformans NURSINGTB.COM Chapter 19: Neurobiology of Schizophrenia, Mood Disorders, and Anxiety Disorders MULTIPLE CHOICE 1. Which would be considered a positive symptom of schizophrenia? 2. The onset of schizophrenia can be triggered by which prenatal occurrence? 3. Which neurotransmitter is reduced in people with schizophrenia? 4. Alterations in which part of the brain are linked to hallucinations, delusions, and thought disorders associated with schizophrenia? Only temporal lobe alterations may be responsible for the production of positive schizophrenic symptoms, such as hallucinations, delusions, thought disorders, and bizarre behavior. 5. Antipsychotic drugs block which neurotransmitter receptor? 6. What data confer the link between bipolar disorders and schizophrenia? 7. Hypothalamic-pituitary-adrenal (HPA) system abnormalities exist in a large percentage of individuals with: 8. The common property among the three types of medications used to treat depression is that they: 9. The link between major depression and cortisol secretion is that individuals with depression: 10. A decrease in receptor binding for which neurotransmitter is found in individuals with depression? 11. When treating individuals with depression, the result produced by electroconvulsive therapy (ECT) is believed to be an alteration in: 12. Which electrolyte imbalance contributes to lithium toxicity? 13. Which neurotransmitter is inhibited in panic disorders? 14. anxiety disorder (GAD) is a period of excessive worrying that lasts for at least how many months? 15. Individuals who eat aged cheese and avocado when taking monoamine oxidase inhibitors (MAOIs) may experience: 16. Electroconvulsive therapy (ECT) is used to treat depression: 17. A notable complication of panic disorder is: 18. Persistent symptoms of posttraumatic stress disorder (PTSD) include: 19. Hallucinations, delusions, and thought disorders occur with alterations to which part of the brain? MULTIPLE RESPONSE 20. Significant numbers of individuals with depression have problems related to: (Select all that apply.) 21. Which neurotransmitter is inhibited in generalized anxiety disorder (GAD)? (Select all that apply.) a. Acetylcholine 22. What are the most common side effects of selective serotonin reuptake inhibitors (SSRIs)? (Select all that apply.) MATCHING Match the terms with the corresponding descriptions. A. Delusions B. Formal thought disorder C. Anhedonia D. Hallucinations E. Alogia F. Avolition 23. Perceptions are experienced without external stimulation of the sense organs. 24. Persistent beliefs are contrary to the educational and cultural background of the individual. 25. Fluent speech is difficult to comprehend. 26. Spontaneous speech is absent. 27. Condition is characterized by an inability to have emotional experiences. 28. Condition is characterized by a deficit in spontaneous or goal-directed activities. Chapter 20: Alterations of Neurologic Function in Children MULTIPLE CHOICE 1. The neural groove closes dorsally during which week of gestational life? a. Second c. Eighth b. Fourth d. Twelfth 2. Which nutritional deficiency in a pregnant woman is associated with neural tube defect (NTD)? 3. Which defect of neural tube closure is most common? 4. What is the anomaly in which the soft bony component of the skull and much of the brain is missing? 5. The most common cause of obstructive hydrocephalus in infants is: 6. What is the term for a herniation or protrusion of brain and meninges through a defect in the skull? 7. What is the result of a Chiari type II malformation associated with a myelomeningocele? 8. Prompt surgical repair of a myelomeningocele is critical to best prevent: 9. Which body system is the largest site for human immunodeficiency virus (HIV) infection in infants and children? 10. An infant diagnosed with hydrocephalus is observed to demonstrate: 11. Gait disturbances and instability are characteristic of which form of cerebral palsy? 12. Children with phenylketonuria (PKU) are unable to synthesize: 13. Benign febrile seizures are characterized by: 14. What is the most common general symptom of a localized childhood brain tumor? 15. The tonic neck reflex observed in a newborn should no longer be obtainable by: 16. What term is used to describe a hernial protrusion of a saclike cyst that contains meninges, spinal fluid, and a portion of the spinal cord through a defect in a posterior arch of a vertebra? 17. What test is performed on amniotic fluid and maternal blood to test for neural tube defect? 18. The clinical manifestations of dyskinetic cerebral palsy include: MULTIPLE RESPONSE 19. Which musculoskeletal deformities are associated with myelomeningocele? (Select all that apply.) 20. True microcephaly can be caused by: (Select all that apply.) 21. Which statements regarding the term myelodysplasia are true? (Select all that apply.) MATCHING Match the tumor name with its site of development. A. Medulloblastoma B. Ependymoma C. Cerebellar astrocytNomURaSINGTB.COM D. Craniopharyngioma E. Neuroblastoma 22. Originates in the neural crest that normally forms the sympathetic ganglia and adrenal medulla. 23. Develops in the fourth ventricle. 24. Develops in the vermis of the cerebellum and may extend to the fourth ventricle. 25. Originates from the pituitary or hypothalamus. 26. Causes unilateral symptoms such as nystagmus. NURSINGTB.COM Chapter 21: Mechanisms of Hormonal Regulation MULTIPLE CHOICE 1. What imbalance lessens the rate of secretion of parathyroid hormone (PTH)? 2. Regulation of the release of catecholamines from the adrenal medulla is an example of which type of regulation? 3. How does a faulty negative-feedback mechanism result in a hormonal imbalance? 4. Which substance is a water-soluble protein hormone? Peptide or protein hormones, such as insulin, pituitary, hypothalamic, and parathyroid, are water soluble and circulate in free (unbound) forms. All the remaining options are fat-soluble hormones. 5. Which of the following is a lipid-soluble hormone? 6. Most protein hormones are transported in the bloodstream and are: .COM 7. When insulin binds its receptors on muscle cells, an increase in glucose uptake by the muscle cells is the result. This is an example of what type of effect by a hormone? 8. Thyroid-stimulating hormone (TSH) is released to stimulate thyroid hormone (TH) and is inhibited when plasma levels of TH are adequate. This is an example of: 9. Lipid-soluble hormone receptors are located: 10. Which second messenger is stimulated by epinephrine binding to a -adrenergic receptor? 11. Which hormone does the second messenger calcium (Ca++) bind to activate phospholipase C through a G protein? 12. The control of calcium in cells is important because it: 13. The portion of the pituitary that secretes oxytocin is: 14. Antidiuretic hormone acts to cause vasoconstriction when: 15. What is the target tissue for prolactin-releasing factor? 16. Where is antidiuretic hormone (ADH) synthesized, and where does it act? 17. Where is oxytocin synthesized? 18. The releasing hormones that are made in the hypothalamus travel to the anterior pituitary via the: 19. Which mineral is needed for thyroid-stimulating hormone (TSH) to stimulate the secretion of thyroid hormone (TH)? 20. Which hormone triggers uterine contractions? 21. What effect does hyperphosphatemia have on other electrolytes? 22. Insulin transports which electrolyte in the cell? 23. A person who has experienced physiologic stresses will have increased levels of which hormone? 24. What is the action of calcitonin? 25. Which hormone is involved in the regulation of serum calcium levels? 26. Which hormone inhibits the secretion of growth hormone (GH)? 27. Target cells for parathyroid hormone are located in the: 28. Which compound or hormone is secreted by the adrenal medulla? 29. The secretion of adrenocorticotropic-stimulating hormone (ACTH) will result in the increased level of which hormone? 30. Which human physiologic system is believed to be an integral factor in unhealthy aging? 31. What are the effects of aging on pancreatic cells? 32. Aldosterone directly increases the reabsorption of: 33. Which is an expected hormonal change in an older patient? MULTIPLE RESPONSE 34. What are actions of glucocorticoids? (Select all that apply.) MATCHING Match the anatomic structure with its hormone. Names of structures may be used more than once. A. Anterior pituitary B. Posterior pituitary C. Thyroid D. Adrenal cortex E. Adrenal medulla 35. Calcitonin 36. Cortisol 37. Oxytocin 38. Glycoproteins 39. Epinephrine Chapter 22: Alterations of Hormonal Regulation MULTIPLE CHOICE 1. The effects of the syndrome of inappropriate antidiuretic hormone (SIADH) secretion include solute: 2. The common cause of elevated levels of antidiuretic hormone (ADH) secretion is: 3. Which laboratory value would the nurse expect to find if a person is experiencing syndrome of inappropriate antidiuNreUtRicShINoGrmTBo.nCeO(MSIADH)? 4. Diabetes insipidus is a result of: 5. A patient who is diagnosed with a closed head injury has a urine output of 6 to 8 L/day. Electrolytes are within normal limits, but his antidiuretic hormone (ADH) level is low. Although he has had no intake for 4 hours, no change in his polyuria level has occurred. These symptoms support a diagnosis of: 6. Diabetes insipidus, diabetes mellitus, and syndrome of inappropriate antidiuretic hormone all exhibit which symptom? 7. The cause of neurogenic diabetes insipidus (DI) is related to an organic lesion of the: 8. Which form of diabetic insipidus (DI) will result if the target cells for antidiuretic hormone (ADH) in the renal collecting tubules demonstrate insensitivity? 9. Which laboratory value is consistently low in a patient with diabetes insipidus (DI)? 10. Which form of diabetes insipidus (DI) is treatable with exogenous antidiuretic hormone (ADH)? 11. Which condition may result from pressure exerted by a pituitary tumor? 12. The term used to describe a person who experiences a lack of all hormones associated with the anterior pituitary is: 13. Visual disturbances are a result of a pituitary adenoma because of the: 14. Which disorder is considered a co-morbid condition of acromegaly? 15. Which disorder is caused by hypersecretion of the growth hormone (GH) in adults? 16. Giantism occurs only in children and adolescents because their: 17. Amenorrhea, galactorrhea, hirsutism, and osteoporosis are each caused by a: 18. Graves disease develops from a(n): 19. The signs of thyrotoxic crisis include: 20. Pathologic changes associated with Graves disease include: 21. The level of thyroid-stimulating hormone (TSH) in individuals with Graves disease is usually: 22. Palpation of the neck of a person diagnosed with Graves disease would detect a thyroid that is: 23. A deficiency of which chemical may result in hypothyroidism? 24. What are clinical manifestations of hypothyroidism? 25. Diagnosing a thyroid carcinoma is best performed with: 26. Renal failure is the most common cause of which type of hyperparathyroidism? 27. The most common cause of hypoparathyroidism is: 28. The most probable cause of low serum calcium after a thyroidectomy is: 29. A patient diagnosed with diabetic ketoacidosis (DKA) has the following laboratory values: arterial pH 7.20; serum glucose 500 mg/dl; positive urine glucose and ketones; serum potassium (K+) 2 mEq/L; serum sodium (Na+) 130 mEq/L. The patient reports that he has been sick with the “flu” for 1 week. What relationship do these values have to his insulin deficiency? 30. Polyuria occurs with diabetes mellitus because of the: 31. Type 2 diabetes mellitus is best described as a(an): 32. A person diagnosed with type 1 diabetes experiences hunger, lightheadedness, tachycardia, pallor, headache, and confusion. The most probable cause of these symptoms is: 33. Which serum glucose level would indicate hypoglycemia in a newborn? 34. When comparing the clinical manifestations of both diabetic ketoacidosis (DKA) and hyperglycemic hyperosmolar nonketotic syndrome (HHNKS), which condition is associated with only DKA? 35. Hypoglycemia, followed by rebound hyperglycemia, is observed in those with: 36. The first laboratory test that indicates type 1 diabetes is causing the development of diabetic nephropathy is: 37. Which classification of oral hypoglycemic drugs decreases hepatic glucose production and increases insulin sensitivity and peripheral glucose uptake? 38. What causes the microvascular complications in patients with diabetes mellitus? 39. Retinopathy develops in patients with diabetes mellitus because: 40. A person has acne, easy bruising, thin extremities, and truncal obesity. These clinical manifestations are indicative of which endocrine disorder? MULTIPLE RESPONSE 41. A person may experience which complications as a result of a reduction in parathyroid hormone (PTH)? (Select all that apply.) 42. A chronic complication of diabetes mellitus is likely to result in microvascular complications in which areas? (Select all that apply.) MATCHING Match the phrases with the corresponding terms. A. Acromegaly B. Cushing disease C. Addison disease D. Graves disease E. Myxedema F. Pheochromocytoma 43. Hypersecretion of thyroid hormone (TH) 44. Hypersecretion of adrenocorticotropic hormone (ACTH) 45. Hypersecretion of adrenal medulla hormones 46. Hyposecretion of thyroid hormone (TH) 47. Hyposecretion of adrenal cortex hormones 48. Hypersecretion of growth hormone (GH) Chapter 23: Obesity and Disorders of Nutrition MULTIPLE CHOICE 1. If a patient with multiple sclerosis starts coughing frequently during meals and starts to eat significantly less food than normal, the patient may have 2. For a patient with dysphagia, the food that would be most difficult to swallow is NURSINGTB.COM Patients with dysphagia often have difficulty swallowing thin liquids, such as chicken noodle soup. Thicker, pureed foods such as applesauce, mashed potatoes, and chocolate pudding are usually easier to swallow. 3. If a patient has difficulty swallowing, the best position for eating is 4. The most acute risk for patients with dysphagia is 5. The most helpful recommendation for a client who often experiences heartburn at night would be to 6. An example of a meal that is likely to relax the lower esophageal sphincter and allow gastroesophageal reflux is 7. Peptic ulcer disease (PUD) would be most like to occur in someone who uses medica- tion to treat 8. Nutrition therapy for peptic ulcers should be individualized, depending on 9. If a patient who has undergone NgUasRtrSiIcNbGyTpBa.CssOsMurgery for treatment of extreme obesity experiences sudden sweating, nausea, and stomach cramps after meals, the patient may have 10. An appropriate meal for someone with dumping syndrome would be 11. If a patient has esophagitis and also has worn tooth enamel, he or she may have 12. An example of a meal that may contain gluten is . 13. A patient with lactose intolerance would be most likely to experience symptoms if he or she ate a 14. Milk may be made suitable for patients with lactose intolerance by treating it with tab- lets that contain 15. For patients with inflammatory bowel disease, nutrition therapy is 16. Because patients with active Crohns disease have intestinal inflammation, they benefit from high intake of 17. Patients with inflammatory bowel disease may benefit from a high-fiber diet during 18. Fluid loss is most likely to be a problem for a patient with 19. The most significant nutritional concern for a patient with an ileostomy is 20. For patients with ostomies, a lower amount of output occurs 21. If a patient has had a large portion of their small intestine removed because of cancer and is unable to maintain a stable weight, a feeding regimen that would be most appropri- ate is 22. If a patient receiving chemotherapy is struggling with nausea and vomiting, helpful suggestions may include 23. The best way to prevent formation of diverticula in the colon is to 24. Someone who may benefit from avoiding sugar-free chewing gum is a patient with 25. In consuming a high-fiber diet, it is important to also consume adequate amounts of 26. If a client complains of excessive gas, a good question to ask is whether he or she 27. An example of a daily change that may help decrease constipation is 28. An example of a high-fiber food item to include with lunch is . 29. A possible cause of acute diarrhea is 30. Treatment of diarrhea generally begins with NURSINGTB.COM Chapter 24: Structure and Function of the Reproductive Systems MULTIPLE CHOICE 1. The initial reproductive structures of the male and female embryos appear the same until which week of gestation? 2. The absence of which major hormone is a determinant of sexual differentiation (wolffian system) in utero? 3. Which gland produces the associated hormones that are found in high levels in a female fetus? 4. Which hormone is linked to an increase in appetite during puberty? 5. The Skene glands are located on either side of which structure? 6. What is the function of the mucus secreted by the Bartholin glands? 7. Which change is a result of puberty and defends the vagina from infection? 8. What happens to the vagina’s lining at puberty? 9. Which structure is lined with columnar epithelial cells? 10. Where is the usual site of fertilization of an ovum? 11. Where is the usual site of cervical dysplasia or cancer in situ? 12. Having ejected a mature ovum, the ovarian follicle develops into a(n): 13. The mucosal secretions of the cervix secrete which immunoglobulin? 14. The equivalent to the female gonad is the male: 15. A surge of which hormone causes the corpus luteum to produce progesterone? 16. What directly causes ovulation duNriUnRgStIhNeGmTBen.CsOtrMual cycle? 17. Which anatomic structure secretes follicle stimulating hormone (FSH) and luteinizing hormone (LH)? 18. During the time that ovulation occurs, which statement concerning basal body temperature (BBT) is true? 19. What structure in the male lies posterior to the urinary bladder? 20. When do penile erections begin? 21. Which statement is true regarding the major difference between male and female sex hormone production? 22. Where in the male body does spermatogenesis occur? a. Epididymis c. Seminiferous tubules b. Rete testes d. Vas deferens 23. Which immunoglobulin is contained in breast milk? 24. Which hormone promotes the development of the lobular ducts in the breasts? 25. What causes the vasomotor flushes (hot flashes) that are associated with declining ovarian function with age? 26. When does the male body begin to produce sperm? 27. The human zygote has a total of how many chromosomes? 28. Which hormone promotes the development of testosterone in both males and females? 29. Which hormone stimulates gonads to produce both male and female hormones? 30. Which hormone relaxes the myometrium and prevents lactation until the fetus is born? 31. A Sims-Huhner test is of particular interest to a patient experiencing which condition? MULTIPLE RESPONSE 32. Estrogen has many biological effects on the female body including: (Select all that apply.) 33. Which statements about the human papillolmavirus (HPV) and vaccine are true? (Select all that apply.) 34. Which statements are true regarding the female menstrual cycle? (Select all that apply.) 35. Testosterone is believed to have a role in: (Select all that apply.) 36. What are normal characteristics of aging of the male reproductive system? (Select all that apply.) Chapter 25: Alterations of the Female Reproductive System MULTIPLE CHOICE 1. In 95% of children of delayed puberty, the problem is caused by: 2. What is the first sign of puberty in girls? 3. Which type of precocious pubertyNcUaRuSseINs GthTeBc.ChOilMd to develop some secondary sex characteristics of the opposite sex? 4. The release of which chemical mediator causes primary dysmenorrhea? 5. Considering the pathophysiologic characteristics of primary amenorrhea, what anatomic structure is involved in compartment II? 6. Considering the pathophysiologic characteristics of primary amenorrhea, what anatomic structure is involved in compartment IV? 7. Which condition is considered a clinical cause of amenorrhea? 8. Clinical manifestations that include irregular or heavy bleeding, the passage of large clots, and the depletion of iron stores support which diagnosis? 9. What statement concerning the pathogenetic mechanisms of polycystic ovarian syndrome 10. What is the leading cause of infertility in women? 11. Considering the mediating factors of premenstrual syndrome (PMS), which medication may be used either continually or only during the menstrual period as a treatment for the condition? 12. Which statement regarding pelvic inflammatory disease (PID) is true? 13. When a woman’s uterus is assessed as protruding through the entrance of the vagina to the hymen, which grade of prolapse does this indicate? 14. Which term is used to identify the descent of the posterior bladder and trigone into the vaginal canal? 15. What type of cyst develops when an ovarian follicle is stimulated but no dominant follicle develops and completes the maturity process? 16. Which term is used to identify benign uterine tumors that develop from smooth muscle cells in the myometrium and are commonly called uterine fibroids? 17. What theory is used to describe the cause of endometriosis? 18. Which virus is a precursor for developing cervical intraepithelial neoplasia (CIN) and cervical cancer? 19. Which description is used when a progressive neoplastic change involves the full epithelial thickness of the cervix? 20. Which factor increases the risk for ovarian cancer after the age of 40 years? 21. Infertility is defined as the inability to conceive after how many months of unprotected intercourse with the same partner? 22. Which of the following is not considered a cause of galactorrhea? 23. Fluid-filled squishy sacs characterize which breast disorder? 24. What are typical findings on breast palpation of a woman diagnosed with simple fibroadenoma? 25. Which benign breast tumor affects postmenopausal women and is characterized by the principal lactiferous ducts becoming dilated and filled with cellular debris? 26. The majority of the small percentage of ovarian cancers that are associated with a known pattern of inheritance are associated with: 27. What is usually the first clinical manifestation of breast cancer? MULTIPLE RESPONSE 28. What is a recognized treatment for the symptoms often associated with pelvic organ prolapse? (Select all that apply.) a. Pessary 29. Dysfunctional uterine bleeding (DUB), secondary to ovarian dysfunction, is abnormal uterine bleeding resulting from: (Select all that apply.) 30. The size of benign uterine tumors, such as leiomyomas, is thought to be caused by the influence of which hormone? (Select all that apply.) 31. What are the common clinical manifestations of endometriosis? (Select all that apply.) NURSINGTB.COM Chapter 26: Alterations of the Male Reproductive System MULTIPLE CHOICE 1. In the 95% of those with delayed puberty, the problem is caused by which condition? a. Disruption in the hypothalamus c. Deficit in estrogen or testosterone b. Disruption of the pituitary d. Physiologic hormonal delays In 95% of cases, delayed puberty is a physiologic delay; that is, hormonal levels are normal and the hypothalamic-pituitary-gonadal (HPG) axis is intact, but maturation is happening slowly. This selection is the only option that accurately describes 95% of those with delayed puberty. PTS: 1 REF: Page 886 2. What is the first sign of puberty in boys? a. Thickening of the scrotal skin c. Enlargement of the testes b. Growth of pubic hair d. Change in voice The first sign of puberty in boys is an enlargement of the testes and a thinning of the scrotal skin. PTS: 1 REF: Page 886 3. Which type of precocious pubertyNcUaRuSseINs GthTeBc.ChOilMd to develop some secondary sex characteristics of the opposite sex? a. Mixed c. Isosexual b. Incomplete d. Homosexual Mixed precocious puberty (i.e., virilization of a girl or feminization of a boy) causes the child to develop some secondary sex characteristics of the opposite sex. This selection is the only option that accurately identifies the type of precocious puberty described. PTS: 1 REF: Page 887 4. What term is used to identify a condition in which the foreskin cannot be retracted over the glans penis? a. Paraphimosis c. Prephimosis b. Priapism d. Phimosis Phimosis is the only term used to identify the condition in which the foreskin cannot be retracted back over the glans. PTS: 1 REF: Page 888 5. What term is used to identify a fibrotic condition that causes lateral curvature of the penis during erection, which is associated with a local vasculitis-like inflammatory reaction and decreased tissue oxygenation? a. Phimosis c. Lateral paraphimosis b. Lateral phimosis d. Peyronie disease Peyronie disease (bent nail syndrome) is a fibrotic condition of the tunica albuginea of the penis, resulting in varying degrees of curvature and sexual dysfunction (see Figure 25-2). Although the exact cause is unknown, a local vasculitis-like inflammatory reaction occurs and decreased tissue oxygenation results in fibrosis and calcification. Peyronie disease is the only term used to identify the pathophysiologic condition described. PTS: 1 REF: Pages 889-890 6. What term is used to identify an inflammation of the glans penis? a. Glanitis c. Priapism b. Balanitis d. Hydrocelitis Balanitis is the only term used to identify an inflammation of the glans penis (see Figure 25-4). PTS: 1 REF: Page 890 7. Cryptorchidism can be defined as which of the following? a. Normal developmental state of the testes b. Abnormal state in which the teNsUteRsSaINreGoTvBe.CrdOeMveloped c. Lack of scrotum d. Testicular maldescent Cryptorchidism is a condition of testicular maldescent, the only option that accurately defines cryptorchidism. PTS: 1 REF: Page 892 8. What is the most common infectious cause of orchitis and one that usually affects postpubertal boys? a. Herpes c. Mumps b. Escherichia coli d. Cytomegalovirus Of the options available, mumps is the most common infectious cause of orchitis and usually affects postpubertal boys. PTS: 1 REF: Pages 894-895 9. The risk of which cancer is greater if the man has a history of cryptorchidism? a. Penile c. Prostate b. Testicular d. Epididymal The risk of testicular cancer is 35 to 50 times greater in men with cryptorchidism or in those with a history of cryptorchidism than it is for the general male population. This is not true of the other options. PTS: 1 REF: Pages 893-894 10. What are the clinical manifestations of testicular cancer? a. Firm, nontender testicular mass c. Painful fluid-filled testicular mass b. Painful, mobile, firm testicular mass d. Soft, nontender testicular mass Of the options available, a firm, painless testicular enlargement is commonly identified as the first sign of testicular cancer. PTS: 1 REF: Pages 895-896 11. How does the epididymis become infected? a. The pathogenic microorganisms ascend the vasa deferentia from an already infected urethra or bladder. b. The pathogenic microorganisms are attached to sperm that travel through the genital tract. c. The pathogenic microorganisms from the tunica vaginalis are transported to the epididymis. d. The pathogenic microorganisms from the prostate fluid ascend to the epididymis. The pathogenic microorganisms usually reach the epididymis by ascending the vasa deferentia from an already infecteNdUuRreStIhNrGaToBr.CblOaMdder. Of the selections available, this is the only option that accurately describes how the epididymis becomes infected. PTS: 1 REF: Page 897 12. Symptoms of benign prostatic hyperplasia (BPH) are a result of which pathophysiologic condition? a. Infection of the prostate c. Ischemia of the urethra b. Obstruction of the urethra d. Compression of the urethra BPH becomes problematic as prostatic tissue compresses the urethra, where it passes through the prostate. Of the selections available, only this option accurately describes the pathophysiologic condition behind the symptoms of BPH. PTS: 1 REF: Pages 897-899 13. Which infection has clinical manifestations that include the sudden onset of malaise, low back pain, and perineal pain with high fever and chills, dysuria, nocturia, and urinary retention? a. Orchitis c. Epididymitis b. Balanitis d. Bacterial prostatitis Bacterial prostatitis can exhibit common manifestations that include a sudden onset of malaise, low back and perineal pain, high fever (up to 40° C [104° F]), and chills, as well as dysuria, inability to empty the bladder, nocturia, and urinary retention. Myalgia and arthralgia also may occur. This selection is the only option that exhibits the symptoms described. PTS: 1 REF: Pages 899-900 14. Priapism has been associated with the abuse of what substance? a. Marijuana c. Cocaine b. Alcohol d. Heroin Of the options available, priapism has been associated with cocaine use. PTS: 1 REF: Page 890 15. Which age group should be targeted for testicular cancer education and screening? a. 15 to 35 year olds c. 30 to 55 year olds b. 20 to 45 year olds d. 45 to 70 year olds Overall, testicular cancers are rare, yet they are the most common form of cancer in young men between the ages of 15 and 35 years. PTS: 1 REF: Page 895 16. What is the reason breast cancer inNUmReSnINhGasTBsu.CcOhMa poor prognosis? a. Breast cancer is extremely aggressive in men. b. Treatment is usually delayed as a result of late detection. c. Chemotherapies are not as effective in men. d. Breast tumors tend to be small and hard to isolate. Breast cancer is relatively uncommon in men, but it has a poor prognosis because men tend to delay seeking treatment until the disease is advanced. This selection is the only option that accurately identifies the reason breast cancer in men has a poor prognosis. PTS: 1 REF: Page 914 MULTIPLE RESPONSE 17. Which are clinical manifestations of male breast cancer? (Select all that apply.) a. Ulceration present on the breast b. Retraction of breast tissue c. Nipple discharge d. Palpable mass midline of the nipple e. Unilateral solid mass , B, C, E The malignant male breast lesion is usually a unilateral solid mass located near the nipple. Because the nipple is commonly involved, crusting and nipple discharge are typical clinical manifestations. Other findings include skin retraction, ulceration of the skin over the tumor, and axillary node involvement. PTS: 1 REF: Page 914 18. Which statements are true regarding urethritis? (Select all that apply.) a. A purulent drainage may be present. b. A clear mucus-like discharge may be present. c. Symptoms include urethral tingling and itching or burning on urination. d. A 24-hour urine test is required to diagnose the disorder. e. Treatment includes appropriate antibiotic therapy. , B, C, E Symptoms of urethritis include urethral tingling and itching or a burning sensation on urination (dysuria), frequency, and urgency. The individual may note a purulent or clear mucus-like discharge from the urethra. Nucleic acid detection amplification tests allow easy detection of Neisseria gonorrhoeae and Chlamydia trachomatis in first-void urine. Treatment consists of appropriate antibiotic therapy for infectious urethritis and an avoidance of future chemical or mechanical irritation. PTS: 1 REF: Page 888 19. Which statements are true regarding prostate cancer? (Select all that apply.) a. It ranks second to lung cancer as being most common among American men. b. A familial history of prostate cancer is a risk factor. c. Dietary habits seem to play a rNoUleRiSnINitGsTdBe.vCeOloMpment. d. African-American men have an increased risk for its development. e. Being over 65 years of age increases the risk for developing prostate cancer. , C, D, E Prostate cancer is the most commonly diagnosed non–skin cancer in American men, and the incidence varies greatly worldwide. Possible causes include a genetic predisposition, environmental and dietary factors, inflammation, and alterations in levels of hormones (e.g., testosterone, dihydrotestosterone, estradiol) and growth factors. Incidence is greatest among northwestern European and North American men (particularly African Americans) older than 65 years of age. PTS: 1 REF: Pages 900-910 MATCHING Match the description with the disorder. A. Painless diverticulum of the epididymis located between the head of the epididymis and the testis B. Collection of fluid in the tunica vaginalis C. Rotation of a testis, which twists blood vessels of the spermatic cord D. Abnormal dilation of the vein within the spermatic cord 20. Varicocele 21. Hydrocele 22. Testicular torsion 23. Spermatocele 20. ANS: D PTS: 1 REF: Page 891 MSC: A varicocele is an abnormal dilation of a vein within the spermatic cord and is classically described as a bag of worms 21. ANS: B PTS: 1 REF: Page 892 MSC: A hydrocele is a collection of fluid within the tunica vaginalis 22. ANS: C PTS: 1 REF: Page 894 MSC: Torsion of the testis is rotation of a testis, which twists blood vessels in the spermatic cord. 23. ANS: A PTS: 1 REF: Page 892 MSC: A spermatocele is a painless diverticulum of the epididymis located between the head of the epididymis and the testis. NURSINGTB.COM Chapter 27: Sexually Transmitted Infections MULTIPLE CHOICE 1. What unique factor causes adolescent girls to have a high risk for sexually transmitted infections (STIs)? a. They are in an experimental phase with sexual intercourse and believe they are resistant to developing STIs. b. The adolescent cervix is immature and lacks immunity. c. The length of the vaginal canal is short in adolescents, allowing a greater concentration of microorganisms within the internal genitalia. d. In adolescent girls, the anus to the vaginal introitus are in close proximity. Partly, perhaps, because of risk-taking behavior (unprotected intercourse or selection of high-risk partners), many adolescents have an increased risk for STI exposure and infection. The unique factor for adolescent women is that they have a physiologically increased susceptibility to infection because of increased cervical immaturity and lack of immunity. The remaining options are not considered legitimate risk factors for STIs. PTS: 1 REF: Pages 918-919 2. How is gonorrhea transmitted from a pregnant woman to her fetus? a. Unbound in the blood via the placenta b. Attached to immunoglobulin G (IgG) via the placenta c. Across amniotic membranes bNyUtRheSIdNiGreTcBt .iCnOoMculation with the fetal scalp electrodes during labor monitoring d. Predominately through infected cervical and secretions during the birth process A pregnant woman can transmit gonorrhea to her fetus during the birth process. The infection passes from mother to child predominately through infected cervical and vaginal secretions. The transmission is not associated with the other options. PTS: 1 REF: Page 920 3. Which statement is false about the factors that facilitate the ascent of gonococci into the uterus and fallopian tubes? a. Ascent of gonococci is facilitated because the cervical plug disintegrates during menstruation. b. Ascent of gonococci is facilitated because the vaginal pH decreases to 2 or 3. c. Ascent of gonococci is facilitated because the uterine contractions may cause retrograde menstruation into the fallopian tubes. d. Ascent of gonococci is facilitated because the bacteria may adhere to sperm and be transported to the fallopian tubes. Several factors can facilitate the ascent of gonococci into the uterus and the fallopian tubes, where they cause pelvic inflammatory disease (PID). Among these factors are (1) disintegration of the cervical mucous plug and (2) a rise in vaginal pH greater than 4.5 during menstruation. The other options are accurate statements. PTS: 1 REF: Page 921 4. In women, what is the usual site of original gonococcal infection? a. Endocervical canal c. Fallopian tube b. Vagina d. Labia majora In women, the endocervical canal (inner portion of the cervix) is the usual site of original gonococcal infection, although urethral colonization and infection of Skene or Bartholin glands also are common. The other options are not usually associated with gonococcal infections. PTS: 1 REF: Page 921 5. What is the primary site for uncomplicated local gonococci infections in men? a. Epididymis c. Urethra b. Lymph nodes d. Prostate Uncomplicated local infections are observed primarily as urethral infections in men. PTS: 1 REF: Page 921 NURSINGTB.COM 6. What local complication of a gonococcal infection is diagnosed in approximately 10% of affected women? a. Acute salpingitis c. Vaginitis b. Cystitis d. Cervicitis Acute salpingitis, or pelvic inflammatory disease (PID), is the most common local complication in women. Approximately 10% of women with untreated cervical gonorrhea develop PID. PTS: 1 REF: Page 921 7. Which laboratory test is considered adequate for an accurate and reliable diagnosis of gonococcal urethritis in a symptomatic man? a. Ligase chain reaction (LCR) c. Polymerase chain reaction (PCR) b. Gram-stain technique d. DNA testing Microscopic evaluation of Gram-stained slides of clinical specimens is deemed positive for Neisseria gonorrhoeae if gram-negative diplococci with the typical “kidney bean” morphologic appearance are found inside polymorphonuclear leukocytes. Such a finding is considered adequate for the diagnosis of gonococcal urethritis in a symptomatic man. The other options are not relevant to the diagnosis of this condition. PTS: 1 REF: Page 922 8. How does an established gonococcal infection usually express itself in newborns? a. Generalized skin rash 4 to 6 days after birth b. Systemic infection with fever c. Bilateral corneal ulceration d. Yellow vaginal or penile discharge approximately 10 days after birth Established infection causes bilateral corneal ulceration. The other options are not usual sites for such an infection. PTS: 1 REF: Page 922 9. What is the major concern regarding the treatment of gonococci infections? a. Development of antibiotic resistance c. Changes in pathogenicity b. Changes in virulence d. Mutations into different strains Several types of drug-resistant strains have been identified; they are penicillinase-producing Neisseria gonorrhoeae (PPNG), which is resistant to penicillin; tetracycline-resistant N. gonorrhoeae (TRNG), which is resistant to tetracycline; chromosomal control of mechanisms of resistance of N. gonorrhoeae (CMRNG), which is resistant to penicillin and tetracycline; and increasingly a fluoroquinolone-resistant N. gonorrhoeae (QRNG). The other options are not major concerns. PTS: 1 REF: Page 922 NURSINGTB.COM 10. Which sexually transmitted infection frequently coexists with gonorrhea? a. Syphilis c. Chlamydia b. Herpes simplex virus d. Chancroid The coexistence of chlamydial infection with gonorrhea frequently occurs. No coexistence exists with the other options. PTS: 1 REF: Page 922 11. During which stage of syphilis do bloodborne bacteria spread to all the major organ systems? a. Primary c. Latent b. Secondary d. Tertiary Bloodborne bacteria spread to all major organ systems during only stage II, secondary syphilis (see Box 26-2). PTS: 1 REF: Page 923 12. In which stage of syphilis would the following clinical manifestations be found: destructive skin, bone and soft tissue lesions, aneurysms, heart failure, and neurosyphilis? a. Primary c. Latent b. Secondary d. Tertiary Stage IV, tertiary syphilis, is the only stage during which significant morbidity and mortality occur, including destructive skin, bone, and soft-tissue lesions (see Box 26-2). PTS: 1 REF: Page 924 13. Which organism is responsible for the development of syphilis? a. Neisseria syphilis c. Haemophilus ducreyi b. Treponema pallidum d. Chlamydia trachomatis S. pallidum is the only cause of syphilis. PTS: 1 REF: Page 923 14. Which is a characteristic lesion of secondary syphilis? a. Condylomata lata c. Chancroid b. Gummas d. Donovan bodies The only secondary syphilis lesion is the condylomata lata. PTS: 1 REF: Pages 924-925 15. By which method is the organism that causes syphilis best identified? a. Acid-fast stain c. In vitro culture b. Gram-stained slide NURSINGTdB..CODMarkfield microscopy Because Treponema pallidum cannot be cultured in vitro, early definitive diagnosis of primary or secondary syphilis depends on darkfield microscopy of a specimen taken from a chancre, regional lymph node, or other lesion. The remaining options are not relevant. PTS: 1 REF: Page 925 16. When a patient has small, vesicular lesions that last between 10 and 20 days, which sexually transmitted infection is suspected? a. Genital herpes c. Syphilis b. Chancroid d. Chlamydia If symptoms occur, the individual may have small (1 to 2 mm), multiple, vesicular lesions that are generally located on the labia minora, fourchette, or penis. They may also appear on the cervix, buttocks, and thighs and are often painful and pruritic. These lesions usually last approximately 10 to 20 days. The other options do not demonstrate these symptoms. PTS: 1 REF: Page 933 17. Which statement is false regarding the risk of transmission of the herpes simplex virus (HSV) from mother to fetus? a. Neonatal infection of HSV rarely occurs in the intrapartum or postpartum period. b. The risk is higher in women who have a primary HSV infection. c. The risk is higher in women who experience ruptured membranes more than 6 hours before delivery. d. The risk is higher when internal fetal monitoring devices are used. Neonatal infections can occur in utero or, more commonly, during the intrapartum or postpartum period. The other options are accurate statements. PTS: 1 REF: Page 933 18. During the latent period of a herpes virus infection, where in the host cell is the genome of the virus maintained? a. Mitochondria c. Nucleus b. Lysosomes d. Cytoplasm During the latent period, the genome for the virus is maintained in the host cell nucleus without causing the death of the cell. PTS: 1 REF: Page 933 19. During reactivation (release from latency), herpes virus genomes are transported through which nerves to the dermal surface? a. Somatic c. Autonomic b. Peripheral sensory d. Peripheral motor NURSINGTB.COM Only during reactivation are the viral genomes transported through the peripheral sensory nerves back to the dermal surface. PTS: 1 REF: Page 933 20. Which statement provides the most accurate information regarding the transmission of herpes simplex virus (HSV)? a. HSV is transmitted only when vesicles are present. b. HSV is transmitted only while lesions are present. c. The use of condoms prevents the transmission of HSV. d. The risk of transmission is present even during latent periods. Latent infections can become reactivated and cause a recurrent infection with similar manifestations. The other options are not accurate statements regarding the transmission of HSV. PTS: 1 REF: Pages 933-934 21. Which drug may be prescribed orally for outbreak management of herpes simplex viral (HSV) infections? a. Acyclovir (Zovirax) c. Zidovudine (AZT) (Retrovir) b. 5-Fluorouracil (5-FU) d. Bichloroacetic acid (BCA) Although no curative treatment for HSV infection is known, only oral acyclovir, valacyclovir, penciclovir, and famciclovir are used for primary and periodic outbreaks and to prevent recurrences. PTS: 1 REF: Page 934 22. Which of the following causes condylomata acuminata or genital warts? a. Chlamydia c. Human papillomavirus (HPV) b. Adenovirus d. Herpes simplex virus 1 (HSV-1) Genital warts are quite contagious and are a result of only HPV. PTS: 1 REF: Pages 934-935 23. Which treatment is used for trichomoniasis? a. Topical application of 5-Fluorouracil (5-FU) b. Topical application of acyclovir c. Systemic metronidazole d. Systemic tetracycline The treatment of choice for trichomoniasis is a single 2-gram dose of metronidazole (Flagyl) or tinidazole. The other options are not applicable. PTS: 1 REF: Page 938 24. A woman diagnosed with trichomNoUniRaSsIiNs GasTkBs.CifOhMer sexual partner should be treated as well. What is the appropriate response? a. Sexual partners should be treated only if symptoms are present. b. Sexual partners should be treated even if they are asymptomatic. c. Infections in men are self-limiting; therefore a male sexual partner does not require treatment. d. Sexual partners should be treated to prevent infection. Sexual partners, even if asymptomatic, are also treated and examined for coexisting sexually transmitted infections. PTS: 1 REF: Page 938 25. Which microorganism is sexually transmitted, primarily by homosexual men, through infected feces? a. Shigellosis c. Giardia lamblia b. Cytomegalovirus (CMV) d. Entamoeba histolytica Only the Shigella infection, termed shigellosis, is transmitted by contact with infected feces particularly among homosexual men. PTS: 1 REF: Page 940 | Table 26-3 26. Which hepatitis virus is known to be sexually transmitted? a. A c. C b. B d. D Only hepatitis B virus (HBV) is known to be sexually transmitted. PTS: 1 REF: Page 940 27. Which sexually transmitted disease occasionally causes clinical manifestations of scant intermittent penile discharge, slight pruritus, and mild dysuria? a. Campylobacter enteritis c. Cytomegalovirus enteritis b. Shigellosis d. Trichomoniasis Most men with trichomoniasis are asymptomatic but may have scant intermittent discharge, slight pruritus, and mild dysuria. The other options do not demonstration these symptoms. PTS: 1 REF: Page 937 MULTIPLE RESPONSE 28. Which statements are true regarding the hepatitis B infection? (Select all that apply.) a. Hepatitis B poses a significant risk for chronic liver disease. b. Hepatocellular cancer is a common comorbid condition. c. Universal vaccination of infants and children is recommended. d. The preventive method of choNicUeRiSsIiNmGmTBun.CiOzaMtion. e. Universal vaccination of sexually active adults is recommended. , B, C, D Hepatitis B infection poses significant health risks including chronic liver disease and hepatocellular cancer. Immunization against hepatitis B is the most effective means of preventing transmission. Universal vaccination of infants and children is recommended, as well as vaccination of high-risk adults. PTS: 1 REF: Page 941 29. What are the common modes of transmission for the hepatitis B virus (HBV)? (Select all that apply.) a. Needle punctures b. Blood transfusions c. Contact with infected body fluids d. Skin cuts e. Ingestion of infected substances , B, C, D Transmission of HBV can occur through needle puncture, blood transfusion, cuts in the skin, and contact with infected body fluids. Ingestion is not a recognized transmission mode. PTS: 1 REF: Page 941 30. Which statements are true regarding the parasitic infection referred to as scabies? (Select all that apply.) a. Scabies is spread through skin-to-skin contact. b. The crab lice, Phthirus pubis, cause scabies. c. Severe pruritus is its major clinical manifestation. d. Symptoms worsen at night. e. Treatment is provided through oral medication therapy. , C, D Scabies is a common parasitic infection that can be spread by skin-to-skin contact and sexual contact. The scabies mite burrows through the skin, depositing two or three large eggs per day. Intense pruritus, especially at night, is the most pronounced clinical manifestation. Treatment consists of topical application of a pediculicide. Pediculosis pubis (crabs) is commonly transmitted sexually and is caused by the crab louse, P. pubis. PTS: 1 REF: Pages 938-939 31. Which statements are true concerning the sexually transmitted infection (STI) lymphogranuloma venereum? (Select all that apply.) a. Lymphogranuloma venereum is an STI commonly diagnosed in the United States. b. It begins as a skin infection. c. Lymphogranuloma venereum spreads to lymph tissues. d. Primary and secondary lesions are apparent with this STI. e. A 60-day course of oral erythromycin is the recommended treatment. , C, D Lymphogranuloma venereum is aNcUhRroSnINicGSTTBI.CuOnMcommon in the United States. The lesion begins as a skin infection and spreads to the lymph tissue, causing inflammation, necrosis, buboes, and abscesses of the inguinal lymph nodes. Primary lesions appear on the penis and scrotum in men and on the cervix, vaginal wall, and labia in women. Secondary lesions involve inflammation and swelling of the lymph nodes with the formation of large blue buboes that rupture and form draining ulcerative lesions. A 21-day or longer course of oral doxycycline or erythromycin is needed for treatment. Treatment of sexual partners is recommended. PTS: 1 REF: Pages 931-932 MATCHING Match the disease with the corresponding causative organism. A. Trichomoniasis B. Granuloma inguinale C. Amebiasis D. Syphilis E. Chancroid 32. Treponema pallidum 33. Haemophilus ducreyi 34. Calymmatobacterium granulomatis 35. Entamoeba histolytica 36. Trichomonas vaginalis 32. ANS: D PTS: 1 REF: Page 923 MSC: T. pallidum is the cause of syphilis. 33. ANS: E PTS: 1 REF: Page 925 MSC: H. ducreyi, a gram-negative bacillus, causes chancroid. 34. ANS: B PTS: 1 REF: Page 929 MSC: Granuloma inguinale (donovanosis) is a chronic, progressively destructive bacterial infection caused by Calymmatobacterium granulomatis. 35. ANS: MSC: C PTS: 1 REF: Page 919 | Table 26-1 E. histolytica is the cause of amebiasis. 36. ANS: MSC: A PTS: 1 REF: Page 937 Trichomoniasis is a result of infection caused by T. vaginalis. NURSINGTB.COM Chapter 28: Structure and Function of the Hematologic System MULTIPLE CHOICE 1. What is the most abundant class of plasma protein? a. Globulin c. Clotting factors b. Albumin d. Complement proteins Albumin (approximately 60% of total plasma protein at a concentration of about 4 g/dl) is the most abundant plasma protein. PTS: 1 REF: Page 946 2. What is the effect of low plasma albumin? a. Clotting factors decrease, thus increasing the chance of prolonged bleeding. b. Fewer immunoglobulins are synthesized, thus impairing the immune function. c. Less iron is stored, thus increasing the incidence of iron deficiency anemia. d. Osmotic pressure decreases, thus water moves from the capillaries to the interstitium. In the case of decreased production (e.g., cirrhosis, other diffuse liver diseases, protein malnutrition) or excessive loss of albumin (e.g., certain kidney diseases, extensive burns), the reduced oncotic pressure leads to excessive movement of fluid and solutes into the tissues and decreased blood volume. The other options are not accurate descriptions of the effect of low plasma albumin. NURSINGTB.COM PTS: 1 REF: Page 946 3. What is the life span of an erythrocyte (in days)? a. 20 to 30 c. 100 to 120 b. 60 to 90 d. 200 to 240 Because it cannot undergo mitotic division, the erythrocyte has a limited life span of approximately 120 days. PTS: 1 REF: Pages 947-948 4. Which statement concerning erythrocytes is true? a. Erythrocytes contain a nucleus, mitochondria, and ribosomes. b. Erythrocytes synthesize proteins. c. Erythrocytes have the ability to change shape to squeeze through microcirculation. d. Erythrocyte colony-stimulating factor (E-CSF) stimulates erythrocytes. Reversible deformity enables the erythrocyte to assume a more compact torpedo-like shape, squeeze through the microcirculation, and return to normal. The other options are not accurate statements about erythrocytes. PTS: 1 REF: Page 948 5. Granulocytes that contain granules of vasoactive amines, such as histamine, are called: a. Neutrophils c. Monocytes b. Eosinophils d. Basophils Basophils contain cytoplasmic granules that hold an abundant mixture of biochemical mediators, including histamine, chemotactic factors, proteolytic enzymes, and an anticoagulant (heparin) (see Figure 27-3, C). This is not an accurate description of any of the other options. PTS: 1 REF: Page 949 6. Which of the following are formed elements of the blood that are not cells but are disk-shaped cytoplasmic fragments essential for blood clotting? a. Monocytes c. Macrophages b. Platelets d. Erythrocytes Platelets (thrombocytes) are not true cells but are disk-shaped cytoplasmic fragments that are essential for blood coagulation and control of bleeding. This description is not accurate for any of the other options. PTS: 1 REF: Pages 950-951 7. Blood cells that differentiate into macrophages are known as: a. Monocytes NURSINGTcB..COEMosinophils b. Neutrophils d. Basophils Only monocytes migrate into a variety of tissues and fully mature into tissue macrophages and myeloid dendritic cells (see Table 27-3). PTS: 1 REF: Page 950 8. Without prior exposure to an antigen, which cells are able to destroy some types of tumor cells and some virus-infected cells? a. Lymphocytes c. Megakaryocytes b. Plasma cells d. Natural killer (NK) cells NK cells, which resemble large granular lymphocytes, kill some types of tumor cells (in vitro) and some virus-infected cells without being induced by previous exposure to these antigens. This capability is not true of the other options. PTS: 1 REF: Page 950 9. What is the life span of platelets (in days)? a. 10 c. 90 b. 30 d. 120 A platelet circulates for approximately 10 days and ages. Macrophages of the mononuclear phagocyte system, mostly in the spleen, remove platelets. PTS: 1 REF: Page 951 10. Fetal hematopoiesis occurs in which structure? a. Gut c. Bone marrow b. Spleen d. Thymus The spleen is the largest of the secondary lymphoid organs and the site of fetal hematopoiesis. PTS: 1 REF: Page 951 11. What is the consequence of a splenectomy? a. The level of iron in circulation increases. b. Antibody production increases to improve immune function. c. The number of defective cells in circulation increases. d. The number of clotting factors increases. Splenic absence from any cause (e.g., atrophy, traumatic injury, removal because of disease) has several secondary effects on the body, among them an increase in morphologically defective blood cells in the circulation, confirming the spleen’s role in removing old or damaged cells. This description of the consequence of a splenectomy is not accurate for the other options. NURSINGTB.COM PTS: 1 REF: Pages 951-952 12. During an infection, why do lymph nodes enlarge and become tender? a. B lymphocytes proliferate. b. The nodes are inflamed. c. The nodes fill with purulent exudate. d. The nodes are not properly functioning. The B lymphocyte proliferation in response to significant antigen (e.g., during infection) may result in lymph node enlargement and tenderness (reactive lymph node). This description is not accurate for the other options. PTS: 1 REF: Page 954 13. Which blood cells are the chief phagocytes involved in the early inflammation process? a. Neutrophils c. Eosinophils b. Monocytes d. Erythrocytes Neutrophils are the chief phagocytes of early inflammation. PTS: 1 REF: Page 949 14. Which blood cells are biconcave in shape and have the capacity to be reversibly deformed? a. Neutrophils c. Eosinophils b. Monocytes d. Erythrocytes The erythrocyte’s size and shape are ideally suited to its function as a gas carrier. A red blood cell (RBC) is a small disk with two unique properties: (1) a biconcave shape and (2) the capacity to be reversibly deformed. These are characteristics not observed in any of the other options. PTS: 1 REF: Page 948 15. Which hemoglobin is made from oxidized ferric iron (Fe3+) and lacks the ability to bind oxygen? a. Deoxyhemoglobin c. Methemoglobin b. Oxyhemoglobin d. Glycosylated hemoglobin Without reactivation by methemoglobin reductase, the Fe3+-containing hemoglobin (methemoglobin) cannot bind oxygen. This capability is not true of the other types of hemoglobin mentioned. PTS: 1 REF: Page 961 16. The absence of parietal cells would prevent the absorption of an essential nutrient necessary to prevent which type of anemia? a. Iron deficiency NURSINGTcB..COFMolic acid deficiency anemia b. Pernicious anemia d. Aplastic anemia Dietary vitamin B12 is a large molecule that requires a protein secreted by parietal cells into the stomach (intrinsic factor [IF]) to transport across the ileum. Defects in IF production lead to decreased B12 absorption and pernicious anemia. The other options are not the result of this process. PTS: 1 REF: Page 962 17. Which nutrients are necessary for the synthesis of DNA and the maturation of erythrocytes? a. Protein and niacin c. Cobalamin (vitamin B12) and folate b. Iron and vitamin B6 (pyridoxine) d. Pantothenic acid and vitamin C Cobalamin and folate are necessary for the synthesis of DNA and for the maturation of erythrocytes. The remaining options are not necessary for these processes to occur. PTS: 1 REF: Page 962 | Table 27-6 18. Which nutrients are necessary for hemoglobin synthesis? a. Protein and niacin c. Cobalamin (vitamin B12) and folate b. Iron and vitamin B6 (pyridoxine) d. Pantothenic acid and vitamin C Iron and B6 (pyridoxine) are necessary for hemoglobin synthesis (see Table 27-6). The remaining options are not necessary for hemoglobin synthesis. PTS: 1 REF: Page 962 | Table 27-6 19. Recycling of iron from erythrocytes is made possible by which of the following? a. Transferrin c. Apoferritin b. Hemosiderin d. Erythropoietin Transferrin is recycled (transferrin cycle) in the following manner: (1) the transferrin-iron complex binds to a transferring receptor on the erythroblast’s plasma membrane; (2) the complex moves into the cell by receptor-mediated endocytosis; (3) iron is released (dissociated) from transferrin; and (4) the dissociated transferrin is returned to the bloodstream for reuse. The other options do not present an accurate description of the recycling of erythrocytic iron. PTS: 1 REF: Pages 963-964 20. By which structure are mature erythrocytes removed from the bloodstream? a. Liver c. Thymus b. Lymph nodes d. Spleen After approximately 100 to 120 days in the circulation, old erythrocytes are removed by tissue macrophages, primarily in the spleen. NURSINGTB.COM PTS: 1 REF: Page 962 21. Which substance is used to correct the chronic anemia associated with chronic renal failure? a. Iron c. Cobalamin (vitamin B12) b. Erythropoietin d. Folate One of the most significant advances in the study of hematopoietic growth factors has been the development of erythropoietin for individuals with chronic renal failure. The other options are not associated with the treatment of chronic anemia. PTS: 1 REF: Pages 960-961 22. What is the role of thromboxane A (TXA2) in the secretion stage of hemostasis? a. Stimulates the synthesis of serotonin. b. Promotes vasodilation. c. Stimulates platelet aggregation. d. Promotes formation of cyclooxygenase. Platelet aggregation is primarily stimulated by TXA2 and adenosine diphosphate (ADP), which induce functional fibrinogen receptors on the platelet. The other options do not present an accurate description of the role of thromboxane A. PTS: 1 REF: Page 969 23. Which of the following is the role of nitric oxide (NO) in hemostasis? a. Stimulates the release of fibrinogen to maintain the platelet plug. b. Stimulates the release of clotting factors V and VII. c. Causes vasoconstriction and stimulates platelet aggregation. d. Controls platelet activation through cyclic adenosine monophosphate (cAMP)–mediated signaling. Endothelial cell NO synthase produces NO, which controls platelet activation through cAMP-mediated signaling. The other options do not present an accurate description of the role of NO in hemostasis. PTS: 1 REF: Page 966 | Figure 27-18 24. The drug heparin acts in hemostasis by which processes? a. Inhibiting thrombin and antithrombin III (AT-III) b. Preventing the conversion of prothrombin to thrombin c. Shortening the fibrin strands to retract the blood clot d. Degrading the fibrin within blood clots Clinically administered heparin or heparin sulfate (on the surface of endothelial cells) binds to AT-III and induces a conformational change that greatly enhances its activity. Under normal conditions, the presence of endothelial cell heparin sulfate and available AT-III in the circulation cooperateNUtoRpSrIoNtGecTtBt.hCeOMvessels from the effects of spontaneously activated thrombin. The other options do not accurately describe the role heparin plays in hemostasis. PTS: 1 REF: Page 970 25. What is plasmin’s role in the clotting process? a. Stimulates platelet aggregation. b. Inhibits platelet adhesion and aggregation. c. Prevents the conversion of prothrombin to degrade the fibrin within blood clots. d. Degrades the fibrin within blood clots. Plasmin (also called fibrinase or fibrinolysin) is a serine protease that degrades fibrin polymers in clots. It is not capable of the functions described in the remaining options. PTS: 1 REF: Pages 971-972 26. What does polycythemia at birth indicate? a. Hypoxia in utero c. Congenitally absent spleen b. Dysfunctional bone marrow d. Dehydration in utero The hypoxic intrauterine environment stimulates erythropoietin production in the fetus and accelerates fetal erythropoiesis, producing polycythemia (excessive proliferation of erythrocyte precursors) of the newborn. The other options are not related to polycythemia. PTS: 1 REF: Page 975 27. Where are Kupffer cells located? a. Kidneys c. Pancreas b. Liver d. Spleen The liver macrophages are the only location for Kupffer cells. PTS: 1 REF: Page 950 | Page 962 | Table 27-3 28. Where are Langerhans cells found? a. Skin c. Kidney b. Intestinal lining d. Thyroid Of the available options, only the skin is the location for Langerhans cells. PTS: 1 REF: Page 950 | Table 27-3 29. What is the role of collagen in the clotting process? a. Initiates the clotting cascade. c. Stimulates fibrin. b. Activates platelets. d. Deactivates fibrinogen. NURSINGTB.COM In the clotting process, collagen provides a particularly strong stimulus to activate platelets. Collagen does not bring about any of the other options. PTS: 1 REF: Page 969 30. Which form of iron (Fe) can be used in the formation of normal hemoglobin? a. Fe+ c. Fe3+ b. Fe2+ d. Fe4+ It is crucial that the iron be correctly charged; only reduced ferrous iron (Fe2+) can bind oxygen in the lungs and release it in the tissues. PTS: 1 REF: Page 961 31. Where are alveolar macrophages found? a. Skin c. Gastrointestinal tract b. Breasts d. Lungs The lung is the only location for alveolar macrophages. PTS: 1 REF: Page 950 | Table 27-3 32. What changes to the hematologic system is related to age? a. Platelet adhesiveness decreases. b. Lymphocyte function decreases. c. Cellular immunity increases. d. Erythrocyte reproduction accelerates. Blood composition changes little with age. A delay in erythrocyte replenishment may occur after bleeding, presumably because of iron deficiency. Lymphocyte function appears to decrease with age. Particularly affected is a decrease in cellular immunity. Platelet adhesiveness probably increases with age. PTS: 1 REF: Page 975 33. What is the function of erythrocytes? a. Tissue oxygenation c. Infection control b. Hemostasis d. Allergy response Erythrocytes are solely responsible for tissue oxygenation. PTS: 1 REF: Pages 947-948 MULTIPLE RESPONSE 34. Which characteristics allow erythrocytes to function as gas carriers? (Select all that apply.) a. Permanent shape b. Compactness c. Reversible deformability NURSINGTB.COM d. Presence of hyperactive mitochondria e. Biconcavity , E A red blood cell (RBC) is a small disk with two unique properties: (1) a biconcave shape and (2) the capacity to be reversibly deformed. The other options are not relevant to the function of gas transport. PTS: 1 REF: Page 948 35. Which statements about plasma proteins are correct? (Select all that apply.) a. Provide clotting factors. b. Transport triglycerides. c. Synthesize complement proteins. d. Create hydrostatic pressure. e. Transport cholesterol. , B, C, E Plasma proteins do not create hydrostatic pressure. The other options are all accurate statements regarding plasma proteins. PTS: 1 REF: Pages 945-947 36. What are the primary anticoagulant mechanisms? (Select all that apply.) a. Antithrombin III b. Tissue factor pathway inhibitor c. Hematopoiesis d. Protein C e. Phagocytosis , B, D The major regulatory factors that control hemostasis reside where the greatest probability of clotting would occur—on the endothelial cell surface. The primary anticoagulant mechanisms include thrombin inhibitors (e.g., antithrombin III), tissue factor inhibitors (e.g., tissue factor pathway inhibitor), and mechanisms for degrading activated clotting factors (e.g., protein C). Hematopoiesis and phagocytosis are processes that are not related to anticoagulation. PTS: 1 REF: Page 970 37. Which statements are true regarding the role of the endothelium in clot formation? (Select all that apply.) a. The surface of the endothelium produces plasma protease inhibitors. b. Plasma protease inhibitors assist in preventing clot formation. c. Thrombomodulin is a protein that is converted on the surface of endothelial cells. d. Protein A binds to thrombomodulin. e. Activated protein C enhances the adhesion ability of neutrophils. , B, C The surface of the endothelium produces plasma protease inhibitors to resist clot formation. Thrombomodulin is a mNUemRSbIrNaGneTBth.CroOmMbin-binding protein matter and is converted to activated protein C (see Figure 27-18) on the surface of endothelial cells. Protein C in the circulation binds to thrombomodulin. Activated protein C inhibits the adhesion of neutrophils to the endothelium. PTS: 1 REF: Pages 970-971 38. Which statements characterize albumin? (Select all that apply.) a. Retains sodium to maintain water balance. b. Provides colloid osmotic pressure. c. Is synthesized in the liver. d. Is a carrier for drugs that have low water solubility. e. Is a small molecule , C, D Albumin is a plasma protein produced by the liver. It serves as a carrier molecule for the normal components of blood, as well as for drugs that have low solubility in water (e.g., free fatty acids, lipid-soluble hormones, thyroid hormones, bile salts). Albumin molecules are large and do not diffuse freely through the vascular endothelium, thus they maintain the critical colloidal osmotic pressure (or oncotic pressure) that regulates the passage of water and solutes into the surrounding tissues (see Chapters 1 and 3). PTS: 1 REF: Page 946 MATCHING Match the descriptions with the corresponding terms. A. Clotting B. Red blood cell development C. Red blood cell destruction D. Platelet formation E. Blood cell production 39. Endomitosis 40. Hemostasis 41. Hematopoiesis 42. Erythropoiesis 43. Phagocytosis 39. ANS: D PTS: 1 REF: Page 965 MSC: During thrombopoiesis, the megakaryocyte progenitor is programmed to undergo an endomitotic cell cycle called endomitosis, during which DNA replication of platelets occurs. 40. ANS: A PTS: 1 REF: Page 965 MSC: Hemostasis is defined as arrest of bleeding. 41. ANS: E PTS: 1 REF: Page 954 MSC: Blood cell production (hematopoiesis) is ongoing, occurring in the liver and spleen of the fetus and only in bone marrow (medullary hematopoiesis) after birth. 42. ANS: B PTS: 1 REF: Page 959 MSC: It was not until the 1850s that the bone marrow was identified as the site of erythropoiesis, or the development of red blood cells. 43. ANS: C PTS: 1 REF: Page 950 MSC: Monocytes and macrophages NarUeRaScItNivGeTpBh.aCgOocMytes that participate in the immune and inflammatory responses. They also ingest dead or defective host cells, particularly blood cells. Chapter 29: Alterations of Erythrocyte Platelet, Hemostatic Function MULTIPLE CHOICE 1. What term is used to describe the capacity of some erythrocytes to vary in size, especially in relationship to some anemias? a. Poikilocytosis c. Anisocytosis b. Isocytosis d. Microcytosis Additional descriptors of erythrocytes associated with some anemias include anisocytosis (assuming various sizes) or poikilocytosis (assuming various shapes) (see Figure 28-1). The remaining terms are not associated with this condition. PTS: 1 REF: Page 982 2. What is the fundamental physiologic manifestation of anemia? a. Hypotension c. Hypoxia b. Hyperesthesia d. Ischemia The fundamental physiologic manifestation of anemia is a reduced oxygen-carrying capacity of the blood, resulting in tissue hypoxia. PTS: 1 REF: Page 982 | Page 985 3. The paresthesia that occurs in vitNamURinSIBN1G2TdBe.fCiOciMency anemia is a result of which of the following? a. Reduction in acetylcholine receptors in the postsynaptic nerves b. Myelin degeneration in the spinal cord c. Destruction of myelin in peripheral nerves d. Altered function of neurons in the parietal lobe Effects on the nervous system can occur if a vitamin B12 deficiency causes the anemia. Myelin degeneration may occur with the resultant loss of fibers in the spinal cord, producing paresthesia (numbness), gait disturbances, extreme weakness, spasticity, and reflex abnormalities. This selection is the only option that accurately describes the cause of paresthesia in such anemias. PTS: 1 REF: Page 985 | Page 987 4. Which of the following describes how the body compensates for anemia? a. Increasing rate and depth of breathing b. Decreasing capillary vasoconstriction c. Hemoglobin holding more firmly onto oxygen d. Kidneys releasing more erythropoietin Tissue hypoxia creates additional demands and compensatory actions on the pulmonary and hematologic systems. The rate and depth of breathing increase in an attempt to increase the availability of oxygen. This selection is the only option that accurately describes the compensation mechanism in such anemias. PTS: 1 REF: Page 985 5. Which of the following is classified as a megaloblastic anemia? a. Iron deficiency c. Sideroblastic b. Pernicious d. Hemolytic Pernicious anemia is the most common type of megaloblastic anemia. The remaining options are not classified as megaloblastic anemias. PTS: 1 REF: Pages 987-988 6. Deficiencies in folate and vitamin B12 alter the synthesis of which of the following? a. RNA c. DNA b. Cell membrane d. Mitochondria Deficiencies in folate and vitamin B12 result in defective erythrocyte precursor DNA synthesis. These deficiencies are not associated with alterations of the other options. PTS: 1 REF: Page 987 7. The underlying disorder of whichNaUneRmSIiNaGisTBa.rCeOsuMlt of the defective secretion of the intrinsic factor, which is essential for the absorption of vitamin B12? a. Microcytic c. Hypochromic b. Pernicious d. Hemolytic ANS: B Vitamin B12 deficiency causes pernicious anemia, the most common type of megaloblastic anemia. PTS: 1 REF: Pages 987-988 8. After a person has a subtotal gastrectomy for chronic gastritis, which type of anemia will result? a. Iron deficiency c. Folic acid b. Aplastic d. Pernicious From the options available, only pernicious anemia is caused by vitamin B12 deficiency, which is often associated with the end-stage type A chronic atrophic gastritis. PTS: 1 REF: Page 988 9. What causes the atrophy of gastric mucosal cells that result in pernicious anemia? a. Erythrocyte destruction c. Vitamin B12 malabsorption b. Folic acid malabsorption d. Poor nutritional intake ANS: C Deficiency in intrinsic factor (IF) secretion may be congenital or may result from adult onset gastric mucosal atrophy and the destruction of parietal cells. In older adults, virtually all vitamin B12-deficiency anemia is caused by a failure of IF-related absorption. This selection is the only option that accurately identifies the cause of gastric mucosal cell atrophy. PTS: 1 REF: Page 988 10. Which statement best describes a Schilling test? a. Administration of radioactive cobalamin and the measurement of its excretion in the urine to test for vitamin B12 deficiency b. Measurement of antigen-antibody immune complexes in the blood to test for hemolytic anemia c. Measurement of serum ferritin and total iron-binding capacity in the blood to test for iron deficiency anemia d. Administration of folate and measurement in 2 hours of its level in a blood sample to test for folic acid deficiency anemia. The Schilling test indirectly evaluates vitamin B12 absorption by administering radioactive B12 and measuring excretion in the urine. This selection is the only option that accurately describes a Schilling test. PTS: 1 REF: Page 988 11. What is the treatment of choice for pernicious anemia (PA)? a. Cyanocobalamin by oral intakNeURSINGTB.COM b. Vitamin B12 by injection c. Ferrous fumarate by Z-track injection d. Folate by oral intake Replacement of vitamin B12 (cobalamin) is the treatment of choice for PA. Initial injections of vitamin B12 are administered weekly until the deficiency is corrected, followed by monthly injections for the remainder of the individual’s life. The other options are not treatments for PA. PTS: 1 REF: Page 988 12. Which condition resulting from untreated pernicious anemia (PA) is fatal? a. Brain hypoxia c. Heart failure b. Liver hypoxia d. Renal failure Of the options available, untreated PA is fatal, usually because of heart failure. PTS: 1 REF: Page 989 13. How is the effectiveness of vitamin B12 therapy measured? a. Reticulocyte count c. Hemoglobin b. Serum transferring d. Serum vitamin B12 The effectiveness of cobalamin replacement therapy is determined by a rising reticulocyte count. The other options are not used as indicators of the effectiveness of vitamin B12 therapy PTS: 1 REF: Pages 988-989 14. Which statement about folic acid is false? a. Folic acid absorption is dependent on the enzyme folacin. b. Folic acid is stored in the liver. c. Folic acid is essential for RNA and DNA synthesis within erythrocytes. d. Folic acid is absorbed in the upper small intestine. Folic acid absorption is not dependent on the enzyme folacin. The other options are true statements regarding folic acid. PTS: 1 REF: Page 989 15. Which anemia produces small, pale erythrocytes? a. Folic acid c. Iron deficiency b. Hemolytic d. Pernicious The microcytic-hypochromic anemias, which include iron deficiency anemia (IDA), are characterized by erythrocytes that are abnormally small and contain abnormally reduced amounts of hemoglobin. This description is not true of the other options. NURSINGTB.COM PTS: 1 REF: Pages 989-990 16. Which type of anemia is characterized by fatigue, weakness, and dyspnea, as well as conjunctiva of the eyes and brittle, concave nails? a. Pernicious c. Aplastic b. Iron deficiency d. Hemolytic Early symptoms of iron deficiency anemia (IDA) include fatigue, weakness, and shortness of breath. Pale earlobes, palms, and conjunctivae (see Figure 28-4) are also common signs. Progressive IDA causes more severe alterations, with structural and functional changes apparent in epithelial tissue (see Figure 28-4). The nails become brittle, thin, coarsely ridged, and spoon-shaped or concave (koilonychia) as a result of impaired capillary circulation. The tongue becomes red, sore, and painful. These symptoms are not associated with the other options. PTS: 1 REF: Pages 990-991 17. What is the most common cause of iron deficiency anemia (IDA)? a. Decreased dietary intake c. Vitamin deficiency b. Chronic blood loss d. Autoimmune disease The most common cause of IDA in well-developed countries is pregnancy and chronic blood loss. PTS: 1 REF: Page 990 18. Continued therapy of pernicious anemia (PA) generally lasts how long? a. 6 to 8 weeks c. Until the iron level is normal b. 8 to 12 months d. The rest of one’s life Because PA cannot be cured, maintenance therapy is a life-long endeavor. PTS: 1 REF: Pages 988-989 19. Sideroblastic anemia can occasionally result from an autosomal recessive transmission inherited from which relative? a. Mother c. Grandfather b. Father d. Grandmother An occasional autosomal recessive transmission occurs only with mitochondrial mutations from the mother. PTS: 1 REF: Page 992 20. Clinical manifestations of mild-to-moderate splenomegaly and hepatomegaly, bronze-colored skin, and cardiac dysrhythmias are indicative of which anemia? a. Iron deficiency NURSINGTcB..COSMideroblastic b. Pernicious d. Aplastic Of the options available, only sideroblastic anemia exhibits mild-to-moderate enlargement of the spleen (splenomegaly) and liver (hepatomegaly), as well as abnormal skin pigmentation (bronze colored). Heart rhythm disturbances, along with congestive heart failure, are major life-threatening complications related to cardiac iron overload. PTS: 1 REF: Page 992 21. Considering sideroblastic anemia, what would be the expected effect on the plasma iron levels? a. Plasma iron levels would be high. b. Levels would be low. c. Levels would be normal. d. Levels would be only minimally affected. Plasma iron levels would be high (see Table 28-3). PTS: 1 REF: Page 986 | Table 28-3 22. In aplastic anemia (AA), pancytopenia develops as a result of which of the following? a. Suppression of erythropoietin to produce adequate amounts of erythrocytes b. Suppression of the bone marrow to produce adequate amounts of erythrocytes, leukocytes, and thrombocytes c. Lack of DNA to form sufficient quantities of erythrocytes, leukocytes, and thrombocytes d. Lack of stem cells to form sufficient quantities of leukocytes AA is a critical condition characterized by pancytopenia, which is a reduction or absence of all three blood cell types, resulting from the failure or suppression of bone marrow to produce adequate amounts of blood cells. This selection is the only option that accurately identifies the cause of pancytopenia. PTS: 1 REF: Page 993 23. What is the most common pathophysiologic process that triggers aplastic anemia (AA)? a. Autoimmune disease against hematopoiesis by activated cytotoxic T (Tc) cells b. Malignancy of the bone marrow in which unregulated proliferation of erythrocytes crowd out other blood cells c. Autoimmune disease against hematopoiesis by activated immunoglobulins d. Inherited genetic disorder with recessive X-linked transmission Most cases of AA result from an autoimmune disease directed against hematopoietic stem cells. Tc cells appear to be the main culprits. None of the remaining options is considered a common trigger of AA. PTS: 1 REF: Page 995 NURSINGTB.COM 24. An allogenic bone marrow transplantation remains the preferred method for treating which anemia? a. Polycythemia vera c. Sideroblastic b. Aplastic d. Anemia of chronic disease (ACD) Of the options available, bone marrow and, most recently, peripheral blood stem cell transplantation from a histocompatible sibling are the preferred treatments for the underlying bone marrow failure observed in aplastic anemias. PTS: 1 REF: Page 995 25. Which statement is true regarding warm autoimmune hemolytic anemia? a. Warm autoimmune hemolytic anemia occurs primarily in men. b. It is self-limiting and rarely produces hemolysis. c. Erythrocytes are bound to macrophages and sequestered in the spleen. d. Immunoglobulin M coats erythrocytes and binds them to receptors on monocytes. The immunoglobulin G–coated red blood cells bind to the Fc receptors on monocytes and splenic macrophages and are removed by phagocytosis. The other options are not true when considering this type of anemia. PTS: 1 REF: Page 998 26. When considering hemolytic anemia, which statement is true regarding the occurrence of jaundice? a. Erythrocytes are destroyed in the spleen. b. Heme destruction exceeds the liver’s ability to conjugate and excrete bilirubin. c. The patient has elevations in aspartate transaminase (AST) and alanine transaminase (ALT). d. The erythrocytes are coated with an immunoglobulin. Jaundice (icterus) is present when heme destruction exceeds the liver’s ability to conjugate and excrete bilirubin. This selection is the only option that accurately describes the process that affects the occurrence of hemolytic anemia–related jaundice. PTS: 1 REF: Page 1000 27. Erythrocyte life span of less than 120 days, ineffective bone marrow response to erythropoietin, and altered iron metabolism describe the pathophysiologic characteristics of which type of anemia? a. Aplastic c. Anemia of chronic disease b. Sideroblastic d. Iron deficiency Anemia of chronic disease results from a combination of (1) decreased erythrocyte life span, (2) suppressed production of erythropoietin, (3) ineffective bone marrow erythroid progenitor response to erythropoietin, and (4) altered iron metabolism and iron sequestration in macrophages. This result is not true of the other options. NURSINGTB.COM PTS: 1 REF: Page 1001 28. What is the primary cause of the symptoms of polycythemia vera? a. Decreased erythrocyte count c. Increased blood viscosity b. Destruction of erythrocytes d. Neurologic involvement As polycythemia vera progresses, many of the symptoms are related to the increased blood cellularity and viscosity. No other option is the primary cause of the symptoms of polycythemia vera. PTS: 1 REF: Page 1003 29. Treatment for polycythemia vera involves which of the following? a. Therapeutic phlebotomy and radioactive phosphorus b. Restoration of blood volume by plasma expanders c. Administration of cyanocobalamin d. Blood transfusions In low-risk individuals, the recommended therapy is phlebotomy and low-dose aspirin, whereas radioactive phosphorus has been used to suppress erythropoiesis. The other options are not considered in the treatment of polycythemia vera. PTS: 1 REF: Pages 1003-1004 30. Considering iron replacement therapy prescribed for iron deficiency anemia, who is likely to require long-term daily maintenance dosage? a. A woman who has not yet experienced menopause b. A teenager who is involved in strenuous athletics c. A middle-aged man who smokes two packs of cigarettes a day d. An older person demonstrating signs of dementia Menstruating women may need daily oral iron replacement therapy (325 mg/day) until menopause as a result of their menstrual blood loss. None of the other options are a chronic source of blood loss. PTS: 1 REF: Page 991 31. Which statement is true regarding the physical manifestations of vitamin B12 deficiency anemia? a. Vitamin B12 deficiency anemia seldom results in neurologic symptoms. b. The chances of a cure are good with appropriate treatment. c. The condition is reversible in 75% of the cases. d. Symptoms are a result of demyelination. The neurologic manifestations characteristic of vitamin B12 deficiency anemia result from nerve demyelination that may produce neuronal death. These complications pose a serious threat because they are not reversible, even with appropriate treatment. NURSINGTB.COM PTS: 1 REF: Page 988 MULTIPLE RESPONSE 32. A 2000 ml blood loss will produce which assessment finding? (Select all that apply.) a. Air hunger b. Normal blood pressure in the supine position c. Rapid thready pulse d. Cold clammy skin e. lactic acidosis , C, D With a 2000 ml loss of blood, central venous pressure, cardiac output, and arterial blood pressure are below normal, even when at rest and in the supine position. The person commonly has air hunger; a rapid, thready pulse; and cold, clammy skin. With a 1500 ml loss of blood, supine blood pressure and pulse can still be normal. Lactic acidosis is observed with a blood loss of 2500 ml or more. PTS: 1 REF: Page 996 | Table 28-5 33. Which medications are associated with an intermediate increase in a person’s risk for developing aplastic anemia? (Select all that apply.) a. Penicillin b. Chloramphenicol (Chloromycetin) c. Phenytoin (Dilantin) d. Trimethoprim-sulfamethoxazole (Bactrim) e. Thiazides , C, D Chloramphenicol (Chloromycetin), phenytoin (Dilantin), and trimethoprim-sulfamethoxazole (Bactrim) are associated with an intermediate increase in the risk of developing aplastic anemia. The other options are not associated with a rare increase in risk. PTS: 1 REF: Page 994 | Table 28-4 34. Which conditions are generally included in the symptoms of pernicious anemia (PA)? (Select all that apply.) a. Weakness b. Weight gain c. Low hemoglobin d. Paresthesias e. Low hematocrit , C, D, E When the hemoglobin and hematocrit levels in the blood have significantly decreased, the individual experiences the classic symptoms of PA—weakness, fatigue, paresthesias of the feet and fingers, difficulty in walking, loss of appetite, abdominal pains, and weight loss. PTS: 1 REF: Page 986 | Page 988 | Table 28-3 NURSINGTB.COM 35. What are the clinical manifestations of folate deficiency anemia? (Select all that apply.) a. Constipation b. Flatulence c. Dysphagia d. Stomatitis e. Cheilosis , C, D, E Specific symptoms of folate deficiency anemia include severe cheilosis (scales and fissures of the lips and corners of the mouth), stomatitis (inflammation of the mouth), and painful ulcerations of the buccal mucosa and tongue. Gastrointestinal symptoms may be present and include dysphagia (difficulty swallowing), flatulence, and watery diarrhea. PTS: 1 REF: Page 989 36. Which diseases are commonly associated with anemia of chronic disease? (Select all that apply.) a. Rheumatoid arthritis b. Acquired immunodeficiency syndrome (AIDS) c. Polycythemia vera d. Systemic lupus erythematosus e. Chronic hepatitis , B, D, E AIDS, rheumatoid arthritis, systemic lupus erythematosus, malaria, acute and chronic hepatitis, and chronic renal failure are commonly associated with anemias of chronic disease. Polycythemia vera is not associated with this form of anemia. PTS: 1 REF: Page 1001 MATCHING Match the phrases with the corresponding terms. Options may be used more than once. A. Normocytic-normochromic anemia B. Microcytic-hypochromic anemia C. Macrocytic-normochromic anemia 37. Pernicious anemia 38. Sideroblastic anemia 39. Aplastic anemia 37. ANS: C PTS: 1 REF: Pages 987-988 MSC: Pernicious anemia, a form of macrocytic-normochromic anemia, is caused by vitamin B12 deficiency. 38. ANS: B PTS: 1 REF: Page 989 MSC: The microcytic-hypochromic anemias include sideroblastic anemia. 39. ANS: A PTS: 1 REF: Page 993 MSC: Normocytic-normochromic anemias, including aplastic anemia, are characterized by erythrocytes that are relatively normal in size but with hemoglobin content that is insufficient in number. NURSINGTB.COM Chapter 30: Alterations of Leukocyte, Lymphoid Function MULTIPLE CHOICE 1. What change is observed in leukocytes during an allergic disorder (type I hypersensitivity) often caused by asthma, hay fever, and drug reactions? a. Neutrophilia c. Eosinophilia b. Basophilia d. Monocytosis Eosinophilia is an absolute increase (more than 450/µL) in the total numbers of circulating eosinophils. Allergic disorders (type I hypersensitivity) associated with asthma, hay fever, and drug reactions, as well as parasitic infections (particularly with metazoal parasites), are often cited as causes. This change is not identified by any of other options. PTS: 1 REF: Pages 1010-1011 2. In infectious mononucleosis (IM), what does the Monospot test detect? a. Immunoglobulin E (IgE) c. Immunoglobulin G (IgG) b. Immunoglobulin M (IgM) d. Immunoglobulin A (IgA) Heterophile antibodies are a heterogeneous group of IgM antibodies that are agglutinins against nonhuman red blood cells (e.g., sheep, horse) and are detected by qualitative (monospot) or quantitative (heterophile antibody) test methods. This statement is not true of the other options. NURSINGTB.COM PTS: 1 REF: Pages 1012-1013 3. Which description is consistent with acute lymphocytic leukemia (ALL)? a. ALL is a progressive neoplasm defined by the presence of greater than 30% lymphoblasts in the bone marrow or blood. b. Leukocytosis and a predominance of blast cells characterize the bone marrow and peripheral blood. As the immature blasts increase, they replace normal myelocytic cells, megakaryocytes, and erythrocytes. c. B cells fail to mature into plasma cells that synthesize immunoglobulins. d. The translocation of genetic material from genes 9 and 22 create an abnormal, fused gene identified as BCR-ABL. ALL is a progressive neoplasm defined by the presence of greater than 30% lymphoblasts in the bone marrow or blood. None of the other options provide an accurate description of ALL. PTS: 1 REF: Page 1016 4. Which description is consistent with chronic myelogenous leukemia (CML)? a. Defects exist in the ras oncogene, TP53 tumor-suppressor gene, and INK4A, the gene encoding a cell-cycle regulatory protein. b. Leukocytosis and a predominance of blast cells characterize the bone marrow and peripheral blood. As the immature blasts increase, they replace normal myelocytic cells, megakaryocytes, and erythrocytes. c. B cells fail to mature into plasma cells that synthesize immunoglobulins. d. The translocation of genetic material from genes 9 and 22 creates an abnormal, fused protein identified as BCR-ABL1. The Philadelphia chromosome is present in more than 95% of those with CML, and the presence of the BCR-ABL1 protein is responsible for the initiation of CML. The other options do not accurately describe CML. PTS: 1 REF: Pages 1014-1015 | Page 1021 5. Which description is consistent with chronic lymphocytic leukemia (CLL)? a. Defects exist in the ras oncogene, TP53 tumor-suppressor gene, and INK4A, the gene encoding a cell-cycle regulatory protein. b. Leukocytosis and a predominance of blast cells characterize the bone marrow and peripheral blood. As the immature blasts increase, they replace normal myelocytic cells, megakaryocytes, and erythrocytes. c. B cells fail to mature into plasma cells that synthesize immunoglobulins. d. The translocation of genetic material from genes 9 and 22 creates an abnormal, fused protein identified as BCR-ABL. CLL is derived from transformation of a partially mature B cell that has not yet encountered antigen. The other options do not accurately describe CLL. PTS: 1 REF: Pages 1N0U20R-S1I0N2G1TB.COM 6. Which electrolyte imbalance accompanies multiple myeloma (MM)? a. Hyperkalemia c. Hyperphosphatemia b. Hypercalcemia d. Hypernatremia Elevated levels of calcium in the blood (hypercalcemia) characterize the common presentation of MM. The other options do not accompany MM. PTS: 1 REF: Page 1032 7. Reed-Sternberg (RS) cells represent malignant transformation and proliferation of which of the following? a. Interleukin (IL)–1, IL-2, IL-5, and IL-6 b. Tumor necrosis factor–beta c. B cells d. T cells ANS: C Although the molecular events that cause malignant transformation remain controversial, RS cells are apparently from B-cell lineage. The other options are not relevant to this process. PTS: 1 REF: Pages 1024-1025 8. Local signs and symptoms of Hodgkin disease–related lymphadenopathy are a result of which of the following? a. Pressure and ischemia c. Inflammation and ischemia b. Pressure and obstruction d. Inflammation and pressure Local symptoms caused by pressure and obstruction of the lymph nodes are the result of lymphadenopathy. The other options do not contribute to the lymphadenopathy associated with Hodgkin disease. PTS: 1 REF: Page 1025 9. Which virus is associated with Burkitt lymphoma in African children? a. Cytomegalovirus c. Human papillomavirus b. Adenovirus d. Epstein-Barr virus Epstein-Barr virus, found in nasopharyngeal secretions, is associated with Burkitt lymphoma in African children. The other options are not associated with this malignancy. PTS: 1 REF: Page 1029 10. Which term is used to describe a red-purple discoloration caused by diffuse hemorrhage into the skin tissue? a. Petechiae c. Ecchymosis b. Hematoma d. Purpura NURSINGTB.COM Diffuse hemorrhage into skin tissues that is visible through the skin causes a red-purple discoloration identified as a purpura. None of the other options are used to identify this symptom. PTS: 1 REF: Page 1037 11. Which statement best describes heparin-induced thrombocytopenia (HIT)? a. Immunoglobulin G immune–mediated adverse drug reaction that reduces circulating platelets b. Hematologic reaction to heparin in which the bone marrow is unable to produce sufficient platelets to meet the body’s needs c. Immunoglobulin E–mediated allergic drug reaction that reduces circulating platelets d. Cell-mediated drug reaction in which macrophages process the heparin and platelet complexes that are then destroyed by activated cytotoxic T cells. Heparin is a common cause of drug-induced thrombocytopenia. HIT is an immune-mediated, adverse drug reaction caused by immunoglobulin G antibodies that leads to increased platelet consumption and a decrease in platelet counts. None of the other options accurately describe HIT. PTS: 1 REF: Page 1038 12. Immune thrombocytopenia (ITP) is a(n) condition in adults and a(n) condition in children. a. Acute; acute c. Acute; chronic b. Chronic; chronic d. Chronic; acute ITP may be acute or chronic. The acute form is frequently observed in children. Chronic ITP is more commonly observed in adults, with the highest prevalence in women between 20 and 40 years of age. PTS: 1 REF: Pages 1038-1039 13. Vitamin is required for normal clotting factor synthesis by the . a. K; kidneys c. K; liver b. D; kidneys d. D; liver Vitamin K, a fat-soluble vitamin, is necessary for the synthesis and regulation of prothrombin, procoagulant factors (VII, IX, X), and anticoagulant regulators (proteins C and S) in the liver. PTS: 1 REF: Pages 1042-1043 14. What is the most common cause of vitamin K deficiency? a. Administration of warfarin (Coumadin) b. Total parenteral nutrition with antibiotic therapy c. An immunoglobulin G–mediaNteUdRaSuINtoGimTBm.CuOneMdisorder d. Liver failure The most common cause of vitamin K deficiency is parenteral nutrition in combination with broad-spectrum antibiotics that destroy normal gut flora. None of the other options are commonly associated with vitamin K deficiency. PTS: 1 REF: Page 1043 15. Which disorder is described as an unregulated release of thrombin with subsequent fibrin formation and accelerated fibrinolysis? a. Disseminated intravascular coagulation (DIC) b. Immune thrombocytopenic purpura (ITP) c. Heparin-induced thrombocytopenia (HIT) d. Essential thrombocythemia (ET) DIC is an acquired clinical syndrome characterized by widespread activation of coagulation resulting in the formation of fibrin clots in medium and small vessels throughout the body. This description does not accurately identify any of the other options. PTS: 1 REF: Page 1043 16. In disseminated intravascular coagulation (DIC), what activates the coagulation cascade? a. Cytokines, such as platelet-activating factor (PAF), and tumor necrosis factor- alpha (TNF-) b. Thromboxane A, causing platelets to aggregate and consume clotting factors c. Tissue factor (TF) located in the endothelial layer of blood vessels and subcutaneous tissue d. Endotoxins from gram-negative and gram-positive bacteria circulating in the bloodstream Direct tissue damage (ischemia and necrosis, surgical manipulation, crushing injury) causes the endothelium to release TF. The common pathway for DIC appears to be excessive and widespread exposure of TF. The other options are not responsible for the activation of the coagulation cascade. PTS: 1 REF: Pages 1043-1044 17. Which proinflammatory cytokines are responsible for the development and maintenance of disseminated intravascular coagulation (DIC)? a. Granulocyte colony-stimulating factor (G-CSF); interleukin (IL)–2, IL-4, and IL-10; and tumor necrosis factor-gamma (IFN-) b. Granulocyte-macrophage colony-stimulating factor (GM-CSF); and IL-3, IL-5, IL-9, and IFN- c. Macrophage colony-stimulating factor (M-CSF); IL-7, IL-11, and IL-14; and PAF d. Tumor necrosis factor-alpha (TNF-); IL-1, IL-6, and IL-8; and platelet-activating factor (PAF) NURSINGTB.COM Endotoxin, in particular, triggers the release of multiple cytokines that play a significant role in the development and maintenance of DIC. Proinflammatory cytokines—TNF-; IL-1, IL-6, IL-8; PAF—are responsible for the clinical signs and symptoms associated with the sepsis associated with DIC. None of the other options perform this function. PTS: 1 REF: Page 1044 18. In disseminated intravascular coagulation (DIC), what are the indications of microvascular thrombosis? a. Reduced amplitude in peripheral pulses b. Symmetric cyanosis of fingers and toes c. Numbness and tingling in fingers and toes d. Bilateral pallor and edema of fingers and toes Several organ systems are susceptible to microvascular thrombosis that affects their function. Indicators of multisystem failure include changes in the level of consciousness, behavior, and mentation; confusion; seizure activity; oliguria; hematuria; hypoxia; hypotension; hemoptysis; chest pain; and tachycardia. Symmetric cyanosis of the fingers and toes (i.e., “blue finger/toe syndrome”) and, in some instances, of the nose and breasts may be present. The other options are not recognized indicators of microvascular thrombosis. PTS: 1 REF: Page 1046 19. What is the most reliable and specific test for diagnosing disseminated intravascular coagulation (DIC)? a. Prothrombin time (PT) b. Activated partial thromboplastin time (aPTT) c. Fibrin degradation products (FDP) d. D-dimer D-dimer testing measures a specific DIC-related product. This statement is not true of the other options. PTS: 1 REF: Page 1047 20. What term is used to identify thrombi that occlude arterioles and capillaries and are made up of platelets with minimal fibrin and erythrocytes? a. Essential (primary) thrombocythemia (ET) b. Acute idiopathic thrombotic thrombocytopenic purpura c. Thrombotic thrombocytopenic purpura (TTP) d. Immune thrombocytopenic purpura (ITP) Of the available options, only TTP is characterized by thrombotic microangiopathy in which platelets aggregate and cause occlusion of arterioles and capillaries in the microcirculation. PTS: 1 REF: Page 1040 NURSINGTB.COM 21. Which of the following is characterized by what is referred to as pathognomonic pentad of symptoms? a. Acute idiopathic thrombotic thrombocytopenic purpura b. Essential (primary) thrombocythemia (ET) c. Immune thrombocytopenic purpura (ITP) d. Thrombotic thrombocytopenic purpura (TTP) Acute idiopathic thrombotic thrombocytopenic purpura is characterized by a pathognomonic pentad of symptoms that includes extreme thrombocytopenia (fewer than 20,000 platelets/mm3), intravascular hemolytic anemia, ischemic signs and symptoms most often involving the central nervous system (approximately 65% exhibit memory disturbances, behavioral irregularities, headaches, or coma), kidney failure (affecting approximately 65% of individuals), and fever (present in approximately 33% of individuals The other options do not demonstrate these symptoms. PTS: 1 REF: Page 1040 22. Which statement relates to immune thrombocytopenic purpura (ITP)? a. ITP is formed in conditions of low flow and is made up of mostly red cells with larger amounts of fibrin and few platelets. b. An alteration of multipotent stem cells, resulting in an excess production of platelets, causes ITP. c. Mononuclear phagocytes in the spleen remove antibody-coated platelets from circulation. d. Arterial clots are made up of mostly platelet aggregates held together by fibrin strands. ITP involves the antigen usually forming immune complexes with circulating antibodies, and it is thought that the immune complexes bind to Fc receptors on platelets, leading to their destruction in the spleen. None of the other options are accurately related to ITP. PTS: 1 REF: Pages 1038-1039 23. When the demand for mature neutrophils exceeds the supply, immature neutrophils are released indicating: a. A shift to the right c. Leukocytosis b. A shift to the left d. Leukemia When the demand for circulating mature neutrophils exceeds the supply, the marrow begins to release immature neutrophils (and other leukocytes) into the blood. Premature release of the immature white cells is responsible for the phenomenon known as a shift to the left or leukemoid reaction. None of the remaining options would be used to identify the process described. PTS: 1 REF: Page 1009 24. Hodgkin disease is characterized by the presence of which of the following? a. Philadelphia chromosome NURSINGTcB..COMMicrovascular thrombi b. Virchow triad d. Reed-Sternberg (RS) cells Hodgkin disease is characterized by its progression from one group of lymph nodes to another, the development of systemic symptoms, and the presence of RS cells (see Figure 29-8), but not the involvement of the Philadelphia chromosome. Virchow triad is a symptom related to thrombus formation. Disseminated intravascular coagulation is associated with microvascular thrombi. PTS: 1 REF: Page 1024 MULTIPLE RESPONSE 25. Which classic clinical manifestations are symptoms of IM? (Select all that apply.) a. Lymph node enlargement b. Hepatitis c. Pharyngitis d. Edema in the area of the eyes e. Fever , C, E At the time of diagnosis, the individual usually has the classic triad of symptoms: fever, pharyngitis, and lymphadenopathy of the cervical lymph nodes. The triad does not include hepatitis or orbital edema. PTS: 1 REF: Page 1012 26. Early detection of acute leukemia would include which of the following symptoms? (Select all that apply.) a. Dizziness b. Paresthesia c. Anorexia d. Bruising e. Bone pain , D, E Signs and symptoms related to bone marrow depression include fatigue caused by anemia, bleeding resulting from thrombocytopenia (reduced numbers of circulating platelets), and fever caused by infection. Anorexia can occur in all varieties of acute leukemia and is associated with weight loss. Pain in the bones and joints is thought to result from leukemia infiltration with secondary stretching of the periosteum. The other options are not generally associated with acute leukemia. PTS: 1 REF: Page 1017 | Page 1019 27. What are the most significant risk factors for the development of thrombus formation as referred to by the Virchow triad? (Select all that apply.) a. Endothelial injury to blood vessels b. Turbulent arterial blood flow NURSINGTB.COM c. Rapid coagulation of the blood d. Stagnant venous blood flow e. History of obesity , B, C, D The risk for developing spontaneous thrombi is related to several factors, referred to as the Virchow triad: (1) injury to the blood vessel endothelium, (2) abnormalities of blood flow, and (3) hypercoagulability of the blood. Obesity is not associated with the triad. PTS: 1 REF: Pages 1048-1049 28. Which statements are true regarding leukemias? (Select all that apply.) a. A single progenitor cell undergoes a malignant change. b. Leukemia is a result of uncontrolled cellular proliferation. c. Bone marrow becomes overcrowded. d. Leukocytes are under produced. e. Hematopoietic cell production is decreased. , B, C, E In the leukemias, a single progenitor cell undergoes malignant transformation. The common feature of all forms of leukemia is an uncontrolled proliferation of malignant leukocytes, causing an overcrowding of bone marrow and decreased production and function of normal hematopoietic cells. PTS: 1 REF: Page 1015 29. The two major forms of leukemia, acute and chronic, are classified by which criteria? (Select all that apply.) a. Predominant cell type b. Rate of progression c. Age of individual when cells differentiation occurs d. Stage of cell development when malignancy first occurs e. Serum level of leukocytes , B The current classification of leukemia is based on (1) the predominant cell of origin (either myeloid or lymphoid) and (2) the rate of progression, which usually reflects the degree at which cell differentiation was arrested when the cell became malignant (acute or chronic) (see Figure 29-2). The remaining options are inaccurate statements regarding the classification criteria. PTS: 1 REF: Page 1013 30. What are the clinical manifestations of advanced non-African Burkitt lymphoma? (Select all that apply.) a. Abdominal swelling b. Night sweats c. Fever d. Weight gain e. Dementia , B, C NURSINGTB.COM In non-African Burkitt lymphoma, the most common presentation is abdominal swelling. More advanced disease may exhibit night sweats, fever, and weight loss. Dementia is not associated with this disease. PTS: 1 REF: Page 1029 MATCHING Match the causes or diagnostic tests with the hematologic disorders. A. Epstein-Barr virus B. Bence Jones protein C. Diagnosed by the Reed-Sternberg cell D. Diagnosed by the Philadelphia chromosome 31. Infectious mononucleosis 32. Chronic myelogenous leukemia 33. Multiple myeloma 34. Hodgkin lymphoma 31. ANS: A PTS: 1 REF: Page 1011 MSC: The most common etiologic agent is Epstein-Barr virus, a ubiquitous, lymphotrophic, gamma-group herpesvirus. 32. ANS: D PTS: 1 REF: Pages 1014-1015 MSC: The Philadelphia chromosome is present in more than 95% of patients with chronic myelogenous leukemia. 33. ANS: B PTS: 1 REF: Page 1032 MSC: The myeloma may produce free immunoglobulin light chain (Bence Jones protein) that is present in the blood and urine in approximately 80% of patients. 34. ANS: C PTS: 1 REF: Page 1024 MSC: Hodgkin lymphoma is characterized by its progression from one group of lymph nodes to another, the development of systemic symptoms, and the presence of Reed-Sternberg cells NURSINGTB.COM Chapter 31: Alterations of Hematologic Function in Children MULTIPLE CHOICE 1. What is the cause of polycythemia in the fetus? a. Fetal hemoglobin has a greater affinity for oxygen as a result of diphosphoglycerate (DPG). b. The fetus has a different hemoglobin structure of two - and two -chains rather than two -and two -chains. c. Increased erythropoiesis occurs in response to the hypoxic intrauterine environment. d. The lungs of the fetus are undeveloped and unable to diffuse oxygen adequately to the pulmonary capillaries. The hypoxic intrauterine environment stimulates erythropoietin production in the fetus. This selection is the only option that accurately explains why the fetus develops polycythemia. PTS: 1 REF: Page 1057 2. Why does fetal hemoglobin have a greater affinity for oxygen than adult hemoglobin? a. The fetus does not have its own oxygen supply and must rely on oxygen from the maternal vascular system. b. The fetus has two -chains on the hemoglobin, rather than two -chains as in the adult. NURSINGTB.COM c. Fetal hemoglobin interacts less readily with diphosphoglycerate (DPG), which inhibits hemoglobin-oxygen binding. d. Fetal hemoglobin production occurs in the vessels and liver rather than in the bone marrow as in the adult. Fetal hemoglobin has greater affinity for oxygen than does adult hemoglobin because it interacts less readily with the enzyme, DPG, which inhibits hemoglobin-oxygen binding. This selection is the only option that accurately explains why fetal hemoglobin has a greater affinity for oxygen than adult hemoglobin. PTS: 1 REF: Page 1056 3. Which blood cell type is elevated at birth but decreases to adult levels during the first year of life? a. Monocytes c. Neutrophils b. Platelets d. Lymphocytes Only monocyte counts are high in the first year of life and then decrease to adult levels. PTS: 1 REF: Page 1057 4. In a full-term infant, the normal erythrocyte life span is days, whereas the adult erythrocyte life span is _ days. a. 30 to 50; 80 c. 90 to 110; 140 b. 60 to 80; 120 d. 120 to 130; 150 In full-term infants, normal erythrocyte life span is 60 to 80 days; in premature infants it may be as short as 20 to 30 days; and in children and adolescents, it is 120 days, the same as that in adults. PTS: 1 REF: Page 1057 5. What is the most common cause of insufficient erythropoiesis in children? a. Folic acid deficiency c. Hemoglobin abnormality b. Iron deficiency d. Erythrocyte abnormality Similar to the anemias of adulthood, ineffective erythropoiesis or premature destruction of erythrocytes causes the anemias of childhood. The most common cause of insufficient erythropoiesis is iron deficiency. The other options may be causes but are not common ones. PTS: 1 REF: Page 1058 6. How does hemolytic disease of the newborn (HDN) cause acquired congenital hemolytic anemia? a. HDN develops when hypoxia or dehydration causes the erythrocytes to change shapes, which are then recognNizUeRdSaIsNfGoTrBei.gCnOMand removed from circulation. b. HDN is an alloimmune disease in which the mother’s immune system produces antibodies against fetal erythrocytes, which are recognized as foreign and removed from circulation. c. HDN develops when the polycythemia present in fetal life continues after birth, causing the excessive number of erythrocytes to be removed from circulation. d. HDN is an autoimmune disease in which the fetus’s immune system produces antibodies against fetal erythrocytes, which are recognized as foreign and removed from circulation. HDN is an alloimmune disease in which maternal blood and fetal blood are antigenically incompatible, causing the mother’s immune system to produce antibodies against fetal erythrocytes. Fetal erythrocytes that have been attacked by (or bound to) maternal antibodies are recognized as foreign or defective by the fetal mononuclear phagocyte system and are removed from the circulation by phagocytosis, usually in the fetal spleen. This selection is the only option that accurately explains how HDN causes acquired congenital hemolytic anemia. PTS: 1 REF: Page 1058 7. Erythroblastosis fetalis is defined as an: a. Allergic disease in which maternal blood and fetal blood are antigenically incompatible b. Alloimmune disease in which maternal blood and fetal blood are antigenically incompatible c. Autoimmune disease in immature nucleated cells that are released into the bloodstream d. Autosomal dominant hereditary disease Erythroblastosis fetalis, also known as hemolytic disease of the newborn (HDN), is an alloimmune disease in which maternal blood and fetal blood are antigenically incompatible, causing the mother’s immune system to produce antibodies against fetal erythrocytes. This selection is the only option that accurately defines erythroblastosis fetalis. PTS: 1 REF: Page 1058 8. An infant’s hemoglobin must fall below g/dl before signs of pallor, tachycardia, and systolic murmurs occur. a. 11 c. 7 b. 9 d. 5 When the hemoglobin falls below 5 g/dl, pallor, tachycardia, and systolic murmurs may occur. PTS: 1 REF: Page 1059 9. Which vitamin improves the absorption of oral iron taken to treat iron deficiency anemia in children? NURSINGTB.COM a. A c. C b. B d. E Of the available options, only additional vitamin C may be used to promote iron absorption. PTS: 1 REF: Page 1059 10. Hemolytic disease of the newborn (HDN) can occur if the mother: a. Is Rh-positive and the fetus is Rh-negative b. Is Rh-negative and the fetus is Rh-positive c. Has type A blood and the fetus has type O d. Has type AB blood and the fetus has type B HDN can occur only if antigens on fetal erythrocytes differ from antigens on maternal erythrocytes. Maternal-fetal incompatibility exists only if the mother and fetus differ in ABO blood type or if the fetus is Rh-positive and the mother is Rh-negative. This erythrocyte incompatibility does not exist in any of the other options. PTS: 1 REF: Page 1059 11. When diagnosed with hemolytic disease of the newborn (HDN), why does the newborn develop hyperbilirubinemia after birth but not in utero? a. Excretion of unconjugated bilirubin through the placenta into the mother’s circulation is no longer possible. b. Hemoglobin does not break down into bilirubin in the intrauterine environment. c. The liver of the fetus is too immature to conjugate bilirubin from a lipid-soluble to water-soluble form. d. The destruction of erythrocytes producing bilirubin is greater after birth. Hyperbilirubinemia occurs in the neonate after birth because excretion of lipid-soluble unconjugated bilirubin through the placenta is no longer possible. This selection is the only option that accurately explains why HDN causes hyperbilirubinemia after birth but not in utero. PTS: 1 REF: Page 1060 12. Fetuses who do not survive anemia in utero are usually stillborn with gross edema of the entire body. Which term is used to identify this condition? a. Spherocytosis c. Erythroblastosis fetalis b. Icterus gravis neonatorum d. Hydrops fetalis Fetuses that do not survive anemia in utero are usually stillborn with gross edema in the entire body, a condition called hydrops fetalis. This selection is the only option that accurately identifies the condition with these specific symptoms. PTS: 1 REF: Page 10N6U0RSINGTB.COM 13. What is the name of the disorder in which levels of bilirubin remain excessively high in the newborn and are deposited in the brain? a. Kernicterus c. Jaundice b. Icterus neonatorum d. Icterus gravis neonatorum Without replacement transfusions, during which the child receives Rh-negative erythrocytes, the bilirubin is deposited in the brain, a condition called kernicterus. This selection is the only option that accurately identifies the condition with the provided symptoms. PTS: 1 REF: Page 1060 14. What treatment prevents the development of kernicterus in an infant born with hemolytic disease of the newborn (HDN)? a. Administration of intravenous fluids to dilute the blood b. Replacement transfusion of new Rh-positive blood that is not contaminated with anti-Rh antibodies c. Performance of a splenectomy to prevent the destruction of abnormal erythrocytes d. Replacement transfusion of Rh-negative erythrocytes If antigenic incompatibility of the mother’s erythrocytes is not discovered in time to administer Rh immunoglobulin and the child is born with HDN, then the treatment consists of exchange transfusions in which the neonate’s blood is replaced with new Rh-positive blood that is not contaminated with anti-Rh antibodies. This treatment is administered during the first 24 hours of extrauterine life to prevent kernicterus. This selection is the only option that accurately prevents kernicterus. PTS: 1 REF: Page 1061 15. Glucose 6-phosphate dehydrogenase (G6PD) deficiency is what type of inherited disorder? a. X-linked dominant c. Autosomal dominant b. X-linked recessive d. Autosomal recessive G6PD deficiency is an inherited, X-linked recessive disorder. This selection is the only option that accurately identifies the mode of inheritance for the stated disorder. PTS: 1 REF: Page 1062 16. Sickle cell disease is classified as a(an): a. Inherited X-linked recessive disorder b. Inherited autosomal recessive disorder c. Disorder initiated by hypoxemia and acidosis d. Disorder that is diagnosed equally in men and women Sickling is an occasional, intermittent phenomenon that can be triggered or sustained by one or more of the following stresNsoUrRsS: IdNeGcrTeBa.sCeOdMoxygen tension (PO2) of the blood (hypoxemia), increased hydrogen ion concentration in the blood (decreased pH), increased plasma osmolality, decreased plasma volume, and low temperature (see Figure 30-7). This selection is the only option that accurately identifies the classification of the stated disorders. PTS: 1 REF: Page 1062 | Page 1065 17. Hemoglobin S (HbS) is formed in sickle cell disease as a result of which process? a. Deficiency in glucose 6-phosphate dehydrogenase (G6PD) that changes hemoglobin A (HbA) to HbS. b. Genetic mutation in which two amino acids (histidine and leucine) are missing. c. Genetic mutation in which one amino acid (valine) is replaced by another (glutamic acid). d. Autoimmune response in which one amino acid (proline) is detected as an antigen by abnormal immunoglobulin G (IgG). HbS is formed by a genetic mutation in which one amino acid (valine) replaces another (glutamic acid) (see Figure 30-5, A). This selection is the only option that accurately identifies how HbS is formed in sickle cell disease. PTS: 1 REF: Page 1063 18. Sickle cell disease (SCD) is what type of inherited disorder? a. Autosomal dominant c. X-linked dominant b. Autosomal recessive d. X-linked recessive SCD is an inherited autosomal recessive disorder that is expressed as sickle cell anemia, sickle cell–thalassemia disease, or sickle cell–hemoglobin C (HbC) disease, depending on mode of inheritance. This selection is the only option that accurately identifies the mode of inheritance for the stated disorder. PTS: 1 REF: Page 1063 19. What is the reason most children diagnosed with sickle cell anemia are not candidates for either bone marrow or stem cell transplants? a. Well-matched stem cell donors are difficult to find. b. The child is usually too weak to survive the procedure. c. The child’s immune system will not appropriately respond to the antirejection medications. d. Although effective for adults, neither procedure has been proven effective for children. Bone marrow or stem cell transplants can cure sickle cell anemia. However, the only reason these procedures are not currently an option for most children is because well-matched stem cell donors are often difficult to find. PTS: 1 REF: Page 1063 20. Which manifestations of vasoocclNuUsiRvSeIcNrGisTisB.aCrOeMassociated with sickle cell disease (SCD) in infants? a. Atelectasis and pneumonia b. Edema of the hands and feet c. Stasis ulcers of the hands, ankles, and feet d. Splenomegaly and hepatomegaly Symmetric, painful swelling of the hands and feet (hand-foot syndrome) caused by infarction in the small vessels of the extremities is often the initial manifestation of SCD in infants. This selection is the only option that accurately identifies the manifestations of a vasoocclusive crisis associated with SCD in infancy. PTS: 1 REF: Page 1066 21. What is the chance with each pregnancy that a child born to two parents with the sickle trait will have sickle cell disease (SCD)? a. 20% c. 33% b. 25% d. 50% A 25% chance exists with each pregnancy that a child born to two parents with sickle cell trait will have SCD. Genetic counseling enables people with SCD or with the sickle cell trait to make informed decisions about transmitting this genetic disorder to their offspring. PTS: 1 REF: Pages 1068-1069 22. Which type of anemia occurs as a result of thalassemia? a. Microcytic, hypochromic c. Macrocytic, hyperchromic b. Microcytic, normochromic d. Macrocytic, normochromic The only option that identifies the anemic manifestation of thalassemia is microcytic-hypochromic hemolytic anemia. PTS: 1 REF: Page 1069 23. What is the fundamental defect that results in beta-thalassemia major? a. The spleen prematurely destroys the precipitate-carrying cells. b. A severe uncoupling of - and -chain synthesis occurs. c. All four beta-forming genes are defective. d. Hemoglobin H (HbH) develops when three genes are defective. The fundamental defect in beta-thalassemia is the uncoupling of - and -chain synthesis. -Chain production is moderately depressed in the heterozygous form—beta-thalassemia minor, and severely depressed in the homozygous form—beta-thalassemia major (also called Cooley anemia). The defects described in the other options are not related to beta-thalassemia major. PTS: 1 REF: Page 1069 24. The alpha- and beta-thalassemias NarUeRcSoINnsGidTeBr.eCdOMwhat types of inherited disorder? a. Autosomal recessive c. X-linked recessive b. Autosomal dominant d. X-linked dominant The alpha- and beta-thalassemias are inherited autosomal recessive disorders. This selection is the only option that correctly identifies how these disorders are inherited. PTS: 1 REF: Page 1069 25. Hemophilia B is caused by a deficiency of which clotting factor? a. V c. IX b. VIII d. X Only factor IX deficiency causes hemophilia B (Christmas disease). PTS: 1 REF: Page 1071 26. Hemophilia A is considered to be what type of inherited disorder? a. Autosomal dominant c. X-linked recessive b. Autosomal recessive d. X-linked dominant Hemophilia A (classic hemophilia) is inherited as an X-linked recessive disorder. This selection is the only option that correctly identifies how this disorder is inherited. PTS: 1 REF: Page 1071 27. Which disease is an autosomal dominant inherited hemorrhagic disease? a. Hemophilia A c. Christmas disease b. von Willebrand disease d. Hemophilia B The bleeding disorder, von Willebrand disease, results only from an inherited autosomal dominant trait. PTS: 1 REF: Page 1071 28. Idiopathic thrombocytopenic purpura (ITP) is an autoimmune process involving antibodies attacking which type of cells? a. Neutrophils c. Platelets b. Eosinophils d. Basophils ITP is a disorder of platelet consumption. This selection is the only option that correctly identifies which type of cell is attacked by ITP. PTS: 1 REF: Page 1073 29. Which disorder results in decreased erythrocytes and platelets with changes in leukocytes and has clinical manifestations of pallor, fatigue, petechiae, purpura, bleeding, and fever? a. Idiopathic thrombocytopenic purpura (ITP) b. Acute lymphocytic leukemia (NAULRLS)INGTB.COM c. Non-Hodgkin lymphoma (NHL) d. Iron deficiency anemia (IDA) Pallor, fatigue, petechiae, purpura, bleeding, and fever are generally present with the most common symptoms reflecting the consequence of bone marrow failure, which results in decreased red blood cells and platelets and changes in white blood cells. This selection is the only option that correctly identifies the disease with the symptoms described. PTS: 1 REF: Page 1076 30. When does fetal erythrocyte production shift from the liver to the bone marrow? a. Fourth month of gestation c. Eighth month of gestation b. Fifth month of gestation d. At birth By the fifth month of gestation, hematopoiesis begins to occur in the bone marrow and increases rapidly until hematopoietic (red) marrow fills the entire bone marrow space. By the time of delivery, the bone marrow is the only significant site of hematopoiesis. PTS: 1 REF: Pages 1055-1056 31. Which disease is caused by clotting factor VIII deficiency and is an autosomal dominant trait? a. Hemophilia A c. Hemophilia C b. Hemophilia B d. von Willebrand disease Of the options available, only von Willebrand disease is caused by factor VIII deficiency and is the result of an inherited autosomal dominant trait. PTS: 1 REF: Page 1071 32. Which type of hemophilia affects only men? a. Hemophilia A c. Hemophilia C b. Hemophilia B d. von Willebrand disease Of the options available, only hemophilia A (classic hemophilia) is caused by factor VIII deficiency and is inherited as an X-linked recessive disorder that affects men and is transmitted by women. PTS: 1 REF: Page 1071 33. Which hemophilia occurs equally in both men and women? a. Hemophilia A c. Hemophilia C b. Hemophilia B d. von Willebrand disease Of the options available, only hemophilia C (factor XI deficiency) occurs as an autosomal recessive disease while occurring equally in men and women. PTS: 1 REF: Page 10N7U1RSINGTB.COM 34. During childhood, when is dietary iron deficiency commonly diagnosed? a. Between 2 months and 1 year c. Between 12 months and 3 years b. Between 6 months and 2 years d. Between 18 months and 4 years Iron deficiency anemia is the most common blood disorder of infancy and childhood, with the highest incidence occurring between 6 months and 2 years of age. PTS: 1 REF: Page 1059 35. What is the significance of hyperdiploidy when diagnosing and treating leukemia? a. Hyperdiploidy indicates a good prognosis. b. Hyperdiploidy indicates a poor prognosis. c. Hyperdiploidy indicates poor response to a specific treatment. d. Hyperdiploidy indicates the achievement of remission. Hyperdiploidy (increased number of chromosome copies) is associated with a good prognosis. The other options are incorrect regarding the significance of hyperdiploidy. PTS: 1 REF: Page 1075 MULTIPLE RESPONSE 36. What are the common triggers for sickle cell crisis? (Select all that apply.) a. Fever b. Infection c. Dehydration d. Alkalosis e. Exposure to the cold , B, C, E Crises can be prevented by avoiding fever, infection, acidosis, dehydration, constricting clothes, and exposure to cold. PTS: 1 REF: Page 1068 MATCHING Match each sickle cell crisis with its description. Terms may be used more than once. A. Vasoocclusive crisis B. Aplastic crisis C. Sequestration crisis D. Hyperhemolytic crisis 37. Large amounts of blood become acutely pooled in the liver and spleen. 38. Blood flow is impaired by tangled masses of rigid, sickled cells. 39. Crisis occurs in association with certain drugs or infection. 40. Compensatory erythropoiesis is coNmUpRrSoINmGisTeBd.,CtOhMus limiting the number of erythrocytes that are replaced. 37. ANS: C PTS: 1 REF: Page 1066 MSC: In sequestration crisis, large amounts of blood become acutely pooled in the liver and spleen. 38. ANS: A PTS: 1 REF: Page 1066 MSC: Vasoocclusive crisis (thrombotic crisis) begins with sickling in the microcirculation. As blood flow is obstructed by tangled masses of rigid, sickled cells, vasospasm occurs and a log jam effect brings all blood flow through the vessel to a halt. 39. ANS: D PTS: 1 REF: Page 1066 40. ANS: B PTS: 1 REF: Page 1066 MSC: Aplastic crisis, a transient cessation in red blood cell production that results in acute anemia, occurs as a result of a viral infection. The virus causes a temporary shutdown of red blood cell production in the bone marrow, or reticulocytosis. Chapter 32: Structure and Function of the Cardiovascular and Lymphatic Systems MULTIPLE CHOICE 1. Which statement does not accurately describe the pericardium? a. The pericardium is a double-walled membranous sac that encloses the heart. b. It is made up of connective tissue and a surface layer of squamous cells. c. The pericardium protects the heart against infection and inflammation from the lungs and pleural space. d. It contains pain and mechanoreceptors that can elicit reflex changes in blood pressure and heart rate. The pericardium is made up of a surface layer of mesothelium over a thin layer of connective tissue. The remaining options accurately describe the pericardium. PTS: 1 REF: Page 1085 2. Which cardiac chamber has the thinnest wall and why? a. The right and left atria; they are low-pressure chambers that serve as storage units and conduits for blood. b. The right and left atria; they are not directly involved in the preload, contractility, or afterload of the heart. c. The left ventricle; the mean pressure of blood coming into this ventricle is from the lung, which has a low pressure. d. The right ventricle; it pumps bNloUoRdSIiNntGoTtBh.eCOpuMlmonary capillaries, which have a lower pressure compared with the systemic circulation. The two atria have the thinnest walls because they are low-pressure chambers that serve as storage units and conduits for blood that is emptied into the ventricles. This selection is the only option that correctly identifies which heart chambers have the thinnest walls and why that helps cardiac function. PTS: 1 REF: Page 1086 3. Which chamber of the heart endures the highest pressures? a. Right atrium c. Left ventricle b. Left atrium d. Right ventricle Pressure is greatest in the systemic circulation, driven by the left ventricle. PTS: 1 REF: Page 1086 4. What is the process that ensures mitral and tricuspid valve closure after the ventricles are filled with blood? a. Chordae tendineae relax, which allows the valves to close. b. Increased pressure in the ventricles pushes the valves to close. c. Trabeculae carneae contract, which pulls the valves closed. d. Reduced pressure in the atria creates a negative pressure that pulls the valves closed. During ventricular relaxation, the two atrioventricular valves open and blood flows from the higher pressure atria to the relaxed ventricles. With increasing ventricular pressure, these valves close and prevent backflow into the atria as the ventricles contract. This selection is the only option that correctly identifies the process that ensures closing of the mitral and tricuspid valves. PTS: 1 REF: Page 1088 5. Regarding the heart’s valves, what is a function of the papillary muscles? a. The papillary muscles close the semilunar valve. b. These muscles prevent backward expulsion of the atrioventricular valve. c. They close the atrioventricular valve. d. The papillary muscles open the semilunar valve. The papillary muscles are extensions of the myocardium that pull the cusps together and downward at the onset of ventricular contraction, thus preventing their backward expulsion into the atria. This selection is the only option that correctly describes the function of the papillary muscles. PTS: 1 REF: Pages 1087-1088 6. During the cardiac cycle, why do the aortic and pulmonic valves close after the ventricles relax? NURSINGTB.COM a. Papillary muscles relax, which allows the valves to close. b. Chordae tendineae contract, which pulls the valves closed. c. Reduced pressure in the ventricles creates a negative pressure, which pulls the valves closed. d. Blood fills the cusps of the valves and causes the edges to merge, closing the valves. When the ventricles relax, blood fills the cusps and causes their free edges to meet in the middle of the vessel, closing the valve and preventing any backflow. This selection is the only option that accurately explains why the aortic and pulmonic valves close after the ventricles contract. PTS: 1 REF: Page 1088 7. Oxygenated blood flows through which vessel? a. Superior vena cava c. Pulmonary artery b. Pulmonary veins d. Coronary veins Only the four pulmonary veins, two from the right lung and two from the left lung, carry oxygenated blood from the lungs to the left side of the heart. PTS: 1 REF: Page 1088 8. The significance of the atrial kick is that it affects the contraction of the: a. Right atria, which is necessary to open the tricuspid valve. b. Right atria, which is necessary to increase the blood volume from the vena cava. c. Left atria, which increases the blood volume into the ventricle. d. Left atria, that is necessary to open the mitral valve. Left atrial contraction, the atrial kick, provides a significant increase of blood to the left ventricle. PTS: 1 REF: Page 1088 9. Occlusion of the left anterior descending artery during a myocardial infarction would interrupt blood supply to which structures? a. Left and right ventricles and much of the interventricular septum b. Left atrium and the lateral wall of the left ventricle c. Upper right ventricle, right marginal branch, and right ventricle to the apex d. Posterior interventricular sulcus and the smaller branches of both ventricles The left anterior descending artery (LAD), also called the anterior interventricular artery, delivers blood to portions of the left and right ventricles and much of the interventricular septum. This selection is the only option affected by the occlusion described. PTS: 1 REF: Page 1090 10. Occlusion of the circumflex arteryNdUuRrSinINgGaTmB.yCoOcMardial infarction would interrupt blood supply to which area? a. Left and right ventricles and much of the interventricular septum b. Posterior interventricular sulcus and the smaller branches of both ventricles c. Upper right ventricle, right marginal branch, and right ventricle to the apex d. Left atrium and the lateral wall of the left ventricle The circumflex artery supplies blood to the left atrium and the lateral wall of the left ventricle. The circumflex artery often branches to the posterior surfaces of the left atrium and left ventricle. This selection is the only option affected by the occlusion described. PTS: 1 REF: Pages 1090-1091 11. The coronary ostia are located in the: a. Left ventricle c. Coronary sinus b. Aortic valve d. Aorta Coronary arteries receive blood through openings in the aorta, called the coronary ostia. PTS: 1 REF: Page 1090 12. The coronary sinus empties into which cardiac structure? a. Right atrium c. Superior vena cava b. Left atrium d. Aorta The cardiac veins empty only into the right atrium through another ostium, the opening of a large vein called the coronary sinus. PTS: 1 REF: Page 1090 13. What is the ratio of coronary capillaries to cardiac muscle cells? a. 1:1 (one capillary per one muscle cell) b. 1:2 (one capillary per two muscle cells) c. 1:4 (one capillary per four muscle cells) d. 1:10 (one capillary per ten muscle cells) The heart has an extensive capillary network, with approximately 3300 capillaries per square millimeter (ca/mm2) or approximately one capillary per one muscle cell (muscle fiber). PTS: 1 REF: Page 1092 14. During the cardiac cycle, which structure directly delivers action potential to the ventricular myocardium? a. Sinoatrial (SA) node c. Purkinje fibers b. Atrioventricular (AV) node d. Bundle branches Each cardiac action potential travels from the SA node to the AV node to the bundle of His (AV bundle), through the bundle NURSINGTB.COM lly to the Purkinje fibers and the ventricular myocardium, where the impulse is stopped. The refractory period of cells that have just been polarized prevents the impulse from reversing its path. The refractory period ensures that diastole (relaxation) will occur, thereby completing the cardiac cycle. This selection is the only option that accurately describes the structure that delivers the action potential directly to the myocardium. PTS: 1 REF: Page 1124 15. What causes depolarization of a cardiac muscle cell to occur? a. Decrease in the permeability of the cell membrane to potassium b. Rapid movement of sodium into the cell c. Decrease in the movement of sodium out of the cell d. Rapid movement of calcium out of the cell Phase 0 consists of depolarization, which lasts 1 to 2 milliseconds (ms) and represents rapid sodium entry into the cell. This selection is the only option that accurately describes the cause of cardiac muscle cell depolarization. PTS: 1 REF: Page 1094 16. Which event occurs during phase 1 of the normal myocardial cell depolarization and repolarization? a. Repolarization when potassium moves out of the cells b. Repolarization when sodium rapidly enters into the cells c. Early repolarization when sodium slowly enters the cells d. Early repolarization when calcium slowly enters the cells Phase 1 is early repolarization and the only time during which calcium slowly enters the cell. PTS: 1 REF: Page 1094 17. Which phase of the normal myocardial cell depolarization and repolarization correlates with diastole? a. Phase 1 c. Phase 3 b. Phase 2 d. Phase 4 Potassium is moved out of the cell during phase 3, with a return to resting membrane potential only in phase 4. The time between action potentials corresponds to diastole. PTS: 1 REF: Page 1094 18. In the normal electrocardiogram, what does the PR interval represent? a. Atrial depolarization b. Ventricular depolarization c. Atrial activation to onset of ventricular activity d. Electrical systole of the ventricles NURSINGTB.COM The PR interval is a measure of time from the onset of atrial activation to the onset of ventricular activation; it normally ranges from 0.12 to 0.20 second. The PR interval represents the time necessary to travel from the sinus node through the atrium, the atrioventricular (AV) node, and the His–Purkinje system to activate ventricular myocardial cells. This selection is the only option that accurately describes the PR interval. PTS: 1 REF: Page 1095 19. The cardiac electrical impulse normally begins spontaneously in the sinoatrial (SA) node because it: a. Has a superior location in the right atrium. b. Is the only area of the heart capable of spontaneous depolarization. c. Has rich sympathetic innervation via the vagus nerve. d. Depolarizes more rapidly than other automatic cells of the heart. The electrical impulse normally begins in the SA node because its cells depolarize more rapidly than other automatic cells. This selection is the only option that accurately explains why cardiac electrical impulses normally begin spontaneously in the SA node. PTS: 1 REF: Page 1095 20. What period follows depolarization of the myocardium and represents a period during which no new cardiac potential can be propagated? a. Refractory c. Threshold b. Hyperpolarization d. Sinoatrial (SA) During the refractory period, no new cardiac action potential can be initiated by a stimulus. This selection is the only option that accurately identifies the period described in the question. PTS: 1 REF: Page 1095 21. Which complex (wave) represents the sum of all ventricular muscle cell depolarizations? a. PRS c. QT interval b. QRS d. P Only the QRS complex represents the sum of all ventricular muscle cell depolarizations. PTS: 1 REF: Page 1095 22. What can shorten the conduction time of action potential through the atrioventricular (AV) node? a. Parasympathetic nervous system c. Vagal stimulation b. Catecholamines d. Sinoatrial node (SA) Catecholamines speed the heart rate, shorten the conduction time through the AV node, and increase the rhythmicity of NURSINGTB.COM fibers. This selection is the only option that can perform that function. PTS: 1 REF: Page 1096 23. If the sinoatrial (SA) node fails, then at what rate (depolarizations per minute) can the atrioventricular (AV) node depolarize? a. 60 to 70 c. 30 to 40 b. 40 to 60 d. 10 to 20 If the SA node is damaged, then the AV node will become the heart’s pacemaker at a rate of approximately 40 to 60 spontaneous depolarizations per minute. PTS: 1 REF: Page 1095 24. What is the effect of epinephrine on 3 receptors on the heart? a. Decreases coronary blood flow. b. Supplements the effects of both 1 and 2 receptors. c. Increases the strength of myocardial contraction. d. Prevents overstimulation of the heart by the sympathetic nervous system. 3 receptors are found in the myocardium and coronary vessels. In the heart, stimulation of these receptors opposes the effects of 1- and 2-receptor stimulation and negative inotropic effect. Thus 3 receptors may provide a safety mechanism that decreases myocardial contractility to prevent overstimulation of the heart by the sympathetic nervous system. This selection is the only option that accurately describes the effect of epinephrine on 2 receptors on the heart. PTS: 1 REF: Page 1097 25. Where in the heart are the receptors for neurotransmitters located? a. Semilunar and atrioventricular (AV) valves b. Endocardium and sinoatrial (SA) node c. Myocardium and coronary vessels d. Epicardium and AV node Sympathetic neural stimulation of the myocardium and coronary vessels depends on the presence of adrenergic receptors, which specifically bind with neurotransmitters of the sympathetic nervous system. The 1 receptors are found mostly in the heart, specifically the conduction system (AV and SA nodes, Purkinje fibers) and the atrial and ventricular myocardium, whereas the 2 receptors are found in the heart and also on vascular smooth muscle. 3 receptors are also found in the myocardium and coronary vessels. This selection is the only option that accurately identifies the location of the receptors for neurotransmitters. PTS: 1 REF: Page 1097 NURSINGTB.COM 26. What enables electrical impulses to travel in a continuous cell-to-cell fashion in myocardial cells? a. Sarcolemma sclerotic plaques c. Trabeculae carneae b. Intercalated disks d. Bachmann bundles Only intercalated disks, thickened portions of the sarcolemma, enable electrical impulses to spread quickly in a continuous cell-to-cell (syncytial) fashion. PTS: 1 REF: Page 1097 27. Within a physiologic range, what does an increase in left ventricular end-diastolic volume (preload) result in? a. Increase in force of contraction c. Increase in afterload b. Decrease in refractory time d. Decrease in repolarization This concept is expressed in the Frank-Starling law; the cardiac muscle, like other muscles, increases its strength of contraction when it is stretched. This selection is the only option that accurately describes the result of an increase in preload. PTS: 1 REF: Pages 1101-1102 28. As stated in the Frank-Starling law, a direct relationship exists between the of the blood in the heart at the end of diastole and the of contraction during the next systole. a. Pressure; force c. Viscosity; force b. Volume; strength d. Viscosity; strength As stated in the Frank-Starling law, the volume of blood in the heart at the end of diastole (the length of its muscle fibers) is directly related to the force (strength) of contraction during the next systole. This selection is the only option that accurately describes the relationship associated with the Frank-Starling law. PTS: 1 REF: Pages 1101-1102 29. Pressure in the left ventricle must exceed pressure in which structure before the left ventricle can eject blood? a. Superior vena cava c. Inferior vena cava b. Aorta d. Pulmonary veins Pressure in the ventricle must exceed aortic pressure before blood can be pumped out during systole. The aorta is the only structure in which pressure must be less than the amount of blood in the left ventricle for ejection to occur. PTS: 1 REF: Page 1103 30. Continuous increases in left ventricular filing pressures result in which disorder? a. Mitral regurgitation NURSINGTcB..COPMulmonary edema b. Mitral stenosis d. Jugular vein distention Pressure changes are important because increased left ventricular filling pressures back up into the pulmonary circulation, where they force plasma out through vessel walls, causing fluid to accumulate in lung tissues (pulmonary edema). This selection is the only option that accurately identifies the disorder described in the question. PTS: 1 REF: Page 1103 31. When the volume of blood in the ventricle at the end of diastole increases, the force of the myocardial contraction during the next systole will also increase, which is an example of which law or theory about the heart? a. Laplace’s law c. Cross-bridge theory b. Poiseuille law d. Frank-Starling law This concept is expressed only in the Frank-Starling law; the cardiac muscle, like other muscles, increases its strength of contraction when it is stretched. PTS: 1 REF: Page 1101 32. The resting heart rate in a healthy person is primarily under the control of which nervous system? a. Sympathetic c. Somatic b. Parasympathetic d. Spinal The resting heart rate in healthy individuals is primarily under the control of parasympathetic stimulation. This selection is the only option that accurately identifies the nervous system responsible for the healthy resting heart. PTS: 1 REF: Page 1106 33. The Bainbridge reflex is thought to be initiated by sensory neurons in which cardiac location? a. Atria c. Sinoatrial (SA) node b. Aorta d. Ventricles The Bainbridge reflex causes changes in the heart rate after intravenous infusions of blood or other fluid. The changes in heart rate are thought to be caused by a reflex mediated by volume receptors found only in the atria that are innervated by the vagus nerve. PTS: 1 REF: Page 1106 34. After the baroreceptor reflex is stimulated, the resulting impulse is transmitted from the carotid artery by which sequence of events? a. Vagus nerve to the medulla to increase parasympathetic activity and to decrease sympathetic activity b. Glossopharyngeal cranial nerve through the vagus nerve to the medulla to increase sympathetic activity and to deNcrUeRasSeINpGaTraBs.yCmOMpathetic activity c. Glossopharyngeal cranial nerve through the vagus nerve to the medulla to increase parasympathetic activity and to decrease sympathetic activity d. Glossopharyngeal cranial nerve through the vagus nerve to the hypothalamus to increase parasympathetic activity and to decrease sympathetic activity Neural impulses are transmitted over the glossopharyngeal nerve (ninth cranial nerve) from the carotid artery and through the vagus nerve from the aorta to the cardiovascular control centers in the medulla. These centers initiate an increase in parasympathetic activity and a decrease in sympathetic activity, causing blood vessels to dilate and the heart rate to decrease. This selection is the only option that accurately describes the correct sequence of events asked for in the question. PTS: 1 REF: Page 1106 35. Reflex control of total cardiac output and total peripheral resistance is controlled by what mechanism? a. Parasympathetic stimulation of the heart, arterioles, and veins b. Sympathetic stimulation of the heart, arterioles, and veins c. Autonomic control of the heart only d. Somatic control of the heart, arterioles, and veins Reflex control of total cardiac output and peripheral resistance includes (1) sympathetic stimulation of the heart, arterioles, and veins; and (2) parasympathetic stimulation of the heart only. Neither autonomic nor somatic controls are involved in this process. PTS: 1 REF: Pages 1114-1115 36. What is the most important negative inotropic agent? a. Norepinephrine c. Acetylcholine b. Epinephrine d. Dopamine Chemicals affecting contractility are called inotropic agents. The most important negative inotropic agent is acetylcholine released from the vagus nerve. The most important positive inotropic agents produced by the body are norepinephrine released from the sympathetic nerves that supply the heart and epinephrine released by the adrenal cortex. Other positive inotropes include thyroid hormone and dopamine. Many medications have positive or negative inotropic properties that can have profound effects on cardiac function. This selection is the only option that accurately identifies the regulation that is involved in the described process. PTS: 1 REF: Page 1103 37. The right lymphatic duct drains into which structure? a. Right subclavian artery c. Right subclavian vein b. Right atrium d. Superior vena cava The right lymphatic duct drains lyNmUpRhSoINnGlyTBin.CtoOtMhe right subclavian vein. PTS: 1 REF: Page 1118 38. Where is the major cardiovascular center in the central nervous system? a. Frontal lobe c. Brainstem b. Thalamus d. Hypothalamus The major cardiovascular control center is in the brainstem in the medulla with secondary areas in the hypothalamus, the cerebral cortex, the thalamus, and the complex networks of exciting or inhibiting interneurons (connecting neurons) throughout the brain. This selection is the only option that accurately identifies the cardiovascular control center. PTS: 1 REF: Page 1104 39. What is an expected change in the cardiovascular system that occurs with aging? a. Arterial stiffening b. Decreased left ventricular wall tension c. Decreased aortic wall thickness d. Arteriosclerosis Arterial stiffening occurs with aging even in the absence of clinical hypertension. Aging is not responsible for the other conditions. PTS: 1 REF: Page 1123 40. What is the major determinant of the resistance that blood encounters as it flows through the systemic circulation? a. Volume of blood in the systemic circulation b. Muscle layer of the metarterioles c. Muscle layer of the arterioles d. Force of ventricular contraction Of the options available, only the thick, smooth muscle layer of the arterioles is a major determinant of the resistance blood encounters as it flows through the systemic circulation. PTS: 1 REF: Page 1108 41. Which function of the cardiovascular system is often affected by ischemia? a. Cardiac output (CO) c. Heart rate (HR) b. Stroke volume (SV) d. Cardiac index (CI) Common causes of an abnormal heart rate include ischemia, electrolyte imbalance, and drug toxicity. The other options are related to vascular resistance changes. PTS: 1 REF: Page 1120 | Table 31-4 42. What physical sign is the result of turbulent blood flow through a vessel? a. Increased blood pressure durinNgUpReSrIiNoGdsTBo.fCsOtrMess b. Bounding pulse felt on palpation c. Cyanosis observed on excretion d. Murmur heard on auscultation Where flow is obstructed, the vessel turns or blood flows over rough surfaces. The flow becomes turbulent with whorls or eddy currents that produce noise, causing a murmur to be heard on auscultation, such as occurs during blood pressure measurement with a sphygomanometer. This selection is the only option that accurately identifies the physical sign of turbulent vascular blood flow. PTS: 1 REF: Page 1113 43. What is the major effect of a calcium channel blocker such as verapamil on cardiac contractions? a. Increases the rate of cardiac contractions. b. Decreases the strength of cardiac contractions. c. Stabilizes the rhythm of cardiac contractions. d. Stabilizes the vasodilation during cardiac contractions. The L-type, or long-lasting, channels are the predominant type of calcium channels and are the channels blocked by calcium channel–blocking drugs (verapamil, nifedipine, diltiazem). The major effect of these medications is to decrease the strength of cardiac contraction. This selection is the only option that accurately identifies the effect of a calcium channel blocker on the cardiac contractions. PTS: 1 REF: Page 1099 44. An early diastole peak caused by filling of the atrium from peripheral veins is identified by which intracardiac pressure? a. A wave c. C wave b. V wave d. X descent The V wave is an early diastolic peak caused by the filling of the atrium from the peripheral veins. This event is not identified by any of the other options. PTS: 1 REF: Page 1089 45. Which intracardiac pressure is generated by the atrial contraction? a. A wave c. Y descent b. C wave d. X descent Atrial pressure curves are made up of only the A wave, which is generated by atrial contraction. PTS: 1 REF: Page 10N8U9RSINGTB.COM 46. Which intracardiac pressure is produced because of the descent of the tricuspid valve ring and by the ejection of blood from both ventricles? a. V wave c. Y descent b. C wave d. X descent The X descent follows an A wave and is produced because of the descent of the tricuspid valve ring and by the ejection of blood from both ventricles. PTS: 1 REF: Page 1089 MULTIPLE RESPONSE 47. Which statements are true concerning the method in which substances pass between capillaries and the interstitial fluid? (Select all that apply.) a. Substances pass through junctions between endothelial cells. b. Substances pass through pores or oval windows (fenestrations). c. Substances pass between vesicles by active transport across the endothelial cell membrane. d. Substances pass across the endothelial cell membrane by osmosis. e. Substances pass through endothelial cell membranes by diffusion. , B, C, E Substances pass between the capillary lumen and the interstitial fluid in several ways: (1) through junctions between endothelial cells, (2) through fenestrations in endothelial cells, (3) in vesicles moved by active transport across the endothelial cell membrane, or (4) by diffusion through the endothelial cell membrane. PTS: 1 REF: Page 1108 MATCHING Match the description with the corresponding terms. A. Relationship among blood flow, pressure, and resistance B. Increased heart rate from increased volume C. Relationship of wall tension, intraventricular pressure, internal radius, and wall thickness D. Cycles of attachment, movement, and dissociation of thin filaments during the attachments of actin to myosin E. Length-tension relationship of cardiac muscle 48. Poiseuille law 49. Cross-bridge theory 50. Frank-Starling law 51. Laplace’s law 52. Bainbridge reflex 48. ANS: A PTS: 1 REF: Pages 1111-1112 MSC: Poiseuille law for resistance to fluid flow through a tube takes into account the length of the tube, the viscosity of the fluid, and thNeUraRdSiIuNsGoTf Bth.Ce OtuMbe's lumen. 49. ANS: D PTS: 1 REF: Page 1099 MSC: With the attachment of actin to myosin at the cross-bridge, the myosin head molecule undergoes a position change, exerting traction on the rest of the myosin bridge, causing the thin filaments to slide past the thick filaments. During contraction, each cross-bridge undergoes cycles of attachment, movement, and dissociation from the thin filaments. 50. ANS: E PTS: 1 REF: Page 1101 MSC: The Frank-Starling law states that the cardiac muscle, like other muscles, increases its strength of contraction when it is stretched. 51. ANS: C PTS: 1 REF: Pages 1102-1103 MSC: In Laplace's law, wall tension is directly related to the product of intraventricular pressure and internal radius and inversely to the wall thickness. 52. ANS: B PTS: 1 REF: Page 1106 MSC: The Bainbridge reflex causes changes in the heart rate after intravenous infusions of blood or other fluid. Chapter 33: Alterations of Cardiovascular Function MULTIPLE CHOICE 1. What is the initiating event that leads to the development of atherosclerosis? a. Release of the inflammatory cytokines b. Macrophages adhere to vessel walls. c. Injury to the endothelial cells that line the artery walls d. Release of the platelet-deprived growth factor Atherosclerosis begins with an injury to the endothelial cells that line the arterial walls. Possible causes of endothelial injury include the common risk factors for atherosclerosis, such as smoking, hypertension, diabetes, increased levels of low-density lipoprotein (LDL), decreased levels of high-density lipoprotein (HDL), and autoimmunity. The remaining options occur only after the endothelial cells are injured. PTS: 1 REF: Page 1145 2. What is the effect of oxidized low-density lipoproteins (LDLs) in atherosclerosis? a. LDLs cause smooth muscle proliferation. b. LDLs cause regression of atherosclerotic plaques. c. LDLs increase levels of inflammatory cytokines. d. LDLs direct macrophages to the site in the endothelium. Oxidized LDLs are toxic to endotNheUlRiaSlIcNeGllTsB, .cCaOuMse smooth muscle proliferation, and activate further immune and inflammatory responses. This selection is the only option that accurately identifies the effects of LDLs. PTS: 1 REF: Page 1145 3. Which inflammatory cytokines are released when endothelial cells are injured? a. Granulocyte-macrophage colony-stimulating factor (GM-CSF) b. Interferon-beta (IFN-), interleukin 6 (IL-6), and granulocyte colony-stimulating factor (G-CSF) c. Tumor necrosis factor–alpha (TNF-), interferon-gamma (IFN-), and interleukin 1 (IL-1) d. Interferon-alpha (IFN-), interleukin-12 (IL-12), and macrophage colony-stimulating factor (M-CSF) Numerous inflammatory cytokines are released, including TNF-, IFN-, IL-1, toxic oxygen radicals, and heat shock proteins. This selection is the only option that accurately identifies which inflammatory cytokines are associated with endothelial cell injury. PTS: 1 REF: Page 1145 4. When endothelia cells are injured, what alteration contributes to atherosclerosis? a. The release of toxic oxygen radicals that oxidize low-density lipoproteins (LDLs). b. Cells are unable to make the normal amount of vasodilating cytokines. c. Cells produce an increased amount of antithrombotic cytokines. d. Cells develop a hypersensitivity to homocysteine and lipids. Injured endothelial cells become inflamed and cannot make normal amounts of antithrombotic and vasodilating cytokines. This selection is the only option that accurately identifies the factor that contributes to atherosclerosis. PTS: 1 REF: Page 1145 5. Which factor is responsible for the hypertrophy of the myocardium associated with hypertension? a. Increased norepinephrine c. Angiotensin II b. Adducin d. Insulin resistance Of the available options, only angiotensin II is responsible for the hypertrophy of the myocardium and much of the renal damage associated with hypertension. PTS: 1 REF: Pages 1132-1138 6. What pathologic change occurs to the kidney’s glomeruli as a result of hypertension? a. Compression of the renal tubules b. Ischemia of the tubule c. Increased pressure from within the tubule d. Obstruction of the renal tubule NURSINGTB.COM In the kidney, vasoconstriction and resultant decreased renal perfusion cause tubular ischemia and preglomerular arteriopathy. This selection is the only option that accurately identifies the pathologic change to the kidney that occurs as a result of hypertension. PTS: 1 REF: Pages 1134-1136 7. What effect does atherosclerosis have on the development of an aneurysm? a. Atherosclerosis causes ischemia of the intima. b. It increases nitric oxide. c. Atherosclerosis erodes the vessel wall. d. It obstructs the vessel. Atherosclerosis is a common cause of aneurysms because plaque formation erodes the vessel wall. This selection is the only option that accurately identifies the effect that atherosclerosis has on aneurysm development. PTS: 1 REF: Pages 1141-1142 8. Regarding the endothelium, what is the difference between healthy vessel walls and those that promote clot formation? a. Inflammation and roughening of the endothelium of the artery are present. b. Hypertrophy and vasoconstriction of the endothelium of the artery are present. c. Excessive clot formation and lipid accumulation in the endothelium of the artery are present. d. Evidence of age-related changes that weaken the endothelium of the artery are present. Invasion of the tunica intima by an infectious agent also roughens the normally smooth lining of the artery, causing platelets to adhere readily. This selection is the only option that accurately describes the mechanism that supports abnormal clot formation. PTS: 1 REF: Pages 1142-1143 9. What is the usual source of pulmonary emboli? a. Deep venous thrombosis c. Valvular disease b. Endocarditis d. Left heart failure Pulmonary emboli originate in the venous circulation (mostly from the deep veins of the legs) or in the right heart. This selection is the only option that accurately identifies the usual source of pulmonary emboli. PTS: 1 REF: Page 1143 10. Which factor can trigger an immune response in the bloodstream that may result in an embolus? a. Amniotic fluid c. Bacteria b. Fat d. Air NURSINGTB.COM Of the options available, only amniotic fluid displaces blood, thereby reducing oxygen, nutrients, and waste exchange; however, it also introduces antigens, cells, and protein aggregates that trigger inflammation, coagulation, and the immune response in the bloodstream. PTS: 1 REF: Pages 1143-1144 11. Which statement best describes thromboangiitis obliterans (Buerger disease)? a. Inflammatory disorder of small- and medium-size arteries in the feet and sometimes in the hands b. Vasospastic disorder of the small arteries and arterioles of the fingers and, less commonly, of the toes c. Autoimmune disorder of the large arteries and veins of the upper and lower extremities d. Neoplastic disorder of the lining of the arteries and veins of the upper extremities Buerger disease is an inflammatory disease of the peripheral arteries. Inflammation, thrombus formation, and vasospasm can eventually occlude and obliterate portions of small- and medium-size arteries. The digital, tibial, and plantar arteries of the feet and the digital, palmar, and ulnar arteries of the hands are typically affected. This selection is the only option that accurately describes Buerger disease. 12. Which statement best describes Raynaud disease? a. Inflammatory disorder of small- and medium-size arteries in the feet and sometimes in the hands b. Neoplastic disorder of the lining of the arteries and veins of the upper extremities c. Vasospastic disorder of the small arteries and arterioles of the fingers and, less commonly, of the toes d. Autoimmune disorder of the large arteries and veins of the upper and lower extremities Attacks of vasospasm in the small arteries and arterioles of the fingers and, less commonly, of the toes characterize Raynaud phenomenon and Raynaud disease and is the only option that accurately describes this disease. PTS: 1 REF: Page 1144 13. What change in a vein supports the development of varicose veins? a. Increase in osmotic pressure c. Damage to the venous endothelium b. Damage to the valves in veins d. Increase in hydrostatic pressure If a valve is damaged, permitting backflow, then a section of the vein is subjected to the pressure exerted by a larger volume of blood under the influence of gravity. The vein swells as it becomes engorged, and the surrounding tissue becomes edematous because increased hydrostatic pressure pushes plasma through the stretched vessel wall. This selection is the only option that acNcUurRaSteINlyGdTeBs.CcrOibMes the development of varicose veins. PTS: 1 REF: Pages 1129-1130 14. Superior vena cava syndrome is a result of a progressive increase of which process? a. Inflammation c. Distention b. Occlusion d. Sclerosis Superior vena cava syndrome (SVCS) is a progressive occlusion of the superior vena cava (SVC) that leads to venous distention in the upper extremities and head. The remaining options are not associated with this disorder. PTS: 1 REF: Page 1131 15. What term is used to identify when a cell is temporarily deprived of blood supply? a. Infarction c. Necrosis b. Ischemia d. Inflammation Coronary artery disease (CAD) can diminish the myocardial blood supply until deprivation impairs myocardial metabolism enough to cause ischemia, a local state in which the cells are temporarily deprived of blood supply. This term is the only option that is used to identify a temporarily deprived blood supply. PTS: 1 REF: Page 1148 16. The risk of developing coronary artery disease is increased up to threefold by which factor? a. Diabetes mellitus c. Obesity b. Hypertension d. High alcohol consumption Hypertension is the only factor responsible for a twofold-to-threefold increased risk of atherosclerotic cardiovascular disease. PTS: 1 REF: Page 1151 17. Which risk factor is associated with coronary artery disease (CAD) because of its relationship with the alteration of hepatic lipoprotein? a. Diabetes mellitus c. Obesity b. Hypertension d. High alcohol consumption Of the available options, only diabetes mellitus is associated with CAD because of the resulting alteration of hepatic lipoprotein synthesis; it increases triglyceride levels and is involved in low-density lipoprotein oxidation. PTS: 1 REF: Pages 1148-1151 18. Nicotine increases atherosclerosis by the release of which neurotransmitter? a. Histamine c. Angiotensin II b. Nitric oxide NURSINGTdB..COEMpinephrine Nicotine stimulates the release of catecholamines (e.g., epinephrine, norepinephrine), which increases the heart rate and causes peripheral vascular constriction. As a result, blood pressure increases, as do both cardiac workload and oxygen demand. None of the other options are associated with this mechanism. PTS: 1 REF: Page 1151 19. Which substance is manufactured by the liver and primarily contains cholesterol and protein? a. Very low–density lipoproteins (VLDLs) b. Low-density lipoproteins (LDLs) c. High-density lipoproteins (HDLs) d. Triglycerides A series of chemical reactions in the liver results in the production of several lipoproteins that vary in density and function. These include VLDLs, primarily triglycerides and protein; LDLs, mostly cholesterol and protein; and HDLs, mainly phospholipids and protein. LDLs are the only lipoproteins that are manufactured by the liver and primarily contain cholesterol and protein. PTS: 1 REF: Page 1149 20. Which elevated value may be protective of the development of atherosclerosis? a. Very low–density lipoproteins (VLDLs) b. Low-density lipoproteins (LDLs) c. High-density lipoproteins (HDLs d. Triglycerides Low levels of HDL cholesterol are also a strong indicator of coronary risk, whereas high levels of HDLs may be more protective for the development of atherosclerosis than low levels of LDLs. Neither VLDLs nor elevated triglycerides are associated with a protective mechanism. PTS: 1 REF: Pages 1149-1151 21. Which laboratory test is an indirect measure of atherosclerotic plaque? a. Homocysteine b. Low-density lipoprotein (LDL) c. Erythrocyte sedimentation rate (ESR) d. C-reactive protein (CRP) Highly sensitive CRP (hs-CRP) is an acute phase reactant or protein mostly synthesized in the liver and, of the available options, is an indirect measure of atherosclerotic plaque-related inflammation. PTS: 1 REF: Page 1152 NURSINGTB.COM 22. Cardiac cells can withstand ischemic conditions and still return to a viable state for how many minutes? a. 10 c. 20 b. 15 d. 25 Cardiac cells remain viable for approximately 20 minutes under ischemic conditions. If blood flow is restored, then aerobic metabolism resumes, contractility is restored, and cellular repair begins. If the coronary artery occlusion persists beyond 20 minutes, then myocardial infarction (MI) occurs. PTS: 1 REF: Page 1153 23. Which form of angina occurs most often during sleep as a result of vasospasms of one or more coronary arteries? a. Unstable c. Silent b. Stable d. Prinzmetal Of the options available, only Prinzmetal angina (also called variant angina) is chest pain attributable to transient ischemia of the myocardium that occurs unpredictably and almost exclusively at rest. PTS: 1 REF: Page 1154 24. When is the scar tissue that is formed after a myocardial infarction (MI) most vulnerable to injury? a. Between 5 and 9 days c. Between 15 and 20 days b. Between 10 and 14 days d. Between 20 and 30 days During the recovery period (10 to 14 days after infarction), individuals feel more capable of increasing activities and thus may stress the newly formed scar tissue. After 6 weeks, the necrotic area is completely replaced by scar tissue, which is strong but unable to contract and relax like healthy myocardial tissue. PTS: 1 REF: Page 1160 25. An individual who is demonstrating elevated levels of troponin, creatine kinase–isoenzyme MB (CK-MB), and lactic dehydrogenase (LDH) is exhibiting indicators associated with which condition? a. Myocardial ischemia c. Myocardial infarction (MI) b. Hypertension d. Coronary artery disease (CAD) Cardiac troponins (troponin I and troponin T) are the most specific indicators of MI. Other biomarkers released by myocardial cells include CK-MB and LDH, but they are not associated with the other options. PTS: 1 REF: Pages 1160-1161 26. What is the expected electrocardioNgUrRamSIN(EGCTBG.C) OpaMttern when a thrombus in a coronary artery permanently lodges in the vessel and the infarction extends through the myocardium from the endocardium to the epicardium? a. Prolonged QT interval b. ST elevation myocardial infarction (STEMI) c. ST depression myocardial infarction (STDMI) d. Non-ST elevation myocardial infarction (non-STEMI) Individuals with this pattern on an ECG usually have significant elevations in the ST segments and are categorized as having STEMI. The other options are not associated with the described pathologic condition. PTS: 1 REF: Pages 1157-1158 27. How does angiotensin II increase the workload of the heart after a myocardial infarction (MI)? a. By increasing the peripheral vasoconstriction b. By causing dysrhythmias as a result of hyperkalemia c. By reducing the contractility of the myocardium d. By stimulating the sympathetic nervous system Angiotensin II is released during myocardial ischemia and contributes to the pathogenesis of a myocardial infarction (MI) in several ways. First, it results in the systemic effects of peripheral vasoconstriction and fluid retention. These homeostatic responses are counterproductive in that they increase myocardial work and thus exacerbate the effects of the loss of myocyte contractility. Angiotensin II is also locally released, where it is a growth factor for vascular smooth muscle cells, myocytes, and cardiac fibroblasts; promotes catecholamine release; and causes coronary artery spasm. This selection is the only option that accurately describes how angiotensin II increases workload after a MI. PTS: 1 REF: Page 1159 28. The pulsus paradoxus that occurs as a result of pericardial effusion is caused by a dysfunction in which mechanism? a. Diastolic filling pressures of the right ventricle and reduction of blood volume in both ventricles b. Blood ejected from the right atrium and reduction of blood volume in the right ventricle c. Blood ejected from the left atrium and reduction of blood volume in the left ventricle d. Diastolic filling pressures of the left ventricle and reduction of blood volume in all four heart chambers. Pulsus paradoxus means that the arterial blood pressure during expiration exceeds arterial pressure during inspiration by more than 10 mm Hg. This clinical finding reflects impairment of diastolic filling of the left ventricle plus a reduction of blood volume within all four cardiac chambers. This seNleUctRiSoInNiGsTthBe.CoOnMly option that accurately describes the mechanism. PTS: 1 REF: Page 1164 29. A patient reports sudden onset of severe chest pain that radiates to the back and worsens with respiratory movement and when lying down. These clinical manifestations describe: a. Myocardial infarction (MI) c. Restrictive pericarditis b. Pericardial effusion d. Acute pericarditis Most individuals with acute pericarditis describe several days of fever, myalgias, and malaise, followed by the sudden onset of severe chest pain that worsens with respiratory movements and with lying down. Although the pain may radiate to the back, it is generally felt in the anterior chest and may be initially confused with the pain of an acute MI. Individuals with acute pericarditis also may report dysphagia, restlessness, irritability, anxiety, and weakness. This selection is the only option with these symptoms. PTS: 1 REF: Page 1163 30. Ventricular dilation and grossly impaired systolic function, leading to dilated heart failure, characterize which form of cardiomyopathy? a. Congestive c. Septal b. Hypertrophic d. Dystrophic Only dilated cardiomyopathy (congestive cardiomyopathy) is characterized by ventricular dilation and grossly impaired systolic function, leading to dilated heart failure. PTS: 1 REF: Page 1165 31. A disproportionate thickening of the interventricular septum is the hallmark of which form of cardiomyopathy? a. Dystrophic c. Restrictive b. Hypertrophic d. Dilated Only hypertrophic cardiomyopathy is characterized by a thickening of the septal wall, which may cause outflow obstruction to the left ventricle outflow tract. PTS: 1 REF: Page 1166 32. Amyloidosis, hemochromatosis, or glycogen storage disease usually causes which form of cardiomyopathy? a. Infiltrative c. Septal b. Restrictive d. Hypertrophic Restrictive cardiomyopathy may occur idiopathically or as a cardiac manifestation of systemic diseases, such as scleroderma, amyloidosis, sarcoidosis, lymphoma, and hemochromatosis, or a number of inherited storage diseases. This characterization is not true of the other forms of cardiomyopathy. NURSINGTB.COM PTS: 1 REF: Page 1167 33. Which condition is a cause of acquired aortic regurgitation? a. Congenital malformation c. Rheumatic fever b. Cardiac failure d. Coronary artery disease (CAD) Rheumatic heart disease, bacterial endocarditis, syphilis, hypertension, connective tissue disorders (e.g., Marfan syndrome, ankylosing spondylitis), appetite suppressing medications, trauma, or atherosclerosis can cause acquired aortic regurgitation. This selection is the only available option that is known to cause acquired aortic regurgitation. PTS: 1 REF: Page 1169 34. Which predominantly female valvular disorder is thought to have an autosomal dominant inheritance pattern, as well as being associated with connective tissue disease? a. Mitral valve prolapse c. Tricuspid valve prolapse b. Tricuspid stenosis d. Aortic insufficiency Mitral valve prolapse tends to be most prevalent in young women. Studies suggest an autosomal dominant and X-linked inheritance pattern. Because mitral valve prolapse often is associated with other inherited connective tissue disorders (e.g., Marfan syndrome, Ehlers-Danlos syndrome, osteogenesis imperfecta), it is thought to result from a genetic or environmental disruption of valvular development during the fifth or sixth week of gestation. This provided history is not associated with any of the other options. PTS: 1 REF: Page 1170 35. Which disorder causes a transitory truncal rash that is nonpruritic and pink with erythematous macules that may fade in the center, making them appear as a ringworm? a. Fat emboli b. Rheumatic fever c. Bacterial endocarditis d. Myocarditis of acquired immunodeficiency syndrome Erythema marginatum is a distinctive truncal rash that often accompanies acute rheumatic fever. It consists of nonpruritic, pink erythematous macules that never occur on the face or hands. This presentation is not associated with any of the other options. PTS: 1 REF: Page 1172 36. What is the most common cause of infective endocarditis? a. Virus c. Bacterium b. Fungus d. Rickettsiae NURSINGTB.COM Infective endocarditis is a general term used to describe infection and inflammation of the endocardium—especially the cardiac valves. Bacteria are the most common cause of infective endocarditis, especially streptococci, staphylococci, or enterococci. PTS: 1 REF: Page 1173 37. What is the most common cardiac disorder associated with acquired immunodeficiency syndrome (AIDS) a. Cardiomyopathy c. Left heart failure b. Myocarditis d. Heart block Pericardial effusion and left heart failure are the most common complications of human immunodeficiency virus (HIV) infection. Other conditions include cardiomyopathy, myocarditis, tuberculous pericarditis, infective and nonbacterial endocarditis, heart block, pulmonary hypertension, and nonantiretroviral drug-related cardiotoxicity. PTS: 1 REF: Page 1175 38. A patient is diagnosed with pulmonary disease and elevated pulmonary vascular resistance. Which form of heart failure may result from pulmonary disease and elevated pulmonary vascular resistance? a. Right heart failure c. Low-output failure b. Left heart failure d. High-output failure Right heart failure is defined as the inability of the right ventricle to provide adequate blood flow into the pulmonary circulation at a normal central venous pressure. This condition is often a result of pulmonary disease and the resulting elevated pulmonary vascular resistance. PTS: 1 REF: Page 1181 39. What cardiac pathologic condition contributes to ventricular remodeling? a. Left ventricular hypertrophy c. Myocardial ischemia b. Right ventricular failure d. Contractile dysfunction Of the options available, myocardial ischemia contributes to inflammatory, immune, and neurohumoral changes that mediate a process called ventricular remodeling. PTS: 1 REF: Page 1175 40. In systolic heart failure, what effect does the renin-angiotensin-aldosterone system (RAAS) have on stroke volume? a. Increases preload and decreases afterload. b. Increases preload and increases afterload. c. Decreases preload and increases afterload. d. Decreases preload and decreases afterload. Activation of the RAAS not only causes an increase in preload and afterload, but it also causes direct toxicity to the myocNURSINGTB.COM tion is the only option that accurately identifies the effect that the RAAS has on stroke volume in this situation. PTS: 1 REF: Page 1175 | Page 1177 41. What is the cause of the dyspnea resulting from a thoracic aneurysm? a. Pressure on surrounding organs c. Formation of atherosclerotic lesions b. Poor oxygenation d. Impaired blood flow Clinical manifestations depend on the location of the aneurysm. Pressure of a thoracic aneurysm on surrounding organs cause symptoms of dysphagia (difficulty in swallowing) and dyspnea (breathlessness). This selection is the only option that accurately describes the cause of dyspnea resulting from a thoracic aneurysm. PTS: 1 REF: Page 1142 42. Which statement is true concerning the cells’ ability to synthesize cholesterol? a. Cell production of cholesterol is affected by the aging process. b. Cells produce cholesterol only when dietary fat intake is low. c. Most body cells are capable of producing cholesterol. d. Most cholesterol produced by the cells is converted to the low-density form. Although cholesterol can easily be obtained from dietary fat intake, most body cells can also manufacture cholesterol. This selection is the only option that accurately describes the cellular role in cholesterol synthesis. PTS: 1 REF: Page 1149 43. What is the trigger for angina pectoris? a. Atherosclerotic lesions c. Myocardial necrosis b. Hyperlipidemia d. Myocardial ischemia Angina pectoris is chest pain caused by myocardial ischemia. None of the other options are considered triggers for angina pectoris. PTS: 1 REF: Page 1154 44. Individuals being effectively managed for type 2 diabetes mellitus often experience a healthy decline in blood pressure as a result of what intervention? a. Managed carbohydrate intake b. Appropriate exercise c. Insulin-sensitivity medication therapy d. Introduction of minimal doses of insulin Many people with type 2 diabetes mellitus, who are treated with drugs that increase insulin sensitivity, experience a decline in their blood pressure without taking antihypertensive drugs. Although the other medications may be included in the management plan, the other options are not associated with a dNeUcrReSaIsNeGiTnBh.CypOeMrtension. PTS: 1 REF: Page 1136 MULTIPLE RESPONSE 45. Which statements are true regarding fatty streaks? (Select all that apply.) a. Fatty streaks progressively damage vessel walls. b. Fatty streaks are capable of producing toxic oxygen radials. c. When present, inflammatory changes occur to the vessel walls. d. Oxidized low-density lipoproteins (LDLs) are involved in their formation. e. Fatty streaks are formed by killer T cells filled with oxidized LDLs. , B, C, D The oxidized LDLs penetrate the intima of the arterial wall and are engulfed by macrophages. Macrophages filled with oxidized LDLs are called foam. Once these lipid-laden foam cells accumulate in significant amounts, they form a lesion called a fatty streak. Once formed, fatty streaks produce more toxic oxygen radicals and cause immunologic and inflammatory changes, resulting in progressive damage to the vessel wall. PTS: 1 REF: Page 1145 | Page 1147 46. What factors contribute to the development of orthostatic hypotension? (Select all that apply.) a. Altered body chemistry b. Drug action of certain antihypertensive agents c. Prolonged immobility d. Effects of aging on postural reflexes e. Any condition that produces volume overload , B, C, D Orthostatic hypotension may be acute or chronic. Acute orthostatic hypotension (temporary type) may result from (1) altered body chemistry, (2) drug action (e.g., antihypertensives, antidepressants), (3) prolonged immobility caused by illness, (4) starvation, (5) physical exhaustion, (6) any condition that produces volume depletion (e.g., massive diuresis, potassium or sodium depletion), and (7) venous pooling (e.g., pregnancy, extensive varicosities of the lower extremities). Older adults are susceptible to this type of orthostatic hypotension, in which postural reflexes are slowed as part of the aging process. PTS: 1 REF: Page 1140 47. Which assessment findings are clinical manifestations of aortic stenosis? (Select all that apply.) a. Jugular vein distention b. Bounding pulses c. Hypotension d. Angina e. Syncope , E NURSINGTB.COM The classic manifestations of aortic stenosis are angina, syncope, and heart failure. None of the other options are associated with aortic stenosis. PTS: 1 REF: Pages 1168-1169 48. Which risk factors are associated with infective endocarditis? (Select all that apply.) a. Rheumatic fever b. Intravenous drug use c. Long-term indwelling catheterization d. Aortic regurgitation e. Heart valve disease , C, E Risk factors for infective endocarditis include acquired valvular heart disease, intravenous drug abuse, long-term indwelling catheterization (e.g., for pressure monitoring, hyperalimentation, or hemodialysis), and recent cardiac surgery. Neither rheumatic fever nor aortic regurgitation is considered a risk factor for infective endocarditis. PTS: 1 REF: Page 1173 | Box 32-3 MATCHING Match the descriptions with the corresponding terms. A. Impairs flow from left atrium to left ventricle B. Impairs flow from the left ventricle C. Backflow into left atrium D. Backflow into right atrium E. Backflow into left ventricle 49. Aortic stenosis 50. Aortic regurgitation 51. Mitral stenosis 52. Tricuspid regurgitation 53. Mitral regurgitation 49. ANS: B PTS: 1 REF: Page 1168 MSC: Outflow obstruction increases pressure within the left ventricle as it tries to eject blood through the narrowed opening. Left ventricular hypertrophy develops to compensate for the increased workload. 50. ANS: E PTS: 1 REF: Pages 1169-1170 MSC: During systole, blood is ejected from the left ventricle into the aorta. If the aortic semilunar valve fails to close completely, then some of the ejected blood flows back into the left ventricle during diastole. 51. ANS: A PTS: 1 REF: Page 1169 MSC: Mitral stenosis impairs the flow of blood from the left atrium to the left ventricle. 52. ANS: D PTS: 1 REF: Page 1170 MSC: Tricuspid regurgitation is more common than tricuspid stenosis and is usually associated with cardiac failure and dilation of the right ventricle, secondary to pulmonary hypertension. 53. ANS: C PTS: 1 REF: Page 1170 MSC: Mitral regurgitation permits the backflow of blood from the left ventricle into the left atrium during ventricular systole, givNinUgRrSisIeNGtoTaBl.oCuOdMpansystolic (throughout systole) murmur heard best at the apex that radiates into the back and axillae. Chapter 34: Alterations of Cardiovascular Function in Children MULTIPLE CHOICE 1. Most cardiovascular developments occur between which weeks of gestation? a. Fourth and seventh weeks c. Twelfth and fourteenth weeks b. Eighth and tenth weeks d. Fifteenth and seventeenth weeks Cardiogenesis begins at approximately 3 weeks’ gestation; however, most cardiovascular development occurs between 4 and 7 weeks’ gestation. PTS: 1 REF: Page 1194 2. The function of the foramen ovale in a fetus allows what to occur? a. Right-to-left blood shunting c. Blood flow from the umbilical cord b. Left-to-right blood shunting d. Blood flow to the lungs The nonfused septum secundum and ostium secundum result in the formation of a flapped orifice known as the foramen ovale, which allows the right-to-left shunting necessary for fetal circulation. The foramen ovale is not involved in the blood flow described by the other options. PTS: 1 REF: Pages 1195-1196 3. At birth, which statement is true?NURSINGTB.COM a. Systemic resistance and pulmonary resistance fall. b. Gas exchange shifts from the placenta to the lung. c. Systemic resistance falls and pulmonary resistance rises. d. Systemic resistance and pulmonary resistance rise. From the available options, the only change that takes place in the circulation at birth is the shift of gas exchange from the placenta to the lungs. PTS: 1 REF: Page 1197 4. When does systemic vascular resistance in infants begin to increase? a. One month before birth b. During the beginning stage of labor c. One hour after birth d. Once the placenta is removed from circulation The low-resistance placenta is removed from circulation, which causes an immediate increase in systemic vascular resistance to approximately twice of that before birth. PTS: 1 REF: Page 1197 5. Which event triggers congenital heart defects that cause acyanotic congestive heart failure? a. Right-to-left shunts c. Obstructive lesions b. Left-to-right shunts d. Mixed lesions Congenital heart defects that cause acyanotic congestive heart failure usually involve left-to-right shunts (see Table 33-4). Acyanotic congestive heart failure does not involve any of the other options. PTS: 1 REF: Pages 1201-1202 | Table 33-4 6. Older children with an unrepaired cardiac septal defect experience cyanosis because of which factor? a. Right-to-left shunts c. Obstructive lesions b. Left-to-right shunts d. Mixed lesions Older children who have an unrepaired septal defect with a left-to-right shunt may become cyanotic because of pulmonary vascular changes secondary to increased pulmonary blood flow. None of the other options accurately describe the process that results in cyanosis. PTS: 1 REF: Page 1202 7. Which congenital heart defects occur in trisomy 13, trisomy 18, and Down syndrome? a. Coarctation of the aorta (COA) and pulmonary stenosis (PS) b. Tetralogy of Fallot and persistent truncus arteriosus c. Atrial septal defect (ASD) andNdUeRxStrINocGaTrBd.iCaOM d. Ventricular septal defect (VSD) and patent ductus arteriosus (PDA) Congenital heart defects that are related to dysfunction of trisomy 13, trisomy 18, and Down syndrome include VSD and PDA (see Table 33-2). The other defects are not associated with dysfunction of trisomy 13, trisomy 18, and Down syndrome. PTS: 1 REF: Page 1200 | Table 33-2 8. An infant has a continuous machine-type murmur best heard at the left upper sternal border throughout systole and diastole, as well as a bounding pulse and a thrill on palpation. These clinical findings are consistent with which congenital heart defect? a. Atrial septal defect (ASD) c. Patent ductus arteriosus (PDA) b. Ventricular septal defect (VSD) d. Atrioventricular canal (AVC) defect If pulmonary vascular resistance has fallen, then infants with PDA will characteristically have a continuous machine-type murmur best heard at the left upper sternal border throughout systole and diastole. If the PDA is significant, then the infant also will have bounding pulses, an active precordium, a thrill on palpation, and signs and symptoms of pulmonary overcirculation. The presentations of the other congenital heart defects are not consistent with the described the symptoms. PTS: 1 REF: Pages 1203-1204 9. An infant has a crescendo-decrescendo systolic ejection murmur located between the second and third intercostal spaces along the left sternal border. A wide fixed splitting of the second heart sound is also found. These clinical findings are consistent with which congenital heart defect? a. Atrial septal defect (ASD) c. Patent ductus arteriosus (PDA) b. Ventricular septal defect (VSD) d. Atrioventricular canal (AVC) defect Because most children with ASD are asymptomatic, diagnosis is usually made during a routine physical examination by the auscultation of a crescendo-decrescendo systolic ejection murmur that reflects increased blood flow through the pulmonary valve. The location of the murmur is between the second and third intercostal spaces along the left sternal border. A wide fixed splitting of the second heart sound is also characteristic of ASD, reflecting volume overload to the right ventricle and causing prolonged ejection time and a delay of pulmonic valve closure. The presentations of other congenital heart defects are not consistent with the described symptoms. PTS: 1 REF: Pages 1204-1205 10. An infant has a loud, harsh, holosystolic murmur and systolic thrill that can be detected at the left lower sternal border that radiates to the neck. These clinical findings are consistent with which congenital heart defect? a. Atrial septal defect (ASD) c. Patent ductus arteriosus (PDA) b. Ventricular septal defect (VSD) d. Atrioventricular canal (AVC) defect On physical examination, a loud, NhaUrRshS,INhGolToBs.yCsOtoMlic murmur and systolic thrill can be detected at the left lower sternal border. The intensity of the murmur reflects the pressure gradient across the VSD. An apical diastolic rumble may be present with a moderate-to-large defect, reflecting increased flow across the mitral valve. The presentations of the other congenital heart defects are not consistent with the described symptoms. PTS: 1 REF: Page 1205 11. Where can coarctation of the aorta (COA) be located? a. Exclusively on the aortic arch b. Proximal to the brachiocephalic artery c. Between the origin of the aortic arch and the bifurcation of the aorta in the lower abdomen d. Between the origin of the aortic arch and the origin of the first intercostal artery COA can occur anywhere between the origin of the aortic arch and the bifurcation of the aorta in the lower abdomen. The other options do not accurately describe the location of a COA. PTS: 1 REF: Page 1210 12. Classic manifestations of a systolic ejection murmur heard at the left interscapular area, cool mottled skin on the lower extremities but hypertension noted in the upper extremities, and decreased or absent femoral pulse are indicative of an older child with which congenital defect? a. Tetralogy of Fallot c. Ventricular septum defect (SD) b. Aortic stenosis d. Coarctation of the aorta (OA) Clinical manifestations of coarctation of the aorta include hypertension noted in the upper extremities with decreased or absent pulses in the lower extremities. Children may also have cool mottled skin and occasionally experience leg cramps during exercise. A systolic ejection murmur, heard best at the left interscapular area, is also considered a classic clinical manifestation of this disorder. The other options are not initially associated with these symptoms. PTS: 1 REF: Pages 1210-1212 13. What is the initial manifestation of aortic coarctation observed in a neonate? a. Congestive heart failure (CHF) c. Pulmonary hypertension b. Cor pulmonale d. Cerebral hypertension Initially, the newborn usually exhibits symptoms of CHF. The other options are not initially associated with aortic coarctation. PTS: 1 REF: Page 1212 14. Which compensatory mechanism NisUsRpSoInNtGanTeBo.CuOslMy used by children diagnosed with tetralogy of Fallot to relieve hypoxic spells? a. Lying on their left side c. Squatting b. Performing the Valsalva maneuver d. Hyperventilating Squatting is a spontaneous compensatory mechanism used by older children to alleviate hypoxic spells. Squatting and its variants increase systemic resistance while decreasing venous return to the heart from the inferior vena cava. The other options would not result in these changes. PTS: 1 REF: Page 1209 15. An infant diagnosed with a small patent ductus arteriosus (PDA) would likely exhibit which symptom? a. Intermittent murmur c. Need for surgical repair b. Lack of symptoms d. Triad of congenital defects Infants with a small PDA usually remain asymptomatic; the other options are incorrect. PTS: 1 REF: Pages 1203-1204 16. What is the most common cause of chronic sustained hypertension observed only in a newborn? a. Renal parenchymal disease c. Renal artery stenosis b. Primary hypertension d. Congenital renal malformation Congenital renal malformation is a cause of chronic sustained hypertension in a newborn. Although renal artery stenosis is observed in newborns, it is also observed in older children. Renal parenchymal disease and primary hypertension are commonly observed in older children diagnosed with chronic sustained hypertension. PTS: 1 REF: Page 1220 | Table 33-8 17. Which condition is consistent with the cardiac defect of transposition of the great vessels? a. The aorta arises from the right ventricle. b. The pulmonary trunk arises from the right ventricle. c. The right ventricle pumps blood to the lungs. d. An intermittent murmur is present. Transposition of the great arteries refers to a condition in which the aorta arises from the right ventricle and the pulmonary artery arises from the left ventricle. A transposition of the great vessels is not associated with any of the other options. PTS: 1 REF: Pages 1214-1215 18. Which scenario describes total anomalous pulmonary venous return? a. The foramen ovale closes after birth. b. Pulmonary venous return is to the right atrium. c. Pulmonary venous return is toNtUheRSleINftGaTtrBiu.CmO.M d. The left atrium receives oxygenated blood. Total anomalous pulmonary venous return occurs when the pulmonary veins abnormally connect to the right side of the heart either directly or through one or more systemic veins that drain into the right atrium. None of the other options accurately describe the presentation of a total anomalous pulmonary venous return. PTS: 1 REF: Page 1216 19. Which heart defect produces a systolic ejection murmur at the right upper sternal border that transmits to the neck and left lower sternal border? a. Coarctation of the aorta c. Aortic stenosis b. Pulmonic stenosis d. Hypoplastic left heart syndrome Blood flow through the stenotic area of the aorta produces a systolic ejection murmur at the right upper sternal border that transmits to the neck and left lower sternal border. None of the other options produce the described assessment findings. PTS: 1 REF: Page 1212 20. Which heart defect produces a systolic ejection click at the upper left sternal border with a thrill palpated at the upper left sternal border? a. Coarctation of the aorta (COA) c. Aortic stenosis b. Pulmonary stenosis (PS) d. Hypoplastic left heart syndrome PS results in a systolic ejection murmur at the left upper sternal border, reflecting an obstruction to flow through the narrowed pulmonary valve. A variable systolic ejection click is present in some children, as well as valvular stenosis at the upper left sternal border. PS also produces a thrill that may be palpated at the upper left sternal border. None of the other options produce the described assessment findings. PTS: 1 REF: Page 1213 21. Which heart defect results in a single vessel arising from both ventricles, providing blood to both the pulmonary and systemic circulations? a. Coarctation of the aorta b. Tetralogy of Fallot c. Total anomalous pulmonary connection d. Truncus arteriosus Truncus arteriosus is the failure of the large embryonic artery, the truncus arteriosus, to divide into the pulmonary artery and the aorta, which results in a single vessel arising from both ventricles, providing blood flow to the pulmonary and systemic circulations. None of the other options produce the described structural malformation. PTS: 1 REF: Page 1217 22. What is the suggested mean bloodNpUrResSsINurGeTfBo.rCaOnM8- to 9-year-old child? a. 104/55 mm Hg c. 112/62 mm Hg b. 106/58 mm Hg d. 121/70 mm Hg The suggested mean blood pressure for an 8- to 9- year-old child is 106/58 mm Hg. For a child of 6 to 7 years old, 104/55 mm Hg is appropriate; for a 12- to 13-year-old child, 112/62 mm Hg is appropriate, and for a 16- to 18-year-old young man, 121/70 mm Hg is appropriate. PTS: 1 REF: Page 1220 | Table 33-6 MULTIPLE RESPONSE 23. What congenital heart defects are associated with intrauterine exposure to rubella? (Select all that apply.) a. Pulmonary stenosis (PS) b. Cardiomegaly c. Patent ductus arteriosus (PDA) d. Coarctation of aorta (COA) e. Ventricular septal defect (VSD) , C, D PS, PDA, and COA are congenital heart defects associated with intrauterine exposure to rubella. Cardiomegaly and VSD are associated with maternal diabetes. PTS: 1 REF: Page 1199 | Table 33-1 24. Which symptoms meet the diagnostic criteria for Kawasaki disease in a child? (Select all that apply.) a. Fever for 5 days or longer b. “Strawberry tongue” c. Peripheral edema d. Inguinal lymphadenopathy e. Bilateral conjunctival infection , B, C, E The child must exhibit five of the following six criteria: (1) fever for 5 days or longer, (2) bilateral conjunctival infection without exudation, (3) changes in oral mucus such as strawberry tongue, (4) a polymorphous rash, (5) cervical lymphadenopathy, and (6) changes in the extremities such as peripheral edema. PTS: 1 REF: Page 1218 | Box 33-3 25. Which statements related to the ambulatory blood pressure monitoring (ABPM) system with children are true? (Select all that apply.) a. ABPM monitors blood pressure for a 24-hour period. b. ABPM assists in identifying children with white coat hypertension. c. ABPM is effective in identifying children at risk for target organ damage d. ABPM assists in identifying children who demonstrate masked hypertension. e. ABPM is effective in determinNiUngRSbIlNoGodTBp.rCeOssMure load or hypertension for at least 48 hours. , B, C, D ABPM records blood pressure over a 24-hour period to help identify those children with white coat hypertension and masked hypertension. ABPM is useful in documenting the blood pressure load, which is the total amount of time the blood pressure is elevated above normal limits during a 24-hour period. By measuring blood pressure load, the ABPM may be able to identify those children who are at greatest risk for target organ damage. PTS: 1 REF: Page 1221 | What's New box MATCHING Match the phrases with the corresponding terms. A. Causes atrial separation B. Gap between the septum primum and the septum secundum C. Conal portion of the ventricular septum D. Abnormal communication between the atria E. Allows right-to-left shunting 26. Atrial septal defect 27. Foramen ovale 28. Septum secundum 29. Ostium primum 30. Bulbus cordis 26. ANS: D PTS: 1 REF: Page 1196 MSC: An atrial septal defect is an abnormal communication between the atria. 27. ANS: E PTS: 1 REF: Pages 1195-1196 MSC: The nonfused septum secundum and ostium secundum result in the formation of a flapped orifice known as the foramen ovale, which allows the right-to-left shunting necessary for fetal circulation. 28. ANS: A PTS: 1 REF: Pages 1195-1196 MSC: The septum secundum is also a fenestrated, membranelike structure located anteriorly that grows toward the endocardial cushions. During fetal development, this structure does not completely fuse with the endocardial cushions, which results in atrial separation. 29. ANS: B PTS: 1 REF: Page 1195 MSC: The septum primum forms along the posterior wall of the common atrium and grows downward toward the septum secundum. The gap between the two structures, known as the ostium primum, normally closes by extensions from the endocardial cushions. 30. ANS: C PTS: 1 REF: Page 1196 MSC: The conal portion of the ventricular septum that separates the aorta from the pulmonary artery forms from the bulbus cordis. NURSINGTB.COM Chapter 35: Structure and Function of the Pulmonary System MULTIPLE CHOICE 1. What pulmonary defense mechanism propels a mucous blanket that entraps particles moving toward the oropharynx? a. Nasal turbinates c. Cilia b. Alveolar macrophages d. Irritant receptors on the nares The submucosal glands of the bronchial lining produce mucus, contributing to the mucous blanket that covers the bronchial epithelium. The ciliated epithelial cells rhythmically beat this mucous blanket toward the trachea and pharynx, where it can be swallowed or expectorated by coughing. This selection is the only option that accurately identifies the pulmonary defense mechanism described. PTS: 1 REF: Page 1229 2. Which term is used to identify the movement of gas and air into and out of the lungs? a. Perfusion c. Respiration b. Ventilation d. Diffusion Of the options available, ventilation is the only term used to identify the mechanical movement of gas or air into and out of the lungs. PTS: 1 REF: Page 12N3U2RSINGTB.COM 3. When an individual aspirates food particles, where would the nurse expect to hear decreased or absent breath sounds? a. Left lung c. Trachea b. Right lung d. Carina The right mainstem bronchus extends from the trachea more vertically than the left main bronchus; therefore aspirated fluids or foreign particles tend to enter the right lung rather than the left or any of the other locations listed. PTS: 1 REF: Page 1228 4. Aspiration is most likely to occur in the right mainstem bronchus because it: a. Extends vertically from the trachea. b. Is narrower than the left mainstem bronchus. c. Comes into contact with food and drink first. d. Is located at the site where the bronchi bifurcate. The right mainstem bronchus extends from the trachea more vertically than the left mainstem bronchus; therefore aspirated fluids or foreign particles tend to enter the right lung rather than the left. The size of both mainstems is equal. The trachea comes into contact with food and drink first, and the carina is the site where the bronchi bifurcate. PTS: 1 REF: Page 1228 5. Air passage among alveoli is collateral and evenly distributed because of the function of which structures? a. Type I alveolar cells c. Acinus pores b. Pores of Kohn d. Alveolar pores Tiny passages called pores of Kohn permit some air to pass through the septa from alveolus to alveolus, promoting collateral ventilation and even distribution of air among the alveoli. This selection is the only option that accurately describes the function that allows air passage among alveoli. PTS: 1 REF: Page 1229 6. Where in the lung does gas exchange occur? a. Trachea c. Alveolocapillary membrane b. Segmental bronchi d. Main bronchus Gas exchange occurs only across the alveolocapillary membrane. PTS: 1 REF: Page 1230 7. Surfactant produced by type II alveolar cells facilitates alveolar distention and ventilation by which mechanism? a. Decreasing thoracic compliancNeURSINGTB.COM b. Attracting water to the alveolar surface c. Decreasing surface tension in the alveoli d. Increasing surface tension in the alveoli Surfactant, a lipoprotein produced by type II alveolar cells, has a detergent-like effect that separates the liquid molecules, thereby decreasing alveolar surface tension. This selection is the only option that accurately describes the mechanism that allows surfactant to facilitate alveolar distention and ventilation. PTS: 1 REF: Pages 1235-1236 8. Which part of the brainstem provides basic automatic rhythm of respiration by sending efferent impulses to the diaphragm and intercostal muscles? a. Dorsal respiratory group (DRG) c. Pneumotaxic center b. Ventral respiratory group d. Apneustic center The basic automatic rhythm of respiration is set by the DRG, a cluster of inspiratory nerve cells located in the medulla that sends efferent impulses to the diaphragm and inspiratory intercostal muscles. This selection is the only option that accurately identifies the appropriate brainstem location. PTS: 1 REF: Page 1233 9. Which structures secrete surfactant? a. Type I alveolar cells c. Alveolar macrophages b. Type II alveolar cells d. Stretch receptors Two major types of epithelial cells appear in the alveolus. Type I alveolar cells provide structure, and type II alveolar cells secrete surfactant, a lipoprotein that coats the inner surface of the alveolus and facilitates its expansion during inspiration, lowers alveolar surface tension at end-expiration, and thereby prevents lung collapse. Neither alveolar macrophages nor stretch receptors secrete surfactant. PTS: 1 REF: Page 1229 10. Which structure is not associated with any lymphatic vessels? a. Trachea c. Acinus b. Bronchi d. Terminal bronchioles No lymphatic structures are located in the acinus. The other options are associated with lymphatic vessels. PTS: 1 REF: Page 1230 11. Which describes the pressure in the pleural space? a. Atmospheric c. Above atmospheric b. Below atmospheric d. Variable NURSINGTB.COM Pressure in the pleural space is usually negative or subatmospheric (4 to 10 mm Hg). This selection is the only option that accurately describes pleural space pressure. PTS: 1 REF: Page 1231 12. The adequacy of a person’s alveolar ventilation is assessed best by monitoring which mechanism? a. Ventilatory rate c. Respiratory effort b. Ventilatory pattern d. Arterial blood gas Observation of the ventilatory rate, pattern, or effort cannot determine the adequacy of alveolar ventilation. If a health care professional needs to determine the adequacy of ventilation, then an arterial blood gas analysis must be performed to measure partial pressure of arterial carbon dioxide (PaCO2). PTS: 1 REF: Page 1232 13. Which normal physiologic change occurs in the aging pulmonary system? a. Decreased flow resistance c. Stiffening of the chest wall b. Fewer alveoli d. Improved elastic recoil Normal alterations include (1) loss of elastic recoil, (2) stiffening of the chest wall, (3) alterations in gas exchange, and (4) increases in flow resistance (see Figure 34-18). The number of alveoli is not affected by age. PTS: 1 REF: Page 1244 14. How is most of the oxygen in the blood transported? a. Dissolved in plasma c. In the form of carbon dioxide (CO2) b. Bound to hemoglobin d. Bound to protein ANS: B Oxygen is transported in the blood in two forms. A small amount dissolves in plasma, and the remainder binds to hemoglobin molecules. The other options are not involved in this process. PTS: 1 REF: Page 1240 15. Stretch receptors and peripheral chemoreceptors send afferent impulses regarding ventilation to which location in the brain? a. Pneumotaxic center in the pons b. Apneustic center in the pons c. Dorsal respiratory group (DRG) in the medulla oblongata d. Ventral respiratory group (VRG) in the medulla oblongata The respiratory center is made up of several groups of neurons located bilaterally in the brainstem: the DRG, the VRG, the pneumotaxic center, and the apneustic center. Of the options available, only the DRG gNroUuRpSIiNnGthTeB.mCOedMulla oblongata receives afferent impulses in the situation described. PTS: 1 REF: Page 1234 16. Which substances cause airway epithelium to constrict? a. Epinephrine and acetylcholine c. Bradykinin and thromboxane A b. Histamine and prostaglandin d. Leukotrienes and prostacyclin Constriction occurs if the irritant receptors in the airway epithelium are stimulated by irritants in inspired air, by endogenous substances (e.g., histamine, serotonin, prostaglandins), by many drugs, and by humoral substances. Of the options available, only histamine and prostaglandin cause constriction. PTS: 1 REF: Page 1234 17. If a patient develops acidosis, the nurse would expect the oxyhemoglobin dissociation curve to react in which manner? a. Shift to the right, causing more oxygen (O2) to be released to the cells b. Shift to the left, allowing less O2 to be released to the cells c. Show no change, allowing the O2 concentration to remain stable d. Show dramatic fluctuation, allowing the O2 concentration to increase A shift to the right depicts hemoglobin’s decreased affinity for O2 or an increase in the ease with which oxyhemoglobin dissociates and O2 moves into the cells. The oxyhemoglobin dissociation curve is shifted to the right by acidosis (low pH) and hypercapnia (increased partial pressure of arterial carbon dioxide [PaCO2]). This selection is the only option that accurately identifies what will happen to the oxyhemoglobin dissociation curve if acidosis occurs. PTS: 1 REF: Pages 1241-1243 18. How is most carbon dioxide (CO2) in the blood transported? a. Attached to oxygen c. Combined with albumin b. In the form of bicarbonate d. Dissolved in the plasma Approximately 60% of the CO2 in venous blood and 90% of the CO2 in arterial blood are carried in the form of bicarbonate. PTS: 1 REF: Page 1243 19. The sternocleidomastoid and scalene muscles are referred to as which group? a. Diaphragmatic muscles c. Intercostal muscles b. Muscles of expiration d. Muscles of inspiration The accessory muscles of inspiration are the sternocleidomastoid and scalene muscles. These muscles are not associated with the other options. PTS: 1 REF: Page 12N3U5RSINGTB.COM 20. An increase in surface tension caused by decreased surfactant production results in which alteration? a. Decrease in alveolar macrophage production b. Increase in lung compliance c. Decrease in alveoli collapse d. Increase in alveoli fluid collection The decrease in surface tension caused by surfactant is also responsible for keeping the alveoli free of fluid. In the absence of surfactant, the surface tension tends to attract fluid into the alveoli. If surfactant production is disrupted or surfactant is not produced in adequate quantities, then the alveolar surface tension increases, causing alveolar collapse, decreased lung expansion, increased work of breathing, and severe gas-exchange abnormalities. The decrease in surface tension caused by surfactant is also responsible for keeping the alveoli free of fluid. The remaining options are not associated with decreased surfactant production. PTS: 1 REF: Pages 1235-1236 21. Decreased lung compliance means that the lungs are demonstrating which characteristic? a. Difficult deflation c. Stiffness b. Easy inflation d. Inability to diffuse oxygen A decrease in compliance indicates that the lungs or chest wall is abnormally stiff or difficult to inflate. This selection is the only option that accurately identifies the meaning of decreased compliance. PTS: 1 REF: Page 1236 22. The lung is innervated by the parasympathetic nervous system via which nerve? a. Vagus c. Brachial b. Phrenic d. Pectoral Fibers of the parasympathetic division of the autonomic nervous system (ANS) travel only in the vagus nerve to the lung. PTS: 1 REF: Page 1234 23. What event is characteristic of the function in Zone 1 of the lung? a. Blood flow through the pulmonary capillary bed increases in regular increments. b. Alveolar pressure is greater than venous pressure but not greater than arterial pressure. c. The capillary bed collapses, and normal blood flow ceases. d. Blood flows through Zone 1, but it is impeded to a certain extent by alveolar pressure. Alveolar pressure exceeds pulmonary arterial and venous pressures in Zone 1. The capillary bed collapses, and normaNlUbRloSoINdGfTloBw.COceMases. Zone II is the portion where alveolar pressure is greater than venous pressure but not greater than arterial pressure. Blood flows through zone II, but it is impeded to a certain extent by alveolar pressure. Zone II is normally above the level of the left atrium. In zone III, arterial and venous pressures are greater than alveolar pressure and blood flow is not affected by alveolar pressure. Zone III is in the base of the lung. Blood flow through the pulmonary capillary bed increases in regular increments from the apex to the base. PTS: 1 REF: Pages 1239-1240 24. Hypoventilation that results in the retention of carbon dioxide will stimulate which receptors in an attempt to maintain a normal homeostatic state? a. Irritant receptors c. Peripheral chemoreceptors b. Central chemoreceptors d. Stretch receptors Central chemoreceptors indirectly monitor arterial blood by sensing changes in the pH of cerebrospinal fluid (CSF). The central chemoreceptors are sensitive to very small changes in the pH of CSF (equivalent to a 1 to 2 mm Hg change in partial pressure of carbon dioxide [PCO2]) and are able to maintain a normal partial pressure of arterial carbon dioxide (PaCO2) under many different conditions, including strenuous exercise. This selection is the only option that accurately identifies the receptors that are associated with the retention of carbon dioxide. PTS: 1 REF: Page 1234 25. What is the most important cause of pulmonary artery constriction? a. Low alveolar partial pressure of arterial oxygen (PaO2) b. Hyperventilation c. Respiratory alkalosis d. Epinephrine The most important cause of pulmonary artery constriction is a low alveolar PaO2. PTS: 1 REF: Page 1230 26. Where does the tracheal bifurcation occur? a. Larynx c. Carina b. Bronchi d. Nasopharynx The trachea, which is supported by U-shaped cartilage, connects the larynx to the bronchi, the conducting airways of the lungs. The trachea divides into the two main airways, or bronchi, at the carina (see Figure 34-1). The division occurs only at the carina. PTS: 1 REF: Page 1228 27. How low must the partial pressure of arterial oxygen (PaO2) drop before the peripheral chemoreceptors influence ventilation? a. Below 100 mm Hg c. Below 70 mm Hg b. Below 80 mm Hg d. Below 60 mm Hg NURSINGTB.COM The PaO2 must drop well below normal (to approximately 60 mm Hg) before the peripheral chemoreceptors have much influence on ventilation. PTS: 1 REF: Page 1234 28. Which receptors are located in the smooth muscles of airways? a. Central chemoreceptors c. Peripheral chemoreceptors b. Stretch receptors d. J-receptors ANS: B Of the options available, only the stretch receptors are located in the smooth muscles of airways. PTS: 1 REF: Page 1234 29. Which receptors are located near the respiratory center? a. Peripheral chemoreceptors c. Central chemoreceptors b. Stretch receptors d. J-receptors Of the options available, only the central chemoreceptors are located near the respiratory center. PTS: 1 REF: Page 1234 30. Which receptors are located in the aortic bodies, aortic arch, and carotid bodies? a. Central chemoreceptors c. J-receptors b. Stretch receptors d. Peripheral chemoreceptors Of the options available, only the peripheral chemoreceptors are located in the aortic bodies, aortic arch, and carotid bodies at the bifurcation of the carotids, near the baroreceptors. PTS: 1 REF: Page 1234 31. What is the purpose of the spirometry measurement? a. To evaluate the cause of hypoxia b. To measure the volume and flow rate during forced expiration c. To measures the gas diffusion rate at the alveolocapillary membrane d. To determine pH and oxygen and carbon dioxide concentrations Spirometry measures volume and flow rate during forced expiration. The alveolar-arterial oxygen gradient is used to evaluate the cause of hypoxia. Diffusing capacity is a measure of the gas diffusion rate at the alveolocapillary membrane. Arterial blood gas analysis can be used to determine pH and oxygen and carbon dioxide concentrations. PTS: 1 REF: Page 1243 MULTIPLE RESPONSE NURSINGTB.COM 32. Which structures belong to the upper conduction airway? (Select all that apply.) a. Oropharynx b. Larynx c. Nasopharynx d. Trachea e. Bronchi , C The conducting airways are the portion of the pulmonary system that provides a passage for the movement of air into and out of the gas-exchange portions of the lung. The nasopharynx, oropharynx, and related structures are often called the upper airway. The remaining options are not considered to be included in the upper conduction airway. PTS: 1 REF: Pages 1225-1226 33. Regarding the respiratory process referred to as remodeling, which statements are true? (Select all that apply.) a. Remodeling involves the vascular walls. b. Scarring and thickening occurs during this respiratory process. c. Remodeling results in a permanent change. d. Pulmonary artery hypotension results. e. Remodeling increases blood flow resistance. , B, C, E Remodeling is a process by which the vascular wall becomes scarred and thickened, thus resulting in permanent decreases in luminal diameter, increased resistance to blood flow, and permanent pulmonary artery hypertension. PTS: 1 REF: Page 1232 | What's New box 34. What are the effects of aging on the pulmonary system? a. Decreased chest wall compliance b. Decreased lung recoil c. Reduced ventilatory reserve d. Decreased partial pressure of arterial oxygen (PaO2) e. Reduced respiratory rate , B, C, D Aging affects the mechanical aspects of ventilation by decreasing chest wall compliance and elastic recoil of the lungs. Changes in these elastic properties reduce ventilatory reserve. Aging causes the PaO2 to decrease but does not affect the partial pressure of arterial carbon dioxide (PaCO2) or respiratory rate. PTS: 1 REF: Pages 1244-1245 MATCHING Match the receptor with its function. A. Irritant receptors B. Stretch receptors C. J-receptors NURSINGTB.COM D. Peripheral chemoreceptors E. Central chemoreceptors 35. Initiates rapid, shallow breathing 36. Monitors pH, partial pressure of carbon dioxide (PaCO2), and partial pressure of oxygen (PaO2) in arterial blood 37. Initiates cough reflex 38. Senses pH of cerebrospinal fluid 39. Hering-Breuer expiratory reflex 35. ANS: C PTS: 1 REF: Page 1234 MSC: J-receptors are sensitive to increased pulmonary capillary pressure, which stimulates them to initiate rapid, shallow breathing; hypotension; and bradycardia. 36. ANS: D PTS: 1 REF: Page 1234 MSC: Although the peripheral chemoreceptors are sensitive to changes in PaCO2 and pH, they are primarily sensitive to oxygen levels in arterial blood (PaO2) and are responsible for all of the increase in ventilation that occurs in response to arterial hypoxemia. 37. ANS: A PTS: 1 REF: Page 1234 MSC: Irritant receptors are sensitive to noxious aerosols (vapors), gases, and particulate matter (e.g., inhaled dusts), which cause them to initiate the cough reflex. 38. ANS: E PTS: 1 REF: Page 1234 MSC: Central chemoreceptors monitor arterial blood indirectly by sensing changes in the pH of cerebrospinal fluid (CSF). 39. ANS: B PTS: 1 REF: Page 1234 MSC: Stretch receptors decrease ventilatory rate and volume when stimulated, an occurrence sometimes referred to as the Hering-Breuer expiratory reflex. NURSINGTB.COM Chapter 36: Alterations of Pulmonary Function MULTIPLE CHOICE 1. Besides dyspnea, what is the most common characteristic associated with pulmonary disease? a. Chest pain c. Cough b. Digit clubbing d. Hemoptysis Pulmonary disease is associated with many signs and symptoms, and their specific characteristics often help in identifying the underlying disorder. The most common characteristics are dyspnea and cough. Others include abnormal sputum, hemoptysis, altered breathing patterns, hypoventilation and hyperventilation, cyanosis, clubbing of the digits, and chest pain. PTS: 1 REF: Page 1248 2. Sitting up in a forward-leaning position generally relieves which breathing disorder? a. Hyperpnea c. Apnea b. Orthopnea d. Dyspnea on exertion Of the options available, only orthopnea is generally relieved by sitting up in a forward-leaning posture or supporting the upper body on several pillows. PTS: 1 REF: Page 12N4U9RSINGTB.COM 3. Kussmaul respirations as a respiratory pattern may be associated with which characteristic(s)? a. Alternating periods of deep and shallow breathing b. Pulmonary fibrosis c. Chronic obstructive pulmonary disease d. Slightly increased ventilatory rate, large tidal volumes, and no expiratory pause Kussmaul respirations are characterized by a slightly increased ventilatory rate, very large tidal volume, and no expiratory pause. Kussmaul respirations are not associated with any of the other options. PTS: 1 REF: Page 1249 4. Respirations that are characterized by alternating periods of deep and shallow breathing are a result of which respiratory mechanism? a. Decreased blood flow to the medulla oblongata b. Increased partial pressure of arterial carbon dioxide (PaCO2), decreased pH, and decreased partial pressure of arterial oxygen (PaO2) c. Stimulation of stretch or J-receptors d. Fatigue of the intercostal muscles and diaphragm Alternating periods of deep and shallow breathing are characteristic of Cheyne-Stokes respirations and are the result of any condition that slows the blood flow to the brainstem, which in turn slows impulses that send information to the respiratory centers of the brainstem. None of the remaining options are responsible for the described breathing pattern. PTS: 1 REF: Page 1250 5. With a total hemoglobin of 9 g/dl, how many grams per deciliter of hemoglobin must become desaturated for cyanosis to occur? a. 3 c. 7 b. 5 d. 9 Cyanosis generally develops when 5 g/dl of hemoglobin is desaturated, regardless of hemoglobin concentration. PTS: 1 REF: Page 1250 6. Which statement is true regarding ventilation? a. Hypoventilation causes hypocapnia. b. Hyperventilation causes hypercapnia. c. Hyperventilation causes hypocapnia. d. Hyperventilation results in an increased partial pressure of arterial carbon dioxide (PaCO2). Hyperventilation is alveolar ventilNaUtiRonSItNhGaTt Bex.CcOeeMds metabolic demands. The lungs remove carbon dioxide at a faster rate than produced by cellular metabolism, resulting in decreased PaCO2 or hypocapnia. None of the remaining options are accurate statements. PTS: 1 REF: Page 1250 7. What term is used to describe the selective bulbous enlargement of the distal segment of a digit that is commonly associated with diseases that interfere with oxygenation of the blood? a. Edema c. Angling b. Clubbing d. Osteoarthropathy Clubbing is the selective bulbous enlargement of the end (distal segment) of a digit (finger or toe) (see Figure 35-1) and is commonly associated with diseases that interfere with oxygenation, such as bronchiectasis, cystic fibrosis, pulmonary fibrosis, lung abscess, and congenital heart disease. None of the remaining options are terms used to identify the condition described. PTS: 1 REF: Page 1250 8. Pulmonary edema and pulmonary fibrosis cause hypoxemia by which mechanism? a. Creating alveolar dead space b. Decreasing the oxygen in inspired gas c. Creating a right-to-left shunt d. Impairing alveolocapillary membrane diffusion Diffusion of oxygen through the alveolocapillary membrane is impaired if the alveolocapillary membrane is thickened or if the surface area available for diffusion is decreased. Abnormal thickness, as occurs with edema (tissue swelling) and fibrosis (formation of fibrous lesions), increases the time required for diffusion across the alveolocapillary membrane. None of the remaining options accurately describes the mechanism that triggers hypoxemia as a result of pulmonary edema or pulmonary fibrosis. PTS: 1 REF: Pages 1251-1252 9. High altitudes may produce hypoxemia through which mechanism? a. Shunting c. Decreased inspired oxygen b. Hypoventilation d. Diffusion abnormalities The presence of adequate oxygen content of the inspired air is the first factor. Oxygen content is lessened at high altitudes. At high altitudes none of the remaining options would be the cause of hypoxemia. PTS: 1 REF: Page 1251 10. Which condition is capable of producing alveolar dead space? a. Pulmonary edema c. Atelectasis b. Pulmonary emboli d. Pneumonia NURSINGTB.COM A pulmonary embolus that impairs blood flow to a segment of the lung results in an area where alveoli are ventilated but not perfused, which causes alveolar dead space. Alveolar dead space is not the result of any of the remaining options. PTS: 1 REF: Page 1252 11. What is the most common cause of pulmonary edema? a. Right-sided heart failure c. Mitral valve prolapse b. Left-sided heart failure d. Aortic stenosis The most common cause of pulmonary edema is heart disease. When the left ventricle fails, filling pressures on the left side of the heart increase and cause a concomitant increase in pulmonary capillary hydrostatic pressure. The remaining options are not common triggers for pulmonary edema. PTS: 1 REF: Page 1260 12. Pulmonary edema usually begins to develop at a pulmonary capillary wedge pressure or left atrial pressure of how many millimeters of mercury (mm Hg)? a. 10 c. 30 b. 20 d. 40 Pulmonary edema usually begins to develop at a pulmonary capillary wedge pressure or left atrial pressure of 20 mm Hg. PTS: 1 REF: Page 1260 13. The collapse of lung tissue caused by the lack of collateral ventilation through the pores of Kohn is referred to as what type of atelectasis? a. Compression c. Absorption b. Perfusion d. Hypoventilation Absorption atelectasis is a result of the gradual absorption of air from obstructed or hypoventilated alveoli or from inhalation of concentrated oxygen or anesthetic agents. The other forms of atelectasis are not a result of the described mechanism. PTS: 1 REF: Pages 1256-1257 | Figure 35-5 14. In what form of bronchiectasis do both constrictions and dilations deform the bronchi? a. Varicose c. Cylindric b. Symmetric d. Saccular Varicose bronchiectasis exists when both constrictions and dilations deform the bronchi. None of the other options involve both constriction and dilation, resulting in bronchi deformity. PTS: 1 REF: Pages 1256-1258 NURSINGTB.COM 15. Which pleural abnormality involves a site of pleural rupture that acts as a one-way valve, permitting air to enter on inspiration but preventing its escape by closing during expiration? a. Spontaneous pneumothorax c. Open pneumothorax b. Tension pneumothorax d. Secondary pneumothorax In tension pneumothorax, the site of pleural rupture acts as a one-way valve, permitting air to enter on inspiration but preventing its escape by closing up during expiration. As more and more air enters the pleural space, air pressure in the pneumothorax begins to exceed barometric pressure. None of the other options result from the pathologic condition described. PTS: 1 REF: Page 1254 16. In which type of pleural effusion does the fluid become watery and diffuse out of the capillaries as a result of increased blood pressure or decreased capillary oncotic pressure? a. Exudative c. Transudative b. Purulent d. Large In transudative pleural effusion, the fluid, or transudate, is watery and diffuses out of the capillaries as a result of disorders that increase intravascular hydrostatic pressure or decrease capillary oncotic pressure. The described mechanism is not associated with the other forms of pleural effusion. PTS: 1 REF: Page 1254 17. Which condition involves an abnormally enlarged gas-exchange system and the destruction of the lung’s alveolar walls? a. Transudative effusion c. Exudative effusion b. Emphysema d. Abscess Emphysema is abnormal permanent enlargement of gas-exchange airways (acini) accompanied by the destruction of alveolar walls without obvious fibrosis. The described mechanism is not associated with the other options. PTS: 1 REF: Page 1268 18. Which term is used to identify a circumscribed area of suppuration and destruction of lung parenchyma? a. Consolidation c. Empyema b. Cavitation d. Abscess An abscess is a circumscribed area of suppuration and destruction of lung parenchyma. The described pathologic abnormality is not associated with the other options. NURSINGTB.COM PTS: 1 REF: Page 1274 19. Which condition is not a cause of chest wall restriction? a. Pneumothorax c. Gross obesity b. Severe kyphoscoliosis d. Neuromuscular disease Unlike the other options that result in chest wall restriction, a pneumothorax is the presence of air or gas in the pleural space caused by a rupture in the visceral pleura (which surrounds the lungs) or the parietal pleura and chest wall. PTS: 1 REF: Page 1254 20. What causes pneumoconiosis? a. Pneumococci bacteria c. Exposure to asbestos b. Inhalation of inorganic dust particles d. Inhalation of cigarette smoke Pneumoconiosis represents any change in the lung caused by the inhalation of inorganic dust particles, which usually occurs in the workplace. Pneumoconiosis is not a result of any of the other options. PTS: 1 REF: Page 1259 21. Which condition is a fulminant form of respiratory failure characterized by acute lung inflammation and diffuse alveolocapillary injury? a. Acute respiratory distress syndrome (ARDS) b. Pneumonia c. Pulmonary emboli d. Acute pulmonary edema ARDS is a fulminant form of respiratory failure characterized by acute lung inflammation and diffuse alveolocapillary injury. The described pathologic characteristics are not associated with the other options. PTS: 1 REF: Page 1261 22. Which structure(s) in acute respiratory distress syndrome (ARDS) release inflammatory mediators such as proteolytic enzymes, oxygen-free radicals, prostaglandins, leukotrienes, and platelet-activating factor? a. Complement cascade c. Macrophages b. Mast cells d. Neutrophils The role of neutrophils is central to the development of ARDS. Activated neutrophils release a battery of inflammatory mediators, among them proteolytic enzymes, oxygen-free radicals (superoxide radicals, hydrogen peroxide, hydroxyl radicals), arachidonic acid metabolites (prostaglandins, thromboxanes, leukotrienes), and platelet-activating factor. These mediators cause extensive damage to the alveolocapillary membrane and greatly increase capillary membrane permeability. The described responses are not associated with the other oNpUtiRonSIsN. GTB.COM PTS: 1 REF: Page 1261 23. Pulmonary edema in acute respiratory distress syndrome (ARDS) is the result of an increase in: a. Levels of serum sodium and water c. Capillary hydrostatic pressure b. Capillary permeability d. Oncotic pressure Increased capillary permeability, a hallmark of ARDS, allows fluids, proteins, and blood cells to leak from the capillary bed into the pulmonary interstitium and alveoli. The resulting pulmonary edema and hemorrhage severely reduce lung compliance and impair alveolar ventilation. The other options would not trigger ARDS-associated pulmonary edema. PTS: 1 REF: Page 1261 24. In acute respiratory distress syndrome (ARDS), alveoli and respiratory bronchioles fill with fluid as a result of which mechanism? a. Compression on the pores of Kohn, thus preventing collateral ventilation b. Increased capillary permeability, which causes alveoli and respiratory bronchioles to fill with fluid c. Inactivation of surfactant and the impairment of type II alveolar cells d. Increased capillary hydrostatic pressure that forces fluid into the alveoli and respiratory bronchioles Lung inflammation and injury damage the alveolar epithelium and the vascular endothelium. Surfactant is inactivated, and its production by type II alveolar cells is impaired as alveoli and respiratory bronchioles fill with fluid or collapse. The other options would not trigger the described response. PTS: 1 REF: Page 1261 25. Which type of pulmonary disease requires more force to expire a volume of air? a. Restrictive c. Acute b. Obstructive d. Communicable Obstructive pulmonary disease is characterized by airway obstruction that is worse with expiration. Either more force (i.e., the use of accessory muscles of expiration) or more time is required to expire a given volume of air. The other options are not associated with a need for an increase of force to expire air. PTS: 1 REF: Page 1263 26. Which immunoglobulin (Ig) may contribute to the pathophysiologic characteristics of asthma? a. IgA c. IgG b. IgE d. IgM NURSINGTB.COM Asthma is a familial disorder, and more than 100 genes have been identified that may play a role in the susceptibility of and the pathogenetic mechanisms that cause asthma, including those that influence the production of interleukin (IL)–4, IL-5, and IL-13; IgE; eosinophils; mast cells; adrenergic receptors; and leukotrienes. The pathophysiologic characteristics of asthma are not associated with the other immunoglobulins. PTS: 1 REF: Pages 1263-1264 27. Which statement about the late asthmatic response is true? a. Norepinephrine causes bronchial smooth muscle contraction and mucus secretion. b. The release of toxic neuropeptides contributes to increased bronchial hyperresponsiveness. c. The release of epinephrine causes bronchial smooth muscle contraction and increases capillary permeability. d. Immunoglobulin G initiates the complement cascade and causes smooth muscle contraction and increased capillary permeability. The late asthmatic response begins 4 to 8 hours after the early response when the release of toxic neuropeptides contributes to increased bronchial hyperresponsiveness. This selection is the only option associated with the late asthmatic response. PTS: 1 REF: Page 1264 28. Clinical manifestations of inspiratory and expiratory wheezing, dyspnea, nonproductive cough, and tachypnea are indicative of which condition? a. Chronic bronchitis c. Pneumonia b. Emphysema d. Asthma At the beginning of an attack, the individual experiences chest constriction, expiratory wheezing, dyspnea, nonproductive coughing, prolonged expiration, tachycardia, and tachypnea. Severe attacks involve the use of accessory muscles of respiration, and wheezing is heard during both inspiration and expiration. The presentations of none of the other options are consistent with the described symptoms. PTS: 1 REF: Page 1264 | Page 1266 29. The most successful treatment for chronic asthma begins with which action? a. Avoidance of the causative agent b. Administration of broad-spectrum antibiotics c. Administration of drugs that reduce bronchospasm d. Administration of drugs that decrease airway inflammation Chronic management of asthma begins with the avoidance of allergens and other triggers. The effectiveness of the other options is reliant on the avoidance of triggers. PTS: 1 REF: Page 1266 30. Which factor contributes to the prNodUuRcStIiNonGToBf .mCOuMcus associated with chronic bronchitis? a. Airway injury c. Increased Goblet cell size b. Pulmonary infection d. Bronchospasms Continual bronchial inflammation causes bronchial edema and increases the size and number of mucous glands and goblet cells in the airway epithelium. Thick, tenacious mucus is produced and cannot be cleared because of impaired ciliary function (see Figure 35-13). The lung’s defense mechanisms are therefore compromised, increasing a susceptibility to pulmonary infection, which contributes to airway injury. Frequent infectious exacerbations are complicated by bronchospasm with dyspnea and productive cough. PTS: 1 REF: Page 1267 31. Clinical manifestations of decreased exercise tolerance, wheezing, shortness of breath, and productive cough are indicative of which respiratory disorder? a. Chronic bronchitis c. Pneumonia b. Emphysema d. Asthma The symptoms that lead individuals with chronic bronchitis to seek medical care include decreased exercise tolerance, wheezing, and shortness of breath. Individuals usually have a productive cough (“smoker’s cough”). The described symptoms are not associated with any of the other options. PTS: 1 REF: Page 1267 32. Clinical manifestations that include unexplained weight loss, dyspnea on exertion, use of accessory muscles, and tachypnea with prolonged expiration are indicative of which respiratory disorder? a. Chronic bronchitis c. Pneumonia b. Emphysema d. Asthma Individuals with emphysema usually have dyspnea on exertion that later progresses to significant dyspnea, even at rest (see Table 35-3). Little coughing and very little sputum are produced. The individual is often thin, has tachypnea with prolonged expiration, and must use accessory muscles for ventilation. The anteroposterior diameter of the chest is increased (barrel chest), and the chest has a hyperresonant sound with percussion. The described symptoms are not associated with any of the other options. PTS: 1 REF: Page 1270 33. Which of the following is the most common route of lower respiratory tract infection? a. Aspiration of oropharyngeal secretions b. Inhalation of microorganisms c. Microorganisms spread to the lung via blood d. Poor mucous membrane protection Aspiration of oropharyngeal secretions is the most common route of lower respiratory tract infection; thus the nasopharynx anNdUoRrSoIpNhGaTryBn.CxOcMonstitute the first line of defense for most infectious agents. The other options are not common routes of lower respiratory tract infections. PTS: 1 REF: Page 1271 34. What is the initial step in the management of emphysema? a. Inhaled anticholinergic agents c. Cessation of smoking b. Beta agonists d. Surgical reduction of lung volume Chronic management of emphysema begins with smoking cessation. Pharmacologic management includes inhaled anticholinergic agents, and beta agonists should be prescribed. Pulmonary rehabilitation, improved nutrition, and breathing techniques all can improve symptoms. Oxygen therapy is indicated in chronic hypoxemia but must be administered with care. In selected patients, lung volume reduction surgery or transplantation can be considered. PTS: 1 REF: Pages 1270-1271 35. In tuberculosis, the body walls off the bacilli in a tubercle by stimulating which action? a. Macrophages that release tumor necrosis factor–alpha (TNF- b. Phagocytosis by neutrophils and eosinophils c. Formation of immunoglobulin G to initiate the complement cascade d. Apoptotic infected macrophages that activate cytotoxic T cells In defense, macrophages and lymphocytes release interferon, which inhibits the replication of the microorganism and stimulates more macrophages to attack the bacterium. Apoptotic infected macrophages can also activate cytotoxic T cells (cluster of differentiation [CD] 8). Tuberculosis does not trigger the mechanisms described by the other options. PTS: 1 REF: Pages 1273-1274 36. The progression of chronic bronchitis is best halted by which intervention? a. Regular use of bronchodilators b. Smoking cessation c. Postural chest drainage techniques d. Identification of early signs of infection By the time an individual seeks medical care for symptoms, considerable airway damage is present. If the individual stops smoking, then disease progression can be halted. If smoking is stopped before symptoms occur, then the risk of chronic bronchitis decreases considerably and eventually reaches that of nonsmokers. The other interventions, although appropriate, are not directed toward halting the progression of the disease process. PTS: 1 REF: Page 1267 37. Clinical manifestations of inspiratory crackles, increased tactile fremitus, egophony, and whispered pectoriloquy are indicative of which respiratory condition? a. Chronic bronchitis NURSINGTcB..COPMneumonia b. Emphysema d. Asthma Physical examination may reveal signs of pulmonary consolidation, such as inspiratory crackles, increased tactile fremitus, egophony, and whispered pectoriloquy, which support a diagnosis of pneumonia. The presentations of the other options are not consistent with the described symptoms. PTS: 1 REF: Page 1273 38. Pulmonary artery hypertension (PAH) results from which alteration? a. Narrowed pulmonary capillaries c. Destruction of alveoli b. Narrowed bronchi and bronchioles d. Ischemia of the myocardium PAH is characterized by endothelial dysfunction with an overproduction of vasoconstrictors (e.g., thromboxane, endothelin) and decreased production of vasodilators (e.g., nitric oxide, prostacyclin), resulting in narrowed pulmonary capillaries. None of the remaining options result in pulmonary hypertension. PTS: 1 REF: Page 1277 39. Squamous cell carcinoma of the lung is best described as a tumor that causes which alterations? a. Abscesses and ectopic hormone production b. Airway obstruction and atelectasis c. Pleural effusion and shortness of breath d. Chest wall pain and early metastasis Typically, the tumors are centrally located near the hila and project into bronchi. Because of this central location, nonproductive cough or hemoptysis is common. Pneumonia and atelectasis are often associated with squamous cell carcinoma. Chest pain is a late symptom associated with large tumors. These tumors can remain fairly well localized and tend not to metastasize until late in the course of the disease. Squamous cell carcinomas are not associated with any of the other options. PTS: 1 REF: Pages 1280-1281 | Table 35-4 40. What medical term is used to identify the accumulation of air in the pleural space? a. Flail chest c. Pleural effusion b. Pneumothorax d. Exudate effusion Pneumothorax is the presence of air or gas in the pleural space caused by a rupture in the visceral pleura (which surrounds the lungs) or the parietal pleura and chest wall. The condition is not identified by any of the other options. PTS: 1 REF: Page 1254 41. What medical term is used to identify the presence of pus in the pleural space? a. Plural effusion NURSINGTcB..COEMmpyema b. Asthma d. Pneumonia Empyema is the presence of pus in the pleural space. This condition is not identified by any of the other options. PTS: 1 REF: Page 1255 42. Fluid in the pleural space characterizes which condition? a. Pleural effusion c. Bronchiectasis b. Atelectasis d. Ischemia Pleural effusion is the presence of fluid in the pleural space. This condition is not identified by any of the other options. PTS: 1 REF: Page 1254 43. Which statement is true regarding hypoxemia? a. Hypoxemia results in the increased oxygenation of arterial blood. b. Respiratory alterations cause hypoxemia. c. Hypoxemia results in the decreased oxygenation of tissue cells. d. Various system changes cause hypoxemia. Hypoxemia, or reduced oxygenation of arterial blood (PaO2), is caused by respiratory alterations, whereas hypoxia, or reduced oxygenation of cells in tissues, may be caused by alterations of other systems as well. PTS: 1 REF: Page 1251 44. Which medication classification is generally included in the treatment of silicosis? a. Corticosteroids c. Bronchodilators b. Antibiotics d. Expectorants No specific treatment exists for silicosis, although corticosteroids may produce some improvement in the early, more acute stages. The other options are not generally prescribed. PTS: 1 REF: Page 1259 45. What medical term is used for a condition that results from pulmonary hypertension, creating chronic pressure overload in the right ventricle? a. Hypoxemia c. Bronchiectasis b. Hypoxia d. Cor pulmonale Cor pulmonale develops as pulmonary hypertension and creates chronic pressure overload in the right ventricle similar to that created in the left ventricle by systemic hypertension. None of the other options identify the condition. PTS: 1 REF: Page 12N7U8RSINGTB.COM MULTIPLE RESPONSE 46. What are the causes of dyspnea? (Select all that apply.) a. Decreased pH, increased partial pressure of arterial carbon dioxide (PaCO2) and decreased partial pressure of arterial oxygen (PaO2) b. Decreased blood flow to the medulla oblongata c. Stimulation of stretch or J-receptors d. Presence of anxiety e. Presence of pain , C, D Dyspnea can be triggered by decreased pH, increased PaCO2, and decreased PaO2. Stimulation of either stretch or J-receptors is also known as a cause of dyspnea. Dyspnea may be the result of pulmonary disease or many other conditions, such as pain, heart disease, trauma, and anxiety. No data are available to support the role of decreased blood flow to the medulla oblongata as being a cause of dyspnea. PTS: 1 REF: Pages 1248-1249 47. Which inflammatory mediators are produced in asthma? (Select all that apply.) a. Histamine b. Bradykinin c. Leukotrienes d. Prostaglandins e. Neutrophil proteases , B, C, D A large number of inflammatory mediators, such as histamine, prostaglandins, and leukotrienes, are produced by asthma. Neutrophil proteases are not produced in relationship to asthma. PTS: 1 REF: Page 1265 | Figure 35-12 48. Which clinical manifestation is associated with pulmonary hypertension? (Select all that apply.) a. Systemic blood pressure greater than 130/90 mm Hg b. Rhonchi bilaterally c. Dyspnea on exertion d. Peripheral edema e. Jugular venous distention , D, E Symptoms of fatigue, chest discomfort, tachypnea, and dyspnea on exertion, palpitations, and cough are common. Examination may reveal peripheral edema, jugular venous distention, a precordial heave, and accentuation of the pulmonary compartment of the second heart sound. Neither rhonchi nor a systemic blood pressure of 130/90 mm Hg are associated with pulmonary hypertension. PTS: 1 REF: Pages 1277-1278 NURSINGTB.COM 49. Which statements are true regarding exudative effusion? (Select all that apply.) a. Exudative effusion contains high concentrations of white blood cells. b. Exudative effusion produces a very thick exudate. c. Exudative effusion may occur in response to an inflammatory process. d. The presence of a malignant cancer can trigger exudative effusion. e. Exudative effusion is a result of increased capillary permeability. , C, D, E Exudative effusion is less watery and contains high concentrations of white blood cells and plasma proteins. Exudative effusion occurs in response to inflammation, infection, or malignancy and involves inflammatory processes that increase capillary permeability. PTS: 1 REF: Page 1254 50. Which characteristics are symptomatic of a flail chest? (Select all that apply.) a. Involves the fracture of several consecutive ribs. b. Involves multiple fractures to individual ribs. c. Can involve the fracture of the sternum. d. Is generally a result of the inflammatory process. e. Is more common among the older adult population. , B, C A flail chest results from the fracture of several consecutive ribs in more than one place or the fracture of the sternum and several consecutive ribs. Age and inflammation are not generally considered factors in this disorder. PTS: 1 REF: Page 1253 51. Which statements regarding Mycobacterium tuberculosis are true regarding the bacilli’s ability to go into dormancy? (Select all that apply.) a. Neutrophils and macrophages all play a role in its dormancy. b. Mycobacterium tuberculosis is capable of dormancy but for only a short period. c. The immune system is the controlling factor regarding its length of dormancy. d. The bacilli are sealed off in tubercles to allow for dormancy. e. An attack by lymphocytes brings the bacilli out of their dormant state. , C, D Neutrophils, lymphocytes, and macrophages seal off the colonies of bacilli, forming a granulomatous lesion called a tubercle. Once the bacilli are isolated in tubercles and immunity develops, tuberculosis may remain dormant for life. If the immune system is impaired, however, or if live bacilli escape into the bronchi, active disease occurs and may spread through the blood and lymphatic system to other organs. This microorganism can remain dormant for extended periods. Reverting from dormancy is not related to a lymphocyte attack. PTS: 1 REF: Pages 1273-1274 MATCHING NURSINGTB.COM Match the descriptions with the corresponding terms. A. Passage of fluid and solid particles into the lung B. Inflammatory obstruction of small airways C. Excessive amount of connective tissue in the lung D. Lung tissue collapse E. Abnormal dilation of the bronchi 52. Pulmonary fibrosis 53. Atelectasis 54. Bronchiectasis 55. Aspiration 56. Bronchiolitis 52. ANS: MSC: C PTS: 1 REF: Page 1258 Pulmonary fibrosis is an excessive amount of fibrous or connective tissue in the lung. 53. ANS: MSC: D PTS: 1 REF: Page 1256 Atelectasis is the collapse of lung tissue. 54. ANS: MSC: E PTS: 1 REF: Page 1256 Bronchiectasis is persistent abnormal dilation of the bronchi. 55. ANS: MSC: A PTS: 1 REF: Page 1255 Aspiration is the passage of fluid and solid particles into the lung. 56. ANS: MSC: B PTS: 1 REF: Page 1258 Bronchiolitis is inflammation of the small airways or bronchioles. Chapter 37: Alterations of Pulmonary Function in Children MULTIPLE CHOICE 1. How does chest wall compliance in an infant differ from that of an adult? a. An adult’s chest wall compliance is lower than an infant’s. b. An adult’s chest wall compliance is higher than an infant’s. c. An adult’s chest wall compliance is the same as an infant’s. d. An adult’s chest wall compliance is dissimilar to that of an infant’s. Chest wall compliance is higher in infants than it is in adults, particularly in premature infants. PTS: 1 REF: Page 1292 2. Why is nasal congestion a serious threat to young infants? a. Infants are obligatory nose breathers. b. Their noses are small in diameter. c. Infants become dehydrated when mouth breathing. d. Their epiglottis is proportionally greater than the epiglottis of an adult’s. Infants up to 2 to 3 months of age are obligatory nose breathers and are unable to breathe in through their mouths. Nasal congestion is therefore a serious threat to a young infant. This selection is the only option that accurately describes why nasal congestion is a serious threat to young infants. NURSINGTB.COM PTS: 1 REF: Page 1290 3. The risk for respiratory distress syndrome (RDS) decreases for premature infants when they are born between how many weeks of gestation? a. 16 and 20 c. 24 and 30 b. 20 and 24 d. 30 and 36 Surfactant is secreted into fetal airways between 30 and 36 weeks. The other options are not true regarding the timeframe when the risk for RDS decreases. PTS: 1 REF: Page 1292 4. Which type of croup is most common? a. Bacterial c. Fungal b. Viral d. Autoimmune In 85% of children with croup, a virus is the cause, most commonly parainfluenza. However, other viruses such as influenza A or respiratory syncytial virus (RSV) also can cause croup. PTS: 1 REF: Pages 1295-1296 5. What is the chief predisposing factor for respiratory distress syndrome (RDS) of the newborn? a. Low birth weight b. Alcohol consumption during pregnancy c. Premature birth d. Smoking during pregnancy RDS of the newborn, also known as hyaline membrane disease (HMD), is a major cause of morbidity and mortality in premature newborns. None of the other options are considered the chief predisposing factors for RDS. PTS: 1 REF: Page 1301 6. What is the primary cause of respiratory distress syndrome (RDS) of the newborn? a. Immature immune system c. Surfactant deficiency b. Small alveoli d. Anemia ANS: C RDS is primarily caused by surfactant deficiency and secondarily by a deficiency in alveolar surface area for gas exchange. None of the other options are related to the cause of RDS. PTS: 1 REF: Page 1301 7. What is the primary problem resulting from respiratory distress syndrome (RDS) of the newborn? NURSINGTB.COM a. Consolidation c. Atelectasis b. Pulmonary edema d. Bronchiolar plugging The primary problem is atelectasis, which causes significant hypoxemia and is difficult for the neonate to overcome because a significant negative inspiratory pressure is required to open the alveoli with each breath. None of the other options are considered a primary problem associated with RDS. PTS: 1 REF: Page 1301 8. Which option shows the correct sequence of events after atelectasis develops in respiratory distress syndrome of the newborn? a. Increased pulmonary vascular resistance, atelectasis, hypoperfusion b. Hypoxic vasoconstriction, right-to-left shunt hypoperfusion c. Respiratory acidosis, hypoxemia, hypercapnia d. Right-to-left shunt, hypoxic vasoconstriction, hypoperfusion Atelectasis results in a decrease in tidal volume, causing alveolar hypoventilation and hypercapnia. Hypoxia and hypercapnia cause pulmonary vasoconstriction, which increases intrapulmonary resistance and shunting. This results in hypoperfusion of the lung and a decrease in effective pulmonary blood flow. This selection is the only option that identifies the correct sequence of events. PTS: 1 REF: Page 1301 9. Which statement about the advances in the treatment of respiratory distress syndrome (RDS) of the newborn is incorrect? a. Administering glucocorticoids to women in preterm labor accelerates the maturation of the fetus’s lungs. b. Administering oxygen to mothers during preterm labor increases their arterial oxygen before the birth of the fetus. c. Treatment includes the instillation of exogenous surfactant down an endotracheal tube of infants weighing less than 1000 g. d. Using continuous positive airway pressure (CPAP) supports the infant’s respiratory function. Administering oxygen to the mother is not a valid treatment of RDS. The other statements provide correct information regarding RDS. PTS: 1 REF: Pages 1301-1303 10. Bronchiolitis tends to occur during the first years of life and is most often caused by what type of infection? a. Respiratory syncytial virus (RSV) c. Adenoviruses b. Influenzavirus d. Rhinovirus The most common associated pathogen is RSV, but bronchiolitis may also be associated with adenovirus, rhinovirus, influeNnUzRaS, IpNaGraTiBn.fCluOeMnza virus (PIV), and Mycoplasma pneumoniae. PTS: 1 REF: Page 1305 11. Which immunoglobulin (Ig) is present in childhood asthma? a. IgM c. IgE b. IgG d. IgA Included in the long list of asthma-associated genes are those that code for increased levels of immune and inflammatory mediators (e.g., interleukin [IL]–4, IgE, leukotrienes), nitric oxide, and transmembrane proteins in the endoplasmic reticulum. None of the other options are associated with childhood asthma. PTS: 1 REF: Pages 1308-1309 12. Which T-lymphocyte phenotype is the key determinant of childhood asthma? a. Cluster of differentiation (CD) 4 T-helper Th1 lymphocytes b. CD4 T-helper Th2 lymphocytes c. CD8 cytotoxic T lymphocytes d. Memory T lymphocytes Asthma develops because the Th2 response (in which CD4 T-helper cells produce specific cytokines, such as interleukin [IL]–4, IL-5, and IL-13) promotes an atopic and allergic response in the airways. This selection is the only option that accurately identifies the appropriate T-lymphocyte phenotype. PTS: 1 REF: Page 1309 13. Which cytokines activated in childhood asthma produce an allergic response? a. Interleukin (IL)–1, IL-2, and interferon-alpha (IFN-) b. IL-8, IL-12, and tumor necrosis factor-alpha (TNF-) c. IL-4, IL-10, and colony-stimulating factor (CSF) d. IL-4, IL-5, and IL-13 Related to asthma, IL-4 and IL-13 are particularly important for B-cell switching to favor immunoglobulin E (IgE) production, and IL-5 is crucial for local differentiation and enhanced survival of eosinophils within the airways. This selection is the only option that accurately describes how cytokines produce a childhood asthmatic response. PTS: 1 REF: Page 1309 14. Which statement accurately describes childhood asthma? a. An obstructive airway disease characterized by reversible airflow obstruction, bronchial hyperreactivity, and inflammation b. A pulmonary disease characterized by severe hypoxemia, decreased pulmonary compliance, and diffuse densities on chest x-ray imaging c. A pulmonary disorder involvinNgURanSIaNbGnToBrm.CaOlMexpression of a protein, producing viscous mucus that lines the airways, pancreas, sweat ducts, and vas deferens d. An obstructive airway disease characterized by atelectasis and increased pulmonary resistance as a result of a surfactant deficiency Asthma is an obstructive airway disease characterized by reversible airflow obstruction, bronchial hyperreactivity, and inflammation. This selection is the only option that accurately describes childhood asthma. PTS: 1 REF: Page 1308 15. Which criterion is used to confirm a diagnosis of asthma in an 8-year-old child? a. Parental history of asthma b. Serum testing that confirms increased immunoglobulin E (IgE) and eosinophil levels c. Reduced expiratory flow rates confirmed by spirometry testing d. Improvement on a trial of asthma medication Confirmation of the diagnosis of asthma relies on pulmonary function testing using spirometry, which can be accomplished only after the child is 5 to 6 years of age. Reduced expiratory flow rates that are reversible in response to an inhaled bronchodilator would be characteristic abnormalities. For younger children, an empiric trial of asthma medications is commonly initiated. The remaining options are major historical and physical factors that contribute but do not confirm the diagnosis of asthma in children. PTS: 1 REF: Pages 1309-1310 16. Which statement best describes acute respiratory distress syndrome (ARDS)? a. An obstructive airway disease characterized by reversible airflow obstruction, bronchial hyperreactivity, and inflammation b. A pulmonary disease characterized by severe hypoxemia, decreased pulmonary compliance, and the presence of bilateral infiltrates on chest x-ray imaging c. A respiratory disorder involving an abnormal expression of a protein producing viscous mucus that lines the airways, pancreas, sweat ducts, and vas deferens d. A pulmonary disorder characterized by atelectasis and increased pulmonary resistance as a result of a surfactant deficiency ARDS is a condition that can result from either a direct or indirect pulmonary insult. It is defined as respiratory failure of acute onset characterized by severe hypoxemia that is refractory to treatment with supplemental oxygen, bilateral infiltrates on chest x-ray imaging, and no evidence of heart failure, as well as decreased pulmonary compliance. This selection is the only option that accurately describes ARDS. PTS: 1 REF: Page 13N1U0RSINGTB.COM 17. When considering the signs and symptoms of acute respiratory distress syndrome (ARDS), the absence of which condition is considered characteristic? a. Progressive respiratory distress c. Decreased pulmonary compliance b. Bilateral infiltrates d. Heart failure ARDS is characterized by progressive respiratory distress, severe hypoxemia refractory to treatment with supplemental oxygen, decreased pulmonary compliance, bilateral infiltrates on chest x-ray imaging, and no evidence of heart failure. PTS: 1 REF: Page 1310 18. Examination of the throat in a child demonstrating signs and symptoms of acute epiglottitis may contribute to which life-threatening complication? a. Retropharyngeal abscess c. Rupturing of the tonsils b. Laryngospasms d. Gagging induced aspiration Examination of the throat may trigger laryngospasm and cause respiratory collapse. Death may occur in a few hours. This selection is the only option that accurately identifies the life-threatening complication that can result from an examination of the throat of a child who demonstrates the signs and symptoms of acute epiglottitis. PTS: 1 REF: Page 1297 19. Which statement best describes cystic fibrosis? a. Obstructive airway disease characterized by reversible airflow obstruction, bronchial hyperreactivity, and inflammation b. Respiratory disease characterized by severe hypoxemia, decreased pulmonary compliance, and diffuse densities on chest x-ray imaging c. Pulmonary disorder involving an abnormal expression of a protein-producing viscous mucus that obstructs the airways, pancreas, sweat ducts, and vas deferens d. Pulmonary disorder characterized by atelectasis and increased pulmonary resistance as a result of a surfactant deficiency Cystic fibrosis is best described as a pulmonary disorder involving an abnormal expression of a protein-producing viscous mucus that obstructs the airways, pancreas, sweat ducts, and vas deferens. This selection is the only option that accurately describes cystic fibrosis. PTS: 1 REF: Pages 1310-1311 20. Cystic fibrosis is caused by which process? a. Autosomal recessive inheritance c. Infection b. Autosomal dominant inheritance d. Malignancy Cystic fibrosis is an autosomal recessive inherited disorder that is associated with defective epithelial ion transport. None of the other options cause cystic fibrosis. PTS: 1 REF: Page 13N1U0RSINGTB.COM 21. What are the abnormalities in cytokines found in children with cystic fibrosis (CF)? a. Deficit of interleukin (IL)–1 and an excess of IL-4, IL-12, and interferon-alpha (IFN- b. Deficit of IL-6 and an excess of IL-2, IL-8, and granulocyte colony-stimulating factor (G-CSF) c. Deficit of IL-10 and an excess of IL-1, IL-8, and TNF- d. Deficit of IL-3 and an excess of IL-14, IL-24, and colony-stimulating factor (CSF) Abnormal cytokine profiles have been documented in CF airway fluids, including deficient IL-10 and excessive IL-1, IL-8, and TNF-, all changes conducive to promoting inflammation. This selection is the only option that accurately identifies the abnormalities in cytokines observed in children with CF. PTS: 1 REF: Pages 1311-1312 22. Between which months of age does sudden infant death syndrome (SIDS) most often occur? a. 0 and 1 c. 5 and 6 b. 2 and 4 d. 6 and 7 The incidence of SIDS is low during the first month of life but sharply increases in the second month of life, peaking at 2 to 4 months and is unusual after 6 months of age. PTS: 1 REF: Page 1313 23. Where in the respiratory tract do the majority of foreign objects aspirated by children finally lodge? a. Trachea c. Bronchus b. Left lung d. Bronchioles Approximately 75% of aspirated foreign bodies lodge in a bronchus. The other options are not locations where children aspirate the majority of foreign objects. PTS: 1 REF: Page 1298 24. What is the most common predisposing factor to obstructive sleep apnea in children? a. Chronic respiratory infections c. Obligatory mouth breathing b. Adenotonsillar hypertrophy d. Paradoxic breathing In otherwise healthy children, the most common predisposing factor is adenotonsillar hypertrophy, which causes physical impingement on the nasopharyngeal airway. The other options are not associated with obstructive sleep apnea in children. PTS: 1 REF: Page 1300 MULTIPLE RESPONSE NURSINGTB.COM 25. Which statement is true regarding alveoli? (Select all that apply.) a. The number of functioning alveoli is determined by birth. b. The alveoli begin to increase in size starting at 8 years of age. c. The complexity of the alveoli increases into adulthood. d. These structures produce surfactant. e. Capillaries are the origin of alveoli. , C, E Capillaries grow into the distal respiratory units that keep subdividing (alveolarization) to maximize the surface area for gas exchange. The number of alveoli continues to increase during the first 5 to 8 years of life, after which the alveoli increase in size and complexity. Surfactant is a lipid-protein mix that is produced by type II alveolar cells. PTS: 1 REF: Page 1291 26. Children diagnosed with chronic asthma are likely to exhibit which symptoms? (Select all that apply.) a. Nasal flaring b. Musical expiratory wheezing c. Clubbing of fingers and toes d. Substernal retractions e. Diaphoresis , B, D, E On physical examination, expiratory wheezing that is often described as high pitched and musical is exhibited, along with prolongation of the expiratory phase of the respiratory cycle. Hyperinflation is sometimes visible. The respiratory rate is elevated, as is the heart rate. Nasal flaring and accessory muscle use are evident, with retractions in the substernal, subcostal, intercostal, suprasternal, or sternocleidomastoid areas. Infants may appear to be “head bobbing” because of sternocleidomastoid muscle use. Pulsus paradoxus may also be present. The child may appear anxious or diaphoretic, which are important signs of respiratory compromise. Clubbing of fingers and toes is not typically associated with asthma. PTS: 1 REF: Page 1309 27. Which symptom is not a clinical manifestation of croup? a. Rhinorrhea b. Sore throat c. Low-grade fever d. Barking cough e. Coarse rhonchi ANS: E Typically, a prodrome of rhinorrhea, sore throat, and low-grade fever is exhibited for a few days with croup. The child then develops the characteristic harsh (seal-like) barking cough, hoarse voice, and inspiratory stridor. Rhonchi are associated with lower respiratory diseases. PTS: 1 REF: Page 1295 NURSINGTB.COM 28. What are the clinical manifestations of bacterial pneumonia in children? (Select all that apply.) a. Fever with chills b. Productive cough c. Dyspnea d. Respiratory alkalosis e. Malaise , B, C, E The clinical presentation of bacterial pneumonia, particularly pneumococcal, may include a preceding viral illness, followed by fever with chills and rigors, shortness of breath, and an increasingly productive cough. Auscultation usually reveals such abnormalities as crackles or decreased breath sounds. Other less specific findings may include malaise, emesis, abdominal pain, and chest pain. Respiratory alkalosis is not usually associated with bacterial pneumonia in children. PTS: 1 REF: Page 1306 MATCHING Match the sound of stridor with the location of the problem. A. Sonorous snoring B. Muffled voice C. High-pitched inspiratory sound, voice change, hoarse D. Expiratory stridor or monophonic wheeze E. Inspiratory wheezes 29. Tracheal problems 30. Laryngeal problems 31. Upper trachea obstruction 32. Nasopharyngeal obstruction, such as adenotonsillar hypertrophy. 33. Supralaryngeal obstructions 29. ANS: D PTS: 1 REF: Page 1293 MSC: Expiratory stridors or monophonic wheezes suggest tracheal problems. 30. ANS: C PTS: 1 REF: Page 1294 MSC: Abnormalities of voice or cry (weak or hoarse) suggest problems at the larynx. 31. ANS: E PTS: 1 REF: Page 1298 MSC: Foreign bodies lodged in the upper trachea typically produce inspiratory stridor. 32. ANS: A PTS: 1 REF: Page 1293 MSC: Sonorous snoring is associated with nasopharyngeal obstruction, such as adenotonsillar hypertrophy. 33. ANS: B PTS: 1 REF: Page 1294 MSC: Muffling of the voice, especially in an acute condition, suggests supralaryngeal obstruction, such as epiglottitis or retropharyngeal abscess. NURSINGTB.COM Chapter 38: Structure and Function of the Renal and Urologic Systems MULTIPLE CHOICE 1. The area of the kidneys that contains the glomeruli and portions of the tubules is called the: a. Medulla c. Pyramids b. Cortex d. Columns The cortex contains all the glomeruli and portions of the tubules of the kidneys. Although the other options are also located in the kidney, they do not contain the glomeruli. PTS: 1 REF: Page 1320 2. What is the functional unit of the kidney called? a. Glomerulus c. Collecting duct b. Nephron d. Pyramid The nephron is the functional unit of the kidney. Although the other options are also located in the kidney, they are not its functional units. PTS: 1 REF: Page 1320 3. Which cells have phagocytic properties similar to monocytes and contract like smooth muscles cells, thereby influencingNtUheRSgIlNoGmTeBru.ClaOrMfiltration rate? a. Principle cells c. Mesangial cells b. Podocin cells d. Intercalated cells Mesangial cells and the mesangial matrix, secreted by mesangial cells, lie between and support the glomerular capillaries. Different mesangial cells contract like smooth muscle cells to regulate glomerular capillary blood flow. They also have phagocytic properties similar to monocytes. The other options are not capable of these functions. PTS: 1 REF: Page 1321 4. The only surface inside the nephron where cells are covered with microvilli to increase the reabsorptive surface area is called the: a. Proximal convoluted tubules c. Ascending loop of Henle b. Distal tubules d. Descending loop of Henle The only surface inside the nephron where the cells are covered with microvilli (a brush border) is called the proximal convoluted tubules. This proximal convoluted tubular lumen consists of one layer of cuboidal cells with a surface layer of microvilli that increases the reabsorptive surface area. PTS: 1 REF: Page 1322 5. What part of the kidney controls renal blood flow, glomerular filtration, and renin secretion? a. Macula densa c. Juxtaglomerular apparatus (JGA) b. Visceral epithelium d. Filtration slits Control of renal blood flow, glomerular filtration, and renin secretion occur at the JGA. Together, the juxtaglomerular cells and macula densa cells form the JGA. The control of renal blood flow, glomerular filtration, and renin secretion is not directed by any of the other options. PTS: 1 REF: Page 1322 6. Kidney stones in the upper part of the ureter would produce pain referred to which anatomical area? a. Vulva or penis c. Thighs b. Umbilicus d. Lower abdomen Kidney stones in the upper part of the ureter would produce pain in the umbilicus. Sensory innervation for the upper part of the ureter arises from the tenth thoracic nerve roots with referred pain to the umbilicus. The other options would not experience such referred pain. PTS: 1 REF: Page 1325 7. Innervation of the bladder and internal urethral sphincter is supplied by which nerves? a. Peripheral nerves c. Sympathetic nervous system b. Parasympathetic fibers NURSINGTdB..COTMenth thoracic nerve roots The innervation of the bladder and internal urethral sphincter is supplied by parasympathetic fibers of the autonomic nervous system. The process is not dependent on any of the other options. PTS: 1 REF: Page 1326 8. How much urine accumulates in the bladder before the mechanoreceptors sense bladder fullness? a. 75 to 100 ml c. 250 to 300 ml b. 100 to 150 ml d. 350 to 400 ml When the bladder accumulates 250 to 300 ml of urine, it contracts and the internal urethral sphincter relaxes through activation of the spinal reflex arc (known as the micturition reflex). PTS: 1 REF: Page 1326 9. What is the trigone? a. A smooth muscle that comprises the orifice of the ureter b. The inner mucosal lining of the kidneys c. A smooth triangular area between the openings of the two ureters and the urethra d. One of the three divisions of the loop of Henle The trigone is a smooth triangular area lying between the openings of the two ureters and the urethra. The other options do not accurately identify the trigone. PTS: 1 REF: Page 1325 10. The glomerular filtration rate is directly related to which factor? a. Perfusion pressure in the glomerular capillaries b. Diffusion rate in the renal cortex c. Diffusion rate in the renal medulla d. Glomerular active transport The filtration of the plasma per unit of time is known as the glomerular filtration rate (GFR), which is directly related to only the perfusion pressure in the glomerular capillaries. PTS: 1 REF: Page 1326 11. On average, what percent of cardiac output do the kidneys receive? a. 10% to 20% c. 20% to 25% b. 15% to 20% d. 30% to 35% The kidneys are highly vascular organs and usually receive 1000 to 1200 ml of blood per minute, or approximately 20% to 25% of the cardiac output. NURSINGTB.COM PTS: 1 REF: Page 1326 12. What effects do exercise and body position have on renal blood flow? a. Exercise and body position activate renal parasympathetic neurons and cause mild vasoconstriction. b. They activate renal sympathetic neurons and cause mild vasoconstriction. c. Both activate renal parasympathetic neurons and cause mild vasodilation. d. They activate renal sympathetic neurons and cause mild vasodilation. Exercise and change of body position activate renal sympathetic neurons and cause mild vasoconstriction. The other options do not have these effects on renal blood flow. PTS: 1 REF: Page 1327 13. Blood vessels of the kidneys are innervated by the: a. Vagus nerve c. Somatic nervous system b. Sympathetic nervous system d. Parasympathetic nervous system The blood vessels of the kidney are innervated by the sympathetic noradrenergic fibers that cause arteriolar vasoconstriction and reduce renal blood flow. The other options are not involved in this process. 14. When renin is released, it is capable of which action? a. Inactivation of autoregulation b. Direct activation of angiotensin II c. Direct release of antidiuretic hormone (ADH) d. Formation of angiotensin I When renin is released, it cleaves an -globulin (angiotensinogen produced by liver hepatocytes) in the plasma to form angiotensin I. PTS: 1 REF: Page 1327 15. What effect do natriuretic peptides have during heart failure when the heart dilates? a. Stimulates antidiuretic hormones. c. Stimulates renin and aldosterone. b. Inhibits antidiuretic hormones. d. Inhibits renin and aldosterone. Natriuretic peptides inhibit renin and aldosterone during heart failure when the heart dilates. These make up a group of peptide hormones, including atrial natriuretic peptide (ANP), secreted from myocardial cells in the atria and brain natriuretic peptide (BNP) secreted from myocardial cells in the cardiac ventricles. When the heart dilates during volume expansion or heart failure, ANP and BNP inhibit sodium and water absorption by kidney tubules, inhibit the secretion of renin and aldosterone, vasodilate the afferent arterioles, and constrict the efferent arterioles. The result is increased urine formation, leading to decreased blood volume and blood pressure. NURSINGTB.COM PTS: 1 REF: Page 1327 16. What is the direct action of atrial natriuretic hormone? a. Sodium retention c. Water retention b. Sodium excretion d. Water excretion Atrial natriuretic peptide (ANP) and brain natriuretic peptide (BNP) inhibit the secretion of renin, inhibit angiotensin-induced secretion of aldosterone, vasodilate the afferent and constrict the efferent glomerular arterioles, and inhibit sodium and water absorption by kidney tubules. The other actions are not a result of the atrial natriuretic hormone. PTS: 1 REF: Page 1327 17. What term is used to identify the movement of fluids and solutes from the tubular lumen to the peritubular capillary plasma? a. Tubular secretion c. Tubular reabsorption b. Ultrafiltration d. Tubular excretion ANS: C Tubular reabsorption is the movement of fluids and solutes from the tubular lumen to the peritubular capillary plasma. This selection is the only option that correctly identifies the process. PTS: 1 REF: Page 1328 18. How high does the plasma glucose have to be before the threshold for glucose is achieved? a. 126 mg/dl c. 180 mg/dl b. 150 mg/dl d. 200 mg/dl When the plasma glucose reaches 180 mg/dl, as occurs in the individual with uncontrolled diabetes mellitus, the threshold for glucose is achieved. PTS: 1 REF: Page 1330 19. Which hormone is required for water to be reabsorbed in the distal tubule and collecting duct? a. Antidiuretic hormone c. Cortisol b. Aldosterone d. Adrenocorticotropin hormone Antidiuretic hormone is required for water to be reabsorbed in the distal tubule and collecting duct. The later, straight segment of the distal tubule and the collecting duct are permeable to water as controlled by antidiuretic hormone. The other options are not involved in this process. PTS: 1 REF: Page 1331 20. Which glycoprotein protects against urolithiasis and is a ligand for lymphokines? a. Uromodulin c. Urodilatin b. Nephrin NURSINGTdB..COCMystatin Tamm-Horsfall glycoprotein, also known as uromodulin, is the most abundant urinary protein, protects against bacterial adhesion and urolithiasis, and is a ligand for lymphokines. This statement is not true of the other options. PTS: 1 REF: Page 1331 21. What is the end-product of protein metabolism that is excreted in urine? a. Glucose c. Bile b. Ketones d. Urea Of the options available, only urea is an end-product of protein metabolism and is the major constituent of urine along with water. PTS: 1 REF: Page 1332 22. What is the action of urodilatin? a. Urodilatin causes vasoconstriction of afferent arterioles. b. It causes vasodilation of the efferent arterioles. c. Urodilatin inhibits antidiuretic hormone secretion. d. It inhibits salt and water reabsorption. Urodilatin (a natriuretic peptide) inhibits sodium and water reabsorption from the medullary part of collecting duct, thereby producing diuresis. It is not involved in the actions described by the other options. PTS: 1 REF: Pages 1327-1328 | Table 37-1 23. The concentration of the final urine is determined by antidiuretic hormone (ADH), which is secreted by which gland? a. Posterior pituitary c. Parathyroid b. Thyroid d. Anterior pituitary ADH, which is secreted from the posterior pituitary gland, controls the concentration of the final urine. ADH is not secreted by any of the other options. PTS: 1 REF: Pages 1332-1333 24. Which statement is true regarding urodilatin? a. Urodilatin inhibits sodium chloride and water reabsorption in the medullary part of the collecting duct. b. It inhibits antidiuretic hormone (ADH) to prevent water reabsorption in the medullary part of the collecting duct. c. Urodilatin is stimulated by a rise in blood pressure and an increase in extracellular volume. d. It is stimulated by a fall in blood pressure and a decrease in extracellular volume. ANS: C When the circulating volume and NinUcRreSaINseGdTbBl.oCoOdMpressure are increased, the distal tubule and collecting duct produces urodilatin (a natriuretic peptide). Urodilatin inhibits sodium and water reabsorption from the medullary part of collecting duct, thereby producing diuresis. PTS: 1 REF: Page 1328 | Table 37-1 25. What substance stimulates renal hydroxylation in the process of producing vitamin D? a. Erythropoietin c. Calcitonin b. Thyroid hormone d. Parathyroid hormone Parathyroid hormone stimulates renal hydroxylation in the process of producing vitamin D. The first step occurs in the liver with hydroxylation at the 25th carbon (calcifediol); the second step in hydroxylation occurs at the first carbon position in the kidneys. The other options are not involved in this process. PTS: 1 REF: Page 1334 26. Which hormone is synthesized and secreted by the kidneys? a. Antidiuretic hormone c. Erythropoietin b. Aldosterone d. Angiotensinogen Erythropoietin is produced by the fetal liver and in the adult kidney and is essential for normal erythropoiesis. This statement is not true of the other options. PTS: 1 REF: Page 1334 27. What provides the best estimate of the functioning of renal tissue? a. Glomerular filtration rate b. Hourly urine output c. Serum blood urea nitrogen and creatinine d. The specific gravity of the solute concentration of the urine The glomerular filtration rate provides the best estimate of the level of functioning of renal tissue. The other options are not used to assess renal tissue function. PTS: 1 REF: Page 1334 28. Which renal change is found in older adults? a. Sharp decline in glomerular filtration rate b. Sharp decline in renal blood flow c. Decrease in the number of nephrons d. Decrease in urine output With aging, the number of nephrons decreases. The other options are not necessarily related to aging. PTS: 1 REF: Page 13N3U6RSINGTB.COM 29. Compared with a younger individual, how is the specific gravity of urine in older adults affected? a. Specific gravity of urine in older adults is increased. b. Specific gravity of urine in older adults is considered high normal. c. Specific gravity of urine in older adults is considered low normal. d. Specific gravity of urine in older adults is decreased. The specific gravity of the urine in older individuals tends to be on the low side of normal. PTS: 1 REF: Page 1336 30. What process allows the kidney to respond to an increase in workload? a. Glomerular filtration b. Secretion of 1,25-dihydroxyvitamin D3 c. Increased heart rate d. Compensatory hypertrophy Compensatory hypertrophy allows the kidney to respond to an increase in workload throughout life. The remaining options are not relevant to accommodating an increased workload. PTS: 1 REF: Page 1336 31. Which process makes it possible for ureters to be transplanted successfully? a. Compensatory hypertrophy c. Peristalsis b. Erythropoietin secretion d. Collateral circulation Peristalsis is the process which makes it possible for ureters to be transplanted successfully. This process is maintained even when the ureter is denervated. The remaining options are not relevant to transplant success. PTS: 1 REF: Page 1325 MULTIPLE RESPONSE 32. Which structures are parts of the nephron? (Select all that apply.) a. Loop of Henle b. Renal corpuscle c. Proximal convoluted tubule d. Calyx e. Collecting duct , B, C, E The nephron is a tubular structure with subunits that include the renal corpuscle, proximal convoluted tubule, loop of Henle, distal convoluted tubule, and collecting duct, all of which contribute to the formation of final urine. The calyx is not a structure contained in the nephrons. NURSINGTB.COM PTS: 1 REF: Page 1320 33. Which forces create passive transport of water in the proximal tubule? (Select all that apply.) a. Peritubular capillary hydrostatic pressure b. Peritubular capillary oncotic pressure c. Interstitial hydrostatic pressure d. Interstitial osmotic pressure e. Peritubular capillary osmotic pressure , E The osmotic force generated by active sodium transport promotes the passive diffusion of water out of the tubular lumen and into the peritubular capillaries. The elevated oncotic pressure of the blood in the peritubular capillaries further enhances the passive transport of water. The remaining options are not forces that create passive transport of water in the proximal tubule. PTS: 1 REF: Page 1330 34. Which hormones are produced by the kidney? (Select all that apply.) a. Renin b. Erythropoietin c. 1,25-dihydroxyvitamin D3 d. Calcitonin e. Aldosterone , B, C The kidney also has an endocrine function, secreting the hormones renin, erythropoietin, and 1,25-dihydroxyvitamin D3 for the regulation of blood pressure, erythrocyte production, and calcium metabolism, respectively. Neither calcitonin nor aldosterone is produced by the kidney. PTS: 1 REF: Page 1319 35. Which statements are true regarding renal circulation? (Select all that apply.) a. The interlobar arteries travel down into the renal columns. b. The arcuate arteries branch to form the interlobar arteries. c. The arcuate arteries arch over the base of the pyramids. d. The interlobar arteries run parallel to the surface of the kidneys. e. The interlobar arteries run between the pyramids. ANS: A, C, E The interlobar arteries are further subdivisions that travel down the renal columns and between the pyramids. At the cortical medullary junction, interlobar arteries branch into the arcuate arteries that arch over the base of the pyramids and run parallel to the surface of the kidney. PTS: 1 REF: Page 1325 MATCHING NURSINGTB.COM Match the descriptions with the corresponding terms. A. Good estimate of glomerular filtration rate B. Form in concentrated acidic or alkaline urine C. Cylindric with distinct borders D. Hematuria E. Pyuria 36. Crystals 37. Casts 38. Leukocytes 39. Creatinine clearance 40. Erythrocytes 36. ANS: MSC: B PTS: 1 REF: Page 1336 Crystals tend to form in a concentrated acidic or alkaline urine. 37. ANS: MSC: C PTS: 1 REF: Page 1336 Casts are cylindrical with distinct borders. 38. ANS: MSC: E PTS: 1 REF: Page 1336 White blood cells in the urine (a condition termed pyuria) are indicative of urinary tract infection, particularly when bacteria are present. 39. ANS: A PTS: 1 REF: Page 1334 MSC: Creatinine clearance provides a good measure of glomerular filtration rate because only one blood sample is required in addition to a 24-hour volume of urine. 40. ANS: D PTS: 1 REF: Pages 1335-1336 MSC: Normal urine contains few or no red blood cells. If a large number of red blood cells are present, then a condition known as hematuria results, and the sediment may be red. NURSINGTB.COM Chapter 39: Alterations of Renal and Urinary Tract Function MULTIPLE CHOICE 1. How does progressive nephrons injury affect angiotensin II activity? a. Angiotensin II activity is decreased. b. It is elevated. c. Angiotensin II activity is totally suppressed. d. It is not affected. ANS: B Angiotensin II activity is elevated with progressive nephron injury. This selection is the only accurate identification of the effect of progressive nephron injury on angiotensin II activity. PTS: 1 REF: Page 1364 | Page 1366 2. Which mineral accounts for the most common type of renal stone? a. Magnesium-ammonium-phosphate c. Calcium oxalate b. Uric acid d. Magnesium phosphate Calcium stones (calcium phosphate or calcium oxalate) account for 70% to 80% of all stones requiring treatment. PTS: 1 REF: Page 1343 NURSINGTB.COM 3. Regarding the formation of renal calculi, what function does pyrophosphate, potassium citrate, and magnesium perform? a. They inhibit crystal growth. b. Pyrophosphate, potassium citrate, and magnesium stimulate the supersaturation of salt. c. They facilitate the precipitation of salts from a liquid to a solid state. d. Pyrophosphate, potassium citrate, and magnesium enhance crystallization of salt crystals to form stones. Stone or crystal growth inhibiting substances, including potassium citrate, pyrophosphate, and magnesium, are capable of crystal growth inhibition. They are not capable of the functions stated by the other options. PTS: 1 REF: Page 1343 4. Hypercalciuria is primarily attributable to which alteration? a. Defective renal calcium reabsorption b. Intestinal hyperabsorption of dietary calcium c. Bone demineralization caused by prolonged immobilization d. Hyperparathyroidism Hypercalciuria is usually attributable to intestinal hyperabsorption of dietary calcium and less commonly to a defect in renal calcium reabsorption. Hyperparathyroidism and bone demineralization associated with prolonged immobilization are also known to cause hypercalciuria but too a much lesser degree. PTS: 1 REF: Page 1343 5. Detrusor hyperreflexia develops from neurologic disorders that originate where? a. Spinal cord between C2 and S1 c. Above the pontine micturition center b. Spinal cord between S2 and S4 d. Below the cauda equina Neurologic disorders that develop above the pontine micturition center result in detrusor hyperreflexia, also known as an uninhibited or reflex bladder. This selection is the only option responsible for detrusor hyperreflexia. PTS: 1 REF: Page 1345 6. Considering the innervation of the circular muscles of the bladder neck, which classification of drug is used to treat bladder neck obstruction? a. -Adrenergic blocking medications c. Parasympathomimetic medications b. -Adrenergic blocking medications d. Anticholinesterase medications Because the bladder neck consists of circular smooth muscle with adrenergic innervation, detrusor sphincter dyssynergia may be managed by -adrenergic blocking (antimuscarinic) medications. This selection is the only option capable of this specific function. NURSINGTB.COM PTS: 1 REF: Page 1346 7. Renal cell carcinoma, classified as clear cell tumors, arises from epithelial cells in which structure? a. Proximal tubule c. Nephron b. Distal tubule d. Glomerulus Renal cell carcinoma, classified as clear cell tumors according to cell type and extent of metastasis, arises from the proximal tubular epithelium. These tumors are not associated with the other options. PTS: 1 REF: Page 1347 8. Bladder cancer is associated with the gene mutation of which gene? a. c-erbB2 b. Human epidermal growth factor receptor 2 (HER2) c. TP53 d. myc Oncogenes of the ras gene family and tumor-suppressor genes including TP53 mutations and the inactivation of the retinoblastoma gene (pRb) are implicated in bladder cancer. This process is not associated with the other options. PTS: 1 REF: Page 1348 9. What is the most common cause of uncomplicated urinary tract infections? a. Staphylococcus c. Proteus b. Klebsiella d. Escherichia coli The most common infecting microorganisms are uropathic strains of E. coli (80% to 85%). PTS: 1 REF: Page 1350 10. Which differentiating sign is required to make the diagnosis of pyelonephritis from that of cystitis? a. Difficulty starting the stream of urine b. Spasmodic pain that radiates to the groin c. Increased glomerular filtration rate d. Urinalysis confirmation of white blood cell casts Clinical assessment, alone, is difficult to differentiate the symptoms of cystitis from those of pyelonephritis. Urine culture, urinalysis, and clinical signs and symptoms establish the specific diagnosis. White blood cell casts indicate pyelonephritis, but they are not always present in the urine. This selection is the only option that is considered a required sign of pyelonephritis. PTS: 1 REF: Pages 1351-1352 NURSINGTB.COM 11. Considering host defense mechanisms, which element in the urine is bacteriostatic? a. High pH (alkaline urine) c. High glucose b. High urea d. High calcium Dilute urine washes out bacteria, and urine with higher urea concentrations (high osmolarity) is more bacteriostatic. PTS: 1 REF: Page 1350 12. Which clinical manifestations of a urinary tract infection may be demonstrated in an 85-year-old individual? a. Confusion and poorly localized abdominal discomfort b. Dysuria, frequency, and suprapubic pain c. Hematuria and flank pain d. Pyuria, urgency, and frequency Older adults with cystitis may demonstrate confusion or vague abdominal discomfort or otherwise be asymptomatic. PTS: 1 REF: Page 1351 13. Pyelonephritis is usually caused by which type of organism? a. Bacteria c. Viruses b. Fungi d. Parasites Pyelonephritis is usually caused by the bacteria Escherichia coli, Proteus, or Pseudomonas. PTS: 1 REF: Pages 1351-1352 14. Which abnormal laboratory value is found in glomerular disorders? a. Elevated creatinine concentration c. Elevated immunoglobulin A (IgA) b. Low blood urea nitrogen (BUN) d. Low serum complement Elevated creatinine concentration is an abnormal laboratory value found in glomerular disorders. Reduced glomerular filtration rate during glomerular disease is evidenced by elevated plasma urea, creatinine concentration, or reduced renal creatinine clearance. Glomerular disorders are not associated with the other options. PTS: 1 REF: Page 1357 15. Which glomerular lesion is characterized by thickening of the glomerular capillary wall with immune deposition of immunoglobulin G (IgG) and C3? a. Proliferative c. Mesangial b. Membranous d. Crescentic The thickening of the glomerular capillary wall characterizes only membranous lesions. NURSINGTB.COM PTS: 1 REF: Page 1355 | Table 38-6 16. Goodpasture syndrome is an example of which of the following? a. Antiglomerular basement membrane disease b. Acute glomerulonephritis c. Chronic glomerulonephritis d. Immunoglobulin A (IgA) nephropathy ANS: A Antiglomerular basement membrane disease (Goodpasture syndrome) is associated with immunoglobulin G (IgG) antibody formation against pulmonary capillary and glomerular basement membranes. Goodpasture syndrome is not an example of any of the other options. PTS: 1 REF: Page 1355 | Table 38-5 17. A patient exhibits symptoms including hematuria with red blood cell casts and proteinuria exceeding 3 to 5 g/day, with albumin as the major protein. These data suggest the presence of which disorder? a. Cystitis c. Glomerulonephritis b. Chronic pyelonephritis d. Nephrotic syndrome The data suggest the patient has the disorder known as glomerulonephritis. Two major changes distinctive of more severe glomerulonephritis are (1) hematuria with red blood cell casts and (2) proteinuria exceeding 3 to 5 g/day with albumin as the major protein. These symptoms do not support the diagnosis of the other options. PTS: 1 REF: Page 1357 18. Hypothyroidism, edema, hyperlipidemia, and lipiduria characterize which kidney disorder? a. Nephrotic syndrome c. Chronic glomerulonephritis b. Acute glomerulonephritis d. Pyelonephritis Symptoms of nephrotic syndrome include edema, hyperlipidemia, lipiduria, vitamin D deficiency, and hypothyroidism. These symptoms do not support the other options. PTS: 1 REF: Page 1359 19. Which antibiotics are considered “major culprits” in causing nephrotoxic acute tubular necrosis (ATN)? a. Penicillin and ampicillin c. Gentamicin and tobramycin b. Vancomycin and bacitracin d. Cefazolin and cefepime Although numerous antibiotics can produce nephrotoxic ATN, the aminoglycosides (gentamicin, tobramycin) are the major culprits. PTS: 1 REF: Page 13N6U1RSINGTB.COM 20. Which urine characteristics are indicative of acute tubular necrosis (ATN) caused by intrinsic (intrarenal) failure? a. Urine sodium >30 mEq/L b. Urine osmolality >500 mOsm c. Fractional excretion of sodium (FENa) <1% d. Urine sediment has no cells, some hyaline casts Urine sodium >30 mEq/L is the only option indicative of ATN. PTS: 1 REF: Page 1363 | Table 38-11 21. How are glucose and insulin used to treat hyperkalemia associated with acute renal failure? a. Glucose has an osmotic effect, which attracts water and sodium, resulting in more dilute blood and a lower potassium concentration. b. When insulin transports glucose into the cell, it also carries potassium with it. c. Potassium attaches to receptors on the cell membrane of glucose and is carried into the cell. d. Increasing insulin causes ketoacidosis, which causes potassium to move into the cell in exchange for hydrogen. This selection is the only option that accurately describes glucose metabolism, causing potassium to move to the intracellular fluid; insulin infusions therefore can be effective in shifting potassium from the extracellular to intracellular space, along with the transport of glucose. PTS: 1 REF: Page 1363 22. Creatinine is primarily excreted by glomerular filtration after being constantly released from what type of tissue? a. Nervous system c. Muscle b. Kidneys d. Liver Creatinine is constantly released from only muscle tissue to be excreted by glomerular filtration. PTS: 1 REF: Page 1366 23. Which statement is false concerning the skeletal alterations caused by chronic renal failure when the glomerular filtration rate (GFR) declines to 25% of normal? a. Parathyroid hormone is no longer effective in maintaining serum phosphate levels. b. The parathyroid gland is no longer able to secrete sufficient parathyroid hormone. c. The synthesis of 1,25-vitamin D3, which reduces intestinal absorption of calcium, is impaired. d. The synthesis of 1,25-vitamin D3, which impairs the effectiveness of calcium and phosphate resorption from bone by parathyroid hormone, is impaired. NURSINGTB.COM Bone and skeletal changes develop with alterations in calcium and phosphate metabolism (see Table 38-16). These changes begin when the GFR decreases to 25% or less. The combined effect of hyperparathyroidism and vitamin D deficiency can result in renal osteodystrophies (e.g., osteomalacia, osteitis fibrosa with increased risk for fractures). Other consequences of secondary hyperparathyroidism include soft-tissue and vascular calcification, cardiovascular disease, and, less commonly, calcific uremic arteriolopathy. The other options are true. PTS: 1 REF: Page 1368 | Table 38-16 24. Anemia of chronic renal failure can be successfully treated with which element? a. Intrinsic factor c. Vitamin D b. Vitamin B12 d. Erythropoietin Anemia of chronic renal failure can be successfully treated with erythropoietin. Reduced erythropoietin secretion and reduced red cell production are evident in anemia resulting from chronic renal failure. The other options are not relevant to this condition. PTS: 1 REF: Page 1365 | Page 1369 | Table 38-13 25. When the right kidney is obstructed, how will the glomeruli and tubules in the left kidney compensate? a. Increase in number c. Develop collateral circulation b. Increase in size d. Increase speed of production These processes cause the contralateral (unobstructed) kidney to increase the size of individual glomeruli and tubules. The changes described by the other options are not correct. PTS: 1 REF: Page 1342 26. What medical term is used to identify a functional urinary tract obstruction caused by an interruption of the nerve supply to the bladder? a. Neurogenic bladder c. Necrotic bladder b. Obstructed bladder d. Retrograde bladder Neurogenic bladder is a general term for bladder dysfunction caused by neurologic disorders. The types of dysfunction are related to the sites in the nervous system that control sensory and motor bladder function (see Figure 38-3). None of the other options correctly identify the described condition. PTS: 1 REF: Pages 1344-1345 MULTIPLE RESPONSE 27. In glomerulonephritis, what damages the epithelial cells resulting in proteinuria? (Select all that apply.) a. Ischemia b. Lysosomal enzymes c. Compression from edema d. Activated complement NURSINGTB.COM e. Altered membrane permeability , E Activated complement, inflammatory cytokines, oxidants, proteases, and growth factors attack epithelial cells, alter membrane permeability, and cause proteinuria. None of the other options are responsible for this process. PTS: 1 REF: Pages 1353-1357 28. Which statements are true concerning struvite stones? (Select all that apply.) a. They are more common in women than in men. b. Struvite stones are associated with chronic laxative use in women. c. They grow large and branch into a staghorn configuration in renal pelvis and calyces. d. Struvite stones are closely associated with urinary tract infections caused by urease-producing bacteria, such as Pseudomonas. e. They are more common in men than in women. , C, D Women are at greater risk for developing struvite stones, but the risk is greater because women have an increased incidence of urinary tract infections not because of chronic laxative use. Such stones grow large and branch into a staghorn configuration and are associated with Pseudomonas. PTS: 1 REF: Pages 1343-1344 29. Which statements are true regarding renal colic? (Select all that apply.) a. Renal colic results in mild-to-moderate pain. b. Pain originates in the flank area. c. Renal colic indicates the presence of renal stones. d. Pain radiated to the groin. e. Renal colic indicates obstruction of the renal pelvis or proximal ureter. ANS: B, C, D, E Renal colic is described as moderate-to-severe pain often originating in the flank and radiating to the groin. It usually indicates obstruction by renal stones of the renal pelvis or proximal ureter. PTS: 1 REF: Page 1344 30. Which conditions related to the bladder would result from the effects of lesions of the sacral segments below S1? (Select all that apply.) a. Frequency b. Urge incontinence c. Bladder distension d. Urgency e. Urinary retention , E NURSINGTB.COM Lesions that involve the sacral micturition center (below S1; may also be termed cauda equina syndrome) or peripheral nerve lesions result in detrusor areflexia (acontractile detrusor), a lower motor neuron disorder. The result is an acontractile detrusor or atonic bladder with retention of urine and distention. The other options are associated with neurologic lesions that occur between C2 and S1 PTS: 1 REF: Page 1345 31. What are considered risk factors for developing bladder and kidney cancers? (Select all that apply.) a. Cigarette smoking b. Hypertension c. Exposure to aniline dyes d. Below normal body weight e. Male gender , B, C Risk factors for renal cancer include cigarette smoking, obesity, and hypertension. The risk of primary bladder cancer is greater among people who smoke or those who are exposed to metabolites of aniline dyes or other aromatic amines or chemicals and with heavy consumption of phenacetin. Gender is not a recognized risk factor. PTS: 1 REF: Pages 1347-1349 32. Which renal disorders are considered causes of intrarenal renal failure? (Select all that apply.) a. Acute glomerulonephritis b. Allograft rejection c. Tumors d. Acute tubular necrosis (ATN) e. Prostatic hypertrophy , B, C, D Intrarenal (intrinsic) acute kidney injury (AKI) may result from ischemic ATN, nephrotoxic ATN, acute glomerulonephritis, vascular disease, allograft rejection, or interstitial disease (drug allergy, infection, tumor growth). Prostatic hypertrophy is not associated with intrarenal renal failure. PTS: 1 REF: Pages 1360-1361 33. Prerenal injury from poor perfusion can result from which condition? (Select all that apply.) a. Bilateral ureteral obstruction b. Renal vasoconstriction c. Renal artery thrombosis d. Hemorrhage e. Hypotension , C, D, E NURSINGTB.COM Poor perfusion can result from renal artery thrombosis, hypotension related to hypovolemia (dehydration, diarrhea, fluid shifts) or hemorrhage, renal vasoconstriction and alterations in renal regional blood flow, microthrombi, or kidney edema that restricts arterial blood flow. Bilateral ureteral obstruction is not associated with prerenal injuries. PTS: 1 REF: Page 1360 MATCHING Match the predisposing factors causing pyelonephritis to the pathology mechanism. A. Kidney stones B. Vesicoureteral reflux C. Pregnancy D. Neurogenic bladder E. Female sexual trauma 34. Movement of organisms from the urethra into the bladder with infection and retrograde spread to the kidney 35. Dilation and relaxation of the ureter with hydroureter and hydronephrosis 36. Impairment to the bladder, interfering with normal bladder contraction and causing residual urine and ascending infection 37. Obstruction and stasis of urine, contributing to bacteremia and hydronephrosis; irritation of epithelial lining with entrapment of bacteria 38. Chronic reflux of urine up the ureter and into the kidney during micturition, contributing to bacterial infection 34. ANS: E PTS: 1 REF: Page 1352 | Table 38-4 MSC: Female sexual trauma can result from the movement of organisms from the urethra into the bladder with infection and retrograde spread to the kidney. 35. ANS: C PTS: 1 REF: Page 1352 | Table 38-4 MSC: Pregnancy causes the dilation and relaxation of the ureter with hydroureter and hydronephrosis. 36. ANS: D PTS: 1 REF: Page 1352 | Table 38-4 MSC: Neurogenic bladder, caused by neurologic impairment, results in the interference of normal bladder and urethral sphincter contraction and causes residual urine and ascending infection. 37. ANS: A PTS: 1 REF: Page 1352 | Table 38-4 MSC: Kidney stones result in the obstruction and stasis of urine, contributing to bacteriuria and hydronephrosis and causing irritation of epithelial lining with entrapment of bacteria. 38. ANS: B PTS: 1 REF: Page 1352 | Table 38-4 MSC: Vesicoureteral reflux results in the chronic reflux of urine up the ureter and into the kidney during micturition, contributing to bacterial infection. NURSINGTB.COM Chapter 40: Alterations of Renal and Urinary Tract Function in Children MULTIPLE CHOICE 1. The functional kidney is associated with which embryonic organ? a. Metanephros c. Pronephros b. Mesonephros d. Endonephros The functional kidney is associated with the metanephros. The kidney develops from three sets of structures: the pronephros (nonfunctional by the end of the embryonic period), mesonephros (nonfunctional), and metanephros (the functional kidney). Endonephros is not relevant to this process. PTS: 1 REF: Pages 1376-1377 | Figure 39-1 2. When does urine formation and excretion begin? a. At birth c. By 6 months’ gestation b. By 3 months’ gestation d. By 8 months’ gestation Urine formation and excretion begin by the third month of gestation. PTS: 1 REF: Page 1377 3. Compared with an adult, an infant has a greater content of extracellular fluid, as well as a greater rate of fluid exchange. WhNaUt RefSfIeNcGt TdBoe.CsOthMis have on the fluid balance of a child compared with that of an adult? a. Edema development is less of a problem. b. Overhydration is not difficult to manage. c. Daily fluid requirements are greater. d. The control of dehydration is more difficult. An infant not only has a greater content of extracellular fluid, but infants also have a greater rate of fluid exchange. The adult takes in and excretes approximately 2000 ml of water daily, representing 5% of the total body fluid and 14% of the extracellular fluid. In contrast, the infant’s daily exchange of 600 to 700 ml of water represents 290% of the total body fluid or nearly 50% of the extracellular volume, making control of dehydration and overhydration more difficult. This fact makes the other options incorrect. PTS: 1 REF: Page 1378 4. What term is used to identify the condition that exists when the urethral meatus is located on the undersurface of the penis? a. Hypospadias c. Hyperspadias b. Epispadias d. Chordee Hypospadias is a congenital condition in which the urethral meatus is located on the ventral side or undersurface of the penis. This is the only term used for this condition. PTS: 1 REF: Page 1378 5. What initiates inflammation in acute poststreptococcal glomerulonephritis? a. Lysosomal enzymes b. Endotoxins from Streptococcus c. Immune complexes d. Immunoglobulin E (IgE)–mediated response The immune complexes initiate inflammation and glomerular injury in acute poststreptococcal glomerulonephritis. Antigen-antibody complexes are deposited in the glomerulus, or the antigen may be trapped within the glomerulus and immune complexes formed in situ. The other options are not involved in initiating inflammation in this situation. PTS: 1 REF: Page 1381 6. Acute glomerulonephritis (AGN) may be accompanied by a positive throat or skin culture for which bacteria? a. Staphylococcus aureus c. Pseudomonas aeruginosa b. Streptococcus d. Haemophilus AGN may be accompanied by a positive throat or skin culture for Streptococcus. AGN is not associated with any of the other options. PTS: 1 REF: Page 13N8U2RSINGTB.COM 7. What is the cause of smoky, brown-colored urine resulting from acute poststreptococcal glomerulonephritis? a. Presence of red blood cells c. Slough from the collecting tubules b. Presence of urobilinogen d. Protein in the urine The urine is usually smoky brown or cola-colored because of the presence of red blood cells. The other options are not correct statements regarding this condition. PTS: 1 REF: Pages 1381-1382 8. In immunoglobulin G (IgG) nephropathies such as glomerulonephritis, IgG is deposited in which location? a. Juxtamedullary nephrons b. Glomerulus basement membranes c. Mesangium of the glomerular capillaries d. Parietal epithelium Glomerulonephritis develops with the deposition of antigen-antibody complexes (IgG, immunoglobulin A [IgA], and C3 complement) in the glomerulus, or the antigen may be trapped within the glomerulus and immune complexes formed in situ. Immunofluorescence microscopy shows lumpy deposits of IgG and C3 complement on the glomerular basement membrane (see Figure 39-5). When considering IgG nephropathies, the only location of the IgG immunoglobulins is the correct option. PTS: 1 REF: Page 1381 9. What is the pathophysiologic process responsible for the autoimmune disorder of hemolytic-uremic syndrome (HUS)? a. Immunoglobulin A (IgA) coats erythrocytes that are destroyed by the spleen, and remnants are excreted through the kidneys. b. Verotoxin from Escherichia coli is absorbed from the intestines and damages erythrocytes and endothelial cells. c. Endotoxins from E. coli block the erythropoietin produced by the kidneys, which reduces the number of erythrocytes produced by the bone marrow. d. Failure of the nephron to filter urea increases the blood urea nitrogen, which binds to erythrocytes that are subsequently destroyed by the spleen. In HUS, verotoxin from E. coli is absorbed from the intestines, the glomerular arterioles become swollen, and these narrowed vessels damage erythrocytes as they pass through. HUS is responsible for causing a cascade of effects, including lysis of glomerular capillary endothelial cells. The other options are not relevant. PTS: 1 REF: Page 13N8U3RSINGTB.COM 10. What is the first indication of nephrotic syndrome in children? a. Periorbital edema c. Frothy urine b. Scrotal or labial edema d. Ascites Onset of nephritic syndrome is insidious, with periorbital edema as the first sign of the disorder. None of the other options represent the first indication of nephritic syndrome in children. PTS: 1 REF: Page 1384 11. Bacteria gain access to the female urinary tract by which means? a. Systemic blood that is filtered through the kidney b. Bacteria traveling from the lymph adjacent to the bladder and kidneys c. Bacteria ascending the urethra into the bladder d. Colonization of the bladder when urine is static Urinary tract infections (UTIs) in girls occur as a result of perineal bacteria, especially Escherichia coli, ascending the urethra. None of the other options represent the means by which bacteria gain access to the female urinary tract. PTS: 1 REF: Page 1386 12. What causes vesicoureteral reflux to occur in children? a. Children do not ask for help in urinating in a timely manner, and urine is forced up into the ureters. b. The submucosal segment of a child’s ureter is short, making the antireflux mechanism inefficient. c. The trigone lying between the opening to the ureters and the urethra is underdeveloped in children. d. As the bladder fills in infants and children, it pulls the smooth lining of the transitional epithelium away from the ureters, making the reflux valves ineffective. Although reflux is considered abnormal at any age, the shortness of the submucosal segment of the ureter during infancy and childhood renders the antireflux mechanism relatively inefficient and delicate. The other options are not considered reasons for this reflux. PTS: 1 REF: Page 1387 13. What is the mechanism for developing Wilms tumor? a. The development of a Wilms tumor involves tumor-suppressor genes located on chromosome 11. b. Development involves an autosomal dominant inherited disorder involving the Y chromosome. c. Wilms tumor is an autoimmune disorder. d. The development of a Wilms tumor is a congenital anomaly. Wilms tumor–suppressor genes WNTU1RaSnIdNGWTTB.2COarMe located on chromosome 11. The other options are not considered relevant to the development of a Wilms tumor. PTS: 1 REF: Pages 1385-1386 14. Which anomaly is often associated with Wilms tumor? a. Renal anaplasia c. Anemia b. Aniridia d. Hypothyroidism Aniridia (lack of an iris in the eye) is an anomaly often associated with Wilms tumor. Approximately 10% of children who have Wilms tumor also have a loss of other important genes and therefore have a number of congenital anomalies. The other anomalies listed are not associated with a Wilms tumor. PTS: 1 REF: Pages 1385-1386 15. Which statement is false about the causes of enuresis? a. A maturational lag may cause enuresis. b. Enuresis may be related to increased light sleep. c. Obstructive sleep apnea may be a symptom of enuresis. d. Excessive nocturnal levels of vasopressin may cause enuresis. Children who do not have the normal nocturnal elevation of vasopressin produce a higher volume of urine with a lower osmolality. The other options are accurate statements regarding enuresis. PTS: 1 REF: Pages 1388-1389 16. When does an individual have their full complement of renal nephrons? a. At birth c. At puberty b. At 6 months of age d. Between the ages 18 and 21 years All the nephrons are present at birth, and their number does not increase as the kidney grows and matures. PTS: 1 REF: Pages 1376-1377 MULTIPLE RESPONSE 17. Which statements are true regarding the narrow chemical safety margin that infants demonstrate? (Select all that apply.) a. The immaturity of tubules may diminish the response to antidiuretic hormone (ADH). b. An immature tubular transport capacity impairs the excretion of potassium. c. An immature tubular transport capacity impairs the reabsorption of bicarbonate. d. The immaturity of tubules may diminish the response to aldosterone. e. The safety margin begins to expand after 2 years of age. , B, C, E NURSINGTB.COM Because of a high hydrogen ion concentration, a limited ability to regulate the internal environment, and a lowered osmotic pressure, the infant’s renal system has a narrow chemical safety margin. The immaturity and smaller surface area of the tubules also may diminish the water reabsorption response to ADH. An immature tubular transport capacity means that the ability to excrete a potassium load, reabsorb bicarbonate, or buffer hydrogen with ammonia does not become efficient until approximately 2 years of age. PTS: 1 REF: Page 1378 18. The excretion of urea is low in infants because of which feature? (Select all that apply.) a. Medullary nephrons with comparatively short loops at this stage of development b. Immature tubular transport capacity, impairing the excretion of urea c. High anabolic state d. Dilute urine as a result of the immaturity of an infant’s glomeruli e. Available protein used for physical growth , E Urea excretion is low in infants primarily because infants are in a high anabolic state and use their protein for growth. The other options are not involved in their low urea excretion. PTS: 1 REF: Page 1378 19. Which factors are involved in the development of hypospadias? (Select all that apply.) a. Disruption in male hormones, including testosterone b. Mutation of gene HP-1 (chromosome 16) c. 5-reductase mutations d. Hormones administered for in vitro fertilization e. Advanced maternal age , C, D, E The cause of hypospadias is multifactorial and related to disruptions in male hormones, including testosterone biosynthesis defects, 5-reductase mutations, hormones administered for in vitro fertilization, advanced maternal age, and other environmental factors. A mutation of gene HP-1 (chromosome 16) is not relevant. PTS: 1 REF: Page 1378 20. Which cells of the inflammatory process are found in acute poststreptococcal glomerulonephritis? (Select all that apply.) a. Immunoglobulin G (IgG) b. Immunoglobulin A (IgA) c. Complement C3 d. Immunoglobulin E (IgE) e. Immune complexes , B, C, E Antigen-antibody complexes of IgG, IgA, and C3 complement are deposited in the glomerulus, or the antigen may be trapped within the glomerulus and immune complexes formed in situ. IgE is not relevant to this situation. PTS: 1 REF: Page 13N8U1RSINGTB.COM 21. Which symptoms are considered part of the nephrotic syndrome in children? (Select all that apply.) a. Proteinuria b. Pyuria c. Hyperlipidemia d. Edema e. Hypoalbuminemia , C, D, E Nephrotic syndrome is a term used to describe a symptom complex characterized by proteinuria, hypoalbuminemia, hyperlipidemia, and edema. Pyuria is not observed in this condition. PTS: 1 REF: Page 1383 22. Which statements are true regarding hemolytic uremic syndrome (HUS)? (Select all that apply.) a. Microangiopathic hemolytic anemia characterizes HUS. b. Thrombocytopenia is a comorbid condition. c. Wilms tumors are often the trigger for HUS. d. HUS is the most common community-acquired cause of acute renal failure in young children. e. HUS is chronic in nature. , B, D HUS is an acute disorder characterized by microangiopathic hemolytic anemia and thrombocytopenia and is the most common community-acquired cause of acute renal failure in young children. Wilms tumors are not necessarily associated with this disorder. PTS: 1 REF: Pages 1382-1383 23. What problems are commonly associated with the diagnosis of horseshoe kidneys? (Select all that apply.) a. Hydronephrosis b. Nephritis c. Infection d. Kidney stones e. Pyuria , C, D Approximately one-third of individuals with horseshoe kidneys are asymptomatic, and the most common problems are hydronephrosis, infection, and stone formation. Nephritis and pyuria are not associated with this diagnosis. PTS: 1 REF: Page 1378 24. Which structural anomalies are associated with urinary tract malformations? (Select all that apply.) a. Low-set ears b. Prune-belly syndrome c. Broad-bridged nose d. Imperforate anus e. Malformed lips , B, D NURSINGTB.COM Structural anomalies that are associated with urinary tract malformations include low-set, malformed ears; absent abdominal muscles (prune-belly syndrome); and imperforate anus or genital deviation. Anomalies of the either the nose or the lips are not generally associated with urinary tract malformations. PTS: 1 REF: Page 1378 MATCHING Match the kidney disorder with the corresponding descriptions. A. Hemolytic-uremic syndrome B. Henoch-Schönlein purpura nephritis C. Renal dysplasia D. Ureteropelvic junction obstruction E. Polycystic kidney disease 25. Is usually the result of abnormal differentiation of the renal tissues. 26. Is an autosomal dominant inherited disorder. 27. Fibrin-rich thrombi can be found throughout the microcirculation. 28. Is the most common cause of hydronephrosis in neonates. 29. Immunoglobulin A (IgA) nephropathy causes inflammation to glomerular blood vessels. 25. ANS: C PTS: 1 REF: Page 1380 MSC: Renal dysplasia usually results from abnormal differentiation of the renal tissues. 26. ANS: E PTS: 1 REF: Page 1381 MSC: Polycystic kidney disease is an autosomal dominant inherited disorder that occurs in approximately 1 in 1000 live births. 27. ANS: A PTS: 1 REF: Pages 1382-1383 MSC: Hemolytic-uremic syndrome (HUS) results in fibrin-rich thrombi found throughout the microcirculation. 28. ANS: D PTS: 1 REF: Page 1380 MSC: Ureteropelvic junction obstruction is the most common cause of hydronephrosis in neonates. 29. ANS: B PTS: 1 REF: Page 1382 MSC: Henoch-Schönlein purpura nephritis, also known as anaphylactoid purpura, is an IgA nephropathy that affects the glomerular blood vessels, causing inflammation and damage to the vessel wall. NURSINGTB.COM Chapter 41: Structure and Function of the Digestive System MULTIPLE CHOICE 1. In the mouth and stomach, salivary -amylase initiates the digestion of which nutrients? a. Proteins c. Fats b. Carbohydrates d. Fiber Salivary -amylase is an enzyme that initiates only carbohydrate digestion in the mouth and stomach. PTS: 1 REF: Page 1395 2. Which elements in saliva protect against tooth decay? a. Salivary -amylase and ptyalin b. Secretin and IgA c. Endogenous enamelin and salivary -amylase d. Exogenous fluoride and a pH of 7.4 The bicarbonate concentration of saliva sustains a pH of approximately 7.4, which neutralizes bacterial acids and prevents tooth decay. Exogenous fluoride (e.g., fluoride in drinking water) is absorbed and then secreted in the saliva, providing additional protection against tooth decay. Decay prevention is not associated with any of the other options. PTS: 1 REF: Page 13N9U5RSINGTB.COM 3. Saliva contains which immunoglobulin (Ig)? a. IgA c. IgG b. IgE d. IgM Saliva contains only IgA, which helps prevent infection. PTS: 1 REF: Page 1395 4. What effect is a result of inhibiting the parasympathetic nervous system with a drug such as atropine? a. Salivation becomes thinner. c. The pH of saliva changes. b. Salivation decreases. d. Digestive enzymes are inhibited. The sympathetic and parasympathetic divisions of the autonomic nervous system control salivation. Because cholinergic parasympathetic fibers stimulate the salivary glands, atropine (an anticholinergic agent) inhibits salivation and makes the mouth dry. None of the other options is a result of drugs such as atropine. PTS: 1 REF: Page 1395 5. Food enters the stomach via which sphincter? a. Cardiac c. Gastric b. Upper esophageal d. Fundal Each end of the esophagus is opened and closed by a sphincter. The upper esophageal sphincter (cricopharyngeal muscle) prevents entry of air into the esophagus during respiration. The lower esophageal sphincter (cardiac sphincter) prevents regurgitation from the stomach. The lower esophageal sphincter is located near the esophageal hiatus—the opening in the diaphragm where the esophagus ends at the stomach. The cardiac sphincter is the only option that fulfills the function described in the question. PTS: 1 REF: Page 1395 6. Which gastric cells secrete hydrochloric acid and intrinsic factor? a. Parietal c. G b. Chief d. H Of the available options, only the parietal cells (oxyntic cells) secrete hydrochloric acid and intrinsic factor. PTS: 1 REF: Page 1398 7. Which cells in the stomach secrete histamine? a. Oxyntic c. D b. Chief d. Enterochromaffin-like NURSINGTB.COM Of the available options, only enterochromaffin-like cells secrete histamine. PTS: 1 REF: Page 1398 8. The presence of chyme in the duodenum stimulates which hormones? a. Motilin and histamine b. Secretin and cholecystokinin c. Enteroglucagon and gastric inhibitory peptide d. Somatostatin and acetylcholine The movement of chyme from the stomach into the duodenum initiates the intestinal phase of secretion. This phase represents a slowdown of the gastric secretory response; however, the presence of digested protein and amino acids in the duodenum continue to stimulate some gastric secretion. The release of secretin and cholecystokinin stimulate pancreatic secretions and inhibit gastric secretions. This selection is the only option that correctly identifies the hormones that are stimulated by the presence of chyme in the duodenum. PTS: 1 REF: Page 1400 9. Which gastric hormone inhibits acid and pepsinogen secretion, as well as decrease the release of gastrin? a. Bombesin c. Somatostatin b. Histamine d. Acetylcholine Of the options available, only somatostatin inhibits the secretion of acid and pepsinogen and decreases gastrin release. PTS: 1 REF: Page 1397 | Table 40-1 10. Which enzyme breaks down protein-forming polypeptides in the stomach? a. Acetylcholine c. Gastrin b. Pepsin d. Secretin Of the options available, only pepsin, a proteolytic enzyme, breaks down protein-forming polypeptides in the stomach. PTS: 1 REF: Page 1399 11. Exposure to which substance protects the mucosal barrier of the stomach? a. Prostaglandins c. Helicobacter pylori b. Aspirin d. Regurgitated bile Prostaglandins and enterogastrones, such as gastric inhibitory peptide, somatostatin, and secretin, inhibit acid secretion. This selection is the only option that accurately identifies a substance that protects the mucosal barrier of the stomach. PTS: 1 REF: Page 1399 12. The ileum and jejunum are suspenNdUeRdSbIyNGfoTlBd.sCoOfMthe peritoneum that contain an extensive vascular and nervous network. What are these folds called? a. Ligament of Treitz c. Auerbach folds b. Mesentery d. Lamina propria The ileum and jejunum are suspended in loose folds from the posterior abdominal wall by a peritoneal membrane called the mesentery. The mesentery facilitates intestinal motility and supports blood vessels, nerves, and lymphatics. None of the other options accurately fills this description. PTS: 1 REF: Page 1401 13. Where in the small intestines are lymphocytes, plasma cells, and macrophages produced? a. Brush border c. Lamina propria b. Microvilli d. Crypts of Lieberkühn The lamina propria, which is a connective tissue layer of the mucous membrane, lies beneath the epithelial cells of the villi and contains lymphocytes, plasma cells, which produce immunoglobulins, and macrophages. None of the other options performs the described function. PTS: 1 REF: Page 1401 14. Why are water and electrolytes transported in both directions through tight junctions and intercellular spaces rather than across cell membranes? a. The intercellular hydrostatic pressure is inadequate to push the water and electrolytes across the cell membranes. b. A balance of cations and ions among the electrolytes on each side of the cell membranes cannot be maintained. c. The epithelial cell membranes are formed of lipids that are hydrophobic and therefore repel water. d. Receptors on those cell membranes are occupied with a diffusion of amino acids and monosaccharides. The epithelial cell membranes of the small intestine are formed of lipids and are hydrophobic or tend to repel water. Therefore water and electrolytes are transported in both directions—toward the capillary blood or toward the intestinal lumen—through the tight junctions and intercellular spaces rather than across cell membranes. This selection is the only option that accurately describes why water and electrolytes are transported in both directions. PTS: 1 REF: Pages 1401-1402 15. Which statement best describes the gastrointestinal tract? a. The gastrointestinal tract is a muscular tube that transports food from the mouth to the stomach. b. The gastrointestinal tract is a hollow tube that extends from the mouth to the anus. c. The gastrointestinal tract is a baglike structure that propels partially digested food (chyme). NURSINGTB.COM d. The structure is 5 m long and consists of three segments. The gastrointestinal tract is a hollow tube that extends from the mouth to the anus. The esophagus is a muscular tube that transports food from the mouth to the stomach. The stomach is a baglike structure that secretes digestive juices, mixes and stores food, and propels partially digested food (chyme) into the duodenum. The small intestine is 5 m long and has three segments. PTS: 1 REF: Page 1395 16. Glucose transport enhances the absorption of which electrolyte? a. Sodium c. Potassium b. Phosphate d. Chloride Sodium passes through the tight junctions and is actively transported across cell membranes. Sodium and glucose share a common active transport carrier (sodium-glucose ligand transporter 1 [SGLT1]). This statement is not true of any other option. PTS: 1 REF: Page 1402 17. What process is capable of increasing both intrathoracic and intraabdominal pressure, thereby facilitating defecation? a. Relaxation of the internal anal sphincter b. Intestinal peristalsis c. Valsalva maneuver d. Ileogastric reflex Squatting or sitting facilitate defecation; these positions straighten the angle between the rectum and anal canal and increase the efficiency of straining (increasing intraabdominal pressure). Initiating the Valsalva maneuver increases intraabdominal pressure. This maneuver consists of inhaling and forcing the diaphragm and chest muscles against the closed glottis and increases both intrathoracic and intraabdominal pressure, which is transmitted to the rectum. None of the other options facilitate defecation as described. PTS: 1 REF: Page 1408 18. Which pancreatic enzyme is responsible for the breakdown of carbohydrates? a. Trypsin c. Lipase b. Amylase d. Chymotrypsin Salivary and pancreatic amylases break down starches to oligosaccharides by splitting -1,4-glucosidic linkages of long-chain molecules. None of the other options is relevant to this process. PTS: 1 REF: Page 1402 19. The formation of water-soluble molecules to facilitate the absorption of the by-products of lipid hydrolysis is accomplished bNyU: RSINGTB.COM a. Micelles c. Chylomicrons b. Phospholipase d. Colipase The products of lipid hydrolysis must be made water soluble if they are to be efficiently absorbed from the intestinal lumen. The formation of water-soluble molecules known as micelles (see Figure 40-14) accomplishes this process. This selection is the only option that accurately identifies the molecule needed to facilitate lipid hydrolysis. PTS: 1 REF: Page 1404 20. What is the primary source of physiologic iron? a. Transferrin from plasma c. Bile from bilirubin b. Pepsin form pepsinogen d. Heme from animal protein The primary source of iron is heme from animal protein. The other options are not considered primary sources of physiologic iron. PTS: 1 REF: Page 1405 21. Which statement is incorrect regarding the characteristics of vitamin B12? a. Vitamin B12 is absorbed in the terminal ileum. b. Vitamin B12 is absorbed in its free (unbound) form but only in small amounts. c. Vitamin B12 is necessary for platelet maturation. d. Vitamin B12 binds to intrinsic factor. Vitamin B12 is not necessary for platelet maturation. Most vitamin B12 (cobalamin) is bound to intrinsic factor (making it resistant to digestion) and is absorbed in the terminal ileum, although a small amount of the vitamin is absorbed in its free (unbound) form. PTS: 1 REF: Page 1406 22. Which water-soluble vitamin is absorbed by passive diffusion? a. Vitamin B6 c. Vitamin K b. Vitamin B1 d. Folic acid Of the options available, only Vitamin B6 is the water-soluble vitamin absorbed by passive diffusion. PTS: 1 REF: Page 1406 | Table 40-2 23. Which vitamin facilitates the absorption of iron by the epithelial cells of the duodenum and jejunum? a. B6 c. E b. C d. B12 Of the options available, only vitamin C reduces ferric iron to ferrous iron, which is the form more easily absorbed by the epithelial cells of the duodenum and jejunum. NURSINGTB.COM PTS: 1 REF: Page 1405 24. What is the role of the normal intestinal bacterial flora? a. Metabolizing bile salts, estrogens, and lipids b. Breaking down proteins into amino acids c. Facilitating the motility of the colon d. Metabolizing aldosterone and insulin The intestinal bacteria play a role in the metabolism of bile salts, contributing to the intestinal reabsorption of bile and the elimination of toxic bile metabolites. These bacteria also play a role in the metabolism of estrogens, androgens, and lipids, as well as in the conversion of unabsorbed carbohydrates to absorbable organic acids, the synthesis of vitamin K2, and the metabolism of various nitrogenous substances and drugs. This selection is the only option that accurately describes the role of normal intestinal bacterial flora. PTS: 1 REF: Page 1409 25. Kupffer cells are best described as: a. Natural killer cells that produce interferon-gamma (IFN-) b. Contractile and therefore capable of regulating the sinusoid blood flow c. Bactericidal and therefore central to innate immunity d. Able to metabolize estrogen, progesterone, and androgens The sinusoids are lined with phagocytic cells, known as Kupffer cells, which are part of the mononuclear phagocyte system and are the largest population of tissue macrophages in the body. They are bactericidal and central to innate immunity. None of the other options accurately describe Kupffer cells. PTS: 1 REF: Pages 1409-1410 26. Bilirubin is a by-product of the destruction of which aged cells? a. Platelets c. Leukocytes b. Protein d. Erythrocytes Bilirubin is a by-product of only the destruction of aged red blood cells or erythrocytes. PTS: 1 REF: Page 1411 27. The process of conjugation of bilirubin in the liver is best described as which transformation? a. Unconjugated (fat-soluble) bilirubin into urobilinogen b. Unconjugated (fat-soluble) bilirubin into conjugated (water-soluble) bilirubin c. Conjugated (water-soluble) bilirubin into unconjugated (fat-soluble) bilirubin d. Conjugated (water-soluble) bilirubin into urobilinogen In the liver, unconjugated bilirubin moves from plasma in the sinusoids into the hepatocytes. Within hepatocytes NURSINGTB.COM acid to form conjugated bilirubin, which is water-soluble. This selection is the only option that accurately describes the transformation associated with the conjugation of bilirubin. PTS: 1 REF: Pages 1411-1412 28. Which statement is incorrect regarding gallbladder function? a. Within 30 minutes of eating, the gallbladder forces bile into the stomach. b. Cholinergic branches of the vagus nerve mediate gallbladder contraction. c. Cholecystokinin provides hormonal regulation of gallbladder contraction. d. The sphincter of Oddi controls the flow of bile from the gallbladder. Within 30 minutes after eating, the gallbladder begins to contract and the sphincter of Oddi relaxes, forcing bile into the duodenum through the major duodenal papilla. The other options are correct statements regarding the functioning of the gallbladder. PTS: 1 REF: Page 1413 29. Which structure synthesizes clotting factors and the vitamin K necessary for hemostasis? a. Colon c. Gallbladder b. Spleen d. Liver The liver has hemostatic functions. It synthesizes prothrombin, fibrinogen, and factors I, II, VII, IX, and X, all of which are necessary for effective clotting. Vitamin K, a fat-soluble vitamin, is essential for the synthesis of other clotting factors. Because bile salts are needed for the absorption of fats, vitamin K absorption depends on adequate bile production in the liver. Impairment of vitamin K absorption diminishes the production of clotting factors and increases the risk of bleeding. The other structures mentioned are not associated with synthesizing of clotting factors and vitamin K. PTS: 1 REF: Page 1412 30. How many days does it take for the entire epithelial population of the small intestines to be replaced? a. 30 to 45 c. 7 to 15 b. 15 to 25 d. 4 to 7 The entire epithelial population is replaced approximately every 4 to 7 days. PTS: 1 REF: Page 1401 31. Which statement is true regarding the state of the intestinal tract at birth? a. The intestinal tract is colonized by Escherichia coli. b. The intestinal tract is sterile. c. Clostridium welchii is present in the intestinal tract but in very small numbers. d. Streptococcus colonization in the intestinal tract has begun. The intestinal tract is sterile at birtNhUbRuStINbeGcToBm.CeOs Mcolonized with Escherichia coli, Clostridium welchii, and Streptococcus within a few hours. PTS: 1 REF: Page 1409 MULTIPLE RESPONSE 32. Gastric emptying is delayed by the presence of which substances? (Select all that apply.) a. Solids b. Carbohydrates c. Nonisotonic solutions d. Bacteria e. Fats , C, E Of the available options, only solids, fats, and nonisotonic solutions delay gastric emptying. PTS: 1 REF: Page 1397 33. Which statements are true regarding the ileogastric reflex? (Select all that apply.) a. The purpose of ileogastric reflex is to inhibit gastric motility. b. Ileum distension triggers the ileogastric reflex. c. The ileogastric reflex causes the relaxation of the ileocecal sphincter. d. Increased gastric secretion triggers the ileogastric reflex. e. The ileogastric reflex stimulates an increase in ileal motility. , B The ileogastric reflex inhibits gastric motility when the ileum becomes distended. The gastroileal reflex, which is activated by an increase in gastric motility and secretion, stimulates an increase in ileal motility and the relaxation of the ileocecal sphincter. PTS: 1 REF: Page 1407 34. Which hormones are involved in the relaxation of the stomach’s fundus during swallowing? (Select all that apply.) a. Progesterone b. Glucagon c. Motilin d. Gastrin e. Cholecystokinin , E Swallowing causes the fundus to relax (receptive relaxation) to receive a bolus of food from the esophagus. Relaxation is coordinated by efferent, nonadrenergic, noncholinergic vagal fibers and, of the available options, is facilitated only by gastrin and cholecystokinin, two polypeptide hormones secreted by the gastrointestinal mucosa. PTS: 1 REF: Page 1397 35. Which hormones are involved in regulating gastric motility by making the threshold potential of muscle fibers more neNgUatRivSIeN?G(TSeBl.eCcOtMall that apply.) a. Estrogen b. Secretin c. Somatostatin d. Gastrin e. Motilin , D, E Gastrin and motilin (small intestine hormones) and the vagus nerve increase contraction by making the threshold potential of muscle fibers less negative. Sympathetic activity and secretin (another small intestine hormone) are inhibitory and make threshold potential more negative. The rate of peristalsis is mediated by pacemaker cells that initiate a wave of depolarization (basic electrical rhythm), which moves from the upper part of the stomach to the pylorus. Neither estrogen nor somatostatin inhibits gastric motility as described in the question. PTS: 1 REF: Page 1397 36. What requirements are necessary for calcium to be absorbed through the ileum at concentrations of less than 5 mmol/L? (Select all that apply.) a. Receptor site on the ileum b. Vitamin D3 c. Vitamin K d. Carboxypeptidase e. A carrier protein , E At concentrations less than 5 mmol/L, calcium is transported actively across cell membranes, bound to a carrier protein. The carrier formation requires the presence of the active form of vitamin D3 (1,25-dihydroxyvitamin D). These selections are the only options relevant to the transport of calcium. PTS: 1 REF: Page 1405 37. Which water-soluble vitamins are dependent on sodium for absorption? (Select all that apply.) a. Pantothenic acid b. Vitamin B1 c. Vitamin C d. Vitamin B12 e. Folic acid , E Of the options available, only vitamin C and folic acid are water-soluble vitamins that are dependent on sodium for absorption. PTS: 1 REF: Page 1406 | Table 40-2 38. Which statement is correct regarding the functions of the pancreas? (Select all that apply.) a. Cholecystokinin stimulates the release of pancreatic enzymes. b. Bilirubin and S cells inhibit the secretion of pancreatic enzymes. c. Pancreatic polypeptide is releaNsUedRSaIfNteGrTeBa.tCinOgM. d. Acetylcholine (ACh) is liberated from the pancreatic branches of the vagus nerve. e. ACh stimulates the release of pancreatic enzymes. , C, D Enzymatic secretion follows, stimulated by cholecystokinin, which activates ACh from the vagus nerve and the release of ACh from pancreatic stellate cells. Cholecystokinin is released in the duodenum in response to the essential amino and fatty acids already present in chyme. Once in the small intestine, activated pancreatic enzymes inhibit the release of more cholecystokinin and ACh. This feedback mechanism inhibits the secretion of more pancreatic enzymes. Pancreatic polypeptide is released after eating and inhibits postprandial pancreatic exocrine secretion. (Table 40-1 summarizes the hormonal stimulation of pancreatic secretions.) PTS: 1 REF: Page 1415 MATCHING Match the hormone from the small intestine with its action. Hormones may be used more than once. A. Peptide YY B. Secretin C. Cholecystokinin D. Enteroglucagon E. Pancreatic polypeptide 39. Stimulates the gallbladder to eject bile and the pancreas to secrete alkaline fluid. 40. Stimulates the pancreas to secrete alkaline pancreatic juices. 41. Delays gastric and small bowel emptying. 42. Decreases pancreatic and enzyme secretions. 43. Enhances insulin release, lipolysis, and ketogenesis. 39. ANS: MSC: fluid. C PTS: 1 REF: Page 1397 | Table 40-1 Cholecystokinin stimulates the gallbladder to eject bile and the pancreas to secrete alkaline 40. ANS: MSC: B PTS: 1 REF: Page 1397 | Table 40-1 Secretin stimulates the pancreas to secrete alkaline pancreatic juice. 41. ANS: MSC: A PTS: 1 REF: Page 1397 | Table 40-1 Peptide YY delays gastric and small bowel emptying. 42. ANS: MSC: E PTS: 1 REF: Page 1397 | Table 40-1 Pancreatic polypeptide decreases pancreatic and enzyme secretions. 43. ANS: MSC: D PTS: 1 REF: Page 1397 | Table 40-1 Enteroglucagon enhances insulin release, lipolysis, and ketogenesis. NURSINGTB.COM Chapter 42: Alterations of Digestive Function MULTIPLE CHOICE 1. Where in the brain is the vomiting center located? a. Hypothalamus c. Pons b. Medulla oblongata d. Midbrain The vomiting center of the brain lies in the medulla oblongata. The other locations listed are not related to vomiting. PTS: 1 REF: Page 1424 2. Antiemetic agents, such as domperidone and haloperidol, are antagonists for which receptors? a. 5-Hydroxytryptamine (5-HT) serotonin b. Histamine-2 c. Acetylcholine d. Dopamine Metoclopramide, domperidone, and haloperidol are dopamine antagonists, making them effective antiemetic agents. This selection is the only option that identifies a receptor that is involved in the process of vomiting. PTS: 1 REF: Page 14N2U4RSINGTB.COM 3. What type of vomiting is caused by the direct stimulation of the vomiting center by neurologic lesions involving the brainstem? a. Retch c. Duodenal b. Periodic d. Projectile Of the available options, only projectile vomiting is caused by the direct stimulation of the vomiting center by neurologic lesions, such as increased intracranial pressure, tumors, or aneurysms involving the brainstem. PTS: 1 REF: Page 1424 4. Considering the normal frequency of bowel evacuation, how infrequently can evacuation occur and still be considered within normal range? a. Once a day c. Once a week b. Once every 2 days d. Once every 2 weeks Normal bowel habits range from two or three evacuations per day to one per week. PTS: 1 REF: Page 1428 5. How many stools per day are considered the upper limits of normal? a. Two c. Five b. Three d. Seven More than three stools per day is considered abnormal. PTS: 1 REF: Page 1428 6. The adult intestine processes approximately how many liters of luminal content per day? a. 3 c. 9 b. 6 d. 12 The adult intestine processes approximately 9 L of luminal content per day. Of this amount, 2 L is ingested and the remaining 7 L consists of intestinal secretions. PTS: 1 REF: Page 1425 7. A person who has cholera would be expected to have which type of diarrhea? a. Osmotic c. Small volume b. Secretory d. Motility Primary causes of secretory diarrhea are bacterial enterotoxins, particularly those released by cholera or strains of Escherichia coli, and neoplasms, such as gastrinoma or thyroid carcinoma. None of the other options are associated with secretory diarrhea. PTS: 1 REF: Page 1425 NURSINGTB.COM 8. What type of diarrhea is a result of lactase deficiency? a. Motility c. Secretory b. Osmotic d. Small-volume Malabsorption related to lactase deficiency, pancreatic enzyme or bile salt deficiency, small intestine bacterial overgrowth, and celiac disease cause osmotic diarrhea. None of the other options are associated with lactase deficiencies. PTS: 1 REF: Page 1425 9. Which statement is false concerning how abdominal pain is produced? a. Chemical mediators, such as histamine, bradykinin, and serotonin, produce abdominal pain. b. Edema and vascular congestion produce abdominal pain by stretching. c. Ischemia, caused by distention of bowel obstruction or mesenteric vessel thrombosis, produces abdominal pain. d. Low concentrations of anaerobes, such as Streptococci, Lactobacilli, Staphylococci, Enterobacteria, and Bacteroides, produce abdominal pain. Low concentrations of anaerobes are not typically a cause of abdominal pain. PTS: 1 REF: Page 1426 10. How can abdominal pain that is visceral in nature best be described? a. Abdominal pain that is visceral in nature is diffused, vague, poorly localized, and dull. b. It travels from a specific organ to the spinal cord. c. The pain lateralizes from only one side of the nervous system. d. Abdominal pain is associated with the peristalsis of the gastrointestinal tract. Pain is usually felt near the midline in the epigastrium (upper midabdomen), midabdomen, or lower abdomen. The pain is poorly localized, is dull rather than sharp, and is difficult to describe. None of the other options accurately describe this type of pain. PTS: 1 REF: Page 1426 11. What is the cause of gastroesophageal reflux disease? a. Excessive production of hydrochloric acid b. Zone of low pressure of the lower esophageal sphincter c. Presence of Helicobacter pylori in the esophagus d. Reverse muscular peristalsis of the esophagus Normally, the resting tone of the lower esophageal sphincter maintains a zone of high pressure that prevents gastroesophageal reflux. In individuals who develop reflux esophagitis, this pressure tends to be lower than normal from either transient relaxation or a weakness of the sphincter. This selection is the only option that accurately describes the cause of gastroesophageal reflux disease. NURSINGTB.COM PTS: 1 REF: Page 1429 12. What term is used to identify frank bleeding of the rectum? a. Melena c. Occult bleeding b. Hematochezia d. Hematemesis Hematochezia is the only available option that is associated with frank bright red or burgundy blood from the rectum. PTS: 1 REF: Page 1428 13. What is the cause of functional dysphagia? a. Intrinsic mechanical obstruction c. Tumor b. Extrinsic mechanical obstruction d. Neural or muscular disorders Neural or muscular disorders that interfere with voluntary swallowing or peristalsis cause functional dysphagia. This selection is the only option that accurately identifies a cause of functional dysphagia. PTS: 1 REF: Page 1428 14. What is the cause of reflux esophagitis? a. Immune response to gastroesophageal reflux b. Delayed gastric emptying c. Congenital anomaly d. Secretory response to gastroesophageal reflux Delayed gastric emptying contributes to reflux esophagitis by (1) lengthening the period during which reflux is possible and (2) increasing the acid content of chyme. None of the other options are accurate descriptions of the cause of reflux esophagitis. PTS: 1 REF: Page 1429 15. By what mechanism does intussusception cause an intestinal obstruction? a. Telescoping of part of the intestine into another section of intestine, usually causing strangulation of the blood supply b. Twisting the intestine on its mesenteric pedicle, causing occlusion of the blood supply c. Loss of peristaltic motor activity in the intestine, causing an adynamic ileus d. Forming fibrin and scar tissue that attach to the intestinal omentum, causing obstruction Intussusception is the telescoping of part of the intestine into another section of intestine, usually causing strangulation of the blood supply. This selection is the only option that accurately describes how intussusception causes an intestinal obstruction. PTS: 1 REF: Page 1431 | Table 41-2 NURSINGTB.COM 16. What is the most immediate result of a small intestinal obstruction? a. Vomiting c. Electrolyte imbalances b. Dehydration d. Distention Distention begins almost immediately, as gases and fluids accumulate proximal to the obstruction. Within 24 hours, up to 8 L of fluid and electrolytes enters the lumen in the form of saliva, gastric juice, bile, pancreatic juice, and intestinal secretions. Copious vomiting or sequestration of fluids in the intestinal lumen prevents their reabsorption and produces severe fluid and electrolyte disturbances. PTS: 1 REF: Pages 1431-1432 17. An intestinal obstruction at the pylorus or high in the small intestine causes metabolic alkalosis by causing which outcome? a. Gain of bicarbonate from pancreatic secretions that cannot be absorbed b. Excessive loss of hydrogen ions normally absorbed from gastric juices c. Excessive loss of potassium, promoting atony of the intestinal wall d. Loss of bile acid secretions that cannot be absorbed If the obstruction is at the pylorus or high in the small intestine, then metabolic alkalosis initially develops as a result of excessive loss of hydrogen ions that normally would be reabsorbed from the gastric juices. This selection is the only option that accurately describes the cause of metabolic alkalosis in this situation. PTS: 1 REF: Page 1432 18. What are the cardinal symptoms of small intestinal obstruction? a. Constant, dull pain in the lower abdomen relieved by defecation b. Acute, intermittent pain 30 minutes to 2 hours after eating c. Colicky pain caused by distention, followed by vomiting d. Excruciating pain in the hypogastric area caused by ischemia Of the options available, only colicky pain caused by distention followed by vomiting are considered the cardinal symptoms of a small intestinal obstruction. PTS: 1 REF: Pages 1432-1433 19. What is a cause of chronic antral gastritis? a. Helicobacter pylori bacteria b. Development of autoantibodies to gastric H+/K+ ATPase c. Pernicious anemia d. Reflux of bile and alkaline pancreatic secretions Chronic antral gastritis generally involves only the antrum and is more common than fundal gastritis. It is caused by H.NpUylRoSrIiNbGaTcBte.CriOa Mor the chronic use of alcohol, tobacco, and nonsteroidal antiinflammatory drugs. None of the other options are associated with the cause of chronic antral gastritis. PTS: 1 REF: Page 1435 20. What is the primary cause of peptic ulcers? a. Hypersecretion of gastric acid c. Helicobacter pylori b. Hyposecretion of pepsin d. Escherichia coli Infection with H. pylori is a primary cause of peptic ulcers. PTS: 1 REF: Page 1435 21. A peptic ulcer may occur in all of the following areas except the: a. Stomach c. Jejunum b. Duodenum d. Esophagus A peptic ulcer is a break, or ulceration, in the protective mucosal lining of the lower esophagus, stomach, or duodenum. This type of ulcer is not associated with the jejunum. PTS: 1 REF: Page 1435 22. Which statement is false regarding the contributing factors of duodenal ulcers? a. Bleeding from duodenal ulcers causes hematemesis or melena. b. Gastric emptying is slowed, causing greater exposure of the mucosa to acid. c. The characteristic pain begins 30 minutes to 2 hours after eating when the stomach is empty. d. Duodenal ulcers occur with greater frequency than other types of peptic ulcers. Duodenal ulcers can be associated with altered mucosal defenses, rapid gastric emptying, elevated serum gastrin levels, or acid production stimulated by smoking. The other options provide correct information regarding duodenal ulcers. PTS: 1 REF: Page 1435 23. After a partial gastrectomy or pyloroplasty, clinical manifestations that include increased pulse, hypotension, weakness, pallor, sweating, and dizziness are the results of which mechanism? a. Anaphylactic reaction in which chemical mediators, such as histamine, prostaglandins, and leukotrienes, relax vascular smooth muscles, causing shock b. Postoperative hemorrhage during which a large volume of blood is lost, causing hypotension with compensatory tachycardia c. Concentrated bolus that moves from the stomach into the small intestine, causing hyperglycemia and resulting in polyuria and eventually hypovolemic shock d. Rapid gastric emptying and the creation of a high osmotic gradient in the small intestine, causing a sudden shift of fluid from the blood vessels to the intestinal lumen NURSINGTB.COM Dumping syndrome occurs with varying severity in 5% to 10% of individuals who have undergone partial gastrectomy or pyloroplasty. Rapid gastric emptying and the creation of a high osmotic gradient in the small intestine cause a sudden shift of fluid from the vascular compartment to the intestinal lumen. Plasma volume decreases, causing vasomotor responses, such as increased pulse rate, hypotension, weakness, pallor, sweating, and dizziness. Rapid distention of the intestine produces a feeling of epigastric fullness, cramping, nausea, vomiting, and diarrhea. This selection is the only option that accurately identifies the mechanism responsible for the described situation. PTS: 1 REF: Page 1440 24. Which statement is consistent with dumping syndrome? a. Dumping syndrome usually responds well to dietary management. b. It occurs 1 to 2 hours after eating. c. Constipation is often a result of the dumping syndrome. d. It can result in alkaline reflux gastritis. Most individuals with the dumping syndrome respond well to dietary management. None of the other options is associated with the dumping syndrome. PTS: 1 REF: Page 1440 25. What stimulates the desire to eat? a. Agouti-related protein (AgRP) b. Alpha-melanocyte–stimulating hormone (-MSH) c. Cocaine- and amphetamine-regulated transcript (CART) d. Peptide YY (PYY) Specific neurons produce neuropeptide Y (NPY) and AgRP, which stimulates eating and decreases metabolism (anabolic). PTS: 1 REF: Page 1448 26. Which structure regulates eating behavior and energy metabolism? a. Anterior pituitary c. Posterior pituitary b. Hypothalamus d. Parietal lobe The arcuate nucleus (ARC) in the hypothalamus has two sets of neurons with opposing effects that interact to regulate and balance food intake and energy metabolism. This selection is the only option that regulates eating behavior and energy metabolism. PTS: 1 REF: Pages 1447-1448 27. Which symptom is characteristic of bulimia nervosa? a. Recurrent episodes of binge eating with fears of not being able to stop eating. b. Fear of becoming obese, despite progressive weight loss. c. Perception that the body is fat when it is actually underweight. d. Absence of three consecutive NmUeRnSstIrNuGaTl Bpe.CriOoMds. Diagnosis of bulimia is based on, among other findings, recurrent episodes of binge eating during which the individual fears not being able to stop. The remaining options are characteristic of anorexia nervosa. PTS: 1 REF: Page 1450 | Box 41-5 28. The most common clinical manifestation of portal hypertension is what type of bleeding? a. Rectal c. Esophageal b. Duodenal d. Intestinal The vomiting of blood from bleeding esophageal varices is the most common clinical manifestation of portal hypertension. PTS: 1 REF: Page 1453 29. What is the most common manifestation of portal hypertension–induced splenomegaly? a. Leukopenia c. Erythrocytopenia b. Thrombocytopenia d. Pancytopenia Thrombocytopenia (decreased platelet count) is the most common manifestation of congestive splenomegaly and can contribute to a tendency of increased bleeding. PTS: 1 REF: Page 1452 30. Which statement is false concerning the accumulation of fluid in the peritoneal cavity? a. Impaired excretion of sodium by the kidneys promotes water retention. b. Decreased oncotic pressure and increased hepatic sinusoidal hydrostatic pressure cause the movement of fluid into the peritoneal cavity. c. Decreased blood flow to the kidneys activates aldosterone, which retains sodium. d. Circulating nitric oxide causes vasoconstriction, which forces fluid from the capillaries into the peritoneal cavity. The arterial vasodilation theory proposes that circulating nitric oxide or the release of endotoxin from translocation of intestinal bacteria triggers arterial vasodilation of the splanchnic organs early in the course of cirrhosis and stimulates renal sodium retention through the renin-angiotensin-aldosterone system, increased sympathetic tone, and changes in the intrarenal blood flow. The other options provide accurate information regarding the accumulation of fluid in the peritoneal cavity. PTS: 1 REF: Page 1453 31. Which statement is false regarding the sources of increased ammonia that contribute to hepatic encephalopathy? a. End products of intestinal protein digestion are sources of increased ammonia. b. Digested blood leaking from ruptured varices is a source of increased ammonia. c. Accumulation of short-chain fNatUtyRSaIcNidGsTtBh.aCtOiMs attached to ammonia is a source of increased ammonia. d. Ammonia-forming bacteria in the colon are sources of increased ammonia. The accumulation of short-chain fatty acids, serotonin, tryptophan, and false neurotransmitters probably contributes to neural derangement and is not associated with ammonia levels. The other options provide accurate information regarding how the sources of ammonia contribute to hepatic encephalopathy. PTS: 1 REF: Pages 1454-1455 32. Hepatic fat accumulation is observed in which form of cirrhosis? a. Biliary c. Postnecrotic b. Metabolic d. Alcoholic Alcoholic cirrhosis is a complex process that begins with fatty infiltration (hepatic steatosis). Fat deposition (deposition of triglycerides) within the liver hepatocytes is primarily caused by increased lipogenesis and decreased fatty acid oxidation by hepatocytes. This selection is the only option that accurately identifies the correct form of cirrhosis. PTS: 1 REF: Pages 1460-1461 33. Which statement is false concerning the pathophysiologic process of alcoholic cirrhosis? a. Inflammation and damage leading to cirrhosis begin in the bile canaliculi. b. Alcohol is transformed to acetaldehyde, which promotes liver fibrosis. c. Mitochondrial function is impaired, decreasing oxidation of fatty acids. d. Acetaldehyde inhibits export of proteins from the liver. Biliary cirrhosis differs from alcoholic cirrhosis in that the damage and inflammation leading to cirrhosis begin in bile canaliculi and bile ducts, rather than in the hepatocytes. The other options provide true information regarding the pathophysiologic process of alcoholic cirrhosis. PTS: 1 REF: Pages 1460-1462 34. Which statement is false regarding the pathophysiologic process of acute pancreatitis? a. Bile duct or pancreatic duct obstruction blocks the outflow of pancreatic digestive enzymes. b. Acute pancreatitis can also result from direct cellular injury from drugs or viral infection. c. Acute pancreatitis is an autoimmune disease in which immunoglobulin G (IgG) coats the pancreatic acinar cells; consequently, the pancreatic enzymes destroy the cells. d. Acute pancreatitis is usually mild and spontaneously resolves. The backup of pancreatic secretions and the activation and release of enzymes (activated trypsin activates chymotrypsin, lipase, and elastase) within the pancreatic acinar cells cause acute pancreatitis, an obstruNcUtivReSIdNiGseTaBs.eC.OTMhe activated enzymes cause autodigestion (e.g., proteolysis, lipolysis) of the pancreatic cells and tissues, resulting in inflammation. Acute pancreatitis is usually a mild disease and spontaneously resolves; however, approximately 20% of those with the disease develop a severe acute pancreatitis that requires hospitalization. Pancreatitis develops because of a blockage to the outflow of pancreatic digestive enzymes caused by bile duct or pancreatic duct obstruction (e.g., gallstones). Acute pancreatitis can also result from direct cellular injury from drugs or viral infection. PTS: 1 REF: Page 1464 35. The mutation of which gene is an early event associated with the pathogenetic origin of esophageal cancer? a. K-ras mutation c. myc b. TP53 d. HER2 Mutation of the TP53 gene is an early event associated with esophageal cancer. This selection is the only mutation from among the provided options. PTS: 1 REF: Page 1466 36. Obesity is defined as a body mass index (BMI) greater than what measurement? a. 22 c. 28 b. 25 d. 30 Obesity is an energy imbalance, with caloric intake exceeding energy expenditure, and is defined as a BMI greater than 30. PTS: 1 REF: Page 1446 MULTIPLE RESPONSE 37. Which statements are true regarding parietal pain? (Select all that apply.) a. Parietal pain arises from the parietal peritoneum. b. It is generally more localized than visceral pain. c. Parietal pain is usually less intense than visceral pain. d. Nerve fibers that travel to the spinal cord are involved in parietal pain. e. Parietal pain corresponds to dermatomes T6 and L1. , B, D, E Parietal pain arises from the parietal peritoneum and is more localized and intense than visceral pain. Nerve fibers from the parietal peritoneum travel with peripheral nerves to the spinal cord, and the sensation of pain corresponds to skin dermatomes T6 and L1. PTS: 1 REF: Page 1426 38. Which statements are true regarding chronic gastritis? (Select all that apply.) a. Chronic gastritis tends to occur in older adults. b. It causes thinning and degeneration of the stomach wall. c. Chronic gastritis results in chrNonUiRcSiInNfGlaTmBm.CaOtMion and mucosal atrophy. d. Mucosal atrophy is a common outcome of chronic gastritis. e. Epithelial metaplasia is often observed with chronic gastritis. , C, D, E Chronic gastritis tends to occur in older adults and causes chronic inflammation, mucosal atrophy, and epithelial metaplasia. Neither thinning nor degeneration of the stomach wall is associated with chronic gastritis. PTS: 1 REF: Page 1434 39. Which hormones are natural appetite suppressants? (Select all that apply.) a. Insulin b. Cortisol c. Galanin d. Calcitonin e. Serotonin , D, E Insulin, calcitonin, and serotonin are natural appetite suppressants, whereas cortisol and galanin are natural appetite stimulants. PTS: 1 REF: Page 1448 | Box 41-4 40. Which are the early (prodromal) clinical manifestations of hepatitis? (Select all that apply.) a. Fatigue b. Vomiting c. Itching d. Splenomegaly e. Hyperalgia , B, E The prodromal (preicteric) phase of hepatitis begins approximately 2 weeks after exposure and ends with the appearance of jaundice. Fatigue, anorexia, malaise, nausea, vomiting, headache, hyperalgia, cough, and low-grade fever are prodromal symptoms that precede the onset of jaundice. Itching and splenomegaly are not associated with the prodromal phase of hepatitis. PTS: 1 REF: Page 1459 41. Which clinical manifestations are consistent with cancer of the cecum and ascending colon? (Select all that apply.) a. Mahogany-colored blood mixed with stool b. Anemia c. Pain d. Constipation e. Palpable mass in the lower right quadrant , B, C, E Clinical manifestations consistent with cancer of the cecum and ascending colon include pain, a palpable mass in the lowerNrUigRhStINquGaTdBr.aCnOt,Manemia, and dark red or mahogany-colored blood mixed with the stool. Constipation is not associated with this diagnosis. PTS: 1 REF: Page 1471 MATCHING Match the descriptions with the corresponding terms. A. Ulcerative colitis B. Crohn disease 42. Alterations in immunoglobulin G (IgA) production have been found in individuals with this disorder. 43. Inflammation develops in crypts of Lieberkühn in the large intestine. 42. ANS: MSC: B PTS: 1 REF: Page 1442 In Crohn disease, elevations in IgG are associated with the severity of the disease. 43. ANS: MSC: A PTS: 1 REF: Page 1441 Inflammation begins at the base of the crypts of Lieberkühn in the large intestine, primarily the left colon, with infiltration and release of inflammatory cytokines from neutrophils, lymphocytes, plasma cells, macrophages, eosinophils, and mast cells. Chapter 43: Alterations of Digestive Function in Children MULTIPLE CHOICE 1. Incomplete fusion of the nasomedial and intermaxillary process during the fourth week of embryonic development causes which condition in an infant? a. Cleft palate c. Cleft lip b. Sinus dysfunction d. Esophageal malformation Of the available options, only a cleft lip is caused by the incomplete fusion of the nasomedial and intermaxillary process during the fourth week of embryonic development. PTS: 1 REF: Page 1486 2. Increased gastrin secretion by the mother in the last trimester of pregnancy may cause which condition in the infant? a. Pyloric stenosis c. Esophageal atresia b. Meconium ileus d. Galactosemia The cause is unknown but increased gastrin secretion by the mother in the last trimester of pregnancy increases the likelihood of pyloric stenosis in the infant. The overproduction of gastric secretions in the infant may be caused by stress-related factors in the mother. This statement is not true of the other options. PTS: 1 REF: Pages 1N4U88R-S1I4N8G9TB.COM 3. At 2 or 3 weeks of age, an infant who has been well fed and has gained weight begins to vomit for no apparent reason. The vomiting gradually becomes more forceful. These symptoms may be indicative of which disorder? a. Esophageal atresia c. Pyloric stenosis b. Congenital aganglionic megacolon d. Galactosemia Of the options available, only the clinical manifestations of pyloric stenosis—an infant who has been well fed and has gained weight begins to vomit without an apparent reason—can appear between 2 and 3 weeks after birth. The vomiting gradually becomes more forceful. PTS: 1 REF: Page 1489 4. Which term is used to identify a condition in which the developing colon remains in the upper right quadrant instead of moving to its normal location? a. Intestinal malrotation c. Duodenal obstruction b. Ileocecal displacement d. Pyloric stenosis Intestinal malrotation is the only term used to identify a condition in which rotation does not occur and the colon remains in the upper right quadrant, where an abnormal membrane may press on and obstruct the duodenum. PTS: 1 REF: Page 1489 5. Which term is used to identify an intestinal obstruction caused by meconium formed in utero that is abnormally sticky and adheres firmly to the mucosa of the small intestine? a. Meconium cecum c. Meconium obstruction b. Meconium ileus d. Meconium vivax Meconium ileus is the only term used to identify an intestinal obstruction caused by meconium formed in utero that is abnormally sticky and adheres firmly to the mucosa of the small intestine, resisting passage beyond the terminal ileum. The cause is usually a lack of digestive enzymes during fetal life. PTS: 1 REF: Page 1490 6. With which medical diagnosis is meconium ileus often associated? a. Muscular dystrophy c. Cystic fibrosis b. Cerebral palsy d. Congenital aganglionic megacolon The detection of albumin in meconium has been used as a screening test for cystic fibrosis. This condition is not associated with any of the other options. PTS: 1 REF: Page 1490 7. Congenital aganglionic megacolon (Hirschsprung disease) involves inadequate motility of the colon caused by neural malforNmUaRtiSoInNGofTBw.hCiOcMh nervous system? a. Central c. Sympathetic b. Parasympathetic d. Somatic A malformation related only to the parasympathetic nervous system causes congenital aganglionic megacolon. PTS: 1 REF: Page 1491 8. Which term is used to describe an intestinal obstruction caused by the invagination of the ileum into the cecum and part of the ascending colon by collapsing through the ileocecal valve? a. Congenital aganglionic megacolon c. Intussusception b. Malrotation d. Volvulus Intussusception is the telescoping or invagination of one portion of the intestine into another section of intestine. Usually, the ileum invaginates the cecum and part of the ascending colon by collapsing through the ileocecal valve. The other terms are not used to describe this event. PTS: 1 REF: Page 1492 9. An infant suddenly develops abdominal pain, becomes irritable (colicky), and draws up the knees. Vomiting occurs soon afterward. The mother reports that the infant passed a normal stool, followed by one that looked like currant jelly. Based on these data, which disorder does the nurse suspect? a. Congenital aganglionic megacolon c. Malrotation b. Intussusception d. Volvulus Based on these data, the nurse should suspect intussusception. A single normal stool may be passed, evacuating the colon distal to the apex of the intussusception. After passing a normal stool, 60% of infants will pass “currant jelly” stools, which appear dark and gelatinous because of their blood and mucus content. Intussusception is the only option that describes the symptoms listed. PTS: 1 REF: Page 1493 10. Cystic fibrosis is characterized by which symptom? a. Excessive mucus production c. Low sodium content in perspiration b. Elevated blood glucose levels d. Abnormally thin exocrine secretions Excessive mucus production characterizes cystic fibrosis. However, the pathophysiologic triad that is the hallmark of cystic fibrosis includes (1) pancreatic enzyme deficiency, which causes maldigestion; (2) overproduction of mucus in the respiratory tract and an inability to clear secretions, which cause progressive chronic obstructive pulmonary disease; and (3) abnormally elevated sodium and chloride concentrations in sweat. Exocrine secretions tend to be abnormally thick and precipitate in the glandular ducts, obstructing flow. An elevated blooNdURglSuIcNoGsTeBl.eCvOeMl is not associated with this disorder. PTS: 1 REF: Page 1494 11. Which medication compensates for the deficiency that occurs as a result of cystic fibrosis? a. Salt tablets c. Antihypertensives b. Pancreatic enzymes d. Antibiotics Pancreatic replacement enzymes are administered before or with meals, and high-calorie, high-protein diets with frequent snacks and vitamin supplements are used to treat the deficiency. These statements are not true of the other options. PTS: 1 REF: Page 1494 12. What causes a person with cystic fibrosis to experience an exocrine pancreatic insufficiency? a. Pancreatic ducts are obstructed with mucus. b. Impaired blood supply to the pancreas causes ischemia. c. A genetically impaired pancreas is unable to produce digestive enzymes. d. The pancreas has a volvulus at the ampulla of Vater. Approximately 85% of individuals with cystic fibrosis experience pancreatic insufficiency. Obstruction of the pancreatic ducts with thick mucus blocks the flow of pancreatic enzymes and causes degenerative and fibrotic changes in the pancreas. This selection is the only option that accurately describes why an exocrine pancreatic insufficiency is observed in individuals diagnosed with cystic fibrosis. PTS: 1 REF: Page 1494 13. What is the cause of faulty digestion of fats in those diagnosed with cystic fibrosis? a. Bile ducts obstructed with mucus, prohibiting the release of bile b. Failure to metabolize fat-soluble vitamins c. Deficiency of pancreatic enzymes d. Fat malabsorption that now occurs in the jejunum ANS: C Severe problems with maldigestion of proteins, carbohydrates, and fats occur because of the insufficient secretion of pancreatic enzymes. This selection is the only option that accurately describes why fatty stools are observed in individuals diagnosed with cystic fibrosis. PTS: 1 REF: Page 1494 14. Which disorder is characterized by damage to the mucosa of the duodenum and jejunum and impaired secretion of secretin, cholecystokinin, and pancreatic enzymes? a. Wilson disease c. Gluten-sensitive enteropathy b. Cystic fibrosis d. Galactosemia NURSINGTB.COM Gluten-sensitive enteropathy is characterized by damage to the mucosa of the duodenum and jejunum and has secondary effects that exacerbate malabsorption. The secretion of intestinal hormones, such as secretin and cholecystokinin, may be diminished. Because these chemical messengers are scarce, secretion of pancreatic enzymes and expulsion of bile from the gallbladder decrease. These statements are not true of the other options. PTS: 1 REF: Page 1495 15. What factor associated with gluten-sensitive enteropathy (celiac sprue) causes an infant to bruise and bleed easily? a. Vitamin K deficiency from fat malabsorption b. Bone marrow function depression c. Iron, folate, and B12 deficiency anemias d. Prescribed daily warfarin (Coumadin) Deficiencies of fat-soluble vitamins (such as vitamin K) are common in children with gluten-sensitive enteropathy. Vitamin K malabsorption leads to hypoprothrombinemia, causing the child to bruise and bleed easily. This selection is the only option that accurately describes the mechanism that causes bruising and bleeding in children diagnosed with celiac sprue. PTS: 1 REF: Page 1497 16. What distinguishes kwashiorkor from marasmus? a. All nutrients, proteins, fats, and carbohydrates are reduced in kwashiorkor. b. Physical growth of children is stunted in kwashiorkor but not in marasmus. c. Muscle wasting, diarrhea, low hemoglobin, and infection characterize kwashiorkor. d. Subcutaneous fat, hepatomegaly, and fatty liver are present in kwashiorkor. The presence of subcutaneous fat, hepatomegaly, and fatty liver distinguishes kwashiorkor from marasmus. These manifestations are missing in marasmus because caloric intake is not sufficient to support fat synthesis and storage. None of the other options accurately describes the differences among these conditions. PTS: 1 REF: Page 1498 17. Why is prolonged diarrhea more severe in children than it is in adults? a. Less water is absorbed from the colon in children. b. Fluid reserves are smaller in children. c. Children have a higher fluid volume intake. d. Children have diarrhea more often than adults. Infants have low fluid reserves and relatively rapid peristalsis and metabolism. Therefore the danger of dehydration is great. This selection is the only option that correctly identifies the reason prolonged diarrhea is more severe in children. PTS: 1 REF: Page 1500 NURSINGTB.COM 18. In an infant who is 5 weeks old, an increase in bilirubin production and persistent jaundice support which diagnosis? a. Pathologic hyperbilirubinemia c. Hepatitis A b. Physiologic jaundice d. Infantile cirrhosis Physiologic jaundice develops during the second or third day after birth and usually subsides in 1 to 2 weeks in full-term infants and in 2 to 4 weeks in premature infants. After this development, increased bilirubin values and persistent jaundice indicate pathologic hyperbilirubinemia. This selection is the only option that accurately identifies the diagnosis associated with these symptoms and timeline. PTS: 1 REF: Pages 1500-1501 19. Which type of diarrhea results from lactose intolerance? a. Secretory c. Osmotic b. Motility d. Small volume The malabsorption of lactose results in osmotic diarrhea, in which fluids move by osmosis from the vascular compartment into the intestinal lumen. Of the available options, this selection is the only type of diarrhea that results from lactose intolerance. PTS: 1 REF: Page 1500 20. Physiologic jaundice in a newborn is caused by: a. Reabsorption of bilirubin in the small intestine b. Impaired hepatic uptake and excretion of bilirubin c. Increased bilirubin production d. Mild conjugated (indirect-reacting) hyperbilirubinemia Of the available options, physiologic jaundice in a newborn is caused by mild unconjugated (indirect-reacting) hyperbilirubinemia. PTS: 1 REF: Page 1500 21. In children, the risk factors for hepatitis B virus (HBV) are primarily associated with: a. Living in urban communities b. Mothers who are hepatitis C carriers c. Transfusion therapy for hemophilia d. Those of Hispanic ethnic background Risk factors for HBV infection include infants of mothers who are carriers of chronic hepatitis B surface antigen (HBsAg), hemophiliacs who receive frequent blood transfusions, children who abuse parenteral drugs, and children who live in residences for those who are mentally delayed. HBV is endemic in China and other parts of Asia where most infections occur in infants and children as a result of maternal-neonatal transmission. PTS: 1 REF: Page 1502 NURSINGTB.COM 22. Cirrhosis causes intrahepatic portal hypertension in children as a result of which mechanism? a. Fibrosis that increases the resistance to blood flow within the portal system b. Increased pressure from the twisting of the common bile ducts c. Development of collateral circulation within the portal system d. Shunting of fluid to the spleen or abdomen The two basic causes of portal hypertension in children are (1) increased resistance to blood flow within the portal system and (2) increased volume of portal blood flow. This selection is the only option that correctly identifies the cause of intrahepatic portal hypertension in children. PTS: 1 REF: Page 1503 23. What is the most common clinical sign of portal hypertension in children? a. Right heart failure c. Splenomegaly b. Pulmonary edema d. Diarrhea Splenomegaly is the most common sign of portal hypertension in children. PTS: 1 REF: Page 1503 MULTIPLE RESPONSE 24. What factors can contribute to the development of a cleft lip and a cleft palate? (Select all that apply.) a. Maternal deficiency of B vitamins b. Exposure to heavy metals during the second trimester of pregnancy c. Maternal use of tobacco d. Maternal diabetes mellitus e. Genetic mutation of the transforming growth factor , C, D In most cases, cleft lip and cleft palate are caused by multiple gene and environmental interactions, including maternal deficiency of B vitamins (B6, folic acid, and B12), maternal tobacco and alcohol use, maternal diabetes mellitus, and genetic variations of several biomolecules including transforming growth factor, interferon regulatory factor-6, fibroblast growth factor, and other growth factors. Exposure to heavy metals during the second trimester of pregnancy is not a known trigger for such development. PTS: 1 REF: Page 1486 25. Which situations have been associated with possible causes of the failure to thrive (FTT) in infants? (Select all that apply.) a. Gastroesophageal reflux b. Pyloric stenosis c. Intestinal parasites d. Adoption at birth e. Psychosocial isolation , B, C, E NURSINGTB.COM FTT is a disorder having organic (e.g., gastrointestinal and endocrine disorders) and nonorganic (e.g., psychosocial) deprivation causes. Organic FTT has a pathophysiologic cause, such as gastroesophageal reflux, pyloric stenosis, gastroenteritis, malabsorption syndromes, infection by intestinal parasites, congenital anomalies, very low birth weight, or chronic diseases of major body systems. Nonorganic FTT occurs in the absence of any gastrointestinal, endocrine, or other chronic diseases. It is usually associated with psychosocial deprivation, although behavior problems may contribute to its occurrence in the absence of maternal pathologic findings. Adoption, in of itself, is not a cause. PTS: 1 REF: Page 1498 26. Which statements regarding Wilson disease in children are true? (Select all that apply.) a. Wilson disease is a rare autosomal recessive defect. b. Wilson disease affects copper metabolism. c. A lack of necessary copper is a result of Wilson disease. d. The liver is often affected in Wilson disease. e. Corneal damage can be a result of Wilson disease. , C, D, E Wilson disease (hepatolenticular degeneration) is an autosomal recessive defect of copper metabolism that causes toxic amounts of copper to accumulate in the liver, brain, kidneys, and corneas. PTS: 1 REF: Page 1504 27. What are the classic symptoms associated with hepatitis A in children? (Select all that apply.) a. Nausea b. Vomiting c. Diarrhea d. Jaundice e. Muscle pain , B, C Clinical manifestations associated with hepatitis A may include nausea, vomiting, and diarrhea. Neither jaundice nor muscle pain is associated with hepatitis A in children. PTS: 1 REF: Page 1502 28. Cystic fibrosis is directly responsible for complications to which structures? (Select all that apply.) a. Muscles b. Kidneys c. Lymph nodes d. Cervix e. Liver , E Of the options available, only cervical inflammation and portal hypertension (liver) are complications directly related to cNyUstRicSIfNibGrToBsi.sC.OM PTS: 1 REF: Page 1495 | Table 42-1 29. Which foods should be eliminated from the diet for children who have gluten-sensitive enteropathy (celiac sprue)? (Select all that apply.) a. Citrus fruits b. Starchy vegetables c. Cereal grains d. Red meat e. Dairy , E Treatment for celiac sprue consists of the immediate and permanent institution of a diet free of cereal grains (e.g., wheat, rye, barley, oats, malt). Lactose intolerance is presumed because of damage to the villi; therefore lactose (milk sugar) is excluded from the diet. The remaining options are not contraindicated on a celiac sprue–related diet. PTS: 1 REF: Page 1497 If needing more Test Banks, just let me know: [email protected] MATCHING Match the terms with the corresponding characteristics. A. Gluten sensitivity B. Periduodenal band C. Congenital aganglionic megacolon D. Protein energy malnutrition E. Lack of digestive enzymes during fetal life 30. Malrotation 31. Hirschsprung disease 32. Marasmus and kwashiorkor 33. Celiac sprue 34. Meconium ileus 30. ANS: B PTS: 1 REF: Page 1489 MSC: Intestinal malrotation is a condition in which rotation does not occur and the colon remains in the upper right quadrant, where an abnormal membrane may press and obstruct the duodenum. The obstructing band over the duodenum, called a periduodenal band, is one of the most significant findings in malrotation. 31. ANS: C PTS: 1 REF: Page 1491 MSC: Congenital aganglionic megacolon (Hirschsprung disease) is a functional obstruction of the colon caused by the absence of the enteric ganglia along a variable length of the colon with inadequate motility. 32. ANS: D PTS: 1 REF: Page 1497 MSC: Kwashiorkor and marasmus are the two most common types of malnutrition in children. These disorders are collectively known as protein energy malnutrition (PEM). 33. ANS: A PTS: 1 NURSINRGETFB:.CPOaMge 1494 MSC: Gluten-sensitive enteropathy, formerly called celiac sprue or celiac disease, is an autoimmune disease that damages the small intestinal villous epithelium when ingestion of gluten (gliadin), the protein component of cereal grains, occurs. 34. ANS: E PTS: 1 REF: Page 1490 MSC: Meconium ileus is intestinal obstruction caused by meconium formed in utero that is abnormally sticky and adheres firmly to the mucosa of the small intestine, resisting passage beyond the terminal ileum. The cause is usually a lack of digestive enzymes during fetal life. Chapter 44: Structure and Function of the Musculoskeletal System MULTIPLE CHOICE 1. Which bone cells produce osteocalcin when stimulated by 1,25-dihydroxyvitamin D and synthesize osteoid? a. Osteoclasts c. Fibrocytes b. Osteocytes d. Osteoblasts Osteoblasts are cells derived from mesenchymal stem cells and produce several substances, including osteocalcin, transforming growth factor–beta (TGF-) (a growth inhibitor for many cells), macrophage colony–stimulating factor, receptor activator of nuclear factor kappa-B ligand, osteoprotegerin (OPG), and bone matrix when stimulated by 1,25-dihydroxyvitamin D. This statement is not true of the other options. PTS: 1 REF: Page 1514 2. What happens to the original bone during the second phase of bone remodeling? a. The original bone is replaced. c. The original bone is resorbed. b. It hardens. d. It is synthesized. The distribution of these apoptotic osteocytes provides osteoclasts with information about where to begin resorbing damaged bone. In the second phase of remodeling (resorption), the osteoclasts form a cutting cone that gradually resorbs bone, leaving behind an elongated cavity termed a resorptiNoUnRcSaIvNiGtyT.BT.ChiOsMselection is the only option that accurately describes what happens when bone is resorbed. PTS: 1 REF: Pages 1519-1520 3. Which cells function to maintain bone matrix? a. Osteoclasts c. Osteoblasts b. Osteocytes d. Osteophytes Osteocytes help synthesize and replace needed elements of the matrix by signaling osteoclasts and osteoblasts to resorb and form new bone. This selection is the only option that performs that function. PTS: 1 REF: Pages 1514-1515 4. Which bone cells are large and multinucleated and contain lysosomes filled with hydrolytic enzymes? a. Osteoblasts c. Osteocytes b. Osteoclasts d. Fibrocytes Osteoclasts are the major resorptive cells of bone. They are large multinucleated cells with a short life span and contain lysosomes (digestive vacuoles) filled with hydrolytic enzymes. This selection is the only option that is described in this manner. PTS: 1 REF: Page 1515 5. Which bone cell secretes hydrochloric acid to help dissolve bone minerals and collagenase, thus aiding in the digestion of collagen? a. Osteocytes c. Osteoclasts b. Osteoblasts d. Osteophytes Only osteoclasts bind to the bone surface of cell attachment proteins called integrins. They bring about resorption of bone by secreting hydrochloric acid and cathepsin K (a protease enzyme) that help dissolve bone minerals and collagenase, which aids in digesting collagen, along with the action of cytokines. PTS: 1 REF: Page 1515 6. Which glucoprotein is believed to inhibit calcium phosphate precipitation and play a part in bone resorption by recruiting osteoclasts? a. Osteocalcin c. Laminin b. Osteonectin d. Osteopontin The roles of osteocalcin may be to inhibit calcium phosphate precipitation and play a part in bone resorption by recruiting osteoclasts. This statement is not true of any other option. PTS: 1 REF: Page 1516 7. Which glucoprotein is thought to NtrUanRsSpIoNrGt TeBss.CenOtMial elements such as hormones, ions, and other metabolites to and from the bone cells? a. Osteocalcin c. Laminin b. Osteonectin d. Bone albumin Researchers believe bone albumin transports essential elements such as hormones, ions, and other metabolites to and from the bone cells and maintain the osmotic pressure of bone fluid (fluid surrounding mineral crystals and osteoblasts). This statement is not true of any other option. PTS: 1 REF: Page 1516 8. How is the work function of a muscle usually calculated? a. Muscle type c. Foot pounds b. Calculating force distance d. Kilograms The ultimate function of muscle is to accomplish work. Although expressed in such measures as foot-pounds or kilogram-meters, work refers to the amount of energy liberated or the amount of force exerted over a distance (work force distance). Muscle type is not relevant. PTS: 1 REF: Page 1533 9. What is the basic structural unit in compact bone? a. Small channels called canaliculi c. Tiny spaces within the lacunae b. Osteocytes within the lacunae d. Haversian system The basic structural unit in compact bone is the haversian system (see Figure 43-4). This selection is the only option that accurately identifies the basic structure of compact bone. PTS: 1 REF: Page 1517 10. Which part of an injured joint becomes insensitive to pain and regenerates slowly and minimally? a. Synovium c. Bursa b. Articular cartilage d. Tendon Articular cartilage has no blood vessels, lymph vessels, or nerves. Therefore it is insensitive to pain and regenerates slowly and minimally after injury. These statements are not true of the other options. PTS: 1 REF: Page 1525 11. The outer layer of the periosteum contains blood vessels and nerves that penetrate the inner structures of the bone by way of which structure? a. Volkmann canals c. Sharpey canals b. Canaliculi d. Trabeculae NURSINGTB.COM All bones are covered with a double-layered connective tissue called the periosteum. The outer layer of the periosteum contains blood vessels and nerves, some of which penetrate to the inner structures of the bone only through channels called Volkmann canals (see Figure 43-4). PTS: 1 REF: Page 1517 12. What is the function of Sharpey fibers? a. To anchor the outer layer of the periosteum to the inner layer b. To contain blood vessels and nerves on the outer layer of the periosteum c. To help attach tendons and ligaments to the periosteum d. To attach muscles to the periosteum Collagenous fibers (Sharpey fibers) that penetrate the bone anchor the inner layer of the periosteum to the bone. Sharpey fibers help hold or attach tendons and ligaments, not muscle, but to the periosteum of bones. PTS: 1 REF: Page 1517 13. After puberty, the epiphyseal plate calcifies, and the epiphysis merges with the . a. Epiphyseal line c. Metaphysis b. Epiphyseal plate d. Articular cartilage After puberty, the epiphyseal plate calcifies and the epiphysis merges only with the metaphysis. PTS: 1 REF: Page 1518 14. The stage of healing in the bone that involves procallus formation entails which process? a. Formation of a hematoma that allows the development of a fibrin network b. Production of granulation tissue by fibroblasts, capillary buds, and osteoblasts c. Development of a primitive bone matrix termed woven bone d. Remodeling of the periosteal and endosteal bone surfaces Fibroblasts, capillary buds, and osteoblasts move into the wound to produce granulation tissue called a procallus. None of the other options are associated with this process. PTS: 1 REF: Page 1520 15. Which term describes a freely movable joint? a. Synarthrosis c. Biarthrosis b. Amphiarthrosis d. Diarthrosis Based on movement, a joint is classified as a synarthrosis (immovable joint), an amphiarthrosis (slightly movable joint), or a diarthrosis (freely movable joint). Biarthrosis is not a term used to describe a freely movable joint. PTS: 1 REF: Page 15N2U0RSINGTB.COM 16. Which type of joint holds teeth in the maxilla or mandible? a. Amphiarthrosis c. Synarthrosis b. Diarthrosis d. Gomphosis A gomphosis is a special type of fibrous joint in which a conical projection fits into a complementary socket and is held in place by a ligament. Gomphosis is the only term used to identify the joint that holds teeth in the maxilla or mandible. PTS: 1 REF: Page 1520 17. The hyaline cartilage joints between the ribs and sternum are examples of which type of joint? a. Synchondrosis c. Gomphosis b. Symphysis d. Syndesmosis A synchondrosis is the only type of joint in which hyaline cartilage, rather than fibrocartilage, connects the two bones. The joints between the ribs and the sternum are synchondroses and are not examples of any of the other types. PTS: 1 REF: Page 1520 18. The joint that contains a synovial membrane that lines the inner joint capsule is an example of which type of joint? a. Amphiarthrosis c. Synarthrosis b. Diarthrosis d. Biarthrosis The joint that contains a synovial membrane that lines the inner joint capsule is a diarthrosis. A synovial joint consists of the following parts: (1) fibrous joint capsule (articular capsule), (2) synovial membrane that lines the inner surface of the joint capsule, (3) joint cavity (synovial cavity or space formed by the capsule), (4) synovial fluid, which fills the joint cavity and lubricates the joint surface, and (5) articular cartilage, which covers and pads the articulating bony surfaces. PTS: 1 REF: Page 1522 19. What is the function of the synovial membrane’s type A cells within the intima? a. To release mast cells, initiating the inflammatory process after joint injury b. To ingest and remove bacteria and debris by phagocytosis in the joint cavity c. To secrete hyaluronate, a binding agent that gives synovial fluid its viscous quality d. To store fat cells and glycogen, providing adenosine triphosphate for joint activity The intima contains two types of synovial cells: A and B. Type A synovial cells ingest and remove bacteria and particles of debris by phagocytosis in the joint cavity. None of the remaining options accurately describes the function of the synovial membrane’s type A cells. PTS: 1 REF: Page 15N2U2RSINGTB.COM 20. Which statement does not present accurate information concerning synovial fluid? a. Synovial fluid contains protein polysaccharides to repair the synovial membrane after injury. b. It lubricates the joint surfaces. c. Synovial fluid nourishes the pad of the articular cartilage. d. It contains leukocytes to phagocytize joint debris and microorganisms. Synovial fluid lubricates the joint surfaces, nourishes the pad of the articular cartilage that covers the ends of the bones, and contains free-floating synovial cells and various leukocytes that phagocytose joint debris and microorganisms. The other options provide accurate information about synovial fluid. PTS: 1 REF: Page 1522 21. What anchors articular cartilage to the underlying bone? a. Sharpey fibers c. Glycoproteins b. Collagen fibers d. Elastin fibers Collagen fibers are important components of the cartilage matrix because they anchor the cartilage securely to underlying bone. This statement is not true of the other options. PTS: 1 REF: Pages 1524-1525 22. What controls the movement of synovial fluid through cartilage? a. Cartiloregulins c. Proteoglycans b. Hyaluronate d. Chondroitin Only proteoglycans give articular cartilage its stiff quality and regulate the movement of synovial fluid through the cartilage. PTS: 1 REF: Page 1525 23. Which statement is false about muscles? a. Muscle comprises 50% of an adult’s body weight and 40% of a child’s body weight. b. Muscle is 75% water, 20% protein, and 5% organic and inorganic compounds. c. Muscle contains 32% of all protein stores for energy and metabolism. d. Muscles are encased in fascia. Muscle constitutes 40% of an adult’s body weight and 50% of a child’s body weight. The other options are true statements regarding muscles. PTS: 1 REF: Pages 1526-1527 24. Which characteristic is true of type II (white fast-motor) muscle fibers? a. Slow contraction speed c. Profuse capillary supply b. Fast conduction velocities NURSINGTdB..COOMxidative metabolism Type II fibers, also called white fast-motor fibers, are innervated by relatively large type II alpha motor neurons with fast conduction velocities. This selection is the only correct option provided. PTS: 1 REF: Page 1529 25. As the innervation ratio of a particular organ increases, what other property also increases? a. Control c. Coordination b. Movement d. Endurance The greater the innervation ratio of a particular organ, the greater is its endurance. Low-innervation ratios promote control and coordination, whereas high ratios promote strength and endurance. An increase in the innervations ratio does not result in an increase in movement. PTS: 1 REF: Page 1528 26. Which statement describes a neuroregulin? a. Chemical mediator that initiates signals from the anterior horn cell of the spinal card to the axon of motor nerve branches of groups of muscle fibers b. Neurotransmitter that provides a means of reporting changes in length, tension, velocity, and tone in muscles c. Proteoglycan secreted by neurons, which increases acetylcholine receptors d. Mechanoreceptor that lies parallel to muscle fibers and responds to muscle stretching Motor and sensory neurons secrete a proteoglycan called neuroregulin that increases acetylcholine receptors and helps in the formation of muscle spindle fibers. This selection is the only option that accurately describes a neuroregulin. PTS: 1 REF: Pages 1528-1529 27. Which four-step process correctly describes muscle contraction? a. Coupling, contraction, relaxation, excitation b. Contraction, relaxation, excitation, coupling c. Relaxation, excitation, coupling, contraction d. Excitation, coupling, contraction, relaxation Muscle contraction is a four-step process: excitation, coupling, contraction, and relaxation. PTS: 1 REF: Page 1533 28. Which type of ion directly controls the contraction of muscles? a. Sodium c. Calcium b. Potassium d. Magnesium NURSINGTB.COM Contraction begins as the calcium ions combine with troponin, a reaction that overcomes the inhibitory function of the troponin-tropomyosin system. This selection is the only option that has such a direct association with muscle contraction. PTS: 1 REF: Page 1533 29. In which type of contraction does the muscle maintain a constant tension as it moves? a. Isotonic c. Hypertonic b. Isometric d. Hypotonic Only during an isotonic contraction does the muscle maintain a constant tension as it moves. PTS: 1 REF: Page 1535 30. Which term is used to identify a functional muscle contraction in which the muscle contracts but the limb does not move? a. Isotonic c. Eccentric b. Isometric d. Concentric Only during an isometric contraction (static or holding contraction) does the muscle maintain a constant length as tension is increased. Isometric contraction occurs, for example, when the arm or leg is pushed against an immovable object. The muscle contracts, but the limb does not move. PTS: 1 REF: Page 1535 31. Which statement is false about aging and the musculoskeletal system? a. Haversian system erodes, the canals nearest the marrow cavity widened, and the endosteal cortex converts to spongy bone. b. The remodeling cycle increases because of a decreased ability of the basic multicellular units to resorb and deposit bone. c. Cartilaginous rigidity increases because of decreasing water content and decreasing concentrations of glycosaminoglycans. d. Muscle ribonucleic acid (RNA) synthesis declines, although the regenerative function of muscle tissue is reportedly normal in older adults. Aging does not typically have an effect on the haversian system as described. The remaining options are accurate statements regarding the effects of aging. PTS: 1 REF: Page 1536 32. Which component is found in synovial fluid? a. Protein polysaccharides c. Leukocytes b. Water d. Chondrocytes NURSINGTB.COM Synovial fluid lubricates the joint surfaces, nourishes the pad of the articular cartilage that covers the ends of the bones, and contains only free-floating synovial cells and various leukocytes that phagocytose joint debris and microorganisms. None of the remaining options are found in synovial fluid. PTS: 1 REF: Page 1522 33. What term is used to identify an interlacing bundle of dense, white fibrous tissue that is richly supplied with nerves, blood vessels, and lymphatic vessels? a. Procallus c. Hematoma b. Joint capsule d. Elastin fibers The joint capsule is made up of parallel, interlacing bundles of dense, white fibrous tissue. It is richly supplied with nerves, blood vessels, and lymphatic vessels. None of the other options are associated with this structure. PTS: 1 REF: Page 1522 MULTIPLE RESPONSE 34. In adults, hematopoiesis takes place in which bone marrow cavities? (Select all that apply.) a. Skull b. Shoulders c. Sternum d. Long bones e. Pelvis , B, C, E The marrow cavities within certain bones serve as sites of blood cell formation. In adults, blood cells exclusively originate in the marrow cavities of only the skull, vertebrae, ribs, sternum, shoulders, and pelvis. PTS: 1 REF: Page 1510 35. Which statements are true regarding osteocytes? (Select all that apply.) a. An osteocyte is a transformed osteoblast. b. An osteocyte obtains nutrients from capillaries in the canaliculi. c. The functioning of an osteocyte is well understood. d. Osteocytes signal osteoclasts and osteoblasts to form new bone. e. An osteocyte helps maintain levels of calcium and phosphorus in blood plasma. , B, D, E An osteocyte is a transformed osteoblast. Osteocytes communicate with each other and help concentrate nutrients in the matrix. They obtain nutrients from capillaries in the canaliculi, which contain nutrient-rich fluids and also help synthesize and replace needed elements of the matrix by signaling osteoclasts and osteoblasts to resorb and form new bone. Through exchanges among these cells, hormone catalysts, minerals, and optimal levels of calcium, phosphorus, and other minerals are maintained in blood plasma. NURSINGTB.COM PTS: 1 REF: Pages 1514-1515 36. Which minerals are stored in bones? (Select all that apply.) a. Carbonate b. Phosphate c. Selenium d. Magnesium e. Calcium , B, D, E Bones have a crucial role in mineral homeostasis and in storing and releasing minerals (e.g., calcium, phosphate, carbonate, magnesium) that are essential for the proper working of many delicate cellular mechanisms. Selenium is not stored in the bones. PTS: 1 REF: Page 1510 37. Which factors influence the rate of protein synthesis of skeletal muscles? (Select all that apply.) a. Insulin b. Cortisol c. Parathyroid hormone d. Growth hormone e. Amino acid substrates , E The rate of protein synthesis is related to insulin levels amino acid substrates and to overall nutritional status. PTS: 1 REF: Page 1533 MATCHING Match the stages of wound healing of a bone with the description of each. Stages may be used more than once. A. Callus replacement B. Hematoma formation C. Remodeling D. Procallus formation E. Callus formation 38. Fibroblasts, capillary buds, and osteoblasts move into the wound to produce granulation tissue. 39. Periosteal and endosteal surfaces of the bone are formed to the size and shape of the bone before an injury. 40. Osteoblasts form membranous or woven bone. Enzymes increase the phosphate content and permit the phosphate to join with calcium to be deposited. 41. Fibrin and platelets form a meshwork within the initial framework for healing. 42. Osteoblasts continue to restore callus with lamellar bone or trabecular bone. he wound to produce granulation MSC: Remodeling occurs as the periosteal and endosteal surfaces of the bone are remodeled to the size and shape of the bone before injury. 40. ANS: E PTS: 1 REF: Page 1520 MSC: Callus formation occurs as osteoblasts in the procallus form membranous or woven bone (callus). Enzymes increase the phosphate content and permit the phosphate to join with calcium to be deposited as mineral to harden the callus. 41. ANS: B PTS: 1 REF: Page 1520 MSC: Hematoma formation occurs if vessels have been damaged, causing hemorrhage. Fibrin and platelets within the hematoma form a meshwork that is the initial framework for healing with the help of hematopoietic growth factors such as platelet-derived growth factor and transforming growth factor-beta (TGF-b). 42. ANS: A PTS: 1 REF: Page 1520 MSC: Callus replacement occurs as osteoblasts continue to replace the callus with lamellar bone or trabecular bone. Chapter 45: Alterations of Musculoskeletal Function MULTIPLE CHOICE 1. What type of fracture occurs at a site of a preexisting bone abnormality and is a result of a force that would not normally cause a fracture? a. Idiopathic c. Pathologic b. Incomplete d. Greenstick Only a pathologic fracture is a break at the site of a preexisting abnormality, usually by force that would not fracture a normal bone. PTS: 1 REF: Page 1541 2. Which type of fracture usually occurs in an individual who engages in a new activity that is strenuous and repetitive? a. Stress c. Insufficiency b. Greenstick d. Pathologic Only a stress fracture occurs in normal or abnormal bone that is subjected to repeated stress, such as repetitive and strenuous activities that occur during athletics. PTS: 1 REF: Page 1541 3. Which term is used to identify theNtUemRSpIoNrGarTyBd.CisOpMlacement of two bones causing the bone surfaces to partially lose contact? a. Dislocation c. Malunion b. Subluxation d. Nonunion Dislocation is the temporary displacement of a bone from its normal position in a joint. If the contact between the two surfaces is only partially lost, then the injury is referred to as a subluxation. This selection is the only option that identifies the temporary displacement of two bones, causing the bone surfaces to partially lose contact. PTS: 1 REF: Page 1544 4. Improper reduction or immobilization of a fractured femur can result in which outcome after cast removal? a. The muscles around the fracture site are weak. b. The fracture requires 6 to 8 weeks of physical therapy. c. The skin under the cast is dry and flaky. d. The bone is not straight. Improper reduction or immobilization of a fractured bone may result in nonunion, delayed union, or malunion. Malunion is the healing of a bone in a nonanatomic position that could result in the bone not being straight. The other options are not outcomes of improper reduction or immobilization. PTS: 1 REF: Page 1543 5. Which structure attaches skeletal muscle to bone? a. Tendon c. Bursa b. Ligament d. Mesentery A tendon is fibrous connective tissue that attaches skeletal muscle to bone. None of the other options are associated with this function. PTS: 1 REF: Page 1545 6. The tear in a ligament is referred to as a: a. Fracture c. Disunion b. Strain d. Sprain Ligament tears are commonly known as sprains. None of the other options are associated with this damage. PTS: 1 REF: Page 1545 7. Which medical diagnosis is characterized by tissue degeneration or irritation of the extensor carpi radialis brevis tendon? a. Lateral epicondylitis c. Bursitis b. Medial tendinitis d. Lateral tendinitis NURSINGTB.COM Only lateral epicondylopathy, commonly called tennis elbow, is the result of tissue degeneration or irritation of the extensor carpi radialis brevis tendon at its origin. PTS: 1 REF: Page 1546 8. The pain resulting from tendon and ligament injuries is usually described as: a. Dull and diffuse, persisting over the distribution of the tendon or ligament b. Sharp and localized, persisting over the distribution of the tendon or ligament c. Pins-and-needle sensations that occur distal to the injury with movement d. Intermittent and aching, occurring over the distribution of the tendon or ligament The pain resulting from tendon and ligament injuries is usually described as being sharp and localized, persisting over the distribution of the tendon or ligament. This selection is the only option that accurately describes this type of pain. PTS: 1 REF: Page 1545 9. How is rhabdomyolysis characterized? a. Paralysis of skeletal muscles, resulting from an impaired nerve supply b. Smooth muscle degeneration, resulting from ischemia c. Lysis of skeletal muscle cells through the initiation of the complement cascade d. Release of myoglobin from damaged striated muscle cells Rhabdomyolysis involves the release of myoglobin when muscle cells are damaged. This selection is the only accurate description of rhabdomyolysis. PTS: 1 REF: Pages 1547-1550 10. Which pathophysiologic alteration precedes crush syndrome after prolonged muscle compression? a. Muscle ischemia c. Volkmann contracture b. Myoglobinuria d. Neural injury Myoglobinuria is an excess of myoglobin (an intracellular muscle protein) in the urine. Muscle cell damage releases the myoglobin. The most severe form is often called crush syndrome. Less severe and more localized forms of muscle damage are called compartment syndromes. This selection is the only option that accurately identifies the pathophysiologic alteration that precedes crush syndrome. PTS: 1 REF: Pages 1547-1549 11. By the time osteoporosis is visible on an x-ray examination, up to what percent of bone has been lost? a. 30% c. 50% b. 40% d. 60% Generally, osteoporosis is radiographically detected as increased radiolucency of bone. By the time abnormalities are detecteNdUbRySxIN-rGayTBe.xCaOmMination, as much as 25% to 30% of bone tissue may have been lost. PTS: 1 REF: Page 1555 12. A bone density of 645 mg/cm2 would support which diagnosis? a. Osteoplasia c. Osteopenia b. Osteoporosis d. Osteomalacia The World Health Organization (WHO) has defined osteoporosis on the basis of bone density. Normal bone is greater than 833 mg/cm2; osteopenia, or decreased bone mass, is 833 to 648 mg/cm2; osteoporosis is less than 648 mg/cm2. This selection is the only accepted option. PTS: 1 REF: Page 1550 13. Which type of osteoporosis would a person develop after having the left leg in a cast for 8 weeks to treat a compound displaced fracture of the tibia and fibula? a. Iatrogenic c. Idiopathic b. Regional d. Osteoblastic Of the options available, only classic regional osteoporosis is associated with disuse or immobilization of a limb because of fractures, motor paralysis, or bone or joint inflammation. PTS: 1 REF: Page 1553 14. Considering the pathophysiologic process of osteoporosis, after being activated by receptor activator of nuclear factor B ligand (RANKL), receptor activator of nuclear factor B (RANK) activates which of the following? a. Osteoclast apoptosis c. Osteoprotegerin b. Osteoblast survival d. Osteoclast survival RANKL activates the receptor RANK, which is expressed on osteoclasts and their precursors and suppresses apoptosis, which leads to activation and the prolongation of osteoclast survival. This statement is not true of any of the other options. PTS: 1 REF: Page 1553 15. Considering the pathophysiologic process of postmenopausal osteoporosis, which changes are believed to play a significant role in the development of age-related bone loss? a. Increased oxidative stress and increased intracellular reactive oxygen species b. Hypoparathyroidism c. Increased body weight d. Decreased formation and short life span of osteoclasts Postmenopausal osteoporosis ocNcuUrRsSiInNGmTidBd.CleO-Maged and older women. It can occur because of estrogen deficiency, as well as estrogen-independent, age-related mechanisms (e.g., secondary causes such as hyperparathyroidism and decreased mechanical stimulation). Recent studies indicate that increased oxidative stress (OS) and increased intracellular reactive oxygen species (ROS) play significant roles in the development of age-related bone loss, as well as other age-related changes in the body. Hormonal deficiency also can increase with stress, excessive exercise, and low body weight. Increased formation and longevity of osteoclasts results in increased bone resorption and is associated with a cascade of proinflammatory cytokines. PTS: 1 REF: Page 1552 16. Considering the pathophysiologic process of osteoporosis, which hormone exerts antiapoptotic effects on osteoblasts but proapoptotic effects on osteoclasts? a. Parathyroid hormone c. Growth hormone b. Glucocorticoid d. Estrogen Data reveal that sex steroids (e.g., estrogens) exert antiapoptotic effects on osteoblasts but exert proapoptotic effects on osteoclasts; in both scenarios, activating the extracellular signal-regulated kinases (ERKs) accomplish these effects. This process is not true of any of the other options. PTS: 1 REF: Page 1553 17. Considering the pathophysiologic process of osteoporosis, what are the effects of extracellular signal-regulated kinases (ERKs) and receptor activator of nuclear factor B ligand (RANKL) on osteoblasts and osteoclasts? a. ERKs increase the life span of osteoclasts, and RANKL decreases the life span of osteoblasts. b. ERKs and RANKL increase the life span of osteoclasts and decrease the life span of osteoblasts. c. ERKs and RANKL increase the life span of osteoblasts and decrease the life span of osteoclasts. d. ERKs increase the life span of osteoblasts, and RANKL decreases the life span of osteoclasts. In addition to ERKs, RANKL is required for the antiapoptotic effect and thus longer life span of osteoclasts. This effect also shortens the life span of the bone-forming cells, or osteoblasts. This process is not true of any of the other options. PTS: 1 REF: Page 1553 18. What is the most common clinical manifestation of osteoporosis? a. Bone deformity c. Pathologic fracture b. Bone pain d. Muscle strain The most common clinical manifestation of osteoporosis is bone deformity. PTS: 1 REF: Page 15N5U5RSINGTB.COM 19. Which disorder is characterized by the formation of abnormal new bone at an accelerated rate beginning with excessive resorption of spongy bone? a. Osteomalacia c. Osteoporosis b. Paget disease d. Osteosarcoma Of the available options, only Paget disease (osteitis deformans) is a state of increased metabolic activity in bone characterized by abnormal and excessive bone remodeling, both resorption and formation. Chronic accelerated remodeling eventually enlarges and softens the affected bones. PTS: 1 REF: Pages 1557-1558 20. Which statement is false about factors that contribute to the difficulty in treating bone infections? a. Bone contains multiple microscopic channels that are impermeable to the cells and biochemicals of the body’s natural defenses. b. Microcirculation of bone is highly vulnerable to damage and destruction by bacterial toxins, leading to ischemic necrosis of bone. c. Bone cells have a limited capacity to replace bone destroyed by infections. d. Bacteria are walled off by macrophages and T lymphocytes; consequently, the antibiotics cannot penetrate the infected area. Bacteria are not walled off by macrophages and T lymphocytes, thus inhibiting the effects of antibiotics. The other options are true statements regarding factors that contribute to the difficulty in treating bone infections. PTS: 1 REF: Page 1560 21. Bone death as a result of osteomyelitis is due to what? a. Formation of immune complexes at the site of infection b. Localized ischemia c. Tumor necrosis factor–alpha (TNF-) and interleukin 1 (IL-1) d. Impaired nerve innervation at the site of infection Vessel damage causes local thrombosis (blockage) of the small vessels, which leads to ischemic necrosis (death) of bone. This selection is the only option that is associated with bone death as a result of osteomyelitis. PTS: 1 REF: Page 1560 22. When considering osteomyelitis, sequestrum is identified as what? a. An area of devascularized and devitalized bone b. An enzyme that phagocytizes necrotic bone c. A subperiosteal abscess d. A layer of new bone surrounding the infected bone Lifting of the periosteum disruptsNbUloRoSdINvGeTssBe.lCsOtMhat enter bone through the periosteum, which deprives the underlying bone of its blood supply. This deprivation leads to necrosis and death of the area of infected bone, producing sequestrum, an area of devitalized bone. None of the other available options accurately identify the term sequestrum. PTS: 1 REF: Page 1559 23. What pattern of bone destruction is described as not well-defined and not easily separated from normal bone? a. Moth-eaten c. Geographic b. Permeative d. Porous Moth-eaten pattern is the only option that involves destruction that is not well-defined and not easily separated from normal bone. PTS: 1 REF: Pages 1562-1563 | Table 44-5 24. Which statement accurately describes a characteristic of osteosarcoma? a. Slow-growing tumor that begins in the bone marrow and infiltrates the trabeculae b. Solitary tumor that most often affects the metaphyseal region of the femur or tibia c. Aggressive tumor most often found in the bone marrow of long bones d. Tumor that infiltrates the trabeculae in spongy bone and implants in surrounding tissue by seeding An osteosarcoma is a malignant bone-forming tumor. It is aggressive and most often found in bone marrow; it has a moth-eaten pattern of bone destruction. This selection is the only option that accurately describes a characteristic of osteosarcoma. PTS: 1 REF: Page 1563 25. Which statement is false concerning giant cell tumors? a. Giant cell tumors are an overexpression of genes including osteoprotegerin ligand (OPGL). b. The tumors are malignant, solitary, and irregularly shaped. c. Giant cell tumors are typically located in the epiphysis in the femur, tibia, radius, and humerus. d. They are slow-growing tumors that extend over the articular cartilage. The giant cell tumor is generally a benign, solitary, circumscribed tumor that causes extensive bone resorption because of its osteoclastic origin. The other options are true statements concerning giant cell tumors. PTS: 1 REF: Pages 1564-1565 26. Which is a characteristic of inflammatory joint disease? a. Unilateral joint involvement b. Normal joint synovial fluid c. Absence of synovial membrane inflammation d. Systemic symptoms of inflammation NURSINGTB.COM Inflammatory joint disease is characterized by systemic signs of inflammation (fever, leukocytosis, malaise, anorexia, hyperfibrinogenemia) and inflammatory damage or destruction in the synovial membrane or articular cartilage. This selection is the only option that accurately describes a characteristic of inflammatory joint disease. PTS: 1 REF: Page 1568 27. What is a primary defect in osteoarthritis? a. Stromelysin and acid metalloproteinase break down articular cartilage. b. Immunoglobulin G (IgG) destroys the synovial membrane. c. Synovial membranes become inflamed. d. Cartilage-coated osteophytes create bone spurs. Of the options available, the primary defect in osteoarthritis is the loss of articular cartilage. PTS: 1 REF: Pages 1565-1566 28. In osteoarthritis, what is the effect of the disruption of the pumping action of proteoglycans? a. Pump malfunction stimulates the induction of nitric oxide synthase and nitric oxide, which degrades the cartilage. b. Cartilage is damaged by proteolytic enzymes because they cannot be pumped out of the joint. c. Cartilage becomes dry, brittle, and wears away because fluid cannot be pumped into the cartilage. d. Cartilage takes in too much fluid and is unable to withstand the stresses of weight bearing. Changes in the conformation of proteoglycans disrupt the pumping action that regulates the movement of water and synovial fluid into and out of the cartilage. Without the regulatory action of the proteoglycan pump, cartilage imbibes too much fluid and becomes less able to withstand the stresses of weight bearing. This selection is the only option that accurately describes the disruption of the pumping action of proteoglycans when considering osteoarthritis. PTS: 1 REF: Page 1566 29. Which joint disease is characterized by joint stiffness on movement and joint pain of weight-bearing joints that is usually relieved by rest? a. Gouty arthritis c. Osteoarthritis b. Rheumatoid arthritis d. Suppurative arthritis Pain and stiffness in one or more joints, usually weight-bearing or load-bearing joints, are the first symptoms of osteoarthritis. Use-related joint pain relieved by rest is a key feature. This selection is the only option that accurately identifies the disease associated with the described symptoms. NURSINGTB.COM PTS: 1 REF: Page 1567 30. Which medical diagnosis is described as a chronic inflammatory joint disease characterized by stiffening and fusion of the spine and sacroiliac joints? a. Ankylosing spondylitis c. Paget disease b. Rheumatoid arthritis d. Fibromyalgia Of the options available, only ankylosing spondylitis (spondyloarthritis) is described as a chronic, inflammatory joint disease characterized by stiffening and fusion (ankylosis) of the spine and sacroiliac joints. PTS: 1 REF: Page 1572 31. What is the primary pathologic alteration resulting from ankylosing spondylitis (AS)? a. Inflammation of the sacroiliac joint b. Inflammation of the long bones c. Inflammation of fibrocartilaginous joints of the vertebrae d. Inflammation of the small hand and feet bones AS involves inflammation of fibrocartilage in cartilaginous joints, primarily in the vertebrae. The other options do not accurately describe the primary pathologic alterations of AS. PTS: 1 REF: Pages 1573-1574 32. In ankylosing spondylitis, the CD8+ T cells are presented with which antigen? a. Synovium c. Tendons b. Cartilage d. Ligaments Cartilage antigens are proposed as the targets for the immune response and the presentation of such antigens to CD8+ T cells. This statement is not true of any of the other options. PTS: 1 REF: Page 1573 33. People with gout are at high risk for which co-morbid condition? a. Renal calculi c. Anemia b. Joint trauma d. Hearing loss Renal stones are 1000 times more prevalent in individuals with primary gout than they are in the general population. This statement is not true of any of the other options. PTS: 1 REF: Page 1578 34. What causes the crystallization within the synovial fluid of the joint affected by gouty arthritis? a. Reduced excretion of purines b. Overproduction of uric acid NURSINGTB.COM c. Increase in the glycosaminoglycan levels d. Overproduction of proteoglycans When the uric acid reaches a certain concentration in fluids, it crystallizes, forming insoluble precipitates that are deposited in connective tissues throughout the body. Crystallization in synovial fluid causes acute, painful inflammation of the joint, a condition known as gouty arthritis. This selection is the only option that accurately identifies the cause of crystallization in synovial fluid associated with gouty arthritis. PTS: 1 REF: Pages 1574-1575 35. The pathophysiologic presentation of gout is closely linked to the metabolism of which chemical? a. Purine c. Vitamin E b. Pyrimidine d. Amino acid The pathophysiologic presentation of gout is closely linked only to purine metabolism (or cellular metabolism of purines) and kidney function. PTS: 1 REF: Page 1575 36. Which clinical manifestations are associated with fibromyalgia? a. Hot, tender, and edematous muscle groups bilaterally b. Fasciculations of the upper and lower extremity muscles c. Exercise intolerance and painful muscle cramps d. Sensitivity at tender points and profound fatigue Widespread joint and muscle pain, fatigue, and tender points are characteristics of fibromyalgia, a chronic musculoskeletal syndrome. Increased sensitivity to touch (i.e., tender points), the absence of systemic or localized inflammation, and fatigue and sleep disturbances are common. Fatigue is profound. The remaining options include symptoms not generally associated with fibromyalgia. PTS: 1 REF: Pages 1579-1580 37. At what age is peak bone mass and strength reached in women? a. 15 years c. 30 years b. 20 years d. 35 years Bone formation continues at a pace faster than resorption until peak bone mass—or maximum bone density and strength—is reached at approximately 30 years of age, after which bone resorption slowly exceeds bone formation. PTS: 1 REF: Page 1550 38. What event is associated with the beginning of bone loss in women? a. Puberty c. Childbirth b. Sexual activity NURSINGTdB..COMMenopause Bone loss in women is associated with menopause. Bone loss is most rapid in the first years after menopause but persists throughout the postmenopausal years. The other options are not relevant as triggers for bone loss. PTS: 1 REF: Page 1550 39. What term is used to identify the calcium crystals that are associated with chronic gout? a. Stones c. Tophi b. Spurs d. Nodes With time, crystal deposition in subcutaneous tissues causes the formation of small white nodules, or tophi, that are visible through the skin. Crystal aggregates deposited in the kidneys can form urate renal stones and lead to renal failure. None of the other options are associated with the calcium crystals resulting from chronic gout. PTS: 1 REF: Page 1575 MULTIPLE RESPONSE 40. What are the primary sources of bacterial infections that lead to hematogenous bone infection? (Select all that apply.) a. Sinus b. Ear c. Dental d. Cutaneous e. Throat , B, C, D Cutaneous, sinus, ear, and dental infections are all primary sources of bacteria in hematogenous bone infections. Throat infections are not generally associated with bone infections. PTS: 1 REF: Page 1559 41. Which structures are most often affected by Paget disease? (Select all that apply.) a. Vertebrae b. Skull c. Sternum d. Metacarpals e. Pelvis , B, C, E Paget disease most often affects the axial skeleton, especially the vertebrae, skull, sacrum, sternum, and pelvis. The metacarpals are not associated with the axial skeleton or Paget disease. PTS: 1 REF: Page 1558 42. Which clinical manifestations areNcUhaRrSaIcNteGrTisBt.iCcOoMf rheumatoid arthritis? (Select all that apply.) a. Subcutaneous tissue crystals b. Anorexia c. Painful, stiffening of joints d. Edema of the wrists e. Fever , C, E Rheumatoid arthritis begins with general systemic manifestations of inflammation, including fever, fatigue, weakness, anorexia, weight loss, and generalized aching and stiffness. Local manifestations also gradually appear over weeks or months. Typically, the joints become painful, tender, and stiff. Neither tissue crystals nor edema is associated with rheumatoid arthritis. PTS: 1 REF: Page 1571 MATCHING Match the phrases with the corresponding characteristics. A. Caused by sedatives and narcotics, particularly street heroin B. Caused by viruses, bacteria, and parasites C. Exercise intolerance with normal production of lactic acid D. Impairment of the breakdown of glycogen and production of lactic acid E. Autoimmune disease 43. McArdle disease 44. Myoadenylate deaminase deficiency 45. Rhabdomyolysis 46. Polymyositis 47. Myositis 43. ANS: D PTS: 1 REF: Page 1582 MSC: The individual with McArdle disease is not able to break down glycogen or produce lactic acid. 44. ANS: C PTS: 1 REF: Page 1583 MSC: Myoadenylate deaminase deficiency is an enzyme deficiency that produces changes in skeletal muscle and is associated with exercise intolerance. 45. ANS: A PTS: 1 REF: Page 1548 | Box 44-1 MSC: Sedatives and narcotics, particularly street heroin, clofibrate (a hypolipidemic agent), and the antifibrinolytic aminocaproic acid often cause rhabdomyolysis and myoglobinuria. 46. ANS: E PTS: 1 REF: Page 1584 MSC: Inflammation of connective tissue and muscle fibers that presumably causes the destruction of muscle fibers characterize polymyositis and dermatomyositis. The agent that causes the muscle inflammation has not been identified, but recent findings strongly suggest an autoimmune connection. 47. ANS: B PTS: 1 REF: Page 1583 MSC: Viral, bacterial, and parasitic infections of varying severity are known to produce inflammatory changes in skeletal muscle, a group of conditions collectively described by the term myositis. NURSINGTB.COM Chapter 46: Alterations of Musculoskeletal Function in Children MULTIPLE CHOICE 1. Until the skeleton matures and adult stature is reached, where does growth in the length of bone occur? a. Epiphyseal line c. Epiphyseal cartilage b. Physeal plate d. Metaphyseal plate Until the skeleton matures and adult stature is reached, growth in the length of bone occurs only at the physeal plate through endochondral ossification. PTS: 1 REF: Page 1592 2. Which skeletal deformity is normal at birth but generally disappears by 21/2 years of age? a. Genu varum (bowleg) c. Equinovarus (clubfoot) b. Genu valgum (knock knee) d. Pes planus (flat feet) Genu varum (bowleg) generally resolves itself by 21/2 years of age, whereas genu valgum (knock knee) maximizes by 5 to 6 years of age. This statement is not true of either equinovarus or pes planus. PTS: 1 REF: Page 1593 3. The total mass of muscle in the boNdUyRcSaInNGbeTBe.sCtiOmMated from which serum laboratory test value? a. Albumin c. Creatinine b. Blood urea nitrogen d. Creatine Of the options available, the total mass of muscle in the body can be estimated from the amount of creatinine excreted in the urine, because the conversion of creatine to creatinine only takes place in muscle. PTS: 1 REF: Page 1593 4. What is the most common congenital skeletal defect of the upper extremity? a. Vestigial tabs c. Rickets b. Paget disease d. Syndactyly The most common congenital skeletal defect of the upper extremity is syndactyly, or webbing of the fingers. PTS: 1 REF: Page 1593 5. What diagnosis is given when the infant’s hip maintains contact with the acetabulum but is not well seated within the hip joint? a. Dislocatable hip c. Dislocated hip b. Subluxated hip d. Subluxable hip Subluxated hip is the only option used to identify the condition when the hip maintains contact with the acetabulum but is not well seated within the hip joint. PTS: 1 REF: Page 1594 6. Which sign or symptom is a very late indication of developmental dysplasia of the hip? a. Asymmetry of the gluteal or thigh folds b. Leg-length discrepancy c. Waddling gait d. Pain Signs and symptoms of developmental dysplasia of the hip that should be noted include pain very late in the process. This statement is not true of the other options. PTS: 1 REF: Page 1595 7. Which serum laboratory test is elevated in all forms of osteogenesis imperfecta? a. Phosphorus c. Alkaline phosphatase b. Calcium d. Total protein Of the available options, serum alkaline phosphatase is elevated in all forms of the disease. PTS: 1 REF: Page 1598 NURSINGTB.COM 8. The failure of bones to ossify, resulting in soft bones and skeletal deformity, characterizes which disorder? a. Osteogenesis imperfecta c. Osteochondrosis b. Rickets d. Legg-Calvé-Perthes disease Of the available options, only rickets is a disorder in which growing bone fails to become mineralized (ossified) and results in soft bones and skeletal deformity. PTS: 1 REF: Page 1599 9. An insufficient dietary intake of which vitamin can lead to rickets in children? a. C c. B6 b. B12 d. D Rickets results from either insufficient vitamin D, insensitivity to vitamin D, wasting of vitamin D by the kidney, or inability to absorb vitamin D and calcium in the gut. Vitamin D is the only vitamin associated with rickets. PTS: 1 REF: Pages 1599-1600 10. In scoliosis, curves in the thoracic spine greater than how many degrees result in decreased pulmonary function? a. 40 c. 60 b. 50 d. 80 In scoliosis, curves in the thoracic spine greater than 80 degrees result in decreased pulmonary function. PTS: 1 REF: Page 1601 11. In osteomyelitis, bacteria gain access to the subperiosteal space in the metaphysis, which is considered the path of least resistance. What factor makes this route for bacteria the path of least resistance? a. Cortex of the bone in this area is porous or mazelike. b. Blood supply to the metaphysis is easily compromised. c. Macrophages and lymphocytes have limited access to the subperiosteal space. d. Bacteria usually spread down the medullary cavity of the bone. The subperiosteal space in the metaphysis is the path of least resistance because the cortex of the bone in this area is porous or mazelike, and the inflammatory response blocks spread within the bone. This statement is not true of the other options. PTS: 1 REF: Page 1602 12. How do the clinical manifestations and onset of juvenile rheumatoid arthritis (JRA) differ from those of rheumatoid arthritis (RA) in adults? a. JRA begins insidiously with systemic signs of inflammation. b. JRA predominantly affects larNgUe RjoSiInNtGs.TB.COM c. JRA has more severe joint pain than adult RA. d. JRA has a rapid onset of generalized aches as the first symptom. The onset of JRA is less gradual than it is in adult RA. JRA also differs from the adult form in that predominantly the large joints are affected in JRA. The remaining options are not accurate since the statements are true of RA as well. PTS: 1 REF: Page 1604 13. What is the cause of osteochondrosis? a. Imbalance between calcitonin and parathyroid hormone b. Nutritional deficiency of calcium and phosphorus c. Bacterial infection of the bone d. Vascular impairment and trauma to bone Of the options available, only vascular impairment and trauma to bone, coupled with an underlying developmental or genetic predisposition, have been identified as probable causes of osteochondrosis. PTS: 1 REF: Page 1604 14. Which bones are affected in Legg-Calvé-Perthes disease? a. Heads of the femur c. Heads of the humerus b. Distal femurs d. Distal tibias A recurrent interruption of the blood supply to only the femoral heads presumably produces Legg-Calvé-Perthes disease, which is a self-limited disease of the hip. PTS: 1 REF: Page 1604 15. Which statement is true regarding the pain experienced with Legg-Calvé-Perthes disease? a. Pain experienced with Legg-Calvé-Perthes disease in the elbows and upper and lower arms is aggravated by activity and relieved by rest. b. Pain experienced with Legg-Calvé-Perthes disease in the knees, inner thighs, and groin is described as a continuous ache and relieved by antiinflammatory drugs. c. Pain experienced with Legg-Calvé-Perthes disease in the knees, inner thighs, and groin is aggravated by activity and relieved by rest. d. Pain experienced with Legg-Calvé-Perthes disease in the elbows and upper and lower arms is described as a continuous ache and relieved by antiinflammatory drugs. The child with Legg-Calvé-Perthes disease often complains of a limp or pain for several months. The pain is usually referred to the knee, inner thigh, and groin and aggravated by activity and relieved by rest. This selection is the only option that accurately describes the pain associated with Legg-Calvé-Perthes disease. PTS: 1 REF: Page 1605 NURSINGTB.COM 16. Which assessment finding characterizes Osgood-Schlatter disease? a. Lateral epicondylitis of the elbow b. Inflammation of the anterior cruciate ligament c. Bursitis of the subscapular bursa in the glenohumeral joint d. Tendinitis of the anterior patellar tendon Tendinitis of the anterior patellar tendon, within which the patella (kneecap) is embedded, and associated osteochondrosis of the tubercle of the tibia are characteristics of Osgood-Schlatter disease. This selection is the only option that is associated with Osgood-Schlatter disease. PTS: 1 REF: Page 1605 17. At birth, the diagnosis of cerebral palsy (CP) may be made based on what factor? a. Brain trauma during birth c. Major brain malformation b. Prematurity d. Genetic defect The diagnosis of CP is often made when gross motor milestones are not met by predicted ages. In some infants, diagnosis is made at birth because the child has an underlying diagnosis, such as a major brain malformation that is known to be associated with CP. None of the other options are known triggers for CP. PTS: 1 REF: Page 1606 18. Which muscular dystrophy syndrome develops from an X-linked recessive mode of inheritance? a. Duchenne c. Myotonic b. Facioscapulohumeral d. Limb girdle A deletion of a segment of DNA or a single-gene defect on the short arm of the X chromosome is believed to be the cause of the X-linked inherited type of Duchenne muscular dystrophy. This statement is not true of the other options. PTS: 1 REF: Pages 1606-1607 | Table 45-4 19. Which protein, absent in muscle cells of Duchenne muscular dystrophy, mediates the anchoring of skeletal muscle fibers to the basement membrane? a. Syntrophin c. Dystrophin b. Laminin d. Troponin Only dystrophin is present in normal muscle cells and absent in Duchenne muscular dystrophy. Dystrophin mediates anchorage of the actin cytoskeleton of skeletal muscle fibers to the basement membrane through a membrane glycoprotein complex. PTS: 1 REF: Page 1607 20. What pulmonary complication in children with Duchenne muscular dystrophy contributes to their death? NURSINGTB.COM a. Infection c. Impaired formation of alveoli b. Kyphoscoliosis d. Cancer Although the life expectancy of boys with Duchenne continues to rise, death usually occurs from respiratory infection and a compromised respiratory system, with the majority living into their middle 20s. Some individuals who have chosen ventilatory support live a decade or more longer. This selection is the only option that is associated with the death and pulmonary complications experienced by children with this diagnosis. PTS: 1 REF: Pages 1607-1608 21. Generally, what is the first symptom of facioscapulohumeral muscular dystrophy? a. Inability to open the eyes completely c. Drooping shoulders b. Difficulty standing d. Facial pain As the name implies, clinical manifestations begin with weakness and atrophy of facial and shoulder girdle (scapulohumeral) muscles. The illness progresses slowly. An inability to close the eyes completely may be noted in early childhood. The face is expressionless, and pouting of the lips makes whistling impossible. The first symptoms usually include drooping of the shoulders with difficulty in raising the arms above the head. The onset of weakness in the lower limbs is often delayed for 20 to 30 years, and pseudohypertrophy of muscles is rare. PTS: 1 REF: Page 1609 22. What is the most common malignant bone tumor diagnosed during childhood? a. Chondrosarcoma c. Ewing Sarcoma b. Fibrosarcoma d. Osteosarcoma Of the options available, osteosarcoma is the most common bone tumor that occurs during childhood; it originates from bone-producing mesenchymal cells. PTS: 1 REF: Page 1610 23. Molecular analysis has demonstrated that osteosarcoma is associated with which gene? a. TP53 c. myc b. src d. TSC2 Of the options available, only the oncogene src has been associated with osteosarcoma. PTS: 1 REF: Page 1610 24. Osteosarcoma usually metastasizes to the: a. Pancreas c. Lungs b. Liver d. Brain Osteosarcoma disseminates through the bloodstream, usually to the lung. As many as 25% of children diagnosed with osteosaNrUcoRmSIaNGexThBi.bCiOt Mlung metastases at diagnosis. This statement is not true of any of the other options. PTS: 1 REF: Page 1610 25. A Ewing sarcoma arises from the: a. Bone marrow c. Metadiaphysis of long bones b. Bone-producing mesenchymal cells d. Embryonal osteocytes Arising only from bone marrow, Ewing sarcoma can break through the cortex of the bone to form a soft-tissue mass. PTS: 1 REF: Page 1611 26. Rhabdomyosarcoma can develop in which type of muscle? a. Cardiac c. Involuntary b. Smooth d. Striated Rhabdomyosarcoma can develop anywhere striated muscle is located. This statement is not true of the other options. PTS: 1 REF: Page 1612 27. Which organism is the primary cause of osteomyelitis in a newborn? a. Staphylococcus aureus c. Group B streptococcus b. Escherichia coli d. Bacillus anthracis S. aureus is the primary cause of osteomyelitis in a newborn. Group B streptococcus and E. coli infections are responsible for some cases, especially those of multiple bone involvement and in high-risk infants. S. aureus is the responsible microorganism in 80% to 90% of osteomyelitis cases in older children. Bacillus anthracis (anthrax) is not associated with osteomyelitis. PTS: 1 REF: Page 1602 28. What is the cause of structural scoliosis? a. Poor posture c. Poor calcium absorption b. Vertebral rotation d. Intrauterine trauma Structural scoliosis is the curvature of the spine associated with vertebral rotation. No research data suggest that any of the other options results in structural scoliosis. PTS: 1 REF: Page 1600 29. Which statements are true regarding bone growth before adulthood? (Select all that apply.) a. Growth in the length of bone occurs at the physeal plate. b. Growth occurs through endochondral ossification. c. Bone growth takes place under hormonal control. d. Cartilage cells at the epiphyseNalUsRidSeINoGfTtBhe.CpOhMyseal plate multiply and enlarge. e. Cartilage cells at the metaphyseal side of the plate are replaced by bone. B, D, E Until adult stature is reached, growth in the length of bone occurs at the physeal plate through endochondral ossification. Cartilage cells at the epiphyseal side of the physeal plate multiply and enlarge. As rapidly as new cartilage cells form, cartilage cells at the metaphyseal side of the plate are destroyed and replaced by bone. Bone growth is not hormonally controlled. PTS: 1 REF: Page 1592 30. The anatomic makeup of which bone structures make them susceptible locations for osteomyelitis in children? (Select all that apply.) a. Hip joint b. Distal femur c. Proximal humerus d. Distal radius e. Lateral ankle B, C, E Spread of infection to contiguous joints is related to the child’s age. Metaphyseal infection may spread to contiguous joints if the fibrous joint capsule includes the metaphysis and epiphysis. This special situation exists at the hip joint, distal femur, proximal humerus and radius, and lateral ankle. PTS: 1 REF: Page 1603 MATCHING Match the type of muscular dystrophy with its description. Types may be used more than once. A. Duchenne muscular dystrophy B. Facioscapulohumeral muscular dystrophy C. Myotonic dystrophy D. Becker muscular dystrophy 31. Onset occurs at approximately 3 years of age with rapid progression and frequently mental retardation. 32. The face is expressionless, and pouting of the lips makes whistling impossible. 33. Shares the X-linked inheritance pattern but produces milder symptoms. 34. Is an autosomal dominant condition with a slow rate of progression and frequently mental retardation. 31. ANS: A PTS: 1 REF: Pages 1606-1608 | Table 45-4 MSC: Duchenne muscular dystrophy is usually identified in children at approximately 3 years of age, when the parents first notice slow motor development with progressive weakness and muscle wasting. A moderate degree of mentaNlUreRtaSrIdNaGtiToBn.CcaOuMses these children to have a mean intelligence quotient (IQ) of approximately 85. 32. ANS: B PTS: 1 REF: Page 1609 MSC: Facioscapulohumeral muscular dystrophy exhibits a face that is expressionless, and pouting of the lips makes whistling impossible. 33. ANS: D PTS: 1 REF: Page 1608 MSC: Becker muscular dystrophy shares the X-linked inheritance pattern but produces milder clinical features. 34. ANS: C PTS: 1 REF: Page 1606 | Table 45-4 MSC: Myotonic dystrophy is a result of an autosomal dominant gene exhibiting a slow rate of progression and frequently mental retardation. Chapter 47: Structure, Function, and Disorders of the Integument MULTIPLE CHOICE 1. Which component of the epidermis initiates immune responses and provides a defense against environmental antigens? a. Langerhans cells c. Keratinocytes b. Merkel cells d. Melanocytes Langerhans cells (a type of dendritic cell) and dermal dendritic cells initiate an immune response by presenting processed antigen to T cells, thus providing a defense against environmental antigens. This function is not true of the other options. PTS: 1 REF: Page 1617 2. Which cells of the dermis release histamine and play a role in the hypersensitivity reactions of the skin? a. Histiocytes c. Mast cells b. Fibroblasts d. Macrophages Only mast cells release histamine and play a role in hypersensitivity reactions in the skin. PTS: 1 REF: Page 1618 3. Which cells of the dermis secrete NcoUnRnSeIcNtGivTeBt.iCsOsuMe matrix? a. Macrophages c. Fibroblasts b. Mast cells d. Histiocytes Only fibroblasts secrete the connective tissue matrix and collagen. PTS: 1 REF: Page 1618 4. Which gland releases secretions that are important in thermoregulation and cooling of the body through evaporation? a. Sebaceous c. Eccrine b. Apocrine d. Exocrine The eccrine sweat glands are distributed over the body, with the greatest numbers in the palms of the hands, soles of the feet, and forehead. These secretions are important in thermoregulation and cooling of the body through evaporation. This function is not true for the other options. PTS: 1 REF: Page 1618 5. Which receptors of the sympathetic nervous system regulate heat loss through the skin? a. Cholinergic c. -Adrenergic b. ß-Adrenergic d. Anticholinergic Heat loss can be regulated by varying blood flow through the skin by opening and closing the arteriovenous anastomoses in conjunction with evaporative heat loss of sweat. The sympathetic nervous system regulates vasoconstriction and vasodilation through -adrenergic receptors only. PTS: 1 REF: Page 1619 6. What is the first change in the skin that indicates a pressure ulcer? a. Blanchable erythema of intact skin b. Nonblanchable erythema of intact skin c. Blister at the site of pressure d. Reddish-purple discoloration Nonblanchable erythema of intact skin, usually over bony prominences, characterizes stage 1 pressure ulcers. This selection is the only option that accurately identifies the initial skin change indicative of a pressure ulcer. PTS: 1 REF: Page 1625 7. Which type of dressings should be applied to pressure ulcers? a. Flat and dry c. Bulky and dry b. Flat and moist d. Bulky and moist Superficial pressure ulcers should be covered with flat, nonbulky dressings that cannot wrinkle or cause increased pressurNeUoRrSfIrNicGtTioBn.C. SOpMontaneous healing will occur more quickly if the ulcer is kept moist with an occlusive dressing. PTS: 1 REF: Page 1626 8. What term is used to identify skin lesions that are elevated, rounded, and firm with irregular clawlike margins that extend beyond the original site of injury? a. Psoriasis c. Acne b. Dermatitis d. Keloid Of the options available, only keloids typically send out clawlike prolongations. PTS: 1 REF: Page 1626 9. Keloids are sharply elevated, irregularly shaped, progressively enlarging scars caused by excessive amounts of which substance in the corneum during connective tissue repair? a. Elastin c. Stroma b. Collagen d. Reticular fibers Abnormal wound healing with excessive fibroblast activity and collagen formation during dermal connective tissue repair cause keloids. The other options are not associated with keloid formation. PTS: 1 REF: Pages 1626-1627 10. In allergic contact dermatitis, which cells possess the antigens and present them to T cells? a. Langerhans cells c. Keratinocytes b. Merkel cells d. Macrophages In allergic contact dermatitis, only Langerhans cells process the antigen and carry it to T cells that then become sensitized to the antigen-releasing cytokines and chemokines, leading to leukocyte infiltration and inflammation. PTS: 1 REF: Pages 1627-1628 11. In latex allergies, which immunoglobulin (Ig) is associated with an immediate reaction? a. IgA c. IgG b. IgE d. IgM Latex allergy can be either a type IV hypersensitivity to chemicals used in latex rubber processing or a type I immediate hypersensitivity, with IgE antibodies formed in response to latex rubber protein. This selection is the only correct option available. PTS: 1 REF: Page 1628 12. What medical term is used to identify an inflammatory disorder of the skin that is often considered synonymous with dermatitis and characterized by pruritus with lesions that have an indistinct border? a. Eczema NURSINGTcB..COAMtopic dermatitis b. Psoriasis d. Pityriasis rosea The most common inflammatory disorder of the skin is eczema, or dermatitis. Eczema and dermatitis are general terms that describe a particular type of inflammatory response in the skin—these terms can be used interchangeably. Pruritus, lesions with indistinct borders, and epidermal changes generally characterize diseases that are considered eczematous. Of the available options, only eczema is associated with these characteristics. PTS: 1 REF: Page 1627 13. What clinical manifestations do allergic contact and stasis dermatitis have in common? a. Petechiae and hyperpigmentation c. Scaling and crusting of lesions b. Edema and vesicular lesions d. Erythema and pruritus Only erythema and pruritus are exhibited with both conditions. PTS: 1 REF: Pages 1627-1628 14. Lesions on the elbows and knees that are well demarcated, thick, silvery, scaly, and erythematous characterize which type of psoriasis? a. Plaque c. Guttate b. Inverse d. Erythrodermic The description provided is characteristic of only lesions observed in plaque psoriasis. These lesions are well-demarcated, thick, silvery, scaly, erythematous plaque surrounded by normal skin. PTS: 1 REF: Page 1629 15. Which skin disorder begins with a single lesion that is circular, demarcated, and salmon pink, measures approximately 3 to 4 cm in diameter, and is usually located on the trunk? a. Lichen planus c. Psoriasis b. Pityriasis rosea d. Acne rosacea Of the options available, only pityriasis rosea begins as a single lesion known as a herald patch. This lesion is circular, demarcated, and salmon pink; it measures approximately 3 to 4 cm in diameter and is usually located on the trunk. PTS: 1 REF: Page 1630 16. Which immunoglobulin is found in skin biopsy with immunofluorescent observation of people with discoid lupus erythematosus? a. Immunoglobulin A (IgA) c. Immunoglobulin G (IgG) b. Immunoglobulin E (IgE) d. Immunoglobulin M (IgM) Skin biopsy with immunofluorescent observation reveals lumpy deposits of immunoglobulins, especially IgM, in some individuals. This immunoglobulin is the only one associated with discoid lupusNeUryRthSIeNmGaTtoBs.CuOs.M PTS: 1 REF: Page 1632 17. Which term is used to identify a collection of infected hair follicles occurring most often on the back of the neck, the upper back, and the lateral thighs that forms a mass and evolves into an erythematous, painful, and edematous mass and drains through many openings? a. Erysipelas c. Carbuncles b. Furuncles d. Boils The term, carbuncle, is used to identify a collection of infected hair follicles occurring most often on the back of the neck, the upper back, and the lateral thighs. The lesion begins in the subcutaneous tissue and lower dermis as a firm mass that evolves into an erythematous, painful, and swollen mass and drains through many openings. PTS: 1 REF: Page 1635 18. Chickenpox (varicella) may be followed years later by which disorder? a. Erysipelas c. Warts (Verrucae) b. Cytomegalovirus d. Herpes zoster The same herpesvirus—varicella zoster virus (VZV)—causes both herpes zoster (shingles) and varicella (chickenpox). Varicella is the primary infection, followed years later by herpes zoster, particularly among those who are immunosuppressed. These statements are not true of any of the other options. PTS: 1 REF: Page 1636 19. What type of skin infection is tinea corporis (ringworm)? a. Nematode c. Viral b. Fungal d. Bacterial Tinea corporis is a fungal infection of the skin. This selection is the only option that accurately identifies the nature of the infection. PTS: 1 REF: Page 1637 20. Cutaneous vasculitis develops from the deposit of . a. Immune complexes c. Complement proteins b. Immunoglobulin E (IgE) d. T lymphocytes Cutaneous vasculitis involves the deposit of immune complexes, initiating an uncontrolled inflammatory response and causing the lesions that are often polymorphic. PTS: 1 REF: Page 1638 21. Which skin lesion is mediated by NthUeRiSmINmGuTnBo.gClOoMbulin E (IgE)–stimulated release of histamine, bradykinin, or kallikrein from mast cells? a. Dermatitis c. Urticaria b. Scleroderma d. Cutaneous vasculitis Only urticaria is mediated by the IgE-stimulated release of histamine, bradykinin, or kallikrein from mast cells or basophils, or both, which causes the endothelial cells of skin blood vessels to contract. PTS: 1 REF: Page 1639 22. Scleroderma is associated with . a. X-linked recessive gene c. Virus b. X-linked dominant gene d. Autoantibodies Scleroderma means sclerosis of the skin and is associated with immune dysregulation and several autoantibodies. This selection is the only option associated with scleroderma. PTS: 1 REF: Page 1639 23. What name is given to a benign proliferation of basal cells that produces smooth or warty elevated lesions on the chest, back, and face that are tan or waxy, yellow, flesh-colored, or dark brown to black? a. Basal keratosis c. Keratoacanthoma b. Seborrheic keratosis d. Actinic keratosis Seborrheic keratosis is a benign proliferation of cutaneous basal cells that produces smooth or warty elevated lesions. The pathogenetic origin is unknown. Seborrheic keratosis usually occurs in older people as multiple lesions on the chest, back, and face. The color varies from tan to waxy, yellow, flesh-colored, or dark brown to black. No other option exhibits these characteristics. PTS: 1 REF: Page 1640 24. Lesions that usually have depressed centers with rolled borders and are frequently located on the face and neck characterize which malignancy? a. Squamous cell carcinoma c. Malignant melanoma b. Kaposi sarcoma d. Basal cell carcinoma Of the available options, only basal cell carcinoma has depressed centers with rolled borders. Lesions are most often observed on people who live in regions with intense sunlight and on those areas of the skin most exposed—namely, the face and neck. PTS: 1 REF: Pages 1641-1642 25. The alteration of which gene is associated with basal cell carcinoma? a. myc c. src b. TP53 d. Ras NURSINGTB.COM Basal cell carcinoma arises as a consequence of ultraviolet-associated mutation in only the TP53 tumor-suppressor gene leading to the loss of keratinocyte repair functions and apoptosis resistance of DNA-damaged cells. PTS: 1 REF: Page 1642 26. Bowen disease is a form of which type of cancer? a. Kaposi sarcoma c. Basal cell carcinoma b. Malignant melanoma d. Squamous cell carcinoma Squamous cell carcinoma (SCC) is a tumor of the epidermis and the second most common human cancer. Two types are characterized: (1) in situ (Bowen disease) and (2) invasive. Bowen disease is not a form of any of the other options. PTS: 1 REF: Pages 1642-1643 27. A small (less than 1 cm) lesion with regular edges and bristlelike hairs with a color change that can range from skin tones to light brown characterize which form of nevus? a. Junctional c. Intradermal b. Epidermal d. Compound Only intradermal nevus is characterized by a small (less than 1 cm) lesion with regular edges and bristlelike hairs with a color change that can range from skin tones to light brown. PTS: 1 REF: Page 1643 | Table 46-9 28. Which cell is thought to be the progenitor cell of Kaposi sarcoma? a. Endothelial c. Melanocyte b. Keratinocyte d. Exothelial Only the endothelial cell is thought to be the progenitor of Kaposi sarcoma, but the specific origin is elusive. PTS: 1 REF: Page 1645 29. Which intervention is included in the treatment of frostbite? a. Applying local, dry heat c. Immersing in warm water b. Rubbing or massaging the area d. Leaving the area uncovered Immersion in a warm-water bath (40 to 42 C [104 to 107.6 F]) until frozen tissue is thawed is the best treatment for frostbite. Rubbing or massaging the area would damage the traumatized cells. The remaining options have no therapeutic value for frostbite. PTS: 1 REF: Page 1646 30. What is the purpose of administerNinUgRiSbIuNpGrToBfe.CnOtoMindividuals being treated for frostbite? a. Treating fever c. Reducing pain b. Preventing plate aggregation d. Inhibiting prostaglandins Ibuprophen is used to inhibit prostaglandins. Although ibuprofen may be administered for the other reasons stated, those applications are not related to the treatment of frostbite. PTS: 1 REF: Page 1646 31. What is the medical term for a fungal infection of the nail plate? a. Paronychia c. Tinea corporis b. Onychomycosis d. Tinea capitis Onychomycosis is the only term used to identify a fungal or dermatophyte infection of the nail plate that occurs in 2% to 18% of the population. PTS: 1 REF: Page 1647 32. What term is used to identify an inflamed hair root? a. Tinea c. Furuncle b. Verruca d. Erysipelas A furuncle, or “boil,” is used to identify an inflammation of the hair follicles (root) that may develop from a preceding folliculitis and spread through the follicular wall into the surrounding dermis. PTS: 1 REF: Page 1634 MULTIPLE RESPONSE 33. What effect does normal aging have on the wound healing process? (Select all that apply.) a. Decreased cell proliferation b. Decreased blood supply c. Depressed immune responses d. Depressed appetite e. Decreased cognitive function , B, C Decreased cell proliferation, decreased blood supply, and depressed immune responses delay wound healing in aging skin. The other options are not related to wound healing progress. PTS: 1 REF: Page 1619 34. Which statements are true regarding a nevus? (Select all that apply.) a. A nevus is an aggregation of melanocytes b. Nevi begin to form at the ages of 3 to 5 years. c. Nevi are characterized by irregular borders. d. Nevi share a relationship withNmUeRlSaInNoGmTaB..COM e. Nevi always warrant being removed. , B, D A nevus, or mole, is a benign pigmented or nonpigmented lesions that form from melanocytes beginning at ages 3 to 5 years. Over time the cells move down into the dermis and the nevi become nodular and symmetrical without irregular borders. Nevi may undergo transition to malignant melanomas. Nevi repeatedly traumatized, irritated by clothing, or large lesions can be excised. PTS: 1 REF: Page 1641 35. Which statements are true regarding Kaposi sarcoma? (Select all that apply.) a. South America has been the site of the endemic form of Kaposi sarcoma. b. Kaposi sarcoma is a vascular malignancy. c. It is associated with drug-induced immunosuppression. d. Kaposi sarcoma is associated with acquired immunodeficiency syndrome (AIDS). e. Presentation of the classic form of Kaposi sarcoma is observed on the lower legs of older men. , C, D, E Kaposi sarcoma is a vascular malignancy with four different presentations: (1) it is associated with drug-induced immunosuppression; (2) its endemic form has been found in equatorial Africa, (3) the classic form appears on the lower legs of older men, and (4) it is associated with AIDS. PTS: 1 REF: Page 1645 36. Which medications may exacerbate existing psoriasis? (Select all that apply.) a. Antibiotics b. Calcium channel blockers c. Nonsteroidal antiinflammatory drugs (NSAIDs) d. Beta blockers e. Lithium , D, E Antimalarial drugs, lithium, NSAIDs, and beta-blockers tend to exacerbate existing psoriasis. This statement is not true of the remaining options. PTS: 1 REF: Page 1629 37. Which inflammatory mediators are active in frostbite? (Select all that apply.) a. Leukotrienes b. Histamine c. Prostaglandins d. Bradykinin e. Thromboxanes , C, D, E The inflammatory mediators of frostbite are similar to burns and include prostaglandins, thromboxanes, bradykinin, and histamine. Leukotrienes are not associated with frostbite. PTS: 1 REF: Page 16N4U6RSINGTB.COM 38. Women who develop hirsutism may be secreting hormones associated with which condition? (Select all that apply.) a. Adrenal hyperplasia b. Cushing disease c. Polycystic ovaries d. Addison disease e. Adrenal tumor , C, E Women who develop hirsutism may be secreting hormones associated with ovarian or adrenal disease. Such women should be evaluated for polycystic ovaries, adrenal hyperplasia, or adrenal tumors. Neither Cushing nor Addison diseases are associated with hirsutism. PTS: 1 REF: Page 1647 MATCHING Match the descriptions of the skin lesions with the disorder where it is found. A. Elevated, firm circumscribed area less than 1 cm in diameter B. Elevated, firm, and rough lesion with a flat top surface greater than 1 cm in diameter C. Flat circumscribed area that is less than 1 cm in diameter D. Elevated irregular-shaped area of cutaneous edema; solid and transient with a variable diameter E. Elevated circumscribed, superficial lesion filled with serous fluid, less than 1 cm in diameter 39. Urticaria, allergic reaction 40. Varicella (chickenpox), herpes zoster (shingles) 41. Wart (verruca) or lichen planus 42. Psoriasis or seborrheic and actinic keratoses 43. Nevus (flat mole) 39. ANS: D PTS: 1 REF: Page 1621 | Table 46-3 MSC: Urticaria exhibits elevated, irregular-shaped areas of cutaneous edema. Its lesions are solid and transient with a variable diameter. 40. ANS: E PTS: 1 REF: Page 1621 | Table 46-3 MSC: Varicella (chickenpox) and herpes zoster (shingles) are elevated circumscribed, superficial lesions filled with serous fluid and measure less than 1 cm in diameter. 41. ANS: A PTS: 1 REF: Page 1620 | Table 46-3 MSC: Warts (verruca) or lichen planus are elevated, firm, circumscribed areas less than 1 cm in diameter. 42. ANS: B PTS: 1 REF: Page 1620 | Table 46-3 MSC: Psoriasis or seborrheic and actinic keratoses are elevated, firm, and rough lesions with flat-top surfaces that measure greater than 1 cm in diameter. 43. ANS: C PTS: 1 REF: Page 1620 | Table 46-3 MSC: A nevus is a flat, circumscribed area that is less than 1 cm in diameter. NURSINGTB.COM Chapter 48: Alterations of the Integument in Children MULTIPLE CHOICE 1. Which immunoglobulin (Ig) is elevated in atopic dermatitis? a. IgA c. IgE b. IgM d. IgG In the acute phase of atopic dermatitis, inflammation is associated with the activation of T helper 1 (Th-1) cells with an overexpression of cytokines (interleukin [IL]–4, IL-5, and IL-13) and chemokine ligand 1 (CCL1) and 18 (CCL18) with increases in IgE, eosinophils, and macrophages. The remaining options will not be elevated as related to atopic dermatitis. PTS: 1 REF: Page 1654 2. Which leukocytes are elevated in atopic dermatitis? a. Eosinophils c. Basophils b. Neutrophils d. Monocytes In the acute phase of atopic dermatitis, inflammation is associated with the activation of T helper 1 (Th-1) cells with an overexpression of cytokines (interleukin [IL]–4, IL-5, and IL13) and chemokine ligand 1 (CCL1) and 18 (CCL 18) with increases in IgE, eosinophils, and macrophages. Other leukocytes will not be elevated as related to atopic dermatitis. NURSINGTB.COM PTS: 1 REF: Page 1654 3. Which clinical manifestation is considered the hallmark of atopic dermatitis? a. Papular rash c. Vesicles that burst and form crusts b. High fever d. Itching Of the options, only itching is considered a hallmark of atopic dermatitis, and rubbing and scratching to relieve the itch are responsible for many of the clinical changes of atopic dermatitis. PTS: 1 REF: Pages 1654-1655 4. Frequently, diaper dermatitis is secondarily infected with which organism? a. Escherichia coli c. Proteus spp. b. Candida albicans d. Staphylococcus aureus Of the options available, frequently the infant with diaper dermatitis is secondarily infected with C. albicans. PTS: 1 REF: Page 1655 5. The disruption in cellular adhesion observed in bullous impetigo is caused by an exfoliative toxin related to which organism? a. Staphylococcus aureus c. Escherichia coli b. Streptococcus pyogenes d. Candida albicans Bullous impetigo is a rare variant of impetigo caused by S. aureus. The staphylococci produce a bacterial toxin called exfoliative toxin (ET), which causes a disruption in desmosomal adhesion molecules with blister formation characteristic of bullous impetigo. This selection is the only option that identifies the correct organism. PTS: 1 REF: Page 1656 6. The staff member of a crowed day care center is a source for which bacterial infection? a. Atopic dermatitis b. Staphylococcal scalded-skin syndrome c. Impetigo d. Tinea capitis Impetigo is a common bacterial skin infection in infants and children and is particularly infectious among people living in crowded conditions with poor sanitary facilities or in settings such as day care facilities. The other options are not as infectious as impetigo. PTS: 1 REF: Page 1656 7. Skin lesions that rupture, creating a thin, flat, honey-colored crust, are the hallmark clinical manifestation of which skin disordNeUrR? SINGTB.COM a. Rubella c. Atopic dermatitis b. Tinea capitis d. Bullous impetigo Of the options available, only the vesicular impetigo lesions that begin as small vesicles with a honey-colored serum are the hallmark clinical manifestation of bullous impetigo. Yellow to white-brown crusts form as the vesicles rupture and extend radially (see Figure 47-4). PTS: 1 REF: Page 1656 8. Skin lesions caused by tinea corporis are best described as: a. Pink-to-red coalescing maculopapular rash on the scalp or trunk b. Vesicles that rupture, creating a thin, flat, honey-colored crust c. Circular (round or oval) lesions with erythema and scaling patches d. Red papules, vesicles, and pustules in clusters Lesions caused by tinea corporis are often erythematous, round, or oval-scaling patches that peripherally spread with clearing in the center, creating the ring appearance, which is why this disease is commonly referred to as ringworm. None of the other options accurately describe the lesions associated with tinea corporis. PTS: 1 REF: Pages 1657-1658 9. What is a common contact source of tinea corporis? a. Mites c. Ponies b. Kittens d. Ticks Contact with only kittens and puppies is considered a common source of tinea corporis. PTS: 1 REF: Page 1657 10. What is the cause of molluscum contagiosum? a. Bacteria c. Fungi b. Virus d. Rickettsia The poxvirus is the only organism that induces epidermal cell proliferation and blocks immune responses that would control the virus as noted with molluscum contagiosum. PTS: 1 REF: Page 1658 11. Thrush is a superficial infection that commonly occurs in children and is caused by which organism? a. Staphylococcus c. Herpesvirus b. Streptococcus d. Candida albicans C. albicans infection is a superficial fungal infection that commonly occurs in children. C. albicans is part of the normal skin flora in certain individuals and invades susceptible tissue sites if the predisposing facNtoUrsRaSrINe GnToBt e.CliOmMinated. This description is not accurate for any of the other options. PTS: 1 REF: Page 1658 12. How is thrush best defined? a. Presence of Candida in the mucous membranes of the mouths of infants b. Presence of bacteria in the nasal mucous membranes of infants c. Any viral infection of the mucous membranes of the mouths of infants d. Acute immune response to oral medication, located in the mucosal lining of the mouths of infants Thrush is the term used to describe the presence of Candida in the mucous membranes of the mouth of infants and, less commonly, in the mouth of adults. This selection is the only option that accurately describes thrush. PTS: 1 REF: Page 1658 13. Which viral disease has an incubation period of 14 to 21 days and duration of 1 to 4 days? a. Rubeola c. Roseola b. Rubella d. Varicella Only rubella has an incubation period that ranges from 14 to 21 days and a duration of 1 to 4 days. PTS: 1 REF: Page 1658 14. Rubella (German or 3-day measles) is a common communicable disease of children caused by what type of organism? a. Virus c. Fungus b. Bacterium d. Yeast Rubella is a common communicable disease in children and young adults and is caused only by a ribonucleic acid (RNA) virus that enters the bloodstream through the respiratory route. PTS: 1 REF: Page 1658 15. Rubeola is a highly contagious acute disease in children caused by which type of infection? a. Bacterial c. Yeast b. Fungal d. Viral Rubeola, a highly contagious acute disease in children, is a result of only a viral infection. PTS: 1 REF: Page 1659 16. Which clinical manifestation is prNesUeRnStIiNnGrTuBbe.CoOlaMbut not in rubella? a. Conjunctivitis c. Presence of a cough b. Enlarged lymph nodes d. Runny nose Prodromal symptoms of rubeola include high body temperature (up to 40.5 C [104.9 F]), malaise, enlarged lymph nodes, runny nose, conjunctivitis, and a “barking” cough. Prodromal symptoms of rubella are few but may include enlarged cervical and postauricular lymph nodes, low-grade fever, headache, sore throat, runny nose, and cough. PTS: 1 REF: Pages 1658-1660 17. What is the cause of chickenpox? a. Poxvirus c. Adenovirus b. Varicella-zoster virus d. Human papillomavirus Only a varicella-zoster viral infection produces chickenpox (varicella) and herpes zoster (shingles). PTS: 1 REF: Page 1660 18. Which contagious disease has clinical manifestations of burrows several millimeters to 1 cm long, papules, and vesicular lesions with severe itching that worsens at night? a. Pediculosis c. Scabies b. Tinea capitis d. Rubeola Only scabies has symptoms that appear 3 to 5 weeks after infestation. The burrows, papules, and vesicular lesions cause severe itching that worsens at night. PTS: 1 REF: Page 1661 19. Which contagious disease creates a primary skin lesion that is a pinpointed macule, papule, or wheal with hemorrhagic puncture site? a. Pediculosis c. Scabies b. Tinea capitis d. Rubeola Of the options available, only the primary lesion of the body louse (pediculosis) exhibits a pinpoint red macule, papule, or wheal with a hemorrhagic puncture site. PTS: 1 REF: Page 1662 20. Which contagious disease is caused by the itch mite? a. Miliaria c. Pediculosis b. Tinea corporis d. Scabies Scabies is the only contagious disease caused by the itch mite, Sarcoptes scabiei. PTS: 1 REF: Page 1661 21. Which vascular anomaly is associNatUeRdSwINitGhTaBc.CoOnMgenital malformation of dermal capillaries that does not fade with age? a. Cutaneous hemangioma c. Strawberry hemangioma b. Port-wine (nevus flammeus) stain d. Cavernous hemangioma A port-wine stain is the only option that is present at birth or within a few days after birth and does not fade with age. PTS: 1 REF: Pages 1663-1664 22. Which skin disorder is characterized by a vesicular eruption after prolonged exposure to perspiration, with subsequent obstruction of the eccrine ducts? a. Scabies c. Pediculosis b. Tinea corporis d. Miliaria Of the available options, only miliaria is characterized by a vesicular eruption after prolonged exposure to perspiration, with subsequent obstruction of the eccrine ducts. PTS: 1 REF: Page 1664 23. What is the treatment plan for a strawberry hemangioma? a. Cosmetic surgical removal c. Oral antibiotics b. Topical steroid therapy d. Support of its involution Approximately 90% of strawberry hemangiomas involute by 5 to 6 years of age, usually without scarring; therefore self resolution is the usual treatment plan. PTS: 1 REF: Page 1663 If needing more Test Banks, just let me know: [email protected] MULTIPLE RESPONSE 24. Which statements are true of scalded skin syndrome? (Select all that apply.) a. Virulent group II staphylococci cause the scalded skin syndrome. b. A trauma burn triggers the syndrome. c. The syndrome results in a separation involving the epidermis. d. Toxins resulting from scalded skin syndrome are circulated through the blood. e. The lesions of scalded skin syndrome are sites of the infective organism. , C, D Virulent group II staphylococci, which produce an exfoliative toxin that attacks desmoglein and adhesion molecules and that causes a separation of the skin just below the granular layer of the epidermis, cause the scalded-skin syndrome. The toxins are usually produced at body sites other than the skin and arrive at the epidermis through the circulatory system. Staphylococci are not typically found in the skin lesions themselves. PTS: 1 REF: Page 16N5U6RSINGTB.COM 25. Which acne lesions are classified as inflammatory? (Select all that apply.) a. Closed comedones b. Opened comedones c. Nodules d. Papules e. Pustules , D, E Acne lesions may be divided into inflammatory lesions (pustules, papules, nodules) and noninflammatory lesions (closed and open comedones). PTS: 1 REF: Page 1653 26. Which statements are true regarding Koplik spots? (Select all that apply.) a. Koplik spots are associated with rubeola. b. They appear as white spots. c. The lesions are surrounded by a red ring. d. The lesions of Koplik spots are large in size. e. Koplik spots are primarily found on buccal mucosa. , B, C, E Rubeola infection begins with characteristic pinpoint white spots surrounded by an erythematous ring that develops over the buccal mucosa and are known as Koplik spots. PTS: 1 REF: Pages 1659-1660 MATCHING Match the viral disease with the skin lesions produced. Viral diseases may be used more than once. A. Rubella (German measles) B. Rubeola (red measles) C. Roseola (exanthema subitum) D. Varicella (chickenpox) E. Herpes zoster (shingles) 27. Erythematous macular rash over the trunk and neck that lasts 24 hours 28. Pinpoint white spots surrounded by an erythematous ring over the buccal mucosa 29. Groups of vesicles on an inflammatory base following the course of a sensory nerve 30. Pink-to-red coalescing maculopapular rash on the scalp or trunk 31. Red papules, vesicles, and pustules in clusters on the trunk, scalp, or face 27. ANS: C PTS: 1 REF: Page 1660 MSC: After the fever, roseola exhibits an erythematous macular rash that lasts approximately 24 hours and primarily develops over the trunk and neck. 28. ANS: B PTS: 1 REF: Pages 1659-1660 MSC: Rubeola's characteristic pinpoint white spots are surrounded by an erythematous ring, develop over the buccal mucosa, and are known as Koplik spots. 29. ANS: E PTS: 1 REF: Page 1660 MSC: Herpes zoster occurs in partiaNllyURimSImNuGnTeBi.nCdOivMiduals who have had varicella. 30. ANS: A PTS: 1 REF: Page 1658 MSC: Rubella exhibits a faint, pink-to-red coalescing maculopapular rash that develops on the face and spreads to the trunk and extremities 1 to 4 days after the onset of initial symptoms (see Figure 47-8). 31. ANS: D PTS: 1 REF: Page 1660 MSC: The first sign of illness may be itching or the appearance of vesicles, usually on the trunk, scalp, or face. The rash later spreads to the extremities. Characteristically, lesions can be observed in various stages of maturation with macules, papules, and vesicles present in a particular area at the same time (see Figure 47-9). Chapter 49: Shock, Multiple Organ Dysfunction Syndrome, and Burns in Adults MULTIPLE CHOICE 1. What is the final outcome of impaired cellular metabolism? a. Cellular alterations in the heart and brain b. Buildup of cellular waste products c. Cellular alterations in the vasculature structures and kidneys d. Impairment of urine excretion The common pathway in all types of shock is impairment of cellular metabolism as a result of decreased delivery of oxygen and nutrients, which are frequently coupled with an increased demand, the consumption of oxygen and nutrients, and a decreased removal of cellular waste products. Of the options available, this selection is the only accurate outcome. PTS: 1 REF: Page 1669 2. Which clinical manifestation of septic shock confirms an elevation in immune system response? a. Tachycardia c. Low respiratory rate b. Increased white blood cell count d. Hypothermia Clinical manifestations common in septic shock are fever, high heart rate, high respiratory rate, or elevations in immune respNoUnsReSsI,NsGuTchB.aCsOiMncreased white blood cells and circulating blood glucose. PTS: 1 REF: Page 1671 3. The release of catecholamine by the adrenal glands compensate for which initial effects of hypovolemic shock? a. Interstitial fluid moves out of the vascular compartment. b. Systemic vascular resistance is decreased. c. Heart rate is increased. d. Water excretion is increased. Compensatory mechanisms (see Figure 48-3) initially offset hypovolemia. Heart rate and systemic vascular resistance increase as a result of catecholamine release by the adrenal glands, which boosts cardiac output and tissue perfusion pressures. Compelled by a decrease in capillary hydrostatic pressures, interstitial fluid moves into the vascular compartment. The liver and spleen add to blood volume by disgorging stored red blood cells and plasma. In the kidneys, renin (through several intermediaries) stimulates aldosterone release and the retention of sodium and therefore water, whereas antidiuretic hormone (ADH), or vasopressin, from the posterior pituitary gland increases water retention. Data on the compensation of ADH, however, show that as shock worsens, ADH in plasma decreases. PTS: 1 REF: Page 1672 4. Hypovolemic shock begins to develop when intravascular volume has decreased by what percentage? a. 5 c. 15 b. 10 d. 20 Hypovolemic shock begins to develop when intravascular volume has decreased by approximately 15%. PTS: 1 REF: Page 1672 5. What type of shock develops as a result of the overstimulation of the parasympathetic nervous system or the understimulation of the sympathetic nervous system? a. Septic c. Anaphylactic b. Cardiogenic d. Vasogenic Only vasogenic shock refers to a widespread and massive vasodilation resulting from an imbalance between parasympathetic and sympathetic stimulation of vascular smooth muscle. PTS: 1 REF: Pages 1673-1674 6. What is the clinical hallmark of neurogenic shock as a result of the overstimulation of the parasympathetic nervous system? a. Vasoconstriction NURSINGTcB..COInMcreased metabolism b. Vasodilation d. Respiratory distress Neurogenic shock refers to a widespread and massive vasodilation that results from an imbalance between parasympathetic and sympathetic stimulation of vascular smooth muscle. None of the other options are related to this condition. PTS: 1 REF: Page 1673 7. Which form of shock is often more severe than other forms because of its sudden, rapid systemic vasodilation? a. Septic c. Anaphylactic b. Hypovolemic d. Neurogenic Anaphylactic shock is often more severe than other types of shock because the hypersensitivity reaction, which triggers vasodilation, has other pathophysiologic effects that rapidly involve the entire body. This action is not associated with the other options. PTS: 1 REF: Pages 1674-1675 8. What type of shock is related to a decrease in systemic vascular resistance? a. Septic c. Hypovolemic b. Cardiogenic d. Heart failure ANS: A Clinical manifestations of only septic shock are persistent low arterial pressure, low systemic vascular resistance from vasodilation, and an alteration in oxygen extraction by all cells. PTS: 1 REF: Page 1675 9. For which type of shock would antihistamines and corticosteroids be prescribed? a. Septic c. Hypovolemic b. Anaphylactic d. Cardiogenic Only anaphylactic shock responds to the administration of epinephrine to decrease mast cell and basophil degranulation. Antihistamines and steroids are administered to stop the inflammatory reaction. PTS: 1 REF: Page 1675 10. Which condition is best defined as a clinical syndrome involving a systemic response to infection, which is manifested by two or more of the systemic inflammatory response syndrome criteria? a. Bacteremia c. Septicemia b. Sepsis d. Septic shock Of the options available, only sepsis is best defined as a systemic response to infection that is manifested by two or more criteria of the systemic inflammatory response syndrome. NURSINGTB.COM PTS: 1 REF: Page 1676 | Table 48-1 11. In septic shock, which mediators are antiinflammatory? a. Interleukin (IL)–4 (IL-4), IL-10, and IL-13 b. Tumor necrosis factor–alpha (TNF-) and granulocyte cell-stimulating factor c. IL-1, IL-2, and IL-6 d. Prostaglandin, leukotrienes, and bradykinin In septic shock, the only antiinflammatory mediators released include lipopolysaccharide-binding protein; IL-1 receptor antagonist; soluble cluster of differentiation 14 (CD-14); type 2 IL-1 receptor; leukotriene 4-receptor antagonist; IL-4, IL-10, and IL-13; and soluble TNF. PTS: 1 REF: Page 1675 12. What mechanism causes organ injury in primary multiple organ dysfunction syndrome (MODS)? a. Impaired immune response c. Impaired perfusion b. Impaired glucose use d. Impaired ventilation In primary MODS, the organ injury is directly associated with a specific insult, most often ischemia or impaired perfusion from an episode of shock or trauma, thermal injury, soft-tissue necrosis, or invasive infection. None of the other options accurately identifies the cause of MODS. PTS: 1 REF: Page 1680 13. In secondary multiple organ dysfunction syndrome (MODS), what stimulates the normal endothelial cells to change to a proinflammatory state? a. Interleukin (IL)–4 (IL-4) and IL-13 b. IL-1, IL-6, and tumor necrosis factor (TNF) c. Interferon gamma (IFN-) and granulocyte cell-stimulating factor d. Prostaglandin, leukotrienes, histamine, and bradykinin Normal endothelial cells have little interaction with leukocytes except when stimulated by TNF, IL-1, and IL-6. This selection is the only option that accurately describes what stimulates the normal endothelial cells to change to a proinflammatory state. PTS: 1 REF: Page 1680 14. What stimulates the respiratory burst and production of highly toxic free radicals in the multiple organ dysfunction syndrome (MODS)? a. Neutrophils adhering to the endothelium b. Activation of the complement cascade c. Release of prostaglandins, thromboxanes, and leukotrienes d. Activation of the fibrinolytic sNyUstReSmINGTB.COM The accumulation of activated neutrophils in organs is thought to play a key role in the pathogenetic development of MODS. When neutrophils adhere to the endothelium, they undergo a respiratory burst (oxidative burst) and release oxygen radicals. The respiratory burst occurs as the activated neutrophil experiences a sudden increase in oxidative metabolism, producing large quantities of highly toxic oxygen free radicals. This selection is the only option that accurately identifies the stimulant of the respiratory burst that results in the production of toxic free radicals. PTS: 1 REF: Page 1682 15. In multiple organ dysfunction syndrome (MODS), the gut hypothesis attempts to explain which phenomena? a. Paralytic ileus b. Translocation of bacteria c. Maldistribution of blood flow d. Massive diarrhea accompanying septic shock The loss of intestinal barrier function leads to the systemic spread of bacteria and/or endotoxin from the gut (systemic endotoxemia). This phenomenon is called translocation of bacteria. The gut hypothesis provides a possible explanation for the fact that an infectious focus is not always found in individuals with MODS. The gut hypothesis is not related to any other option. PTS: 1 REF: Page 1682 16. Blistering of the skin within minutes occurs in which type of burn injury? a. First degree c. Deep second degree b. Superficial second degree d. Third degree ANS: B The hallmark of superficial partial-thickness injury is the appearance of thin-walled, fluid-filled blisters that develop within only a few minutes after injury. Blistering that occurs within minutes of the burn injury is not a defining characteristic of the other options. PTS: 1 REF: Page 1686 17. Which form of shock occurs from an acute burn injury? a. Hypovolemic c. Cardiogenic b. Septic d. Vasogenic Burn shock consists of a hypovolemic cardiovascular component and a cellular component. Hypovolemia associated with burn shock results from massive fluid losses from the circulating blood volumeN. UTRhSeINotGhTeBr .fCoOrmMs of shock are not directly related to an acute burn injury. PTS: 1 REF: Page 1689 18. Which fluid is most often used in fluid resuscitation after a major burn injury? a. Saline c. Lactated Ringer solution b. Albumin d. Dextrose in water Lactated Ringer solution is used most often because it closely approximates extracellular fluid, the repository of fluid leaving the circulatory system during this phase of extensive edema formation (see Table 48-4). The other options are not most often used in fluid resuscitation after major burns. PTS: 1 REF: Page 1689 19. What is the most reliable criterion of adequate fluid resuscitation after a major burn injury? a. Blood pressure c. Respiratory rate b. Pulse rate d. Urine output The most reliable criterion for adequate resuscitation of burn shock is urine output. None of the remaining options are considered reliable. PTS: 1 REF: Page 1690 20. The endpoint of burn shock is defined as the time when the individual is able to do which of the following? a. Maintain adequate blood pressure for 4 hours. b. Maintain adequate urine output for 2 hours. c. Manage pain without narcotics. d. Manage pain during dressing changes. The endpoint of burn shock is defined as the state in which the individual is able to maintain adequate urine output for 2 hours with the intravenous fluid administration rate equal to the individual’s calculated maintenance rate (see Box 48-4). None of the remaining options are defined as the endpoint of burn shock. PTS: 1 REF: Page 1690 21. Which condition does a burn injury create for an extended period? a. Hypervolemia c. Hyponatremia b. Hypermetabolism d. Hypotension Of the options available, a burn injury induces a hypermetabolic state that persists until wound closure. PTS: 1 REF: Page 1691 NURSINGTB.COM 22. What effect does a fatal burn injury have on interleukins (ILs)? a. Decreases levels of IL-2, which may decrease T helper 1 (Th1) lymphocytes. b. Decreases levels of IL-4, which causes a shift in production from Th1 to Th2 lymphocytes. c. Decreases levels of IL-6, which produces cytokines. d. Decreases levels of IL-12, which stimulates the production of immunoglobulins. A fatal burn injury has often shown decreased levels of IL-2, which may result in decreased Th1 lymphocytes. This option is the only accurate description of the effect a fatal burn injury has on ILs. PTS: 1 REF: Page 1692 23. Daily evaporative water loss after a burn injury is approximately how many times the normal? a. 5 c. 15 b. 10 d. 20 Moncrief and Mason attempted to determine the magnitude of such a loss and determined that daily evaporative water loss was in the range of 20 times normal in the early phase of injury, with gradual decreases as wound closure is achieved. PTS: 1 REF: Page 1693 24. What is the significance of a high level of interleukin 1 (IL-1) in a patient who has experienced severe burns? a. Prognosis is poor. c. Urinary function is improved. b. Antibiotic therapy is required. d. They are less at risk for death. The level of IL-1 inversely correlates with burn survival; low levels may be associated with a higher mortality. This selection is the only option that accurately identifies the significance of a high level of IL-1. PTS: 1 REF: Page 1692 25. What is the purpose of monitoring procalcitonin (PCT) levels in a patient after a burn? a. To help evaluate the potential risk for respiratory complications b. To justify the initiation of antibiotic therapy c. To determine when discontinuing antibiotic use is feasible d. To help in the selection of appropriate antibiotic therapy agents Seeking to decrease the use of antibiotics in the patient who is critically ill and thus prevent resistance to antibiotics is an important strategy in treating infection. Recent research suggests that monitoring serial PCT levels, a precursor hormone to calcitonin, may be used to shorten antibiotic use in the treatment of respiratory infections. PCT, normally not discernible on assay, when elevated may indicate specific proinflammatory response during a bacterial infection. PCT levels should not be used as an indicator to start antibiotics; however, if monitoredNsUeRquSIeNnGtiTalBly.CaOtMthe start of empiric antibiotics and then dropped to low levels, then discontinuation may be clinically indicated. PTS: 1 REF: Page 1679 | What's New box 26. How many milliliters of fluid replacement per hour does a 70-kg adult with a 50% total body surface area burn and a body surface area of 2 m require? a. 150 c. 350 b. 275 d. 500 A 70-kg adult with a 50% total body surface area burn and a body surface area of 2 m requires the following: Basal = (1500 ml/day) (2 m2 body surface area) = 3000 ml/24 hr or 125 ml/hr Evaporative = (25 + 50% total body surface burn) (2m2 total body surface area) = (75) (2) = 150 ml/hr Total maintenance fluids = 125 ml + 150 ml = 275 ml/hr PTS: 1 REF: Page 1690 | Box 48-4 MULTIPLE RESPONSE 27. A patient will be referred to the burn unit when which criteria are met? (Select all that apply.) a. Patient is older than 5 years of age. b. The burn involves the face or a major joint. c. The source of the burn is electrical. d. Partial thickness burns are on more than 10% of the total body surface area (TBSA). e. Patient has a life-threatening trauma injury. ANS: B, C, D A burn unit may treat adults or children or both. Burn injuries that should be referred to a burn unit include the following: partial-thickness burns on more than 10% TBSA, burns that involve the face, hands, feet, genitalia, perineum, or major joints, and electrical burns, including lightning injury. If the trauma poses the greater immediate risk, then the patient’s condition may be initially stabilized in a trauma center before being transferred to a burn center. PTS: 1 REF: Page 1689 | Box 48-3 28. Which feedback loop will further impair oxygen in all types of shock? (Select all that apply.) a. Activation of the fibrinolytic cascade b. Increased circulating volume c. Hypermetabolic state d. Lysosomal enzyme release e. Activation of the clotting cascade , E Both positive and negative compensatory mechanisms, such as anaerobic metabolism, lysosomal enzyme release, decreaNseUdRiSnItNraGvTaBs.cCuOlaMr volume, and activation of the clotting cascade, may further impair oxygen delivery and use. The remaining options are not related to impaired oxygen delivery. PTS: 1 REF: Page 1669 MATCHING Match the types of shock with the corresponding descriptions. Terms can be used more than once. A. Cardiogenic B. Hypovolemic C. Neurogenic D. Anaphylactic E. Septic 29. Follows a systemic inflammatory response. 30. Follows widespread hypersensitivity reaction. 31. Follows myocardial infarction. 32. Follows major burns. 33. Follows parasympathetic stimulation. 29. ANS: E PTS: 1 REF: Page 1675 MSC: Septic shock begins with systemic inflammatory response syndrome. It then evolves into sepsis, into severe sepsis, and finally into septic shock. 30. ANS: D PTS: 1 REF: Page 1674 MSC: Anaphylactic shock is the outcome of a widespread hypersensitivity reaction known as anaphylaxis. 31. ANS: A PTS: 1 REF: Page 1671 MSC: Cardiogenic shock results from the inability of the heart to pump adequate blood to tissues and end organs. This type of shock occurs from any cause, the most common being within hours of an acute myocardial infarction or severe episode of myocardial ischemia. 32. ANS: B PTS: 1 REF: Page 1689 MSC: Hypovolemia associated with burn shock results from massive fluid losses from the circulating blood volume. 33. ANS: C PTS: 1 REF: Pages 1673-1674 MSC: Any factor that stimulates parasympathetic activity or inhibits sympathetic activity of vascular smooth muscle can cause neurogenic shock. NURSINGTB.COM Chapter 50: Shock, Multiple Organ Dysfunction Syndrome, and Burns in Children MULTIPLE CHOICE 1. What is the most common type of shock in children? a. Hypovolemic c. Neurogenic b. Cardiogenic d. Septic Hypovolemic shock, the most common type of shock in children, is associated with a reduction in the intravascular volume relative to the vascular space. PTS: 1 REF: Page 1703 2. Hypotension is likely to occur when an infant or child is greater than % dehydrated. a. 2 c. 7 b. 5 d. 10 Hypotension typically develops when dehydration is greater than 10% in the infant or child or greater than 6% in the adolescent. PTS: 1 REF: Page 1703 3. A prolonged capillary refill time in children is consistent with the development of what type of shock? a. Hypovolemic NURSINGTcB..COCMompensated b. Septic d. Cardiogenic The child with hypovolemic shock demonstrates signs of inadequate blood flow to some tissue beds and some evidence of organ system dysfunction. The infant or child may be irritable or lethargic. Respirations will be rapid and may be labored if shock is severe or associated with myocardial failure. The skin will be mottled, although pallor also may be observed. A prolonged capillary refill time (>2 seconds) is consistent with the development of septic shock. This statement is not necessarily true of the other types of shock. PTS: 1 REF: Page 1704 4. Bradycardia in young children experiencing shock symptoms often suggests which result? a. Onset of cardiac dysfunction b. Effective management of cardiac dysfunction c. Good management of anxiety d. Cardiovascular collapse Bradycardia often indicates impending cardiovascular collapse or cardiac arrest and is the most common terminal cardiac rhythm observed in children. This selection is the only option that accurately describes the impact of bradycardia on a child. PTS: 1 REF: Page 1704 5. What is the cause of appropriately 50% of the deaths in children who have experienced a burn injury? a. Immunosuppression c. Inhalation injury b. Hypermetabolism d. Hypertrophic scarring The leading cause of death in children after burn injury, as in adults, is an inhalation injury. Inhalation injuries cause approximately 50% of all deaths in children with burns. Although the other options are factors, they are not responsible for 50% of the deaths. PTS: 1 REF: Pages 1715-1716 6. In cardiogenic shock, what is the cause of hepatomegaly and periorbital edema? a. Mass vasodilation as a result of chemical mediators released from the myocardium b. Low cardiac output, causing a high central venous pressure c. Tissue damage to the myocardium, causing increased capillary permeability d. Low perfusion of the kidneys, stimulating the renin-angiotensin-aldosterone system to retain sodium and water Evidence of an adequate or high central venous pressure, including hepatomegaly and periorbital edema, is observed in cardiogenic shock. This selection is the only option that accurately identifies the cause of these symptoms. PTS: 1 REF: Page 1704 NURSINGTB.COM 7. Approximately 80% of all hospital-acquired infections in children are a result of which type of organism? a. Bacteria c. Fungi b. Viruses d. Rickettsia In adults and children, approximately 40% of all hospital-acquired infections are linked to gram-negative infections, 40% to gram-positive infections, and 20% to viruses, fungi, or rickettsial microorganisms. PTS: 1 REF: Page 1707 8. Which cytokines are antiinflammatory mediators? a. Interleukin (IL)–1, IL-6, and tumor necrosis factor–alpha (TNF-) b. IL-8, IL-12, and platelet-activating factor c. IL-24, arachidonic acid metabolites, and nitric oxide d. IL-4, IL-11, and colony-stimulating factor Antiinflammatory mediators include only IL-4, IL-10, IL-11, and IL-13; transforming growth factor-beta; colony-stimulating factors; soluble TNF receptor; IL-1 receptor antagonist; and activated protein C. PTS: 1 REF: Page 1707 9. What type of injury is associated with cellular injury caused by the restoration of blood flow and physiologic concentrations of oxygen to cells that have been exposed to injurious but nonlethal hypoxic conditions? a. Hypoxic c. Reperfusion b. Hyperoxygenation d. Ischemic Reperfusion (reoxygenation) injury is associated with cell damage caused by the restoration of blood flow and physiologic concentrations of oxygen to cells that have been exposed to injurious but nonlethal hypoxic conditions. PTS: 1 REF: Page 1710 10. What are the primary goals for the treatment of shock? a. Maximizing oxygen delivery and minimizing oxygen demand b. Maintaining hydration and adequate urinary output c. Supporting all facets to the cardiovascular system d. Maintaining all vital signs within normal functioning ranges The primary goals of the treatment of shock are maximizing oxygen delivery and minimizing oxygen demand. Although the other options are desirable, they are each associated with the primary goals related to oxygen delivery and demand. PTS: 1 REF: Pages 1710-1711 11. To determine a child’s response toNfUluRiSdINthGeTrBap.CyOfMor shock, the nurse should monitor . a. Hematocrit and hemoglobin levels c. Blood pressure and pulse b. Urine output and specific gravity d. Arterial blood gases and heart rate Monitoring of the volume of urine output and specific gravity is most useful in determining the child’s response to fluid therapy. PTS: 1 REF: Page 1711 12. For children who are experiencing shock, crystalloids and colloids are generally administered in boluses of how many milliliters per kilogram (ml/kg)? a. 5 c. 15 b. 10 d. 20 In general, isotonic crystalloids (salt-containing solutions, such as normal saline or lactated Ringer solution) or colloids (protein-containing fluids, such as albumin or blood) are administered in boluses of 20 ml/kg. PTS: 1 REF: Page 1711 13. As the result of the inability to concentrate urine, children are at risk for dehydration before which age? a. 2 years c. 6 years b. 4 years d. 8 years Children younger than 2 years lack the ability to concentrate urine because of the immaturity of the renal system and are therefore at increased risk for dehydration. PTS: 1 REF: Page 1719 14. What causes renal failure after electrical burns in children? a. Cytokines are released after the damaged tissue. b. Immature kidneys are unable to compensate for the electrical burn. c. Cardiac output is reduced. d. Myoglobin is released from damaged muscles. The release of myoglobin may occlude the kidney tubules and result in renal failure. This selection is the only option that accurately describes the correlation between electrical burns and renal failure. PTS: 1 REF: Page 1719 15. Compared with the ebb phase, characteristics of the catabolic flow phase in metabolism after a burn injury in a child include which process? a. Reduced oxygen consumption c. Impaired circulation b. Elevation of catecholamines d. Cellular shock NURSINGTB.COM After the resolution of the shock and the restoration of circulating volume, the metabolic response shifts to a catabolic (flow) phase. A state of hypermetabolism ensues, characterized by increased oxygen consumption and the elevation of catecholamines, glucocorticoids, and glucagon. This selection is the only option that accurately compares the characteristics of the ebb and flow phases. PTS: 1 REF: Page 1720 16. What advantage do impregnated silver dressings have for patients with burn injuries? a. Impregnated silver dressings contain natural-occurring collagens. b. They require only one dressing change every other day. c. Removal is less painful. d. Impregnated silver dressings are cost effective. Impregnated silver dressings not only kill bacteria but most are processed with a special layer, making them less painful to remove. Some of these products can be left on the wound for up to 2 weeks, allowing for less frequent dressing changes. The other options are related to a new extracellular matrix (ECM) product that is now being researched for repair and remodeling of damaged tissues. PTS: 1 REF: Page 1722 | What's New box 17. What is the most serious outcome resulting from limited glycogen stores in children who have been seriously burned? a. Poor wound healing c. Decreased immunity b. Increased morbidity d. Loss of adipose tissue stores Glycogen stores are limited in children, making it hard for them to meet the increased energy demands of the burn. This prolonged metabolic dysfunction may lead to the loss of lean body mass. The most serious affect is increased morbidity; that is, the risk of additional illnesses will impede recovery. The remaining options do not represent the most serious outcome of limited glycogen stores resulting from severe burns. PTS: 1 REF: Page 1720 18. What is the normal range of respirations for an infant (in breaths per minute)? a. 18 to 25 c. 27 to 37 b. 20 to 28 d. 30 to 53 Although the other ranges may be normal for some age groups, the normal respiratory range for infants is 30 to 53 breaths per minute. PTS: 1 REF: Page 1702 | Table 49-1 19. While awake, what is the normal heart rate for toddlers (in beats per minute)? a. 100 to 205 c. 98 to 140 b. 100 to 180 d. 80 to 120 NURSINGTB.COM Although the other ranges may be normal for some age groups, the normal heart rate range for toddlers during waking hours is 98 to 140 beats per minute. PTS: 1 REF: Page 1702 | Table 49-1 MULTIPLE RESPONSE 20. Which statements are true regarding multiple organ dysfunction syndrome (MODS)? (Select all that apply.) a. Diagnosis requires simultaneous failure of at least two organs. b. Primary MODS occurs immediately after the attributing cause. c. Secondary MODS occurs within 3 to 7 days of the initial insult. d. Chronic illness increases a child’s risk for MODS. e. Risk factors for MODS include severe or prolonged shock, sepsis, and trauma. ANS: A, D MODS is the simultaneous failure of at least two organs resulting from a single cause and may be either primary or secondary. Primary MODS is directly attributable to the insult and typically occurs 3 to 7 days after an insult. Secondary MODS typically occurs later and may be associated with the more sequential development of organ dysfunction. Risk factors for MODS include severe or prolonged shock, sepsis, trauma, cardiopulmonary arrest, congenital heart disease, and liver and bone marrow transplantation. Children with chronic diseases have an increased risk for MODS and increased mortality. PTS: 1 REF: Pages 1699-1700 21. The child with septic shock has significant hypovolemia that typically responds to which interventions? (Select all that apply.) a. Aggressive fluid administration b. Antibiotic therapy c. Titration of inotropes d. Vasopressors e. High caloric nasogastric feedings , B, C, D The child with septic shock has significant hypovolemia that typically responds to aggressive fluid administration, antibiotic therapy, titration of inotropes, vasopressors, and vasodilators. Nasogastric feedings are not generally ordered for children with septic shock. PTS: 1 REF: Page 1709 22. Which behaviors in newborns would support the possibility of shock? (Select all that apply.) a. Decreased heart rate variabilitNyURSINGTB.COM b. Temperature instability c. Hyperalertness d. Increased muscle tone e. Hypoglycemia , B, E Nonspecific signs of distress in newborns include jitteriness or lethargy with decreased muscle tone, bradycardia or decreased heart rate variability, temperature instability, and hypoglycemia. PTS: 1 REF: Page 1700 | Box 49-1 23. Which assessment finding would be recognized as a late sign of shock in a child? (Select all that apply.) a. Metabolic (lactic) acidosis b. Cool skin c. Bradycardia d. Prolonged capillary refill e. Hypotension , E Although all of the options are observable, hypotension and bradycardia are recognized as late signs of shock in children. PTS: 1 REF: Page 1700 | Box 49-1 24. Which statements are true regarding how a child’s body compensates for cardiogenic shock? (Select all that apply.) a. Splanchnic arteries are constricted to divert blood from the skin, kidneys, and gut to the heart and brain. b. Peripheral blood vessels are constricted to raise blood pressure. c. Adrenergic responses produce tachycardia to increase cardiac output. d. The renin-angiotensin-aldosterone system is stimulated when renal function decreases. e. Compensation prevents the child from developing hepatic or mesenteric failure. , B, C, D In the early stages of cardiogenic shock, adrenergic compensatory mechanisms produce tachycardia, peripheral vasoconstriction, and constriction of the splanchnic arteries to divert blood flow from the skin, gut, and kidneys to maintain flow to the heart and brain. These compensatory mechanisms may be sufficient to maintain the child’s systolic blood pressure and effective coronary artery and cerebral blood flow. However, tachycardia and systemic arterial constriction increase myocardial oxygen consumption. In addition, reduction in gut and kidney blood flow may produce hepatic, mesenteric, or renal ischemia or failure. Decreased renal perfusion stimulates the renin-angiotensin-aldosterone system, as described for hypovolemic shock. PTS: 1 REF: Page 1704 25. What considerations must the nurse take into account when assessing the severity of a burn injury? (Select all that applyN.)URSINGTB.COM a. Amount of fluid lost over a 24-hour period b. Circumference of the burn injury c. Depth of the burn injury d. Severity of the injury caused to other body systems e. Percentage of total body surface area involved , E The severity of a burn injury is assessed on the basis of the percentage of the total body surface area involved. Because burn trauma represents a three-dimensional wound, the severity of injury is also assessed in relation to the depth of the injury. Although the other options are considered when planning treatment, the severity of the burn injury, itself, is not based on any of these. PTS: 1 REF: Pages 1716-1717 If needing more Test Banks, just let me know: [email protected] MATCHING Match the terms with the corresponding descriptions. A. Scald burn B. Contact burn C. Flame burn D. Electrical burn E. Chemical burn 26. Involves flammable liquids such as gasoline. 27. Is caused by hot grease. 28. Is the result of direct contact with high- and low-voltage current. 29. Is caused by a corrosive agent. 30. Involves cigarette burns and curling irons. 26. ANS: C PTS: 1 REF: Page 1716 MSC: Flame burns involving flammable liquids, especially gasoline, are most common in older children. 27. ANS: A PTS: 1 REF: Page 1715 MSC: Scald injuries (e.g., hot water, grease) are most common among young children. 28. ANS: D PTS: 1 REF: Page 1716 MSC: Electrical burns are the result of direct contact with high- or low-voltage current. 29. ANS: E PTS: 1 REF: Page 1716 MSC: Chemical burns occurring at home may be a result of swallowing corrosive agents. 30. ANS: B PTS: 1 REF: Page 1715 MSC: Contact burns may be intentionally inflicted by contact with cigarettes or other hot objects such as curling irons. NURSINGTB.COM [Show More]
Last updated: 3 years ago
Preview 1 out of 492 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$25.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Mar 18, 2020
Number of pages
492
Written in
All
Additional information
This document has been written for:
Uploaded
Mar 18, 2020
Downloads
0
Views
494

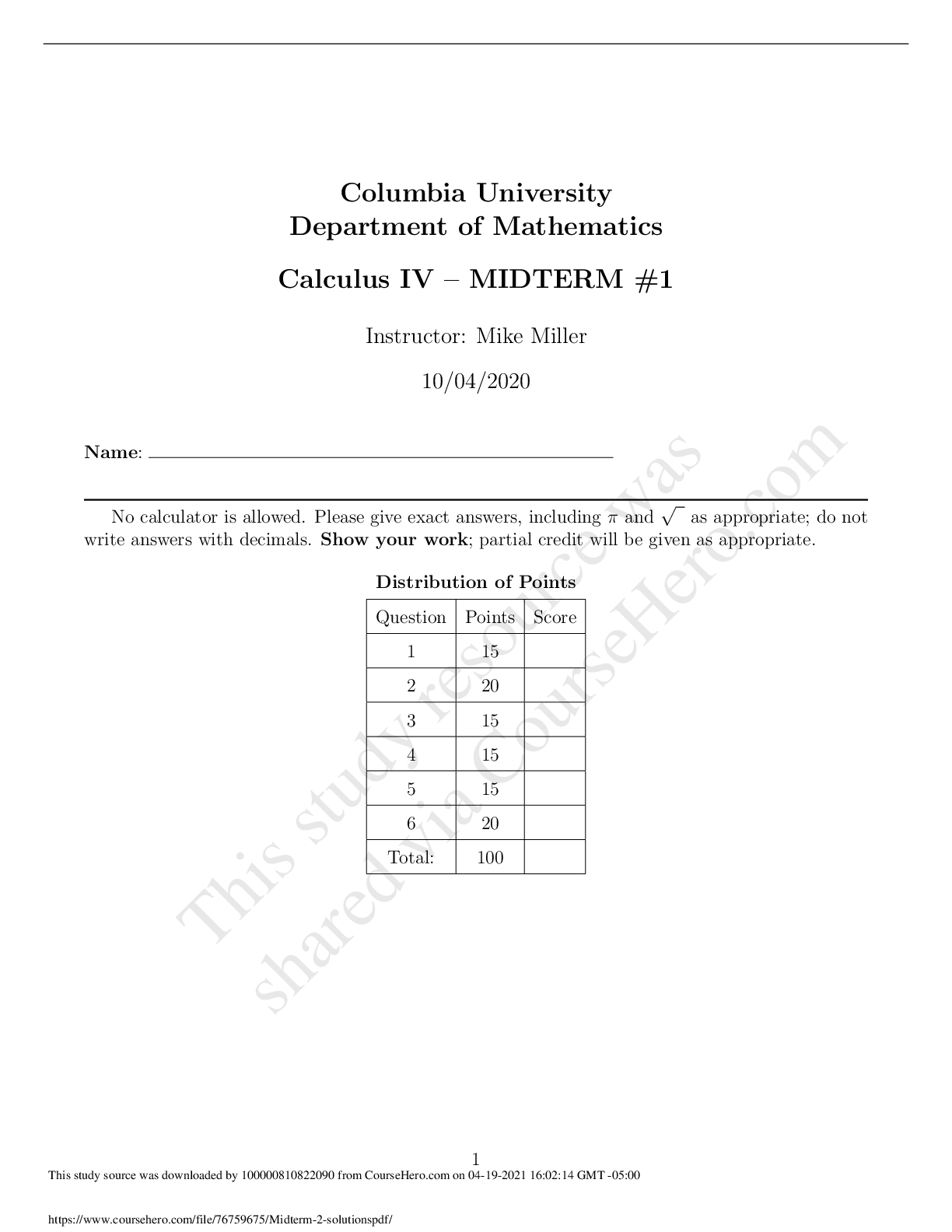


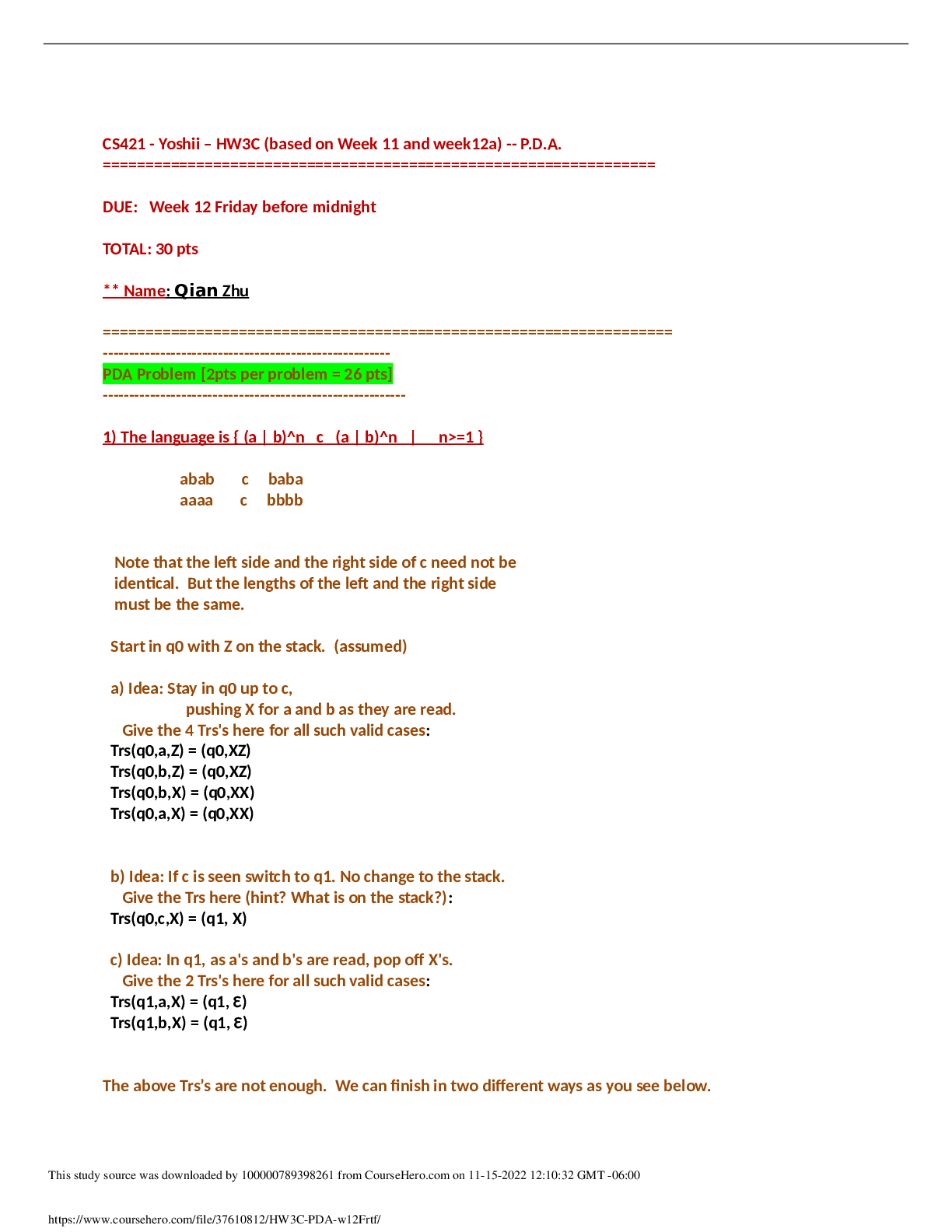


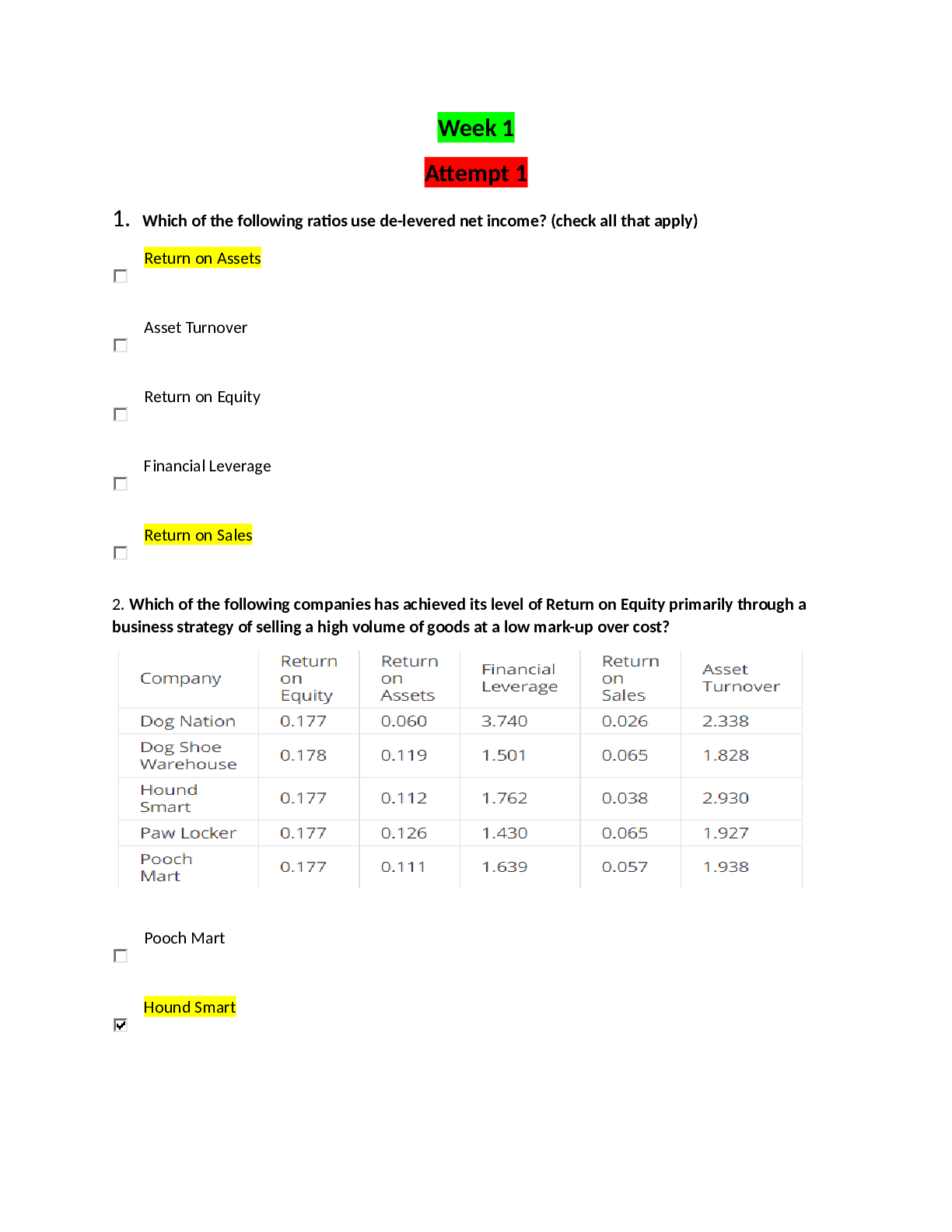
.png)
.png)
.png)
.png)
.png)