Health Care > QUESTIONS & ANSWERS > Respiratory Physiology MCQs. Contains 226 Frequently tested Questions and Answers. Well organised re (All)
Respiratory Physiology MCQs. Contains 226 Frequently tested Questions and Answers. Well organised reading including Answer Explanations.
Document Content and Description Below
Respiratory Physiology Lung Compartments 1. A spirometer can be used to directly measure which of the following? (A) Functional residual capacity (B) Peak flow rate (C) Residual volume (D) Total... lung capacity (E) Vital capacity A spirometer is an instrument that records the volume of air moved into and out of the lungs during breathing, and therefore can only be used to measure lung volumes and capacities that can be exchanged with the environment. Spirometry can be used to measure the vital capacity, which is the maximal amount of gas that can be expired following a maximal inspiration. Spirometry cannot be used to meaure the volume of the gas that remains in the lungs following a maximal expiration (residual volume), and thus cannot directly measure the lung capacities that contain the residual volume, that is, the functional residual capacity and the total lung capacity. The peak flow rate is the maximal rate at which the volume of gas is exhaled. The measurement of flow rate requires a pneumotach, an instrument that integrates exhaled volume to derive the flow rate, or by a peak flow meter that patients can use at home, which are calibrated to record exhaled flow rates. 2. Which of the following lung volumes or capacities can be measured by spirometry? (A) Functional residual capacity (FRC) (B) Physiologic dead space (C) Residual volume (RV) (D) Total lung capacity (TLC) (E) Vital capacity (VC) Residual volume (RV) cannot be measured by spirometry. Therefore, any lung volume or capacity that includes the RV cannot be measured by spirometry. Measurements that include RV are functional residual capacity (FRC) and total lung capacity (TLC). Vital capacity (VC) does not include RV and is, therefore, measurable by spirometry. Physiologic dead space is not measurable by spirometry and requires sampling of arterial PCO2 and expired CO2. 3. Which volume remains in the lungs after a tidal volume (TV) is expired? (A) Tidal volume (TV) (B) Vital capacity (VC) (C) Expiratory reserve volume (ERV) (D) Residual volume (RV) (E) Functional residual capacity (FRC) (F) Inspiratory capacity (G) Total lung capacity During normal breathing, the volume inspired and then expired is a tidal volume (TV). The volume remaining in the lungs alter expiration of a TV is the functional residual capacity (FRC). Respiratory Physiology 4. The volume of gas in the lungs at the end of a normal expiration is referred to as the… (A)Residual volume (RV) (B) Expiratory reserve volume (ERV) (C) Functional residual capacity (FRC) (D)Inspiratory reserve volume (IRV) (E) Total lung capacity (TLC) The functional residual capacity (FRC) is the volume of gas in the lungs at the end of a normal expiration. Because expiration is passive, the lung volume decreases during expiration until the equilibrium volume (i.e., FRC) is reached. The equilibrium volume represents the volume of a distensible structure when the transmural pressure (i.e., the pressure inside minus the pressure outside) is zero. The residual volume (RV) is the volume of gas in the lungs following a maximal expiration. The expiratory re-serve volume (ERV) is the volume of gas that can be forcefully expired after a normal expiration, and the inspiratory reserve volume (IRV) is the additional volume of gas that can be inspired over the tidal volume. The total lung capacity (TLC) is the volume of gas in the lungs after a maximal inspiration. 5. When all ventilatory muscles are relaxed, the volume in the lungs is at: (A)Residual volume (RV) (B) Expiratory reserve volume (ERV) (C) Functional residual capacity (FRC) (D)Inspiratory reserve volume (IRV) (E) Total lung capacity (TLC) Muscles works are required during inspiration and forceful expiration (IRV & ERV). FRC is determined by chest wall recoil and lung recoil pressure, not muscle contractions. 6. A person starts to breathe from a 12 L spirometer containing 10% helium at the end of a passive expiration. If, after several minutes, the helium concentration in the spirometer falls to 8% this person’s functional residual capacity (FRC) is approximately: (A)1.2 L (B) 2.4 L (C) 3.0 L (D)4.0 L (E) 4.8 L V2 (FRC) = V1 × [([He]initial/[He]final) – 1] = 12 × [(10/8) – 1] = 12 × 2/8 = 3 [L]. Respiratory Physiology 7. Which volume remains in the lungs after a maximal expiration? (A) Tidal volume (TV) (B) Vital capacity (VC) (C) Expiratory reserve volume (ERV) (D) Residual volume (RV) (E) Functional residual capacity (FRC) (F) Inspiratory capacity (G) Total lung capacity During a forced maximal expiration, the volume expired is a tidal volume (TV) plus the expiratory reserve volume (ERV). The volume remaining in the lungs is the residual volume (RV). 8. In a maximal expiration, the total volume expired is (A) Tidal volume (TV) (B) Vital capacity (VC) (C) Expiratory reserve volume (ERV) (D) Residual volume (RV) (E) Functional residual capacity (FRC) (F) Inspiratory capacity (G) Total lung capacity The volume expired in a forced maximal expiration is forced vital capacity, or vital capacity (VC). 9. The ventilatory capacity of a patient with respiratory disease is evaluated using spirometry. Which of the following is the correct spirometric term for the largest exhaled volume that this patient can generate during the course of pulmonary function testing? (A)Total lung capacity (TLC) (B) Inspiratory capacity (IC) (C) Forced vital capacity (FVC) (D)Inspiratory reserve volume (IRV) (E) FEV1 Respiratory Physiology 10. A 45-year-old man inhaled as much air as possible and then expired with a maximum effort until no more air could he expired. This produced the maximum expiratory flow-volume curve shown in the following diagram. What is the forced vital capacity of this man (in liters)? (A) 1.5 (B) 2.5 (C) 3.5 (D) 4.5 (E) 5.5 (F) 6.5 The forced vital capacity (FVC) is equal to the difference between the total lung capacity (TLC) and the residual volume (RV). The TLC and RV are the points of intersection between the abscissa and flow-volume curve, that is, TLC = 5.5 L and RV = 1.0 L. Therefore, FVC = 5.5 – 1.0 = 4.5 L. 11. The vital capacity (VC) is the sum of the… (A)Residual volume (RV), tidal volume, and expiratory reserve volume (ERV) (B) RV, tidal volume, and inspiratory reserve volume (IRV) (C) RV, ERV, and IRV (D)ERV, IRV, and tidal volume (E) Functional residual capacity (FRC) and inspiratory capacity The vital capacity (VC) consists of the expiratory reserve volume (ERV), the inspiratory reserve volume (IRV), and the tidal volume. It is the maximal amount of gas that can be expired after a maximal inspiration. Residual volume (RV), the fourth primary subdivision of lung volume, is not included in the VC; it is the small volume of gas that remains in the lungs after a maximal expiration. The RV prevents complete collapse of the alveoli. Respiratory Physiology 12. In the patient’s spirometry tracing below, the expiratory reserve volume equals which of the following? (A) C (B) D (C) E (D) C + D (E) E – D Expiratory reserve volume (ERV) is the maximal volume of gas that can be exhaled in excess of a passive, tidal expiration. The ERV is not labeled in the diagram, but can be calculated from the difference between the functional residual capacity (FRC) and the residual volume (RV), designated as E and D, respectively. The FRC is the volume of gas remaining in the lungs following a passive, tidal exhalation. The RV is the volume of gas remaining in the lungs following a maximal expiration. The inspiratory reserve volume (IRV) is designated by A, the inspiratory capacity (IC) by B, and the vital capacity (VC) by C in the figure. 13. A 35-year-old man has a vital capacity (VC) of 5 L, a tidal volume (TV) of 0.5 L, an inspiratory capacity of 3.5 L, and a functional residual capacity (FRC) of 2.5 L. what is his expiratory reserve volume (ERV)? (A) 4.5 L (B) 3.9 L (C) 3.6 L (D) 3.0 L (E) 2.5 L (F) 2.0 L (G) 1.5 L Answer: G. Expiratory reserve volume (ERV) equals vital capacity (VC) minus inspiratory capacity. [Inspiratory capacity includes tidal volume (TV) and inspiratory reserve volume (IRV)]. Respiratory Physiology 14. At which one of the following lung volumes/capacities is transpulmonary pressure at its greatest? (A)Residual volume (B) Functional residual capacity (C) Total lung capacity (D)When breathing at rest (E) After taking a deep breath prior to diving into water Answer: C (and E). In order to breath more/ inhale more, there will need more negative intrapleural pressure. Thus, higher the lung volume, higher the (negative) pleural pressure. 15. All of the following can reduce vital capacity (VC) EXCEPT… (A)Decreased total lung capacity (TLC) (B) Increased residual volume (RV) (C) Weakness of the inspiratory muscles (D)Weakness of the expiratory muscles (E) Decreased alveolar surface tension A decreased alveolar surface tension increases lung compliance, resulting in an increased total lung capacity (TLC) and an increased vital capacity (VC). The VC equals the TLC minus the residual volume (RV), so either a decrease in TLC or an increase in RV can reduce the VC. Expanding the lungs to the normal TLC requires a strong inspiratory muscle force. Thus, weakness of the inspiratory muscles decreases the TLC. Similarly, expiratory muscle force is required to decrease the lung volume to the normal level of the RV. A decrease in expiratory muscle force can result in an increase in the RV. Questions 16-20 are based on the following graph, which shows a normal respiratory cycle followed by a maximal inspiration, a maximal forced expiration, and another normal respiratory cycle. Respiratory Physiology 16. Select the lettered arrow that corresponds to vital capacity (VC) The vital capacity (VC, indicated by the arrow labeled D) is the maximal volume of gas that can be expired after a maximal inspiration. The VC equals the sum of the tidal volume, the inspiratory reserve volume (IRV), and the expiratory reserve volume (ERV). 17. Select the lettered arrow that corresponds to forced expiratory volume in 1 second (FEV1) The forced expiratory volume in 1 second (FEV1) is the volume of gas that can be expired in 1 second during a maximal forced expiration. The forced expiration begins at the third second on the graph; the volume expired 1 second later is indicated by the arrow labeled C. 18. Select the lettered arrow that corresponds to functional residual capacity (FRC) The functional residual capacity (FRC, indicated by the arrow labeled B) is the reservoir of gas that remains in the lungs after a normal expiration. This gas buffers the changes in the O2 and CO2 tensions in the blood that traverses the capillaries between inspirations. 19. Select the lettered arrow that corresponds to total lung capacity (TLC) The total lung capacity (TLC, indicated by the arrow labeled A) represents the amount of gas in the lungs after a maximal inspiration. 20. Select the lettered arrow that corresponds to residual volume (RV) The residual volume (RV, indicated by the arrow labeled E) is the amount of gas in the lungs after a maximal expiration. The RV cannot be removed from the lungs, because the chest wall becomes rigid, preventing further reduction of lung volume. In older individuals, the RV is set by closure of the airways, which prevents further emptying of the lungs. Lung Mechanics 21. Which one of the following statements best characterizes lung compliance? (A) It is equivalent to △P/△V. (B) It is inversely related to the elastic recoil properties of the lung. (C) It decreases with advancing age. (D) It increases when there is a deficiency of surfactant. (E) It increases in patients with pulmonary edema Respiratory Physiology Lung compliance is an index of lung distensibility or the ease with which the lungs are expanded; thus, compliance is the inverse of elastic recoil. Compliance is defined as the ratio of change of lung volume to the change in pressure required to inflate the lung (△V/△P). Compliance decreases in patients with pulmonary edema or surfactant deficiency and increases when there is a loss of elastic fibers in the lungs, such as occurs in patients with emphysema and with aging. 22. Normally, intrapleural pressure is negative throughout a tidal inspiration and expiration because of which of the following? (A) The lungs have the tendency to recoil outward throughout a tidal breath. (B) The chest wall has the tendency to recoil inward throughout a tidal breath. (C) The intact pleura causes the lungs and chest wall to recoil away from each other throughout a tidal breath. (D) The intact pleura causes the lungs and chest wall to recoil in the same direction throughout a tidal breath. (E) There is always a small leak in the visceral pleura causing some air to escape into the pleural space during a tidal breath When the pleura, and hence the lung-chest wall system, are intact, the inward elastic recoil of the lung opposing the outward elastic recoil of the chest wall results in a subatmospheric (negative) pressure within the pleural space. When one reaches lung volumes in excess of approximately 70% of the total lung capacity, the chest wall recoil is also inward. 23. Which of the following regarding the transmural pressure for the lungs is true? (A)It is always negative (B) It is equal to the interpleural pressure minus the atmospheric pressure (PPL – PB) (C) It is equal to the interpleural pressure minus the alveolar pressure (PPL – PA) (D)It is equal to the alveolar pressure minus the interpleural pressure (PA – PPL) (E) It is independent of lung volume when the muscles are relaxed In the lungs, the transmural pressure is the transpulmonary pressure, which equals the alveolar pressure minus the interpleural pressure (PA – PPL). The transmural pressure simply represents the pressure across the wall of a hollow organ and is defined as the inside pressure minus the outside pressure. In humans, the interpleural pressure is estimated by measuring the esophageal pressure, because the esophagus is a flaccid tube that essentially traverses the pleural space. The interpleural pressure in animal experiments usually is measured by inserting a needle into an intercostal space and connecting it to a pressure gauge. The transmural pressure across the chest wall (i.e., transthoracic pressure) equals the interpleural pressure minus the pressure at the body surface, which is usually equal to the atmospheric pressure (PPL – PB). The lung is a Respiratory Physiology passive, elastic structure so that any change in lung volume produces a change in the trans-mural pressure. 24. Which of the following is true during inspiration? (A) Intrapleural pressure is positive (B) The volume in the lungs is less than the functional residual capacity (FRC) (C) Alveolar pressure equals atmospheric pressure (D) Alveolar pressure is higher than atmospheric pressure (E) Intrapleural pressure is more negative than it is during expiration During inspiration, intrapleural pressure becomes more negative than it is at rest or during expiration (when it returns to its less negative resting value). During inspiration, air flows into the lungs when alveolar pressure becomes lower (due to contraction of the diaphragm) than atmospheric pressure; if alveolar pressure were not lower than atmospheric pressure, air would not flow inward. The volume in the lungs during inspiration is the functional residual capacity (FRC) plus one tidal volume (TV). 25. During inspiration, as the diaphragm contracts, the pressure in the interpleural space becomes… (A)Equal to zero (B) More positive (C) More negative (D)Equal to the pressure in the alveoli (E) Equal to the pressure in the atmosphere Contraction of the inspiratory muscles expands the chest wall, increasing the transpulmonary pressure and making the interpleural pressure more negative. The chest wall expansion also expands the gas in the lungs, because the visceral and parietal pleurae are coupled by the interpleural fluid. The expansion of the alveolar gases decreases the alveolar pressure, which causes the gas to flow into the respiratory system through open airways. 26. During inspiration (as compared to expiration): (A) Intrapleural pressure is increasing (B) Lung recoil is increasing (C) Abdominal muscles are normally contracting (D) Both A and B are correct (E) All of the above are correct During inspiration, intrapleural pressure is becoming more negative, which means the pressure is decreasing. Since the lung enlarges, recoil is increasing. The Respiratory Physiology abdominal muscles are expiratory since they raise abdominal pressure and force the diaphragm into the thorax. 27. Taking a deep inspiration to total lung capacity causes which of the following cardiopulmonary function variables to increase? (A) Alveolar surface tension (B) Airway resistance (C) Elastic recoil of the lung (D) Intrapleural pressure (E) Lung compliance As lung volume increases toward total lung capacity (TLC), the compliance of the lungs (slope of pressure-volume curve) decreases and elastic recoil of the lung increases, that is, the lungs resist further expansion. Intrapleural pressure decreases, becoming more subatmospheric during inspiration, approaching –30 cm H2O at TLC. The more subatmospheric (negative compared to zero reference atmospheric pressure) increases radial traction and the transmural pressure across the intrathoracic airways (Pin – Pout) increases, which increases airway radius, and decreases airway resistance according to Poiseuille law. Alveolar surface tension varies inversely with alveolar radius, decreasing at higher alveolar volumes during inspiration. 28. During a forced expiration, a patient generates an intrapleural pressure of 20 mm Hg. The patient’s equal pressure point will move closer to the mouth and forced expiratory volume will increase if there is an increase in which of the following? (A) Inspired lung volume (B) Lung compliance (C) Airway resistance (D) Expiratory effort (E) Airway smooth muscle tone The equal pressure point is the point at which the pressure inside the airways equals the intrapleural pressure. The intra-airway pressure closest to the alveoli equals the sum of the recoil pressure (exerted by the alveoli) and the intrapleural pressure (produced by the muscles of expiration). The equal pressure point moves further away from the lungs if the recoil force is increased and moves closer to the lungs when the intrapleural pressure is increased. Increasing the lung volume expands the alveoli, making their recoil force greater and the intrapleural pressure less (more negative). This moves the equal pressure point toward the mouth. If airway resistance increases by increasing airway smooth muscle tone or increasing lung compliance, then a greater expiratory effort and consequently a greater intrapleural pressure will be necessary to expel the gas from the lungs. The higher intrapleural pressure when airway resistance is increased will cause the equal pressure point to be reached closer to the alveoli, decreasing the volume of gas exhaled, and increasing residual volume due to air trapping behind the compressed airways. Respiratory Physiology 29. If a person inspires maximally, closes his glottis, and contracts his expiratory muscles as hard as he can (Valsalva maneuver): (A) Intrapleural pressure is higher than alveolar pressure (B) Intrapleural pressure and lung recoil both act to increase pressure within the alveoli (C) Intrapleural pressure is below atmospheric at the apex but above atmospheric at the base (D) All of the above are correct (E) None of the above are correct During the Valsalva maneuver the contraction of expiratory muscles creates a very positive pressure in the thoracic cavity. This represents a force acting to collapse the lung. Since the glottis is closed and no air can flow, the positive intrapleural pressure and the force of recoil will combine to create a positive alveolar pressure. Alveolar pressure will be greater than intrapleural pressure by an amount equal to the force of recoil. 30. A 46 year old male during quiet breathing has an intrapleural pressure is about – 5 cm H2O at the start of inspiration (relative to atmospheric pressure). As inspiration proceeds to a full normal tidal breath, transmural pressure between the alveoli and the pleural space reaches approximately: (A)– 10 cm H2O (B) – 1 cm H2O (C) 0 cm H2O (D)+ 1 cm H2O (E) + 10 cm H2O PTM = PA – PIP. Intrapleural pressure usually change from – 5 to – 8 cm H2O during inspiration. Respiratory Physiology 31. A 28-year-old male oboe player in the symphony is referred to a pulmonologist due to increasing exertional dyspnea while playing. A complete pulmonary function study is ordered, and the patient is instructed to swallow an esophageal balloon for estimating changes in intrapleural pressures at various lung volumes. The figure below illustrates the change in the patient’s intrapleural pressure during a single tidal breath. At which point on the diagram is inspiratory airflow the greatest? During inspiration (curve ABC), the respiratory muscles pull the chest wall out and diaphragm down and intrapleural pressure (PIP) becomes more negative (subatmospheric). The muscles must overcome the elastic recoil forces of the lungs and the resistance of the airways to airflow. The PIP necessary to overcome the elastic forces of the lung is depicted by dashed line AC. The PIP necessary to overcome the airway resistance is the difference between dashed line AC and curve ABC. The maximum airflow occurs at point B, where the difference between the two is the greatest. 32. Maximal inspiratory gas flow occurs when the… (A)Lung volume approaches total lung capacity (TLC) (B) Lung volume approaches residual volume (RV) (C) Alveolar pressure is most negative (D)Interpleural pressure is approximately – 5 cm H2O (E) Abdominal muscles are maximally contracted The driving force for gas flow is the alveolar pressure; during normal breathing, negative pressures cause inspiratory flow, and positive pressures cause expiratory flow. It is the ratio of alveolar pressure to airway resistance that determines the actual flow of gas. As lung volume approaches either total lung capacity (TLC) or residual volume (RV), much of the muscle force is expended in overcoming the low compliance of the respiratory system. When the lung volume is in mid-range, alveolar pressure may he either positive or negative depending on muscle activity. The abdominal muscles are Respiratory Physiology expiratory muscles and, when contracted, generate positive alveolar pressures and expiratory flow if the airways are open. Use the following diagram to answer the next 2 questions. Respiratory Physiology 33. At what time is transpulmonary pressure greatest? (A)0 seconds (B) 1 seconds (C) 2 seconds (D)3 seconds (E) 4 seconds Pleural pressure is the most negative at time 2 seconds. 34. If the graph holds true for a patient breathing over a period of a minute what is the closest approximate to their alveolar minute ventilation (assuming a dead space of 200 ml). (A)2.5 L/min (B) 4 L/min (C) 6.5 L/min (D)8 L/min (E) Cannot be determined from this graph. VA = (VT – VD) × RR = (500 mL – 200 mL) × 1 breath/4.5 seconds = 300 × 13.33 = 4,000 mL = 4 L. 35. Which one of the following statements regarding the compliance of the respiratory system is true? (A)It is greater than the compliance of the chest wall (B) It is greater than the compliance of the lungs (C) It is equal to the compliance of the chest wall (D)It is equal to the compliance of the lungs (E) It is less than the compliance of the chest wall The compliance of the respiratory system (CRS) is determined by the compliance of the lungs (CL) and the chest wall (CCW) and can be calculated as 1/CRS = 1/CL + 1/CCW. Because of the need to add reciprocals, the compliance of the respiratory system always is less than the compliance of either of its parts. Respiratory Physiology 36. Which of the following is illustrated in the graph showing volume versus pressure in the lung-chest wall system? (A) The slope of each of the curves is resistance (B) The compliance of the lungs alone is less than the compliance of the lungs plus chest wall (C) The compliance of the chest wall alone is less than the compliance of the lungs plus chest wall (D) When airway pressure is zero (atmospheric), the volume of the combined system is the functional residual capacity (FRC) (E) When airway pressure is zero (atmospheric), intrapleural pressure is zero By convention, when airway pressure is equal to atmospheric pressure, it is designated as zero pressure. Under these equilibrium conditions, there is no airflow because there is no pressure gradient between the atmosphere and the alveoli, and the volume in the lungs is the functional residual capacity (FRC). The slope of each curve is compliance, not resistance; the steeper the slope is, the greater the volume change is for a given pressure change, or the greater compliance is. The compliance of the lungs alone or the chest wall alone is greater than that of the combined lung-chest wall system (the slopes of the individual curves are steeper than the slope of the combined curve, which means higher compliance). When airway pressure is zero (equilibrium conditions), intrapleural pressure is negative because of the opposing tendencies of the chest wall to spring out and the lungs to collapse. Respiratory Physiology 37. The respiratory system is at the equilibrium position in all of the following conditions EXCEPT… (A)At the end of a normal expiration (B) When the transrespiratory pressure is zero (C) When lung recoil is balanced by chest wall expansion (D)When lung volume is at residual volume (RV) (E) When the respiratory muscles are relaxed and the airway is open At residual volume (RV), the chest wall has a strong tendency to expand because it is far from its equilibrium position, which is about 80% of total lung capacity (TLC). At the same time, the recoil force of the lungs is reduced, because the RV is close to the equilibrium position of the lung. As a result of these unequal forces, either the expiratory muscles must be contracting to hold the respiratory system at that level, or the glottis must be closed to pre-vent gas from entering the airways. If the glottis is closed and the respiratory muscles are relaxed, then the strong expansion force of the chest wall causes the gas in the airways to expand. The alveolar gas pressure becomes less than atmospheric, and the transrespiratory pressure is negative. 38. The figure below represents the inflation pressure-volume curve of three different lungs. If the middle curve represents a normal lung, which of the following statements is correct? (A) The compliance of lungs A and B are both greater than normal. (B) Lung A is more compliant than normal, and at any lung volume recoil will be greater than in normal lungs. (C) Lung B is more compliant than normal, and at any given lung volume recoil will be greater than in normal lungs. (D) Lung A is more compliant than normal, and for a given change in surrounding pressure, a greater change in lung volume will occur than in normal lungs. (E) Lung B is more compliant than normal, and for a given change in surrounding pressure, a greater change in lung volume will occur than in normal lungs. Respiratory Physiology Curve A represents an increase in compliance. Recoil will be less at any given volume, and there will be a greater change in volume for a given change in intrapleural pressure. Curve B is a less compliant lung (stiffer lung). At any given lung volume, recoil will be greater and a large change in intrapleural pressure will be required for a given change in lung volume. 39. The following pressure-volume curves were obtained from subjects X and Y during quiet breathing at a rate of 14/min. What conclusion can you draw from these curves? Subject X has the: (A) Higher pulmonary compliance (B) Higher tidal volume (C) Higher pulmonary compliance and tidal volume (D) Lower pulmonary compliance (E) Lower pulmonary compliance and tidal volume In subjects X and Y, the decrease in intrapleural pressure was the same (close to 3 cm H2O). However, the inspired volume of X was greater than Y. The greater inspired volume of X with the same change in intrapleural pressure as Y means the lungs of subject X are more compliant. Since both subjects were taking a quiet breath, their volume changes represent tidal volumes. Respiratory Physiology 40. A patient comes into your office complaining of shortness of breath. He weighs 360 lbs is a non-smoker and has had no medical history of relevance. Which of the following changes, in any, would you expect to occur? (A)An increase in FRC due to an increase in lung compliance (B) A decrease in FRC due to a decrease in lung compliance (C) A decrease in FRC due to a decrease in chest wall recoil (D)An increase in FRC due to an increase in chest wall recoil (E) None of the above would be observed Too much fat reduces chest wall recoil and thus, shift the CWR curve right, and then FRC, the equilibrium point with lung elasticity decreases. (Smaller LR when the lung volume is smaller). 41. A 37-year-old woman is admitted to the hospital with severe kyphoscoliosis and respiratory muscle weakness. Which of the following physiological variables is most likely decreased in this patient? (A) Airway resistance (B) Alveolar surface tension (C) Arterial carbon dioxide tension (D) Chest wall compliance (E) FEV1/FVC Kyphoscoliosis is a deformity of the spine involving both lateral displacement (scoliosis) and anteroposterior angulation (kyphosis), which decrease the compliance of the chest wall. Decreased chest wall compliance and respiratory muscle weakness cause inadequate alveolar ventilation, which leads to an accumulation of carbon dioxide and a decrease in arterial pH (respiratory acidosis). Restrictive impairments are characterized by a decrease in all lung volumes and capacities, but a normal or increased ratio of FEV1 to FVC. Dynamic Airway Compression 42. An emphysematic patient comes to your office complaining of difficulty in breathing. You encourage him to exhale through pursed lips as this will help him by: (A)Moving the EPP closer to his alveoli (B) Increasing the compliance of his lungs (C) Keeping the oxygen tube in his mouth (D)Decreasing the pressure gradient between the alveoli and trachea (E) Decreasing the compliance of his lungs Let say, PA = gas pressure in alveoli, Paw = gas pressure in airway, PIP = intrapleural pressure, and ERP = elastic recoil pressure created by lung tissue (alveoli). Then, PA = PIP + ERP, and Paw is similar to PA, but PA > Paw. When Paw < PIP, the airway Respiratory Physiology collapse. Since PIP is part of the equation, what keeps the airway open is the value of ERP (ERP = PA – PIP or Paw – PIP). In patients with emphysema, they have increase lung compliance or decrease lung elasticity, thus lower ERP. Therefore, these patients’ airways tend to collapse earlier/proximal/closer to alveoli than healthy people. In order to supplement this loss/decrease, pursed lip creates/generates pressure at the mouth. This pressure can transmits down to the airways and help to keep them open. (Paw = PIP + ERP + PLP, where PLP; pressure created at the mouth by obstruction/narrowing). As a result, Pressure in trachea (normally equals to zero/atmosphere) is increased and thus decreases the pressure gradient between the alveoli and trachea. 43. The maximum expiratory flow-volume curve shown in the following diagram is used as a diagnostic tool for identifying obstructive and restrictive lung diseases. At which of the following points on the curve does airway collapse limit maximum expiratory air flow? the maximum expiratory flow-volume (MEFV) curve is created when a person inhales as much air as possible (point A, total lung capacity = 5.5 L) and then expires the air with a maximum effort until no more air can be expired (point E, residual volume = 1.0 L). The descending portion of the curve indicated by the downward pointing arrow represents the maximum expiratory flow at each lung volume. This descending portion of the curve is sometimes referred to as the “effort-independent” portion of the curve because the patient cannot increase expiratory flow rate to a higher level even when a greater expiratory effort is expended. Respiratory Physiology 44. At which point on the flow-volume loop pictured below will airflow remain constant despite an increased respiratory effort? A maximal expiratory flow volume curve is generated during a forced vital capacity maneuver. Only the initial expiratory flow is effort-dependent. That is, increasing expiratory effort will increase expiratory flow at points E and A (peak flow), but not at point B, which is referred to as the effort-independent portion of the maximal expiratory flow-volume curve. The inability to increase flow rates during the effort-independent portion is caused by compression of the noncartilaginous airways by the positive intrapleural pressures that are generated during a forced expiration when the expiratory muscles are actively contracted, a phenomenon called dynamic compression of the airways. No effort limitation occurs during inspiration (points C and D) because increased inspiratory efforts make the intrapleural pressure more negative, which expands the airways, lowering their resistance. 45. During the effort-independent portion of a forced vital capacity (EVC) maneuver, the expiratory flow rate… (A)Varies as a function of the interpleural pressure (B) Is limited by compression of the airways (C) Depends on the alveolar pressure (D)Is maximal for that individual (E) Is constant Dynamic compression of the airways occurs during forced expiration and limits the flow rate during the terminal 80% of expiration [i.e., effort-independent portion of a forced vital capacity (FVC) maneuver]. The driving force for expiration during the effort-independent period is the transpulmonary pressure, which is a function of lung volume. The term indicates that flow is independent of effort and that changes in expiratory force do not alter the flow rates. Therefore, the expiratory flow rate neither Respiratory Physiology varies as a function of the interpleural pressure nor depends on the alveolar pressure, because these values are altered by expiratory effort. The expiratory flow rate is not maximal, because maximal flow can be achieved only when lung volume is just below total lung capacity (TLC). Surfactant 46. If surfactant is absent from the alveoli, the lungs’: (A) Airway resistance will decrease (B) Compliance will increase (C) Compliance will decrease (D) O2 diffusing capacity will increase (E) Recoil will decrease A loss of surfactant will mean that recoil increases and compliance decreases (stiffer lung). Thus, more negative intrapleural pressures are necessary to keep the lung open and to inflate the lung. Choice A: This is a complex situation. The more negative intrapleural pressures will actually decrease resistance in the large airways, but peripheral congestion and collapse will produce the opposite. Choice D: The diffusing capacity for all gases will decrease because of the peripheral congestion and collapse. This will effectively decrease surface area for exchange. Interstitial edema will also increase membrane thickness. 47. Comparing a premature infant with respiratory distress syndrome to a normal full-term infant, how do lung compliance and surfactant levels compare? Compliance in Preterm Compared to Full Term Infant Surfactant in Preterm Compared to Full Term Infant (A) ↑ ↓ (B) ↑ ↑ (C) ↓ ↓ (D) ↓ ↑ (E) ↔ ↑ (F) ↔ ↓ A premature infant with respiratory distress syndrome has absent or reduced levels of surfactant. Loss of surfactant creates a greater surface tension. Since surface tension accounts for a large portion of lung elasticity, increasing surface tension will increase lung elasticity making the lung stiffer and less compliant. Respiratory Physiology 48. A lack of normal surfactant, as occurs in infants with respiratory distress syndrome (RDS), results in… (A)Increased lung compliance (B) Stabilization of alveolar volume (C) Increased retractive force of the lungs (D)Reduced alveolar-arterial O2 tension difference (E) Decreased filtration forces in the pulmonary capillaries The lack of normal surfactant produces a high alveolar surface tension, which increases the retractile force of the lungs, resulting in a high transmural pressure. The high transmural pressure means that the lungs are less distensible, and the alveoli tend to collapse because of the increased surface forces. In addition, the increased alveolar surface tension decreases the interstitial pressure, which increases the filtration forces across the pulmonary capillaries and leads to edema. The edema and atelectasis cause an abnormal range of values of the ventilation-perfusion ratio (VA/QC), which impairs gas exchange. The alveolar-arterial O2 tension difference is a good measure of the gas exchange capabilities of the lungs; this difference increases in the presence of ventilation-perfusion or diffusion abnormalities. 49. A deficiency of pulmonary surfactant would: (A)Decrease surface tension in the alveoli (B) Decrease the change in intrapleural pressure required to achieve a given tidal volume (C) Decrease lung compliance (D)Decrease the work of breathing (E) Increase functional residual capacity (FRC) Surfactant decreases the surface tension in the alveoli, increases the lung compliance. All other choices are result of surfactant and not the deficiency of surfactant. 50. An infant born prematurely in gestational week 25 has neonatal respiratory distress syndrome. Which of the following would be expected in this infant? (A) Arterial PO2 of 100 mm Hg (B) Collapse of the small alveoli (C) Increased lung compliance (D) Normal breathing rate (E) Lecithin:sphingomyelin ratio of greater than 2:1 in amniotic fluid Neonatal respiratory distress syndrome is caused by lack of adequate surfactant in the immature lung. Surfactant appears between the 24th and the 35th gestational week. In the absence of surfactant, the surface tension of the small alveoli is too high. When the pressure on the small alveoli is too high (P = 2T/r), the small alveoli Respiratory Physiology collapse into larger alveoli. There is decreased gas exchange with the larger, collapsed alveoli, and ventilation/perfusion (V/Q) mismatch, hypoxemia, and cyanosis occur. The lack of surfactant also decreases lung compliance, making it harder to inflate the lungs, increasing the work of breathing, and producing dyspnea (shortness of breath). Generally, lecithin:sphingomyelin ratios greater than 2:l signify mature levels of surfactant. 51. A 35-year-old woman with gestational diabetes develops hypertension and preeclampsia, requiring the preterm delivery of her fetus of 30-weeks’ gestation. The mother is given two doses of betamethasone, 12 mg, intramuscularly, 24 hours apart. Which of the following is the purpose of the antenatal steroid therapy? (A) Increase fetal PO2 (B) Increase blood flow to the fetal lungs (C) Shift the fetal oxyhemoglobin dissociation curve to the right (D) Increase blood flow from the right atrium into the left atrium across the foramen ovale (E) Increase the lecithin/sphingomyelin ratio in the amniotic fluid Maturation of surfactant production in fetal lungs is accelerated by glucocorticoid hormones, which increases the lecithin to sphingomyelin (L/S) ratio of the amniotic fluid. Lecithin (phosphatidylcholine) and sphingomyelin are choline phospholipids found in a variety of tissues. Lecithin is a major component of surfactant and its synthesis increases as the fetus matures and the lungs are prepared for expansion. Surfactant, a lipoprotein mixture, prevents alveolar collapse by permitting the surface tension of the alveolar lining to vary during inspiration and expiration. Thus, measurement of the L/S ratio in amniotic fluid provides an index of fetal lung maturity. 52. A 27-year-old man develops adult respiratory distress syndrome (ARDS) after near-drowning. Conventional mechanical ventilation on 100% O2 together with inhaled nitric oxide do not provide sufficient oxygenation. Porcine surfactant is instilled via fiberoptic bronchoscope, and the PaCO2, fraction of inspired oxygen (FIO2), and shunting improve impressively. The improvements in respiratory function occurred because surfactant increased which of the following? (A) Bronchiolar smooth muscle tone (B) The pressure gradient needed to inflate the alveoli (C) Lung compliance (D) Alveolar surface tension (E) The work of breathing Pulmonary surfactant increases lung compliance by lowering alveolar surface tension. As a result, the pressure gradient needed to inflate the alveoli decreases, as does the work of breathing. Although surfactant replacement therapy has proven to be beneficial in respiratory distress syndrome of the newborn, clinical trials of surfactant therapy in ARDS has had disappointing outcomes. Respiratory Physiology 53. A hospitalized patient has tachypnea and significantly labored respirations requiring mechanical ventilation. Based on the pressure-volume curve of the lungs shown as curve Z in the figure below, which of the following is the most likely diagnosis for the patient? (A) Asthma (B) Emphysema (C) Dyspnea with aging (D) Newborn with lecithin to sphingomyelin (L/S) ratio greater than 2 (E) Pulmonary edema Lung compliance is defined as the ease with which the lungs are expanded, and is calculated as the change in volume per change in pressure (△V/△P), which is the slope of the pressure-volume curve of the lung. Thus, curve Z is the pressure-volume curve of an individual with a decrease in lung compliance. The abnormal accumulation of fluid in the lungs (pulmonary edema) causes a restrictive pulmonary impairment characterized by decreased lung compliance. An L/S ratio ≥ 2 indicates normal biochemical maturation of the lung, with normal surfactant production and lung compliance (normal curve). If the L/S ratio is less than 2, such as may occur in preterm infants, there is an increased incidence of respiratory distress syndrome of the newborn, a restrictive impairment that would be characterized by curve Z. Aging and emphysema are characterized by an increase in lung compliance (curve X), which increases airway resistance. The increase in airway resistance in asthma is not associated with an increase (or decrease) in lung compliance. Respiratory Physiology Airway Resistance 54. Which of the following is the site of highest airway resistance? (A) Trachea (B) Largest bronchi (C) Medium-sized bronchi (D) Smallest bronchi (E) Alveoli The medium-sized bronchi actually constitute the site of highest resistance along the bronchial tree. Although the small radii of the alveoli might predict that they would have the highest resistance, they do not because of their parallel arrangement. In fact, early changes in resistance in the small airways may be “silent” and go undetected because of their small overall contribution to resistance. 55. The major area of airway resistance during breathing is located in the… (A)Oropharynx (B) Trachea and large bronchi (C) Intermediate-sized bronchi (D)Bronchioles < 2 mm in diameter (E) Alveoli The highest resistance to airflow occurs in the intermediate-sized bronchi because of the high airflow velocity in these segments. The airway tree develops such that each generation of airways is only slightly smaller in diameter than the parent airways. Thus, there is almost an exponential increase in cross-sectional area proceeding toward the periphery of the lung. Because of this relation-ship, the linear velocity of gas molecules decreases markedly as these molecules approach the terminal bronchioles. Therefore, very little pressure is required to achieve this velocity (i.e., there is a low resistance). Direct measurements indicate that bronchioles less than 2 mm in diameter represent less than 10% of the total airway resistance. 56. Airway resistance is greater… (A) With laminar flow than with turbulent flow (B) At lower values for Reynolds number (C) During inspiration compared to expiration (D) At low lung volumes compared to high lung volumes (E) In the total cross section of the small airways compared to the total cross section of the central airways As lung volume decreases, intrapleural pressure increases in accordance with Boyle’s law. The greater intrapleural pressure decreases the radial traction on the airways, thereby decreasing airway diameter and increasing airway resistance. During a forced expiration or at residual volume, the intrapleural pressure actually becomes positive, Respiratory Physiology compressing the airways and increasing their resistance. The vagus nerve constricts airway smooth muscle Resistances in parallel add as reciprocals. Thus, the large number of small, peripheral airways increases the number of airways arranged in parallel, and lowers the total resistance of the peripheral airways compared to the total cross-section of the central airways. 57. Resistance in the airways of the lungs decreases: (A) In response to sympathetic nerve stimulation (B) In response to parasympathetic nerve stimulation (C) In response to a decrease in alveolar PCO2 (D) As the diameter of the air tubes decreases (E) As the velocity of airflow increases Sympathetic stimulation of airway smooth muscle causes a relaxation and parasympathetic stimulation causes constriction. Thus, sympathetics cause a decrease in airway resistance. Choice C: There is a local phenomenon in the lung system whereby if PACO2 decreases; there is a decrease in alveolar ventilation due to constriction of the alveolar ducts. This is not nearly as important as hypoxic constriction, but it does tend to keep V/Q closer to the ideal value. Choice D: As the diameter of a tube decreases, resistance would increase. Choice E: An increase in velocity promotes turbulence. A more turbulent system means a higher resistance. 58. Airway resistance can be reduced by… (A)Increasing vagal impulses to the lungs (B) Administering a p-adrenergic blocking drug (C) Decreasing the radial traction exerted by lung tissue (D)Performing a maximal forced expiration (E) Increasing lung volume Increases in lung volume produce a mechanical force (i.e., radial traction) that acts on the airway walls, dilating the airways and reducing resistance. Radial traction is one of the most powerful factors that can alter airway resistance. The aging process can diminish radial traction, contributing to the higher airway resistance often seen in older individuals. Increasing vagal impulses to the lungs or administering a β-adrenergic blocking drug increases airway resistance by narrowing the airways: β-adrenergic blockers inhibit adrenergic substances (e.g., epinephrine) that act as bronchodilators, and stimulating the vagus nerve produces active contraction of bronchial smooth muscle. A forced expiration increases airway resistance, because the positive interpleural pressure compresses the large intrathoracic airways, creating a high-resistance, flow-limiting segment. Respiratory Physiology 59. Which of the following will increase as a result of stimulating cholinergic receptors on the bronchial smooth muscle? (A) Lung compliance (B) Airway diameter (C) Elastic work of breathing (D) Resistive work of breathing (E) Anatomic dead space Methacholine is a cholinergic agonist, which causes constriction of bronchial smooth muscle. Bronchoconstriction reduces airway radius, which increases airway resistance, and thus the resistive work of breathing. Methacholine-induced bronchoconstriction decreases the anatomic dead space but has no significant effect on the lung compliance, and thus does not affect the elastic work of breathing. 60. A 58-year-old woman experiences an acute exacerbation of asthma, which causes her breathing to become labored and faster. As a result, which of the following changes in airflow is expected? (A) Flow in the trachea and upper airways will become more laminar. (B) The pressure gradient required for airflow will increase. (C) The resistance to airflow will decrease. (D) The resistance to airflow will increase linearly with the decrease in airway radius (E) Reynolds number will decrease. An increased velocity of airflow will increase turbulent airflow, as predicted by an increased Reynolds number. Resistance to turbulent airflow exceeds that for laminar airflow, and thus the pressure gradient required for airflow increases when flow is turbulent. Because the velocity of airflow is greatest in the trachea and large airways, the predisposition to turbulent airflow is greater in the central than in the peripheral airways. Airway resistance varies inversely with the fourth power of airway radius, according to Poiseuille law. 61. Which of the following will decrease the oxygen consumption of the respiratory muscles? (A) A decrease in lung compliance (B) A decrease in airway resistance (C) A decrease in the diffusing capacity of the lung (D) An increase in the rate of respiration (E) An increase in tidal volume Respiratory muscles consume oxygen in proportion to the work of breathing. The work of breathing is equal to the product of the change in volume for each breath and the change in pressure necessary to overcome the resistive work of breathing and the elastic work of breathing. Resistive work includes work to overcome tissue as well as airway resistance; thus a decreased airway resistance will decrease the work of breathing Respiratory Physiology and the oxygen consumption of the respiratory muscles. A decreased lung compliance would increase the elastic work of breathing. An increase in respiratory rate or tidal volume increases the work of breathing. Ventilation 62. Which of the following formulas is correct? (A) Vital capacity = inspiratory volume + expiratory reserve volume (B) Dead air space = resting tidal volume + residual volume (C) Alveolar ventilation = (respiratory rate) × (tidal volume – dead air space) (D) Vital capacity = inspiratory reserve volume + resting tidal volume + expiratory reserve volume + residual volume (E) Inspiratory reserve volume = vital capacity – resting tidal volume Alveolar ventilation represents the amount of new fresh air that reaches the alveoli. For each inspiration it will be tidal volume minus dead space (anatomic). For alveolar ventilation per minute we must multiply by the respiratory rate. Vital capacity is the maximum tidal volume possible. It will be the tidal volume plus inspiratory reserve volume plus expiratory reserve volume. Dead space will be the volume of the airways not participating a gas exchange. Inspiratory reserve volume will be vital capacity minus resting tidal volume minus expiratory reserve volume. 63. Alveolar ventilation is equal to the… (A)Dead space ventilation (B) Tidal volume times respiratory rate (C) Minute ventilation (D)Minute ventilation minus dead space ventilation (E) CO2 production/min Alveolar ventilation equals the minute ventilation minus the dead space ventilation. Minute ventilation is the volume of gas expired per minute, which is equal to the product of tidal volume times respiratory rate. Not all of the minute ventilation reaches the gas exchange region of the lungs; some remains in the conducting system. 64. A healthy 65-year-old man with a tidal volume (TV) of 0.45 L has a breathing frequency of l6 breaths/min. His arterial PCO2 is 41 mm Hg, and the PCO2 of his expired air is 35 mm Hg. What is his alveolar ventilation? (A) 0.066 L/min (B) 0.38 L/min (C) 5.0 L/min (D) 6.14 L/min (E) 8.25 L/min Alveolar ventilation is the difference between tidal volume (TV) and dead Respiratory Physiology space multiplied by breathing frequency. TV and breathing frequency are given, but dead space must be calculated. Dead space is TV multiplied by the difference between arterial PCO2 and expired PCO2 divided by arterial PCO2. Thus: dead space = 0.45 × (41 - 35/41) =0.066 L. Alveolar ventilation is then calculated as: (0.45 L - 0.066 L) × 16 breaths/min = 6.14 L/min. 65. A fat patient scheduled for abdominal surgery is sent for preoperative evaluation and testing. His chest x-ray is normal, and pulmonary function results on room air show: Tidal volume = 600 mL PaO2 = 90 mm Hg Respiratory rate = 12/min PaCO2 = 40 mm Hg Vital capacity = 5,000 mL PECO2 = 28 mm Hg The volume of the patient’s physiological dead space, determined by applying the Bohr equation, equals which of the following? (A) 7,200 mL (B) 420 mL (C) 180 mL (D) 150 mL (E) 0.3 mL Physiological dead space is the volume of the respiratory tract that is ventilated but not perfused by the pulmonary circulation. Bohr equation for determination of the ratio of the physiologic dead space (VD) to the tidal volume (VT) is… VD/VT = PaCO2 – PECO2/PaCO2 = 40 – 28/40 = 0.3 VD/VT ×VT = VD = 0.3 × 600 mL = 180 mL Physiologic dead space volume = anatomic + alveolar dead space Anatomic dead space can be measured by Fowler technique, but is often estimated as 1 mL per pound of body weight. Because there is normally no alveolar dead space, physiologic dead space volume approximates anatomic dead space volume in persons with normal lung function. 66. A 125-lb, 40-year-old woman with a history of nasal polyps and aspirin sensitivity since childhood presents to the emergency department with status asthmaticus and hypercapnic respiratory failure. She requires immediate intubation and is placed on a mechanical ventilator on an FIO2 of 40%, a control rate of 15 breaths/min, and a tidal volume of 500 mL. Which of the following is her approximate alveolar ventilation? (A) 375 mL/min (B) 3,500 mL/min (C) 5,250 mL/min (D) 5,625 mL/min (E) 7,500 mL/min Alveolar ventilation (VA) equals the tidal volume (VT) minus the dead space volume (VD) times the breathing frequency (f). The dead space volume can be estimated as 1 mL/lb of body weight. Respiratory Physiology VA = (VT - VD) × f = (500 mL - 125 mL) × 15 breaths/min = 5,625 mL/min 67. A man breathing at a frequency of 20 breaths per minute has a minute ventilation of 8 L/min and a dead space of 150 mL. His alveolar ventilation is: (A)250 mL/min (B) 400 mL/min (C) 2,500 mL/min (D)3,000 mL/min (E) 5,000 mL/min VA = VT – VD = 8 [L/min] – 150 [mL/breath] × 20 [breath/min] = 8 – 3 [L/min] = 5,000 [mL/min]. 68. A patient is on a ventilator adjusted for an inspiratory tidal volume of 1 L at a frequency of 10 b/min. If the patient’s anatomic dead space is 200 mL and the machine’s dead space 50 mL, the patient's alveolar ventilation is: (A)10 L/min (B) 8.0 L/min (C) 7.5 L/min (D)5 L/min (E) Not determinable from the information given VA = VT – VD = (TV – Dead space) × respiratory rate = (1 [L] – 200 [mL] – 50 [mL]) × 10 [breath/min] = 7,500 [mL/min] = 7.5 [L/min]. 69. A medical student waiting to do her first patient interview at the clinical skills center becomes very anxious and increases her rate of alveolar ventilation. If her rate of CO2 production remains constant, which of the following will decrease? (A) pH (B) PaO2 (C) PaCO2 (D) V/Q (E) Alveolar-arterial PO2 difference Because the dead space air does not participate in gas exchange, the entire output of CO2 in the expired gas comes from the alveolar gas. Accordingly, alveolar (and arterial) PCO2 can be expressed in terms of CO2 output and alveolar ventilation according to the equation: PACO2 = PaCO2 = VCO2/VA. Thus, an increase in alveolar ventilation at a constant rate of carbon dioxide production will lower PACO2 and PaCO2. Hyperventilation increases PAO2 and PaO2, with no change in the alveolar-arterial PO2 difference. The V/Q will be normal or increased. Respiratory Physiology 70. Increasing the tidal volume while keeping everything else constant increases the… (A)Dead space ventilation (B) Functional residual capacity (FRC) (C) Inspiratory capacity (D)Alveolar ventilation (E) Alveolar CO2 tension If the respiratory rate, dead space, and ventilation-perfusion ratio (VA/QC) remain constant, then an increase in tidal volume raises the minute and alveolar ventilation. Because the dead space ventilation equals the dead space volume times the respiratory rate, increasing the tidal volume has no effect on the dead space ventilation. The functional residual capacity (FRC) is not altered, and the inspiratory capacity is reduced by increases in tidal volume. Alveolar CO2 tension is reduced by an increased alveolar ventilation because the increased ventilation washes out CO2 from the alveoli. 71. Which of the following could produce a decrease in alveolar ventilation with no change in total ventilation? (A) A decreased functional residual capacity (B) A decreased respiratory rate and tidal volume (C) An increased respiratory rate and decreased tidal volume (D) A decreased respiratory rate and increased tidal volume (E) An increased respiratory rate and tidal volume An increase in the respiratory rate and a decrease in tidal volume indicate a pattern of rapid shallow breathing. If the total ventilation does not change, alveolar ventilation will decrease because of the fact that the first 150 ml of each inspiration is dead-space breathing. An increase in the rate means an increase in dead-space breathing. Choice A: FRC is irrelevant; it is not a determinant of ventilation. Choice B: A decrease in the respiratory rate and tidal volume will decrease alveolar ventilation, but total ventilation will also decrease. Choice D: This situation is the reverse of choice C. Again, total ventilation must remain constant. Under these conditions a decreased rate means less dead-space breathing. Thus, alveolar ventilation must increase. Choice E: An increase in the rate and depth of breathing will increase total and alveolar ventilation. 72. The concentration of CO2 is lowest in the: (A)Anatomical dead space at end inspiration (B) Anatomical dead space at end expiration (C) Alveoli at end inspiration (D)Alveoli at end expiration (E) Blood in the pulmonary veins Respiratory Physiology Since anatomical dead space doesn’t participate in gas exchange, it has low CO2. At the end of inspiration, CO2 concentration should reach the atmospheric level. 73. The major sign of hypoventilation is… (A)Cyanosis (B) Increased airway resistance (C) Hypercapnia (D)Dyspnea (E) Hypoxia Hypercapnia is pathognomonic of hypoventilation, because the alveolar CO2 tension is determined primarily by the alveolar ventilation. Cyanosis may be present with hypoventilation, but it is a sign (and not a very good one) of hypoxia, not hypoventilation. Both an increased airway resistance and dyspnea may be symptoms of air-way disease, but neither is characteristic of hypoventilation. 74. A 62-year-old man is known to have chronic lung disease and hypercapnia. He needs a major operation to remove an intestinal tumor. To ensure that he has adequate alveolar ventilation while being anesthetized, which of the following should be available? (A)Tank of 100% O2 (B) Tank of 95% O2, 5% CO2 (C) Mechanical respirator (D)Cardiac defibrillator (E) Electrocardiograph The only treatment option that provides ventilation is the respirator. Administering supplemental O2 may correct the hypoxia, but to correct hypercapnia, the lungs must be adequately ventilated. The patient certainly does not need extra CO2, because he is hypercapnic. Neither the defibrillator nor the electrocardiograph will aid in ventilating the alveoli. 75. A reduction in local alveolar ventilation is associated with… (A)An increase in regional pulmonary blood flow (B) A decrease in regional alveolar CO2 tension (C) A decrease in regional alveolar O2 tension (D)An increase in regional tissue pH (E) An increase in capillary hemoglobin saturation A decrease in local (i.e., regional) alveolar ventilation decreases the influx of gas to that region of the lung, so that, transiently, more O2 is absorbed, and less CO2 is flushed out. Consequently, in the affected area of the lung, the alveolar O2 tension declines and the alveolar CO2 tension increases. The hypoxia, hypercapnia, and resultant local acidosis cause hypoxic pulmonary vasoconstriction (HPV), which results in a decrease in pulmonary blood flow to the affected area of the lungs. The decrease in local O2 tension reduces the hemoglobin saturation of the blood that leaves this area of the lung. These Respiratory Physiology changes represent the effects of a low ventilation–perfusion ratio (VA/QC) on gas exchange in a localized area of the lung. Alveolar-Blood Gas Exchange 76. The volume of N2 dissolved in body fluids is greatest while breathing which of the following gas mixtures? (A)Air at sea level (B) Air at an altitude of 15,000 feet (C) 20% O2, 20% N2, 60% He, while scuba diving at 2 atm of pressure (D)20% O2, 30% N2, 50% He, while scuba diving at 2 atm of pressure (E) 20% O2, 10% N2, 70% He, while scuba diving at 5 atm of pressure Among these choices, the volume of N2 dissolved in the body fluids is greatest when breathing air at sea level. Henry's law states that the volume of gas dissolved in a liquid equals the partial pressure of the gas times the solubility coefficient. Because the partial pressure of N2 at an altitude of 15,000 feet would be less than the partial pressure of N2 at sea level, the amount of N2 dissolved in the tissues also would be less. The N2 tension when breathing air at sea level is 0.79 atm. Gas equilibration in the body requires approximately 12 hours after any change in pressure and occurs at different rates in different tissues. For N2, equilibration takes the longest in the fatty tissues because of the high N2 solubility and the low blood flow to this type of tissue. Scuba diving at 2 atm while breathing a gas with 20% N2 provides 0.4 atm of N2 tension. The other two scuba conditions yield N2 tensions less than 0.79 atm as well. 77. Which of the following statements regarding the fraction of O2 in inspired (tracheal) gas is true? (A)It equals 0.25 at sea level (B) It decreases as a function of altitude (C) It varies as a function of the weather (D)It is less than the fraction of O2 in the atmosphere (E) It equals the fraction of O2 in the alveoli The fraction of O2 in inspired gas is less than the fraction of O2 in the atmosphere, because nasal breathing adds water vapor to inspired air, which decreases the O2 content of the air by the time it reaches the trachea. The fraction of O2 in the air is constant from sea level to several hundred thousand feet altitude and equals 0.21. However, the O2 tension decreases with increased altitude, because the total pressure declines as one ascends. The partial pressure of any gas is given by the product of the mole fraction of the gas and the total or barometric pressure. Alveolar gas is diluted by the addition of CO2 from the blood; so that the fraction of O2 in the alveoli is less than that in the trachea. Respiratory Physiology 78. The water vapor pressure of alveolar gas at a barometric pressure of 380 mm Hg is: (Assume all other parameters are same as at sea level.) (A)23.5 mm Hg (B) 47.0 mm Hg (C) 76.0 mm Hg (D)94.0 mm Hg (E) 105.0 mm Hg The water vapor pressure is temperature dependent only. 79. Which one of the following statements regarding the CO2 tension in mixed expired gas is true? (A)It is greater than the alveolar CO2 tension (B) It is less than the alveolar CO2 tension (C) It is equal to the alveolar CO2 tension (D)It is equal to the atmospheric CO2 tension (E) It is greater than the CO2 tension in venous blood Mixed expired gas has a lower CO2 tension than alveolar gas because it is a mixture of alveolar and dead space gas. The composition of this gas varies depending on the ratio of dead space ventilation to alveolar ventilation. This fact can be used to determine the dead space-tidal volume ratio: VD/VT = 1 – PEco2/PAco2, where VD/VT = dead space-tidal volume ratio; PEco2 = CO2 tension of mixed, expired gas; and PAco2 = CO2 tension of alveolar gas. The CO2 tension in venous blood is higher than that in alveolar gas, which is why CO2 diffuses from the pulmonary capillaries into the alveoli. 80. The alveolar PO2 of an individual breathing 30% O2 at an atmospheric pressure of 747 mm Hg will be (in mm Hg): (assume R = 1.0 and PACO2 = 40 mm Hg) (A) 224 (B) 210 (C) 170 (D) 164 (E) 100 The calculation involves the alveolar PO2 equation and the appropriate values will be: PAO2 = (Patm – PH2O) × FIO2 – (PACO2/R) = (747 – 47) × 0.30 – (40/1.0) = 170 mm Hg Respiratory Physiology 81. A 56-year-old man presents to the emergency department with severe abdominal pain and a temperature of 103°F The patient is in severe respiratory distress. Moderate amounts of pulmonary edema fluid are aspirated during suctioning. The patient is placed on a ventilator with an FIO2 of 0.5 and an arterial blood gas sample reveals a PO2 of 160 mm Hg and a PCO2 of 40 mm Hg. His alveolar oxygen tension, at a barometric pressure of 747 mm Hg and a respiratory exchange ratio (R) of 0.8, is approximately what? (A) 100 mm Hg (B) 200 mm Hg (C) 300 mm Hg (D) 400 mm Hg (E) 500 mm Hg The alveolar oxygen tension is calculated using the modified alveolar gas equation: PAO2 = PIO2 – PaCO2/R = [0.5 × (747 - 47)] – (40/0.8) = 300 mm Hg 82. A 36-year-old man with a history of AIDS and Pneumocystis infection presents to the emergency department with severe respiratory distress. The patient is placed on a ventilator at a rate of 16, tidal volume of 600 mL, and FIO2 of 1.0. An arterial blood sample taken 20 minutes later reveals a PO2 of 350 mm Hg, a PCO2 of 36 mm Hg, and a pH of 7.32. At a barometric pressure of 757 mm Hg, and assuming a normal respiratory exchange ratio (R) of 0.8, the patient’s alveolar oxygen tension is approximately which of the following? (A) 105 mm Hg (B) 355 mm Hg (C) 576 mm Hg (D) 665 mm Hg (E) 712 mm Hg The alveolar air equation is used to calculate the PaO2. PAO2 = PIO2 - (PaCO2/R) = (1.0)(757 - 47) - (36/0.8) = 710 – 45 = 665 mm Hg 83. If alveolar PCO2 was originally 40 mm Hg but body temperature increased and CO2 production doubled while no change occurred in alveolar ventilation, what decrease should occur in alveolar PO2? (Assume R = 1.0) (A) 10 mm Hg (B) 20 mm Hg (C) 30 mm Hg (D) 40 mm Hg (E) No change If CO2 production doubled, the amount of CO2 entering the alveoli from pulmonary capillary blood would also double. If alveolar ventilation doubled, alveolar PCO2 would stay at 40 mm Hg. If alveolar ventilation did not change, alveolar PCO2 would go from 40 to 80 mm Hg. Since PACO2 affects PAO2, the PAO2 will also change. An increase in PACO2 will cause approximately the same decease in PAO2. Therefore, if PACO2 increases by 40 mm Hg, PAO2 will decrease by 40 mm Hg. Respiratory Physiology 84. An individual’s inspired PO2 was 150 mm Hg and his alveolar PCO2 was 40 mm Hg. If this person’s alveolar ventilation then doubled, his alveolar PO2 would be expected to change by: (assume a new steady state and an R value of 1.0) (A) 20 mm Hg (B) 25 mm Hg (C) 40 mm Hg (D) 50 mm Hg (E) No change An inspired PO2 of 150 mm Hg and an alveolar PCO2 of 40 mm Hg is normal. If this individual’s alveolar ventilation doubles (hyperventilation), alveolar PCO2 would be cut in half to 20 mm Hg. lf the alveolar PCO2 decreases by 20 mm Hg, alveolar PO2 would increase by 20 mm Hg. 85. Arterial PO2 is measured under 5 different conditions. The one you would expect to produce the lowest PaO2 value is the when the individual: (A)Has just completed 15 minutes of strenuous exercise (B) Has spent 10 minutes in a pressure chamber which stimulates an altitude of 16,000 feet (4900 meters) (C) Has a 15% reduction in pulmonary blood flow due to a decreased heart rate (D)Has been in an environmental chamber for 5 minutes in which the temperature is 100°F (38°C) and the relative humidity 95% (E) Has a minute ventilation of 9.0 liters per minute and a cardiac output of 5.0 liters per minute PaO2 doesn’t decrease in a healthy subject with exercise. Increasing ventilation or decreasing perfusion to the lung (high V/Q ratio) without (regional) V/Q mismatch, will not cause decrease in PaO2. Such a subtle change in temperature and humidity will not apply partial pressure of water more than 300 mm Hg, thus, acclimatization to the altitude of 16,000 feet decreases PaO2 more. Respiratory Physiology 86. A 28-year-old man is admitted to the emergency department multiple fractures suffered in a car accident. Arterial blood gases are ordered while the patient is breathing room air. After obtaining the arterial blood sample, the blood-gas technician draws room air into the syringe before measuring the blood-gas values. How does exposure to room air affect the measured values of PaO2 and PaCO2? (A) The measured values of both PaO2 and PaCO2 will be higher than the patient’s actual values. (B) The measured values of both PaO2 and PaCO2 will be lower than the patient’s actual values. (C) The measured PaO2 will be higher and the measured PaCO2 will be lower than the patient’s actual blood gas values. (D) The measured PaO2 will be lower and the measured PaCO2 will be higher than the patient’s actual blood gas values. (E) The measured values of PaO2 and PaCO2 will accurately reflect the actual values. Room air contains 21% O2 and 0.04% CO2, yielding a PIO2 of 160 mm Hg and a PICO2 of 0.3 mm Hg. Thus, if a sample of arterial blood is equilibrated with room air, the measured PaO2 will have an inaccurately high reading and the PaCO2 will have an inaccurately low reading. Alveolar-Blood Gas Transfer/Diffusion 87. A series of gas mixtures is inhaled by a healthy subject. Which one of the following gases would diffuse most slowly from the lungs into the blood? (A) CO2 at PCO2 of 60 mm Hg (B) CO at a PCO of 0.5 mm Hg (C) O2 at a PO2 of 130 mm Hg (D) O2 at a PO2 of 150 mm Hg The factors that affect the rate of gas diffusion are all included in the following equation: Vgas = A/T × D × (P1 – P2) Since we are dealing with the same lung, A (surface area) and T (thickness) will be constant for each gas. Therefore the rate at which each gas diffuses will depend upon its solubility and the partial pressure difference across the alveolar membrane (P1 – P2). CO2 is a very soluble gas and diffuses quickly. The remainders are less soluble, and relative diffusion rates will be determined by the partial pressure gradients. The PCO of capillary blood is about zero and if the PACO is 0.5 mm Hg, the gradient will be only 0.5 mm Hg, a very small gradient. Therefore, CO will be diffusing very slowly across the membrane. On the other hand, the gradients for oxygen will be much greater, thus oxygen will be diffusing much faster than CO. Respiratory Physiology 88. The diffusion coefficient of O2, as compared with that of CO2, is… (A)Greater because O2 combines with hemoglobin (B) Less because O2 is less soluble (C) Greater because of a higher pressure gradient (D)Less because of the lower molecular weight of O2 (E) Essentially the same O2 is much less diffusible than CO2 in the lungs. The diffusion coefficient concerns the movement of molecules in solution and is determined by the molecular weight and the solubility of the substance. O2 has a lower molecular weight than CO2, but is also about 25 times less soluble. The increased diffusibility of CO2 is important because there is a gradient of only approximately 5 mm Hg to cause CO2 to diffuse from the pulmonary capillary blood to the alveoli. 89. Which of the following would be expected to decrease the rate of O2 diffusion across the alveolar-capillary membrane of the lung? (A) A decrease in PO2 difference between the alveolus and pulmonary capillary blood (B) An increase in the surface area of the alveolar-capillary membrane (C) An increase in the thickness of the alveolar-capillary membrane (D) A decrease in O2 solubility in the alveolar membrane The factors that affect the rate of oxygen diffusion are in the following equation: Vgas = A/T × D × (P1 – P2) A decrease in the PO2 difference across the membranes (P1 – P2) will slow oxygen diffusion. An increase in the surface area will increase the rate of diffusion for all gases. Diffusion is inversely related to membrane thickness; thus an increase in membrane thickness will slow diffusion. A decrease in solubility, the main factor determining “D” will also slow diffusion. 90. A subject inspires a mixture of gases containing CO and holds his breath for 10 seconds. It is calculated that during the 10 seconds when the subject held his breath, the alveolar PCO is 0.5 mm Hg, and the CO uptake is 25 ml/min. What is the diffusing capacity for CO (DL)? (DL is uptake of CO in ml/min/mm Hg.) (A) 12.5 (B) 50 (C) 125 (D) 250 (E) 500 The diffusing capacity is the uptake of CO in specific units: ml/min/mm Hg. Given that the uptake is 25 ml/min, we need simply divide by the partial pressure of CO in the alveoli (0.5 mm Hg) to obtain the appropriate units. Therefore, DLCO = 25 [ml/min] / 0.5 [mm Hg] = 50 [ml/min/mm Hg] Respiratory Physiology Alveolar-Arterial O2 Gradient 91. A 68-year-old man who has chronic obstructive pulmonary disease (COPD) presents to his pulmonologist with fatigue, dyspnea at rest, and peripheral edema. His blood gases on room air are PaO2= 60 mm Hg, PaCO2 = 60 mm Hg, and pH = 7.36. His alveolar-arterial (A-a) O2 gradient, at a barometric pressure of 760 mm Hg and a respiratory exchange ratio (R) of 0.8, is approximately what? (A) 5 mmHg (B) 10 mm Hg (C) 15 mmHg (D) 20 mm Hg (E) 25 mmHg The A-a O2 gradient is the partial pressure difference between the alveolar gas and arterial blood. The Pao2 has been measured. The alveolar oxygen tension must be calculated using the modified alveolar gas equation PAO2 = PIO2 -PaCO2/R = [0.21 × (760 - 47)] – (60/0.8) = 75 mm Hg (A-a) O2 gradient = PAO2 – PaO2 = 75 mm Hg – 60 mm Hg = 15 mm Hg The patient’s low arterial oxygen tension (hypoxemia; hypoxic hypoxia) results from a low PAO2 due to hypoventilation (as evidenced by the elevated PaCO2 and thus the (A-a) O2 gradient is within the normal range. 92. A patient presents to you in the emergency department with a history of progressive respiratory distress. You obtain an arterial blood gas (ABG) analysis while the patient is breathing room air that shows the following: PaO2 = 65, SaO2 = 0.90, PaCO2 = 50, pH = 7.30. The patient's temperature is 37 degrees C, barometric pressure is 760 mm Hg, Water vapor pressure at body temperature is 47 mm Hg, the respiratory quotient is 0.8. What is the patient's alveolar-arterial oxygen tension gradient; P(A-a)O2? (A)15 mm Hg (B) 22 mm Hg (C) 85 mm Hg (D)95 mm Hg (E) 35 mm Hg PAO2 = PIO2 – PaCO2/R = (PB – PIH2O) × FIO2 – PaCO2/R = (760 – 47) × 0.21 – 50/0.8 = 87.23 mm Hg. Therefore, A-a gradient is 87.23 – 65 = 22.23 mm Hg. 93. Which person would be expected to have the largest A-a gradient? (A) Person with pulmonary fibrosis (B) Person who is hypoventilating due to morphine overdose (C) Person at 12,000 feet above sea level (D) Person with normal lungs breathing 50% O2 (E) Person with normal lungs breathing 100% O2 Increased A-a gradient signifies lack of O2 equilibration between alveolar gas Respiratory Physiology (A) and systemic arterial blood (a). In pulmonary fibrosis, there is thickening of the alveolar/pulmonary capillary barrier and increased diffusion distance for O2, which results in lack of equilibration of O2, hypoxemia, and increased A-a gradient. Hypoventilation and ascent to 12,000 feet also cause hypoxemia, because systemic arterial blood is equilibrated with a lower alveolar PO2 (normal A-a gradient). Persons breathing 50% or 100% O2 will have elevated alveolar PO2, and their arterial Po2 will equilibrate with this higher value (normal A-a gradient). 94. Which of the following causes of hypoxia is characterized by a decreased arterial PO2 and an increased A-a gradient? (A) Hypoventilation (B) Right-to-left cardiac shunt (C) Anemia (D) Carbon monoxide poisoning (E) Ascent to high altitude Hypoxia is defined as decreased O2 delivery to the tissues. It occurs as a result of decreased blood flow or decreased O2 content of the blood. Decreased O2 content of the blood is caused by decreased hemoglobin concentration (anemia), decreased O2-binding capacity of hemoglobin (carbon monoxide poisoning), or decreased arterial PO2 (hypoxemia). Hypoventilation, right-to-left cardiac shunt, and ascent to high altitude all cause hypoxia by decreasing arterial PO2. Of these, only right-to-left cardiac shunt is associated with an increased A-a gradient, reflecting a lack of O2 equilibration between alveolar gas and systemic arterial blood. In right-to-left shunt, a portion of the right heart output, or pulmonary blood flow is not oxygenated in the lungs and thereby “dilutes” the PO2 of the normally oxygenated blood. With hypoventilation and ascent to high altitude, both alveolar and arterial PO2 are decreased, but the A-a gradient is normal. Oxygen, Carbon Dioxide Transport (Hemoglobins) Use below diagram for next two questions A B Respiratory Physiology 95. In the hemoglobin-O2 dissociation curves shown above, the shift from curve A to curve B could be caused by (A) Increased pH (B) Decreased 2,3-diphosphoglycerate (DPG) concentration (C) Strenuous exercise (D) Fetal hemoglobin (HbF) (E) Carbon monoxide (CO) poisoning Strenuous exercise increases the temperature and decreases the pH of skeletal muscle; both effects would cause the hemoglobin-O2 dissociation curve to shift to the right, making it easier to unload O2 in the tissues to meet the high demand of the exercising muscle. 2,3-Diphosphoglycerate (DPG) binds to the β chains of adult hemoglobin and reduces its affinity for O2, shifting the curve to the right. In fetal hemoglobin, the β chains are replaced by γ chains, which do not bind 2,3-DPG, so the curve is shifted to the left. Because carbon monoxide (CO) increases the affinity of the remaining binding sites for O2, the curve is shifted to the left. 96. The shift from curve A to curve B is associated with (A) Increased P50 (B) Increased affinity of hemoglobin for O2 (C) Impaired ability to unload O2 in the tissues (D) Increased O2-carrying capacity of hemoglobin (E) Decreased O2-carrying capacity of hemoglobin A shift to the right of the hemoglobin-O2 dissociation curve represents decreased affinity of hemoglobin for O2. At any given PO2, the percent saturation is decreased, the P50 is increased (read the PO2 from the graph at 50% hemoglobin saturation), and unloading of O2 in the tissues is facilitated. The O2-carrying capacity is determined by the hemoglobin concentration and is unaffected by the shift from curve A to curve B. Respiratory Physiology 97. In the below figure, if curve N represents the oxygen-Hb dissociation curve of a normal individual, then curve A represents: (A) Polycythemia and B represents anemia (B) Anemia and B represents polycythemia (C) Anemia and B represents carbon monoxide poisoning (D) Carbon monoxide poisoning and B represents anemia (E) Carbon monoxide poisoning and B represents polycythemia Curve N and curve B have the same P50, therefore the Hb has the same affinity for oxygen. However, carrying capacity is reduced in B. This curve fits anemia where there is normal Hb but the concentration is below normal. In curve A the carrying capacity is reduced and the P50 is also reduced. A reduced P50 means the Hb has a greater affinity for oxygen and a lower PO2 produces 50% saturation. The combination of a reduced carrying capacity but increased affinity is consistent with carbon monoxide poisoning. Carbon monoxide molecules attached to Hb make these sites unavailable to oxygen and because of cooperative binding, and also the remaining sites with oxygen have greater affinity. Polycythemia would be characterized as having a normal P50 but a greater than normal carrying capacity. 98. Which of the following best represents the systemic arterial blood of an individual with anemia? (A) Low PO2, low hemoglobin, normal O2 content (B) Low PO2, low hemoglobin, low O2 content (C) Normal PO2, low hemoglobin, low O2 content (D) Normal PO2, normal hemoglobin, low O2 content (E) Low PO2, normal hemoglobin, low O2 content The characteristic feature of anemia is a low Hb concentration but the affinity for oxygen is normal. Because alveolar PO2 is still 100 mm Hg and equilibration still Curves N and B have the same P50 Curve A has a lower P50 A B N PO2 O2 volume % Respiratory Physiology occurs with pulmonary capillary blood, systemic arterial Hb is fully saturated and the plasma has a PO2 of 100 mm Hg. Remember that blood PO2 is determined by dissolved oxygen. The systemic arterial oxygen content is decreased because of the low concentration of Hb, dissolved oxygen is normal. 99. Which of the following best characterizes the systemic arterial blood of an individual suffering from carbon monoxide poisoning? (A) Low [Hb], low O2 content, low PO2 (B) Low [Hb], normal O2 content, low PO2 (C) Low [Hb], low O2 content, normal PO2 (D) Normal [Hb], low O2 content, low PO2 (E) Normal [Hb], low O2 content normal PO2 In carbon monoxide poisoning, Hb cannot be fully saturated with oxygen because some sites are occupied by carbon monoxide. Therefore, even though Hb concentration is normal (acute poisoning), the oxygen content is depressed because of the reduced oxygen saturation. As long as room air is inspired (21% O2) alveolar PO2 and systemic arterial PO2 are normal (depends on dissolved oxygen). An important point is that in an individual with carbon monoxide poisoning and breathing room air, systemic arterial PO2 should be normal. 100. A decrease in blood pH will displace the hemoglobin dissociation curve to the: (A) Right and reduce O2 carrying capacity (B) Right with no change in O2 carrying capacity (C) Left and reduce O2 carrying capacity (D) Left with no change in O2 carrying capacity [Show More]
Last updated: 2 years ago
Preview 1 out of 99 pages
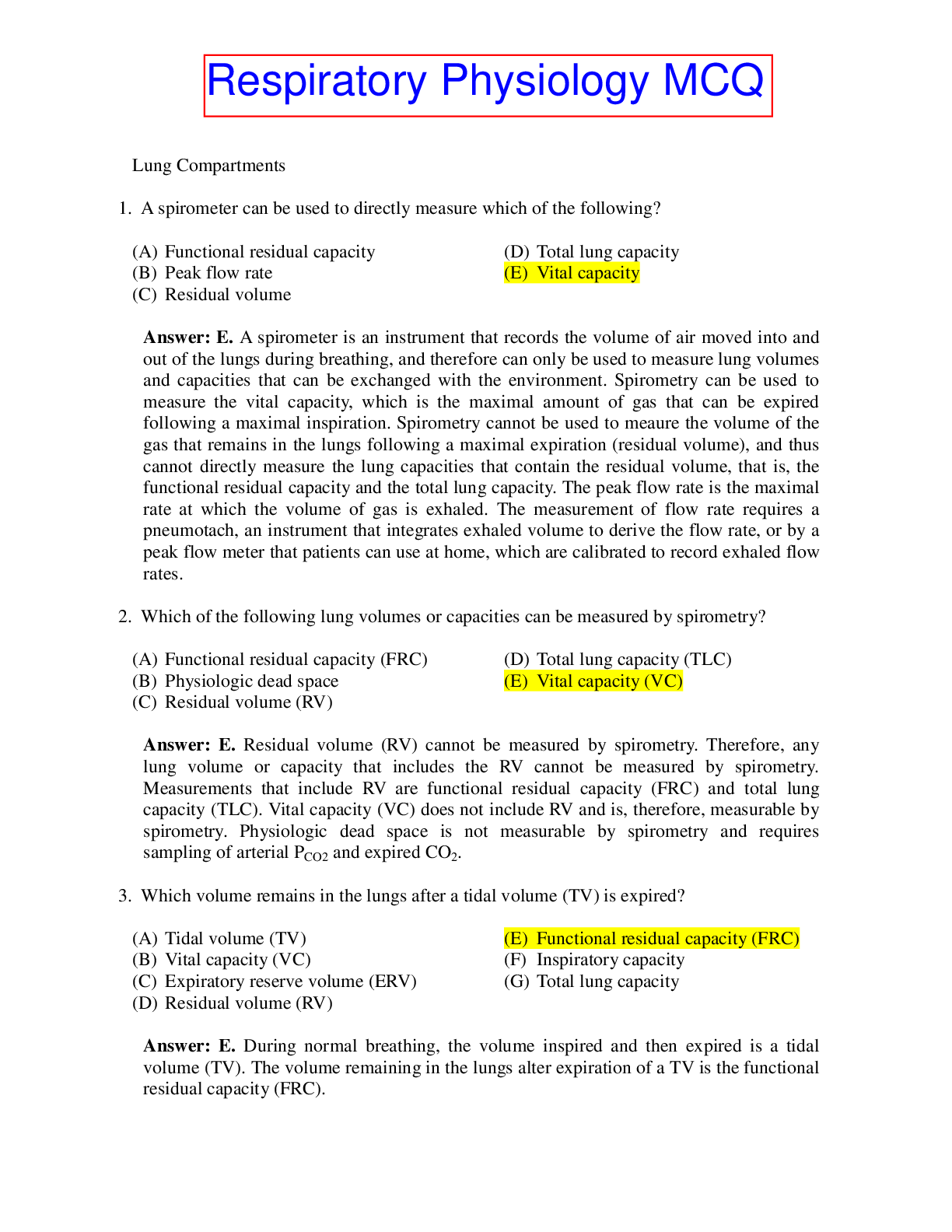
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
May 05, 2021
Number of pages
99
Written in
Additional information
This document has been written for:
Uploaded
May 05, 2021
Downloads
0
Views
360






.png)
.png)
.png)
.png)
.png)
.png)
.png)

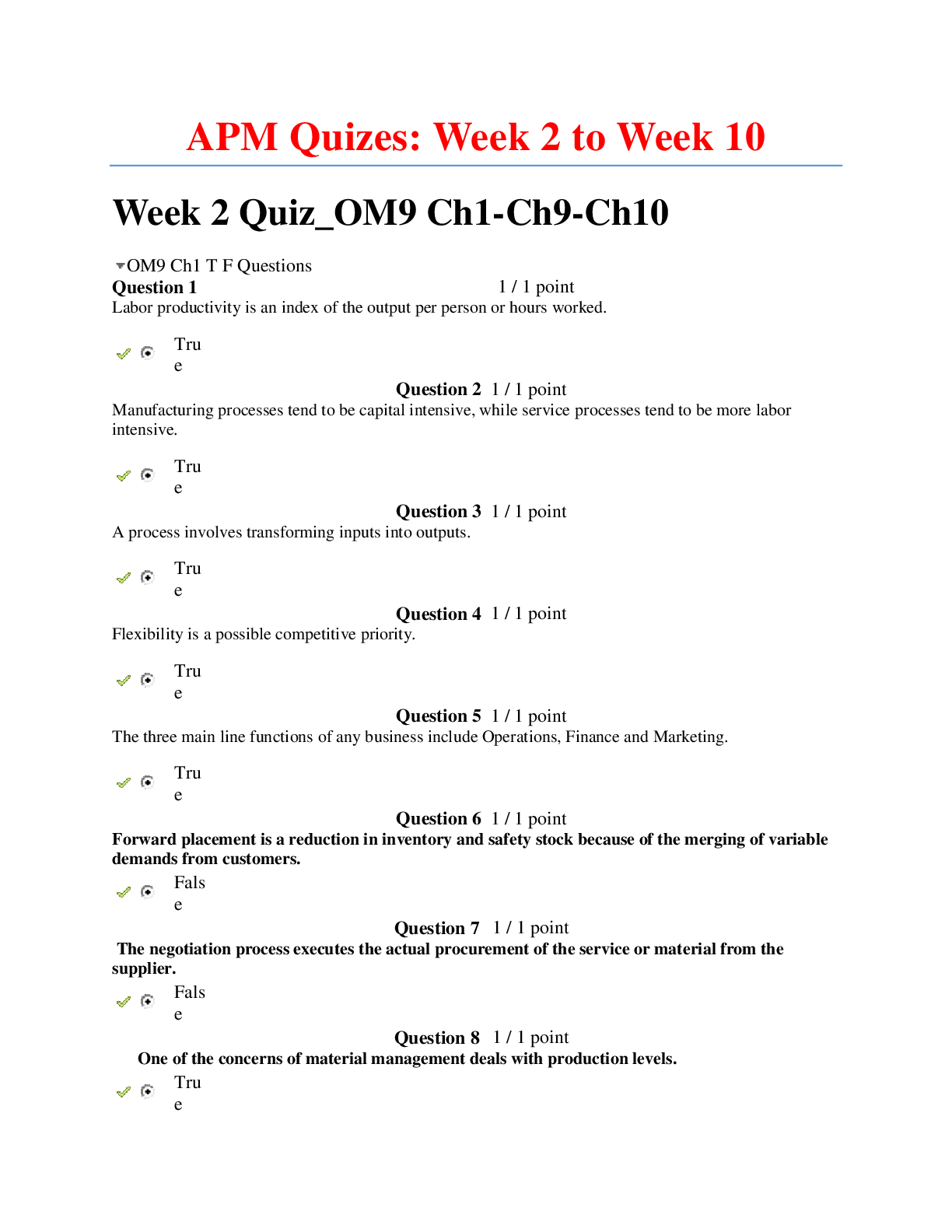
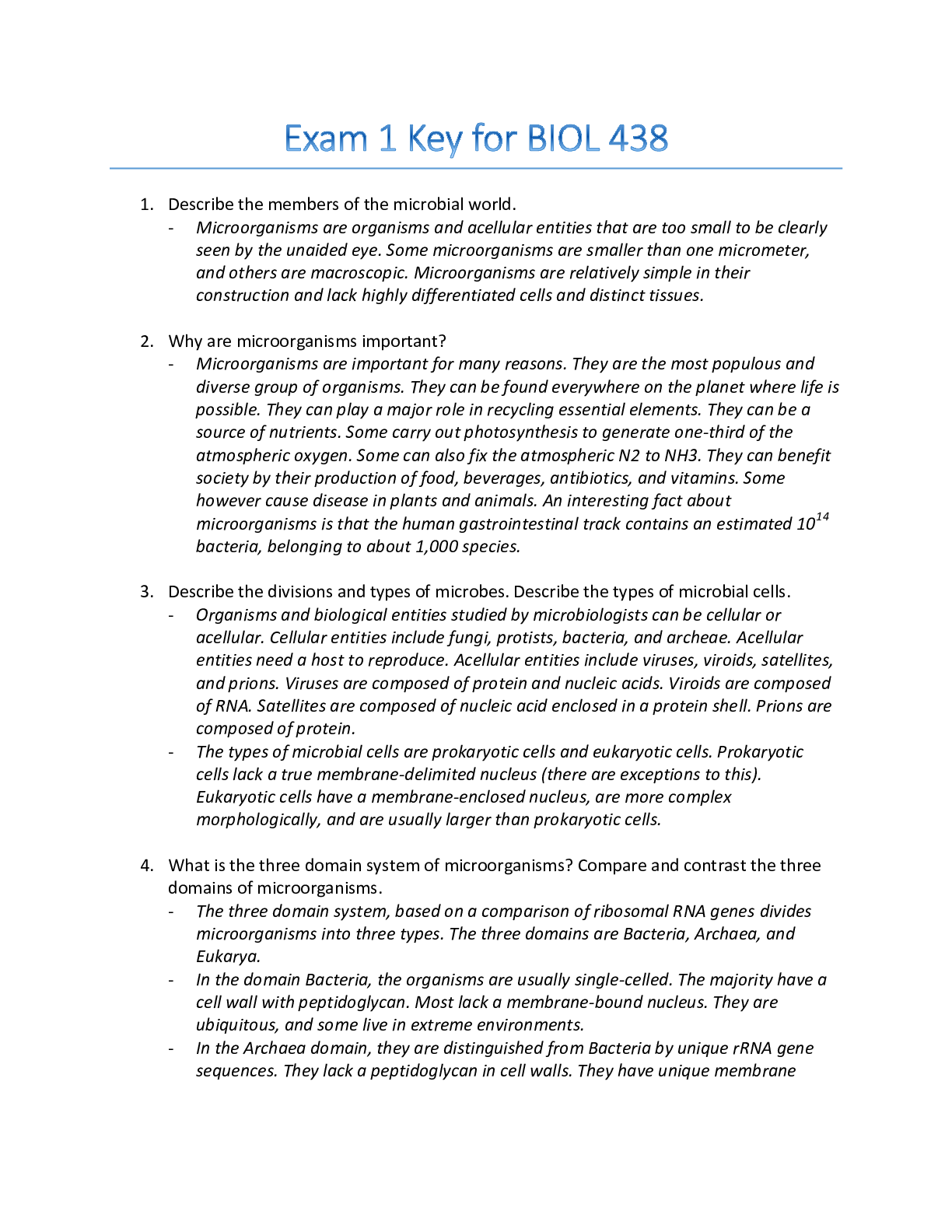


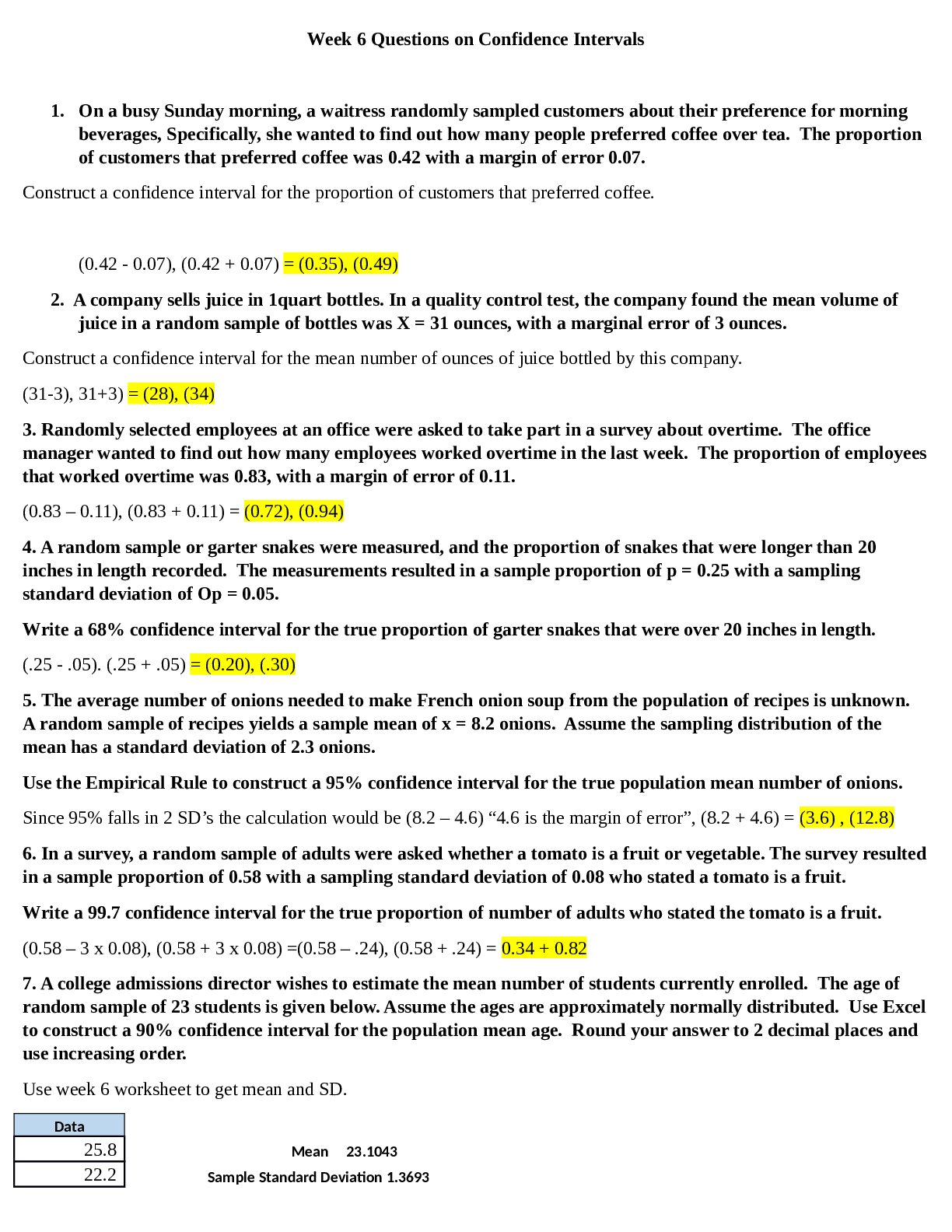

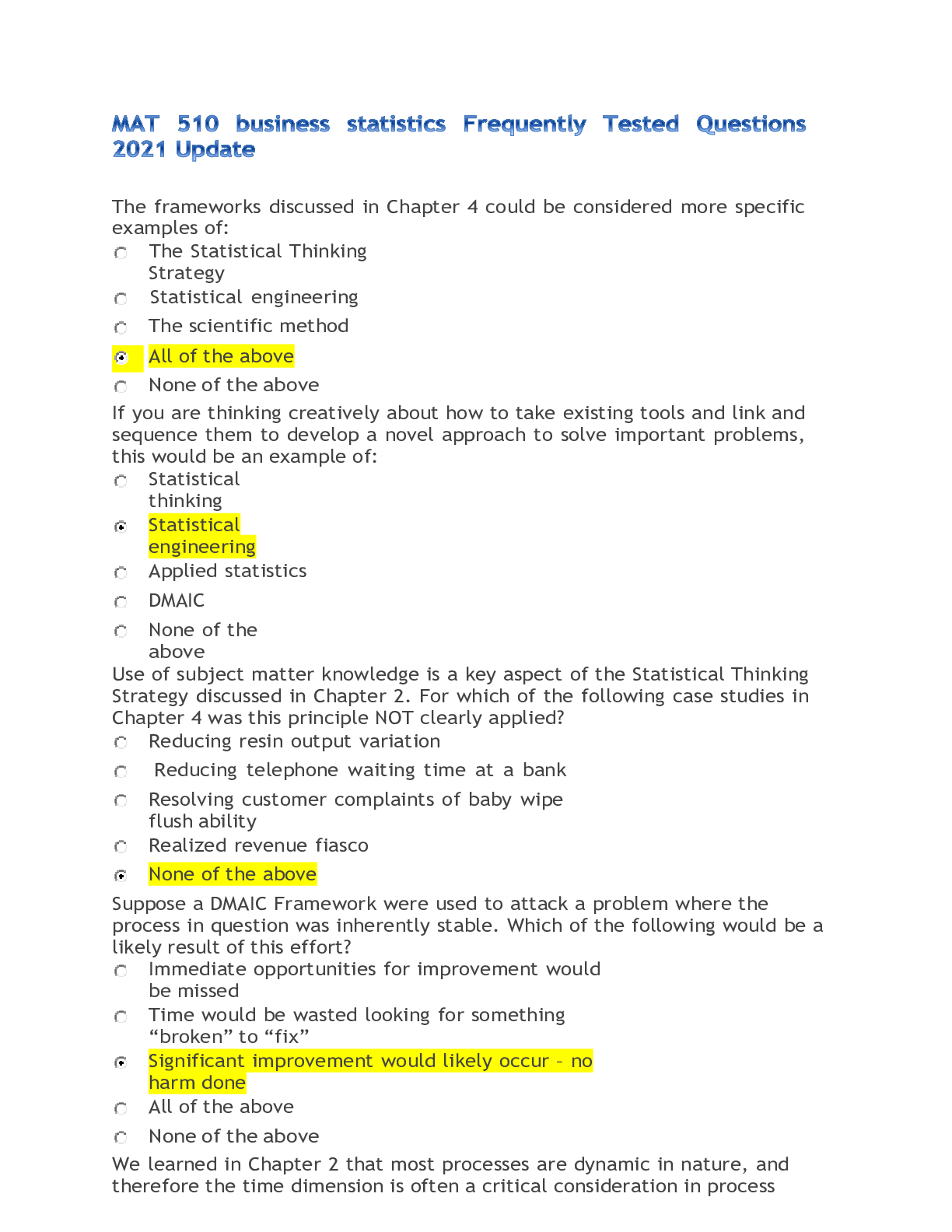



.png)

