*NURSING > QUESTIONS & ANSWERS > Chamberlain College of Nursing - NR 509NR509_SOAP_Note_Template 4. All Filled and Graded A (All)
Chamberlain College of Nursing - NR 509NR509_SOAP_Note_Template 4. All Filled and Graded A
Document Content and Description Below
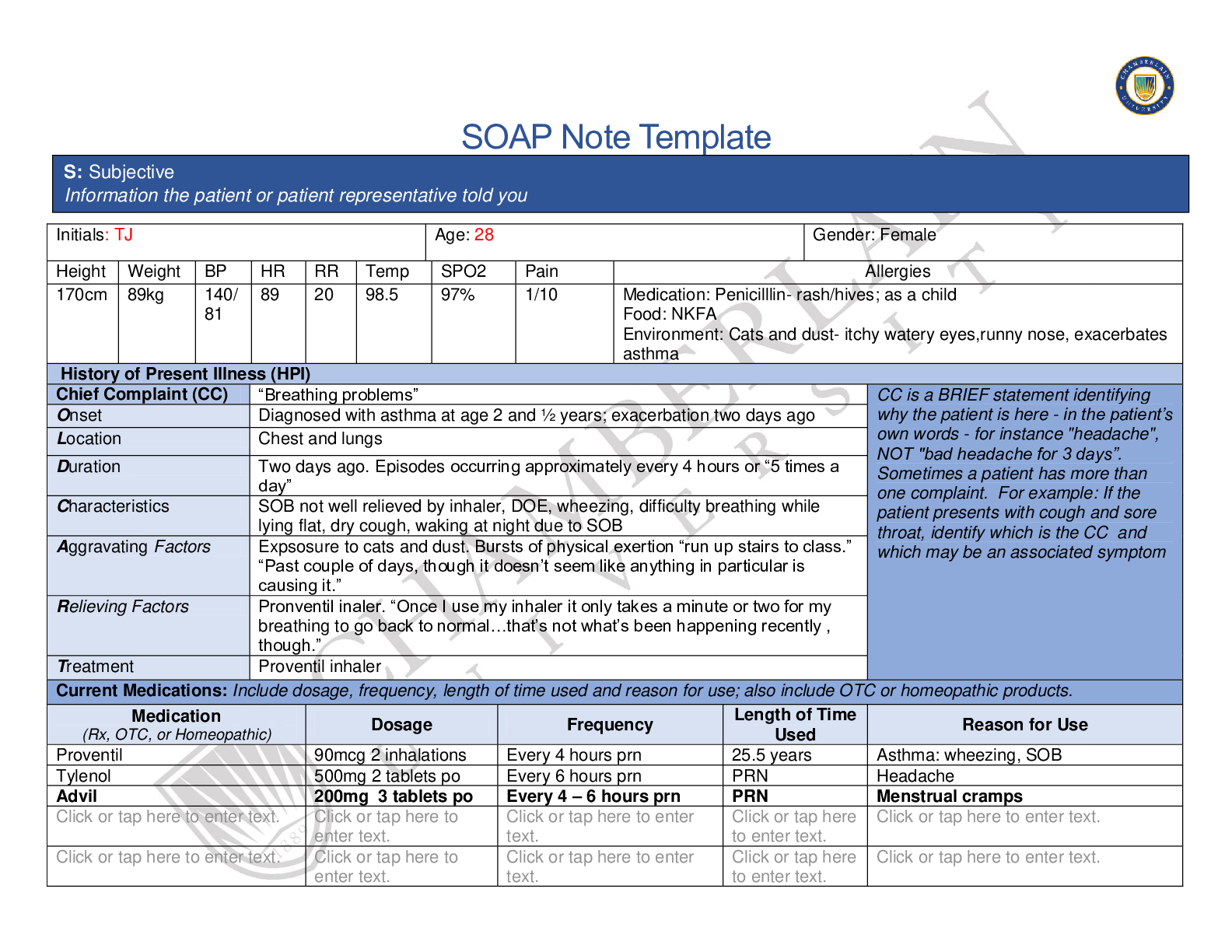
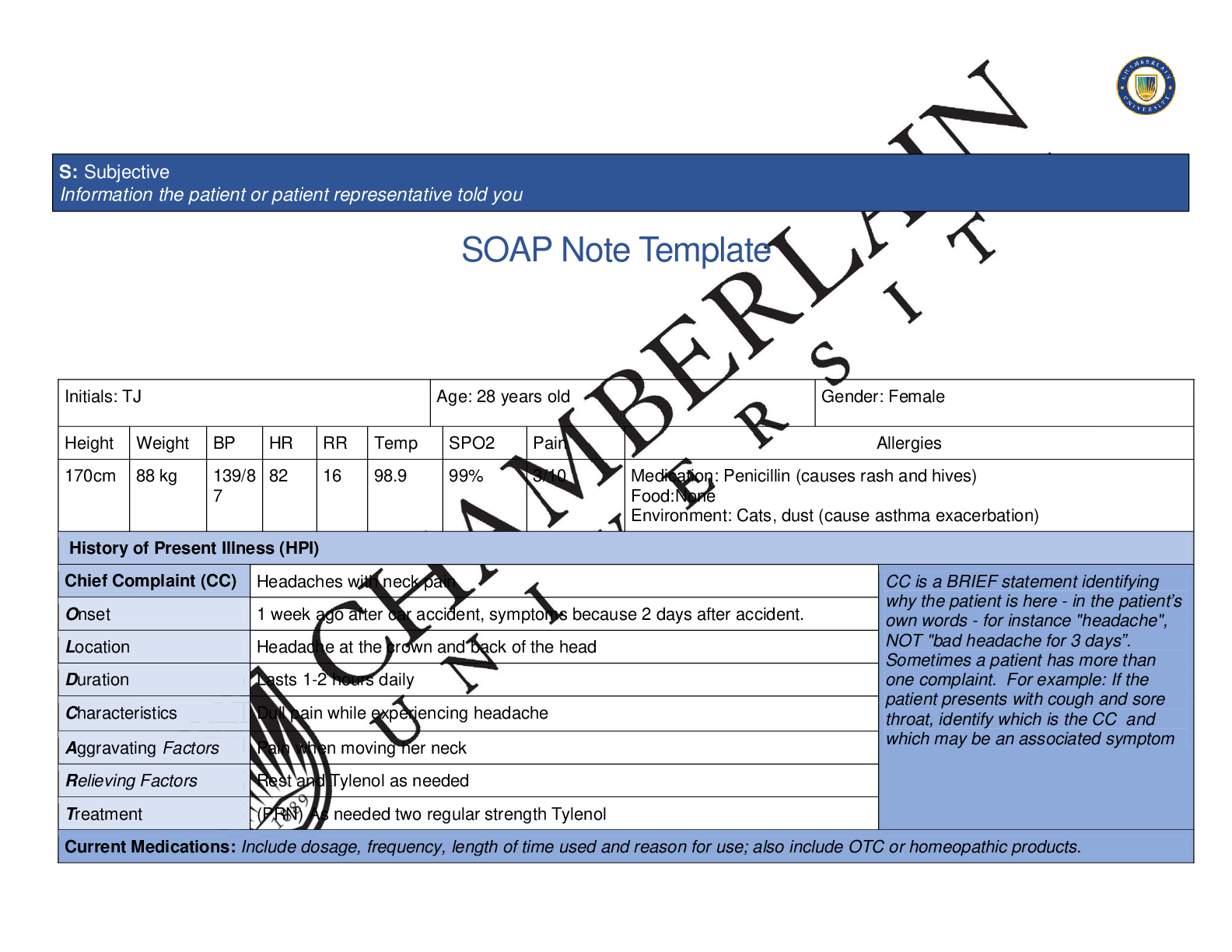
SOAP Note Template Initials: BF Age: 58 Gender: M Height Weight BP HR RR Temp SPO2 Pain Allergies 5 feet 11 inches 197lbs. 146/ 90 104 19 36.7 98 1/10 Medication: Codeine (nausea and vomiting)... Food: None Environment: None History of Present Illness (HPI) Chief Complaint (CC) Chest pain over “middle of chest over heart.” CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a patient has more than one complaint. For example: If the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom Onset Experiencing chest pain for the “past month.” Location Middle of chest over heart, does not radiate Duration Pain lasts “1-2 minutes.” Pain passes with rest. Has experienced chest pain 3x in the last month. Last episode of chest pain experience last Friday. Characteristics Describes the pain as “Tight and uncomfortable.” Denies nausea, vomiting, shortness of breath or palpitations with pain. States the pain is 5/10 when chest pain occurs. Denies pain currently. Denies crushing, gnawing, or burning pain. Aggravating Factors Physical activity. On first occurrence, Mr. Foster was going yard work by pulling weeds, second occurrence he was using stairs to get to 5th floor of office. Denies pain becoming worse with eating or any type of food. Relieving Factors Taking a break or sitting down to rest Treatment No medications currently being taken for chest pain, rest relieves pain Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products. Medication (Rx, OTC, or Homeopathic) Dosage Frequency Length of Time Used Reason for Use Metoprolol (Lopressor) 100mg Daily 1 year Hypertension Atorvostatin (Lipitor) 20mg Daily at bedtime 1 year Hyperlipidemia Omega 3 Fish Oil 1200mg BID 1 year OTC supplement Tylenol of Ibuprofen Recommendation of bottle As needed n/a Headache S: Subjective Information the patient or patient representative told youPast Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses, hospitalizations, and surgeries. Depending on the CC, more info may be needed. Immunizations: Tdap 10/2014, Influenza vaccine this season PMHx: Hypertension – Stage II, diagnosed 1 year ago, Hyperlipidemia- diagnosed 1 year ago SurgHx: No surgical history Has never been diagnosed with angina, diabetes, coronary artery disease Does not monitor blood pressure at home, checks blood pressure at check up appointments. Per patient doctor has never seemed overly concerned about it. EKG done about 3 months ago, per patient as far as he knows test results are “normal.” Last Stress test 4 months ago, Per patient the doctor said “everything looks good.” Primary Care Provider: Dr. Melinda Smith, Last visit was 3 months ago. Does not have a cardiologist Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent data. Include health promotion such as use seat belts all the time or working smoke detectors in the house. No past or present tobacco use Reports drinking 2-3 alcoholic beverages (beer) per week Denies use of marijuana, cocaine, heroin, or other illicit drugs Patient states his work stress is low Denies regular exercise No breakfast this morning. Lunch: roast beef sandwich and little salad. Dinner: buffalo wings Does not monitor salt intake Drinks water mostly, 1-2 cups of coffee most mornings, orange juice, or grape fruit juice sometimes, and a couple of beers on the weekends Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if pertinent. Father: hypertension, hyperlipidemia, obesity, died of colon cancer, age 75 Mother: type 2 diabetes, hypertension, age 80 Brother: died at age 24 in motor vehicle accident Sister: type 2 diabetes, hypertension, age 52 Maternal grandmother: died of breast cancer age 65 Maternal grandfather: died of heart attach, age 54Paternal grandmother: died of pneumonia age 78 Paternal grandfather: died of “old age” age 85 Son: healthy, age 26 Daughter: asthma, age 19 Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive symptom and provide additional details. Constitutional Skin HEENT ☐Fatigue here to . ☐Weakness . ☐Fever/Chills . ☒Weight Gain Gained 20lbs in the last couple of years ☐Weight Loss . ☐Trouble Sleeping Click or tap . ☐Night Sweats . ☒Other: enter text. ☐Itching . ☐Rashes . ☐Nail Changes Click or tap here to enter text. ☐Skin Color Changes Denies cyanosis ☐Other: . ☐Diplopia . ☐Eye Pain . ☐Eye redness Click or tap . ☐Vision changes Denies ☐Photophobia Click or tap . ☐Eye discharge Click or tap . ☐Earache here to . ☐Tinnitus here to . ☐Epistaxis . ☐Vertigo here to . ☒Hearing Changes Denies ☐Hoarseness here to . ☐Oral Ulcers here to . ☐Sore Throat Denies ☐Congestion here to . ☐Rhinorrhea here to . ☐Other: . Respiratory Neuro Cardiovascular ☐Cough Denies ☐Hemoptysis Denies ☐Dyspnea Denies ☐Wheezing Denies ☐Pain on Inspiration Denies ☐Sputum Production . ☐Syncope or Lightheadedness Denies ☒Headache Once in a blue moon ☐Numbness Denies ☐Tingling Denies ☐Sensation Changes . ☒Chest pain Middle chest 5/10 ☐SOB Denies ☐Exercise Intolerance here to . ☐Orthopnea enter text. ☐Edema Denies ☐Palpitations Denies ☐Faintness here to . ☐OC Changes . ☐Claudications . ☐PND . . ☐ text. ☐Speech Deficits . ☐Other: . ☐Murmurs enter text. . ☐Other: . MSK GI GU PSYCH ☐Pain Denies ☐Stiffness Denies ☐Crepitus . ☐Swelling . ☐Limited ROM . ☐Redness . ☐Misalignment . ☐ text. ☐Nausea/Vomiting Denies ☐Dysphasia enter text. ☐Diarrhea enter text. ☐Appetite Change Denies ☐Heartburn enter text. ☐Blood in Stool Denies ☐Abdominal Pain . ☐Excessive Flatus . ☐Food Intolerance . ☐Rectal Bleeding Denies ☐Other: . ☐Urgency . ☐Dysuria Denies ☐Burning Denies ☐Hematuria Denies ☐Polyuria Denies ☐Nocturia Denies ☐Incontinence . ☐Other: . ☐Stress . ☒Anxiety Due to unknown chest pain ☐Depression here to . ☐Suicidal/Homicidal Ideation . ☐Memory Deficits . ☐Mood Changes . ☐Trouble Concentrating Click or tap . ☐Other: . GYN ☐Rash . ☐Discharge . ☐Itching . ☐Irregular Menses . ☐Dysmenorrhea . ☐Foul Odor . ☐Amenorrhea . ☐LMP: . ☐Contraception . ☐Other:. O: Objective Information gathered during the physical examination by inspection, palpation, auscultation, and palpation. If unable to assess a body system, write “Unable to assess”. Document pertinent positive and negative assessment findings.Body System Positive Findings Negative Findings General . Face: Symmetrical no drooping, no redness, no discoloration, no presence of rashes or lesions, no scaring or bruising noted JVP: 3cm above the sternal angle, No jugular venous distention Chest: Symmetrical, no visible abnormalities, no rashes or lesions present no presence of intercostal retraction while breathing, no use of accessory muscles while breathing, no skin growths present, no evidence of skin trauma Abdomen: Symmetrical, contour is flat, appears with no abnormal findings, No presence of rash or striae, no presence of bulging around the umbilicus, no distention noted, no visible masses noted, no discoloration noted, no bruising noted, no excessive hair growth, no visible scares present Hands: Right hand presents with no abnormal findings, no redness noted, no moles or skin tags noted, no masses noted, no freckles noted, no birthmarks noted, no excessive dry or flaking skin noted, no scarring noted, no lacerations noted, no bruising present, no rashes noted. Right finger nails have no visible abnormal findings, no clubbing noted, no pallor, no cyanosis, and no splinter hemorrhages noted. Capillary refill les than 3 seconds. Left Hand: presents with no abnormal findings, no redness noted, no moles or skin tags noted, no masses noted, no freckles noted, no birthmarks noted, no excessive dry or flaking skin noted, no scarring noted, no lacerations noted, no bruising present, no rashes noted. Left finger nails have no visible abnormal findings, no clubbing noted, no pallor, no cyanosis, and no splinter hemorrhages noted. Capillary refill less than 3 seconds Lower extremities: lower right extremity: No visible abnormal findings, no swelling or distortion, no presence of brownish pigmentation, no skin thickening noted, no ulceration noted, no veriose veins noted. No edema present Right lower extremity nails: No visible abnormal findings, no pallor noted, no cyanosis present, no splinter hemorrhages noted, no clubbing noted. Lower left extremity: No visible abnormal findings, no swelling or distortion, no presence of brownish pigmentation, no skin thickening noted, no ulceration noted, no varicose veins noted. No edemapresent Left lower extremity nails: No visible abnormalities noted, no pallor noted, no cyanosis present, no splinter hemorrhages noted, no clubbing noted Skin . . Denies cyanosis nd pallor HEENT . . Denies changes in vision, denies change in sensation of taste, denies sore throat Respiratory . . Denies shortness of breath, denies dyspnea, denies cough Neuro . . Denies dizzinesss, denies numbness or tingling. Headache occurs “once in a blue moon” per pt report. Cardiovascular . Auscultate: right carotid arteries: Bruit Present Heart Sounds: S1, S2, & S3 with Gallops present Breath Sounds: Crackles to posterior Left lower lobes and Right lower lobes present Abdominal Aorta: Bruit present Palpate: Carotid Arteries: Right- thrill 3+(increased) PMI: Discplaced Laterally brisk and tapping, diameter: less than 3cm Auscultate: Left carotid arteries: No bruits present Abdominal Arteries: No bruit in Femoral, Iliac, or Renal Arteries Bowel sounds: All bowel sounds present and normoactive Organs: No friction rub over liver or spleen Palpate Carotid Artieries: Left – no thrill present 2+ Braichial Arteries: Bilaterally no thrill, 2+ amplitude Radial Arteries: Bilaterally no thrill, 2+ amplitude Femoral Arteries: Bilaterally no thrill 2+ amplitude Popliteal Arteries: Bilaterally no thrill 1+ amplitude (Dminished or barely palpable) Tibial Arteries: Bilaterally no thrill, 1+ a,plitude (Diminished or barely palpable) Dorsalis Pedis Artieries: Bilaterally no thrill, 1+ amplitude (diminished or barely palpable) Abdomen, light : No tenderness, no masses, no guarding or ditention noted in all quadrants Abdomen, Deep: No masses palpated Liver: Palpated 1cm below right costal marginProblem List 1. Chest psin 6 . 11 . . 5 . 10 . 15 . Spleen: Not palpable Kidneys: Bilaterally not palpable Percussion: Abdomen: Generally tympanic Spleen: Dullness noted Liver: Liver span 7cm (normal span: 6-12cm) EKG: Regular Sinus Rhythm. No ST changes. Musculoskeletal . . Denies joint or back pain Gastrointestinal . . Denies nocturia Genitourinary . . . Psychiatric . Feeling anxious due to chest pain and not knowing what is going on. Denies history of depression or mood changes. . Gynecological . . . A: Assessment Medical Diagnoses. Provide 3 differential diagnoses which may provide an etiology for the CC. The first diagnosis (presumptive diagnosis) is the diagnosis with the highest priority. Provide the ICD-10 code and pertinent findings to support each diagnosis.Diagnostics: List tests you will order this visit Test Rationale/Citation Echocardiogram For evaluation of the heart (Mayo Clinic, 2019) Carotid Doppler To assess for possible corornary artery disease (Terzi, Arslanoğlu, Demiray, Eren, & Cancuri, 2015) Lipid profile measures the amount of cholesterol and fats called triglycerides in the blood (Terzi, Arslanoğlu, Demiray, Eren, & Cancuri, 2015) CBC, CMP, CRP To test for status of liver, kidneys, cardiovascular disease (Terzi, Arslanoğlu, Demiray, Eren, & Cancuri, 2015) . . Medications: List medications/treatments including OTC drugs you will order and “continue previous meds” if pertinent. Drug Dosage Length of Treatment Rationale/Citation Aspirin 81 mg . For evaluation of the heart Sublingual Nitroglycerin 0.3-0.6ml . For chest pain Calcium Channel Blocker 2.5mg . For cardiovascular disease protection . . . . . . . . Referral/Consults: . Rationale/Citation . Education: Medication education, exercise regimen, diet education Rationale/Citation . Follow Up: Indicate when patient should return to clinic and provide detailed instructions indicating if the patient should return sooner than scheduled or seek attention elsewhere. Diagnosis ICD-10 Code Pertinent Findings Angina . Chest pain CHF . S3 and gallop present Atherosclerosis . Carotid bruit P: Plan Address all 5 parts of the comprehensive treatment plan. If you do not wish to order an intervention for any part of the treatment plan, write “None at this time” but do not leave any heading blank. No intervention is self-evident. Provide a rationale and evidence-based in-text citation for each intervention.In 1 week to reassess any potential chest pain occurrence, potentially start medication Calcium Channel Blocker, Call 911 if chest pain unrelieved by 3 doses of sublingual nitro. Rationale/Citation . References Include at least one evidence-based peer-reviewed journal article which relates to this case. Use the correct APA 6th edition formatting. Terzi, S., Arslanoğlu, S., Demiray, U., Eren, E., & Cancuri, O. (2015). Carotid Doppler ultrasound evaluation in patients with pulsatile tinnitus. Indian journal of otolaryngology and head and neck surgery : official publication of the Association of Otolaryngologists of India, 67(1), 43–47. doi:10.1007/s12070-014-0756-9 Mayo Clinic (2019). Echocardiogram. Retrieved from: https://www.mayoclinic.org/tests-procedures/echocardiogram/about/pac-20393856 Mayo Clinic (2019). Nitroglycerin. Retrieved from: https://www.mayoclinic.org/drugs-supplements/nitroglycerin-oral-route-sublingual-route/properuse/drg-20072863 [Show More]
Last updated: 2 years ago
Preview 1 out of 9 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$18.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jun 07, 2020
Number of pages
9
Written in
Additional information
This document has been written for:
Uploaded
Jun 07, 2020
Downloads
0
Views
91






.png)
.png)
.png)
.png)
.png)
.png)
.png)