Cardiovascular and Lymphatic Systems: Questions, Answers and Study Notes: NURS6220.
Document Content and Description Below
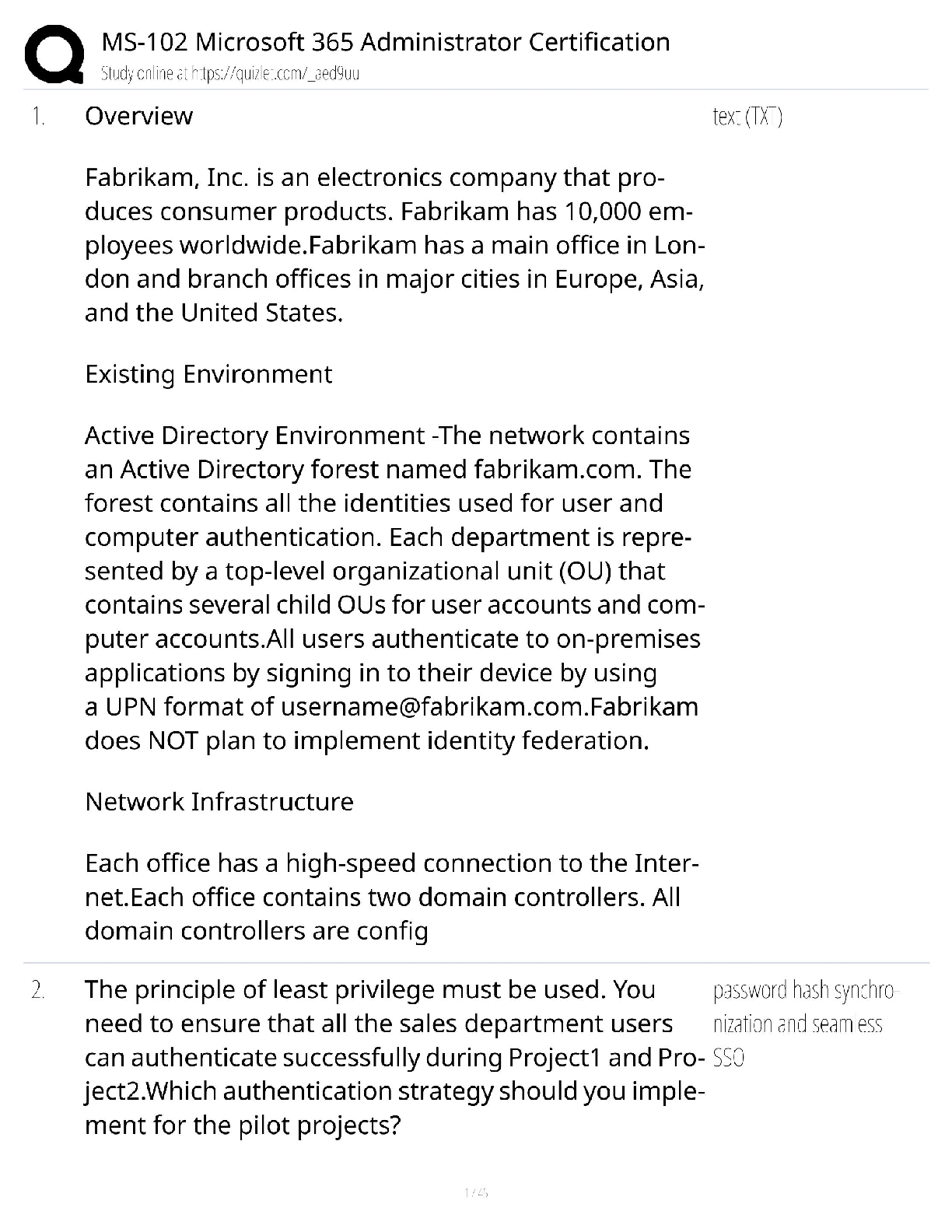
1. Describe the basic anatomy and physiology of the heart and circulatory system.
b. Atrial kick. Definition:
2. Define preload, afterload & contractility, and discuss their relationship to
...
one another.
Afterload- AKA systemic vascular resistance
Contractility-
3. Describe the vascular wall response to injury.
iii. Adventitia - outermost layer; supportive; made of loose connective tissue containing nerve fibers and vasa vasorum
. Describe the pathophysiology, diagnosis, and treatment of peripheral arterial disease
• Raynaud phenomenon and Raynaud disease
5. Describe the physiology of blood pressure regulation and the pathogenesis of hypertension.
iii. Cardiac output is determined by heart rate and stroke volume. The most important determinant of SV is the filling pressure
i. Pathogenesis of secondary HTN
1. Renovascular HTN 0 renal artery stenosis causes decreased
b. Mutations affecting proteins that influence sodium reabsorption.
ii. Quiz notes: Isolated systolic hypertension is an elevated systolic pressure with a normal diastolic pressure.
. Definition: hardening of the arteries; arterial wall thickening and loss of elasticity.
i. Three types:
1. Arteriosclerosis
2. Monckeberg medial sclerosis is characterized by calcification a. Atherosclerosis
. Definition: lesions on the intimal lining of blood vessels i. Pathogenesis - the “response to injury” hypothesis: This model views atherosclerosis as a chronic inflammatory and healing response of the arterial
An embolus is a bolus of matter that is circulating in the blood. A thrombus is a blood clot that remains attached to the vessel wall. Thrombophlebitis is the inflammation caused by a thrombus 2. Identify the laboratory values associated with lipoprotein evaluation. Identify the range of normal and abnormal lab values for cholesterol and triglycerides, and describe the implications of an abnormal lipid profile a. “The National Lipid Association and the National Cholesterol Education Program (NCEP) have set the following guidelines for lipids (total cholesterol, triglycerides, HDL cholesterol, LDL cholesterol, and non HDL cholesterol
6. Discuss vascular anomalies and disorders: including various types of aneurysms, vasculitis, disorders of blood vessel hyperreactivity, and venous disorders. An aneurysm is a localized abnormal dilation of a blood vessel or the heart that may be congenital or acquired. Abdominal aortic aneurysm- aorta becomes abnormally large and balloons out; most commonly caused by atherosclerosis; usually occurs in men ages 50 (to 60) or older Cerebral aneurysm Thoracic aortic aneurysm Non-infectious Vasculitis (pg. 506-512)-
i. Immune complex deposition
a. It is a chronic inflammatory disorder of large to small-sized arteries that principally affects arteries in the head- especially the temporal arteries • Thrombophlebitis and phlebothrombosis are interchangeable and = Deep vein thrombosis and inflammation. Blood vessel hyperactivity - inappropriate or exaggerated vasoconstriction of blood vessels • Myocar dial Vessel Vasospasm (pg. 514)- excessive constriction of coronary arteries or myocardial arterioles may cause ischemia, and persistent vasospasm can cause MI’s. 10. Describe the pathophysiology, clinical presentation, diagnostic procedures, and therapeutic intervention strategies related to:
i. Clinical Presentation
1. Asymptomatic latent period of 10-20 years
2. Exertional dyspnea (most common initial complaint
a. Brain natriuretic peptide (BNP) is a natriuretic peptide that is proposed to be a biochemical marker that screens for left ventricular dysfunction . Pathophysiology- abnormality in leaflets of mitral valve which prevents mitral valve from closing properly so blood backflow from left ventricle to left atrium iii. Therapeutic intervention
1. Manage symptoms of heart failure- beta blocker, ACEI, diuertics
d. Tricuspid regurgitation
. Pathophysiology
. Pathophysiology- stenosis of the valve so there is gradient in diastolic pressure between right ventricle and right atrium 11. Define coronary artery disease (CAD).
• Any vascular disorder that narrows or occludes the coronary arteries. Atherosclerosis • Strong links between lipoproteins and CAD. 12. Discuss the diagnosis and management of CAD. 13. Describe the clinical presentation of acute coronary syndromes (ACS), and discuss acute and long-term treatments. 14. Define congestive heart failure (CHF).
• Occurs when the heart is unable to pump blood at a rate sufficient to meet the metabolic demands of the tissues or can so only at an elevated 15. Describe the etiology, epidemiology, pathophysiology, clinical presentation, diagnosis and management of CHF. Left sided heart failure: most often caused by ischemic heart disease, htn, aortic and mitral valvular diseases, primary myocardial diseases 16. Describe the etiology, presentation, diagnosis and management of pulmonary edema.
dyspnea, need drugs that relieve fluid overload like diuretics, that block renin angiotensin aldosteroine axis (ACE) and that lower adrenergic tone (beta 2 adrenergic blockers).
17. Describe the etiology, clinical presentation, diagnostic procedures, and therapeutic interventions related to: 5. Childbirth- Special form of DCM called peripartum cardiomyopathy can occur late in pregnancy or up to months postpartum. 6. Iron Overload- can happen either from hereditary hemochromatosis or from multiple transfusions. v. Therapeutic Interventions
0. ACE inhibitors, ARBs, Beta Blockers, Aldosterone antagonists
18. Describe the electrophysiology of the heart.
Electrical impulses are generated automatically (when normal) by specialized cardiac cells (normally the SA node). Once an electrical cell generates an electrical impulse 19. Describe the underlying mechanisms of arrhythmia
a. Ischemic or structural changes in the conduction system or by intrinsic myocyte electrical instability. 20. Describe the basic principles and applications of electrocardiography
Electrocardiography is important diagnostic tool to diagnose cardiac disorders. 21. Describe the specific characteristics of basic rhythm disorders; identify common causes.
• Sinus tachycardia- heart rate will be greater than 100; there will be P wave with every QRS wave. Common causes include 22. Describe cardiovascular disorders seen in the pediatric population including congenital and acquired heart disease • Left to Right Shunts-most common congenital heart disease
• Right to Left Shunts- causes cyanosis early in postnatal life, TOF most common 23. Describe pericardial disorders (pg. 573-575).
Pericardial disorders - cause fluid accumulation, inflammation, fibrous constriction due to other cardiac pathology or systemic disease 24. Describe heart disease associated with rheumatologic disorders
a. Rheumatoid Arthritis
ii. Myocardial disease- Myocarditis is rare but is associated with active disease and can be reverses with aggressive immunosuppressive therapy • Kawasaki disease is an acute febrile, usually self-limiting illness of infancy and childhood; it’s associated with an arteritis affecting large to medium
[Show More]
Last updated: 3 years ago
Preview 1 out of 38 pages









.png)
.png)
.png)
.png)
.png)
.png)
.png)