*NURSING > EXAM REVIEW > MED SURGICAL TAH 2-EXAM 2 Adult Health 2 - Exam 2 (All)
MED SURGICAL TAH 2-EXAM 2 Adult Health 2 - Exam 2
Document Content and Description Below
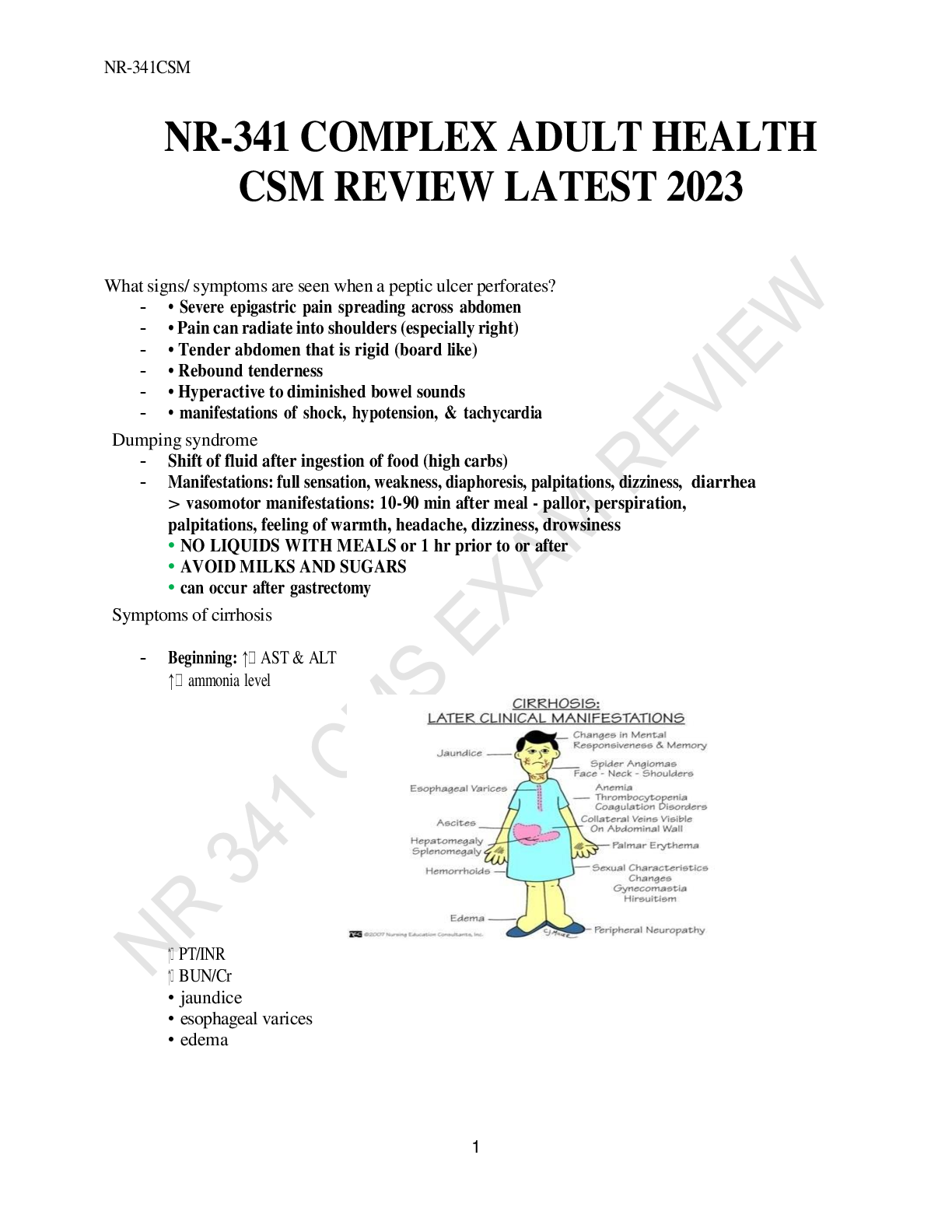
MED SURGICAL TAH 2-EXAM 2 Adult Health 2 - Exam 2 Notes from 1/30 (study guide) ● Pulmonary embolism ○ S&S: new onset sharp pain, SOB, O2 desat, high blood pressure initially and then hypoten... sion ○ Ask the patients when the pain started, hx of DVT, smoking, birth control, long distance traveling, post surgical ○ Commonly comes from lower extremity DVT ○ Saddle PE: ends up in pulmonary artery and affects both lungs ○ Intervention: ■ First: O2 simple mask or nonrebreather ■ Treatment: Give heparin, injectable( lovenox or a heparin drip), pain management opioid narcotic ■ Ambulation doesn't work, no ted stocking or SCDs ■ Vital signs: high blood pressure initially because of fight or flight response, tachycardia, decreased O2 sat and then hypotension ■ Keep O2 sat >92% or above ○ Pulmonary artery PE is the most deadly - Can lead to right sided heart failure and cardiogenic shock - Surgical procedure: embolectomy or IVC filter - Anticoagulation therapy for life - Diagnostic: D-Dimer shows if you have a clot by presence of fibrin degradation products ○ VQ scan( Ventilation and perfusion): measures balance and match with ventilation and blood getting to the alveoli; will see a lack of perfusion ■ Blockage in alveoli or blockage in the lungs, inflammatory ■ Give an inhaled isotope, to see if the lungs are being ventilated ■ Also give an isotope in the vein shows perfusion ○ Ventilation and perfusion for O2 exchange to happen○ All of the shocks play a part in perfusion ○ STAT chest x ray and coag studies for future use of heparin –lovanox (80-100mg) enoxaparin ○ Flail chest ● Pneumothorax ○ Types: hemothorax, pneumothorax closed or open, and chylothorax ■ Tall skinny males are more likely to get closed pneumothorax ○ Closed pneumothorax: blunt trauma ○ Open pneumothorax: stabbings, gsw, (opening from inside to outside causing negative pressure and air gets inside) ■ Low O2 sat, SOB, dyspnea, pallor ■ Concerned about the heart because it pushes on the heart and decompresses the vessels ■ Cardiogenic shock ■ Anoxic brain injury ○ Chest tube system ■ Collection chamber ■ Water seal valve ■ Suction control ■ Indications: status post cabbage, chest trauma ■ Not used for atelectasis because its in a different space ○ Tension pneumothorax: tracheal deviation and goes to the non affected side, low BP because of poor pre load ● Ventilatory and respiratory failure ○ Acute respiratory distress syndrome (ARDS): brain stem injury or stroke, coronary artery bypass graft, pulmonary edema ○ Causes in the hospital setting: Opioids or benzos ● Chest tube ○ Patient pulls chest tube out, what do you need to do? Cover opening with 3 sided dressing and tape ● Acute/chronic kidney injury ○ Pre renal, intra renal and post renal cause for renal failure■ Pre renal: DM, shock, weak LV function, HF, cardiomyopathy, MI ■ Intra renal: Stones, polycystic kidney, nephrotoxic drugs ● Nephrotoxic drugs: NSAIDS and “mycin” antibiotics - cause vessels to vasoconstrict and inhibit prostaglandins ■ Post renal: BPH or stones ● Kidney disease ○ They make pee, excrete waste products: Pollutants, nitrogenous wastes and chemicals ○ Nitrogenous wastes: Blood urea and creatinine are excreted through the kidneys every day. ○ Kidneys shut down, BUN & creatinine go up, GFR decreases ○ Control your electrolytes ○ Acid base regulation: dumping of hydrogen ions and bicarb ○ If kidneys are not working properly they hang on to hydrogen, making more acidic ○ Kusmales, collecting CO2 ○ Controls water, ADH(2O), pulls water to control blood pressure with RAAS ■ Aldosterone helps by returning salt to the renal tubes ○ Regulation of RBC by epoetin and goes to bone marrow and makes RBC ○ Fluid restriction on patients with kidney problems, how do you know they're fluid overloaded? Crackle lung sounds ○ Vascular catheter - hemodialysis ■ Double lumen, with a red and blue connection ■ Inject heparin after dialysis treatment so it doesn't clot off ■ Fistula or AV (arterial venous) ○ Monitor fluids and electrolytes ○ Monitor potassium and place on cardiac monitor ○ With AV fistula you are assessing thrill and bruit ■ If they don’t have the thrill or bruit call the provider ○ Renal failure ■ Electrolyte imbalance, Hyperkalemia , Acidosis ,Kusmales■ Give them fluids ● Kidney infection (Pyelonephritis ) ○ Women most commonly get it because urethra is short ■ High temp ■ Flank pain ■ Treatment: IV, antibiotics and blood cultures x2 from separate arms in case one is infected with staph ■ Percocet for pain and fever reduction ■ Can't give Tylenol before blood cultures because it scues the results ■ Can cause renal failure because of damage of structure ■ Education; pee after sex, wipe from front to back and drink a lot of water ● Ventilators ○ Intubated pts, acute respiratory failure, brain stem injury, stroke, COPD, ○ Pressure limit 10 - 20 cm of water above peak inspiratory pressure in order to get good ventilation ○ Ventilator setting for patient who needs full ventilator support: AC ( Assist control) highest level of control ○ Peep ventilation: Keep alveoli open by preventing collapse when inhaled , treating atelectasis - If patient has atelectasis give O2 and IS Meds: Fentalyn and versed and vecuronium ● Glomerulonephritis ○ Strep A causes this ○ Take urine culture, GFR, BUN and creatinine ○ GFR monitors rate of filtration ○ Complexes get irritated secondary to strep ● Dialysis ○ Hemodialysis and peritoneal ○ Peritoneal dialysis; specific concentration for each patient ○ Cloudy effluent: infection can cause peritonitis and possibly develop sepsis if not treated○ Fluid is in peritoneal sac is known as indwelling ○ Dialysate should be a specific color ○ Concern for peritonitis due to copper catheter inserted - Signs and symptoms of shock - Pain ● Tracheostomy ○ You are creating an airway ○ 20 ml of air in the cuff, blow up to prevent necrosis ● Nephrotic syndrome ○ Results of repeat pyelonephritis, DM, nephrotoxic med, glomerulo, ○ Too much protein; protein channels dilute and proteins flow out of the channels and go to the body causing edema ○ Generalized edema: Anasarca ● Kidney transplants ○ Corticosteroids, antirejection, immunosuppressants ○ Corticosteroids cause immunosuppression and hyperglycemia ● Laryngeal cancer ○ Need tracheostomy ○ Hoarseness ○ Hemorrhage / swelling ○ Speech and language therapy ○ Airway and ventilation problems ● Acute respiratory failure ○ PAO2 <60 from ABG (partial) ○ SAO2 found in pulse ox <90 ○ PACO2 found in blood gas >50 ; more CO2 more acidic, Ph is low ○ PH is < 7.3 ● Flail chest ○ Broken ribs ○ Weakened area ○ No support○ Paradoxical chest movement: inspiration you breath in and expiration you breath out ○ Study guide she sent us Apply your Medical Surgical Mantra to these disease processes. I will let you know if I need to modify this guide. Selected Disorders (Respiratory): Thoracic Surgery Chest tube Insertion and Monitoring Head and neck cancer ● Cancer of the larynx ○ Accounts for approximately half of all head and neck cancers ○ 13,560 new cases and 3640 deaths annually ○ Most common in people over age 65 ○ Four times more common in men ○ Risk factors: refer to Chart 22-6 ● Signs and symptoms ○ Early ■ Hoarseness ■ Persistent cough ■ Sore throat or pain burning in throat ■ Raspy voice, lower pitch ■ Lump in neck ○ Later ■ Dysphagia, dyspnea ■ Nasal obstruction ■ Persistent hoarseness ■ Persistent ulceration■ Foul breath ■ General debilitation ● Medical diagnostics ○ History and physical ○ Laryngoscopy ○ FNA biopsy ○ Barium swallow study ○ Endoscopy, CT, MRI, PET scan ○ Tumors grade and stage by TNM system ● Medical management of laryngeal cancer ○ Stage 1 and 2 ■ Radiation therapy ■ Cordectomy ■ Endoscopic laser excision ■ Partial laryngectomy ○ Stage 3 and 4 ■ Radiation therapy ■ Chemotherapy ■ Chemoradiation ■ Total laryngectomy ● Nursing process: Assessment ○ Health history ○ Physical, psychosocial, and spiritual assessment ○ Nutrition, BMI, albumin, glucose, electrolytes ○ Literacy, hearing, and vision; may impact communication after surgery ○ Coping skills and available support systems for patient and family after surgery ● Nursing process: Diagnoses ○ Knowledge deficit about surgical procedure ○ Anxiety relating to diagnosis ○ Ineffective airway clearance ○ Impaired verbal communication ○ Imbalanced nutrition ○ Disturbed body image○ Self-care deficit ● Postoperative nursing care ○ Reduce anxiety ○ Maintain patent airway, control secretions ○ Support alternative communication ○ Promote adequate nutrition and hydration ○ Promote positive body image, self-esteem ○ Self-care management ● Collaborative problems/potential complications ○ Respiratory distress ○ Hemorrhage ○ Infection ○ Wound breakdown ○ Aspiration ○ Tracheostomal stenosis Tracheostomy ● Tracheotomy is a surgical incision into the trachea to establish an airway ● Tracheostomy is the stoma, or opening, that results from the tracheotomy ● Indications ○ Bypass an upper airway obstruction ○ Facilitate removal of secretions ○ Permit long-term mechanical ventilation ○ Permit oral intake and speech in patient who requires long-term mechanical ventilation ● Advantages ○ Less risk of long-term damage to airway ○ Increased comfort ○ Patient can eat ○ Increased mobility because tube is more secure ● Tracheostomy care ○ Explain purpose before procedure■ Inform patient and family of inability to speak while inflated cuff is used ○ Tubes contain a faceplate or flange ■ Rests on neck between clavicles and outer cannula ○ During insertion, obturator is placed inside the outer cannula with rounded tip protruding from end to ease insertion ○ After insertion, obturator must be immediately removed to allow airflow ○ Keep obturator near bedside in case of decannulation ○ Some tubes have a removable inner cannula for easier cleaning ○ Care involves ■ Suctioning the airway to remove secretions ■ Cleaning around stoma ■ Changing ties ■ Inner cannula care ○ Tube with inflated cuff is used for risk of aspiration or in mechanical ventilation ■ Inflate cuff with minimum volume required to create an airway seal ■ Should not exceed 20 mm Hg or 25 cm H2O ○ Excessive cuff pressure can ■ Compress tracheal capillaries ■ Limit blood flow ■ Predispose to tracheal necrosis ○ Minimal leak technique (MLT) ■ Inflate cuff with minimum amount of air to form seal ■ Then withdraw 0.1 ml of air ■ Risk for aspiration ■ Not used if tracheostomy is bypassing upper airway obstruction ○ Deflation ■ To remove secretions accumulating above the cuff ■ Patient should cough up secretions before deflation to avoid aspiration■ Suction mouth and tube ■ During exhalation because gas helps propel secretions into mouth ■ Patient should cough and be suctioned again ■ Assess patient’s ability to protect the airway from aspiration ■ Remain with patient when cuff is initially deflated unless patient can protect against aspiration and breathe without respiratory distress ○ When patient can protect against aspiration and does not require mechanical ventilation, a cuffless tube is used ○ Reinflation ■ During inspiration ■ Monitor inflation volume daily because it may increase with tracheal dilation from cuff pressure ○ Retention sutures ■ Placed in tracheal cartilage during tracheotomy ■ Free ends taped to skin and left accessible in case tube is dislodged ○ Precautions for tube replacement ■ Tube of equal or smaller size kept at bedside for emergency reinsertion ■ Tapes not changed for at least 24 hours after insertion ■ First change by physician no sooner than 7 days after tracheotomy ○ Accidental dislodging ■ Immediately replace tube ■ Spread opening with retention sutures grasped or hemostat ■ Obturator inserted in replacement tube ● Lubricated with saline poured over tip ● Inserted at 45 degrees to neck ○ If insertion is successful, obturator is removed immediately for air flow through tube ○ Another method for reinsertion■ Insert suction catheter to allow for air passage; serves as a guide for obturator ■ Tube should be threaded over catheter and suction catheter removed ○ If tube cannot be replaced ■ Assess level of respiratory distress ■ Minor dyspnea may be alleviated with semi-Fowler’s position ■ Severe distress may progress to respiratory arrest ■ Cover stoma with sterile dressing and ventilate with bagmask until help arrives ○ Tube should be changed monthly ○ Patient can be taught to change tube using clean technique at home ● Nursing management ○ Providing tracheostomy care ○ Swallowing dysfunction ○ Speech with a tracheostomy tube ○ Decannulation ● Swallowing dysfunction ○ Inflated cuff ■ Interferes with normal function of muscles used to swallow ■ Evaluate risk of aspiration with cuff deflated or substitute with a cuffless tube ○ Evaluate aspiration ■ Add blue coloring to clear liquid and evaluate coughing and secretions or suction trachea for blue fluid ■ Test tracheobronchial secretions for glucose (mucus is generally very low) ● Speech ○ Fenestrated tracheostomy tube with cuff deflated, inner cannula removed, and tracheostomy tube capped to allow air to pass over the vocal cords○ One tube is used for cuff inflation. The second tube is connected to a source of compressed air or oxygen. When the port on the second tube is occluded, air flows up over the vocal cords, allowing speech with an inflated cuff. ○ Techniques to promote speech ■ Spontaneously breathing patient may deflate cuff, allowing exhaled air to flow over vocal cords ■ Patient on mechanical ventilation can allow constant air leak around cuff ■ Tracheostomy tubes and valves have been designed to facilitate speech ■ Promote use to provide psychological benefit and selfcare ○ Fenestrated tube has an opening on the surface of outer cannula to permit air flow over vocal cords to allow ■ Spontaneous breathing through larynx ■ Speech ■ Secretion expectoration with tube in place ○ Fenestrated tube ■ Ability to swallow is determined before use ■ Frequently assess for signs of respiratory distress on first use ■ Potential for development of tracheal polyps ○ Speaking tracheostomy has two pigtail tubings ■ One connects to cuff for inflation ■ Other connects to opening just above cuff ■ When second tube is connected to low-flow air source, it permits speech ○ Ability to tolerate cuff deflation without aspiration or respiratory distress must be evaluated ■ If no aspiration, cuff is deflated and valve placed over opening ○ Provide patient with writing tools if speaking devices are not used ○ When patient can adequately exchange air and expectorate■ Stoma closed with tape and covered with an occlusive dressing ■ Instruct patient to splint stoma with fingers when coughing, swallowing, or speaking ○ Tissue forms in 24 to 48 hours ○ Opening will close in several days without surgical intervention Acute respiratory failure ● ABG values: ○ Pao2 <60 mm Hg ○ Sao2 <90%; or Paco2 >50 mm Hg with pH <7.30 ● Ventilatory failure ○ Physical problem of lungs or chest wall ○ Defect in respiratory control center in brain ○ Poor function of respiratory muscles, especially diaphragm ○ Extrapulmonary causes ○ Intrapulmonary causes ● Oxygenation failure ○ Insufficient oxygenation of pulmonary blood at alveolar level ○ Ventilation normal, lung perfusion decreased ○ Right to left shunting of blood ○ V/Q mismatch ○ Low partial pressure of O2 ○ Abnormal hemoglobin ● Combined ventilatory/oxygenation failure ○ Often occurs in patients with abnormal lungs ■ Chronic bronchitis ■ Emphysema ■ Asthma attack ○ Diseased bronchioles and alveoli cause oxygenation failure; work of breathing increases; respiratory muscles unable to function effectively ● Patient is always hypoxemicAcute respiratory distress syndrome ● Persisting hypoxia ● Decreased pulmonary compliance ● Dyspnea ● Noncardiac-associated bilateral pulmonary edema ● Dense pulmonary infiltrates seen on x-ray ● Diagnostic assessment ○ Lower Pao2 value on ABG ○ Refractory hypoxemia ○ ―Whited-out‖ (ground glass) appearance to chest x-ray ○ No cardiac involvement on ECG ○ Low-to-normal PCWP ■ PCWP, Pulmonary capillary wedge pressure. ● Interventions ○ ET intubation, conventional mechanical ventilation with PEEP or CPAP ■ CPAP, Continuous positive airway pressure; ET, endotracheal; PEEP, positive end-expiratory pressure. ○ Drug and fluid therapy ○ Nutrition therapy ○ Case management Chest trauma-Pneumothorax and Hemothorax ● Chest trauma ○ About 25% of traumatic deaths result from chest injuries ■ Pulmonary contusion ■ Rib fracture ■ Flail chest ■ Pneumothorax ■ Tension pneumothorax ■ Hemothorax ■ Tracheobronchial trauma ● Tension pneumothorax○ Assessment findings ■ Asymmetry of thorax ■ Tracheal movement away from midline toward unaffected side ■ Respiratory distress ■ Absence of breath sounds on one side ■ Distended neck veins ■ Cyanosis ■ Hypertympanic sound on percussion ● Pneumothorax ● Hemothorax○ The amount of blood that can accumulate in the thoracic cavity (leading to hypovolemia) is a much more severe condition than the amount of lung compressed by this blood loss. Pulmonary embolism ● Pulmonary embolism with infarction. ● Collection of particulate matter – solids, liquids, air – that enters venous circulation and lodges in pulmonary vessels usually occurs when a blood clot from a venous thromboembolism in leg or pelvic vein breaks off and travels through the vena cava into the right side of the heart. ● Risk factors ○ Prolonged immobilization ○ Central venous catheters ○ Surgery ○ Obesity ○ Advancing age ○ Conditions that increase blood clotting ○ History of thromboembolism ● Health promotion & illness prevention ○ Smoking cessation ○ Weight reduction○ Increased physical activity ○ If traveling or sitting for long periods, get up frequently and drink plenty of fluids ○ Refrain from massaging/compressing leg muscles ● Clinical manifestations ○ Respiratory ■ Dyspnea, tachypnea, tachycardia, pleuritic chest pain, dry cough, hemoptysis ○ Cardiac ■ Distended neck veins, syncope, cyanosis, systemic hypotension, abnormal heart sounds, abnormal ECG ○ Low-grade fever, petechiae, flu-like symptoms ○ ECG, electrocardiogram ● Laboratory assessment ○ ABGs ○ Pao2–Fio2 ratio falls ○ Pulse oximetry ○ Imaging assessment ● Non surgical management ○ Oxygen therapy (nasal cannula, mask) ○ Continuous patient monitoring ○ Obtain adequate venous access ○ Continuous monitoring of pulse oximetry ○ Drug therapy ■ Anticoagulants ■ Fibrinolytics ● Interventions ○ Assess for bleeding every 2 hr ○ Examine all stool, urine, drainage, vomitus for gross blood; test for occult blood ○ Measure abdominal girth every 8 hr ○ Monitor laboratory values ○ Surgical management ■ Embolectomy ■ Inferior vena cava filtration● ● ● Mechanical Ventilation Selected Disorders (Renal) Hemodialysis ● Hemodialysis: used when patient is acutely ill until the kidneys resume function and for long-term replacement therapy in CKD and ESRD ● Objective is to extract toxic nitrogenous substances from the blood and to remove excess fluid: ○ Diffusion, osmosis, and ultrafiltration ● Vascular access ○ Arteriovenous fistula ○ Arteriovenous graft Peritoneal ● Goals are to remove toxic substances and metabolic wastes and to reestablish normal fluid and electrolyte balance ● Peritoneal membrane serves as semipermeable membrane ○ Ultrafiltration ○ Peritoneal catheter ● Acute intermittent, continuous ambulatory, continuous cyclic ● Complications: peritonitis, leakage, bleeding Acute kidney failure/injury ● Causes ○ Hypovolemia ○ Hypotension ○ Reduced cardiac output and heart failure ○ Obstruction of the kidney or lower urinary tract ○ Obstruction of renal arteries or veinsChronic kidney disease ● Causes ○ Diabetes mellitus ○ Hypertension ○ Chronic glomerulonephritis ○ Pyelonephritis or other infections ○ Obstruction of urinary tract ○ Hereditary lesions ○ Vascular disorders ○ Medications or toxic agents Acute Glomerulonephritis ● Postinfectious glomerulonephritis, rapidly progressive glomerulonephritis, and membranous glomerulonephritis ● Secondary to beta hemolytic strep infection ● Manifestations include hematuria, edema, azotemia, proteinuria, and hypertension ● May be mild or may progress to acute kidney disease or death ● Medical management includes supportive care and dietary modifications; treat cause if appropriate—antibiotics, corticosteroids, and immunosuppressants ● Nursing management ○ Patient assessment ○ Maintain fluid balance ○ Fluid and dietary restrictions ○ Patient education ○ Follow-up care Renal transplant● ● Postoperative nursing management ○ Assessment: include all body systems, pain, fluid and electrolyte status, and patency and adequacy of urinary drainage system ○ Diagnoses: ineffective airway clearance, ineffective breathing pattern, acute pain, fear and anxiety, impaired urinary elimination, and risk for fluid imbalance ○ Complications: bleeding , pneumonia, infection, and DVT ● Postoperative interventions ○ Pain relief measures, analgesic medications ○ Promote airway clearance and effective breathing pattern, turn, cough, deep breathe, incentive spirometry, positioning ○ Monitor UO and maintain potency of urinary drainage systems ○ Use strict asepsis with catheter ○ Monitor for signs and symptoms of bleeding ○ Encourage leg exercises, early ambulation, and monitor for signs of DVT ● Patient education ○ Instruct both patient and family ○ Drainage system care ○ Strategies to prevent complications ○ Signs and symptoms ○ Follow-up care○ Fluid intake ○ Health promotion and health screening [Show More]
Last updated: 2 years ago
Preview 1 out of 21 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$10.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
May 16, 2021
Number of pages
21
Written in
Additional information
This document has been written for:
Uploaded
May 16, 2021
Downloads
0
Views
128




.png)