*NURSING > QUESTIONS & ANSWERS > Chamberlain College of Nursing - NR 509_BF_SOAP_Wk4 Cardiovascular: Chest tightness, hypertension, T (All)
Chamberlain College of Nursing - NR 509_BF_SOAP_Wk4 Cardiovascular: Chest tightness, hypertension, Tachycardia, Crackles in bilateral lower lobes, Exertion intolerance, hyperlipidemia
Document Content and Description Below
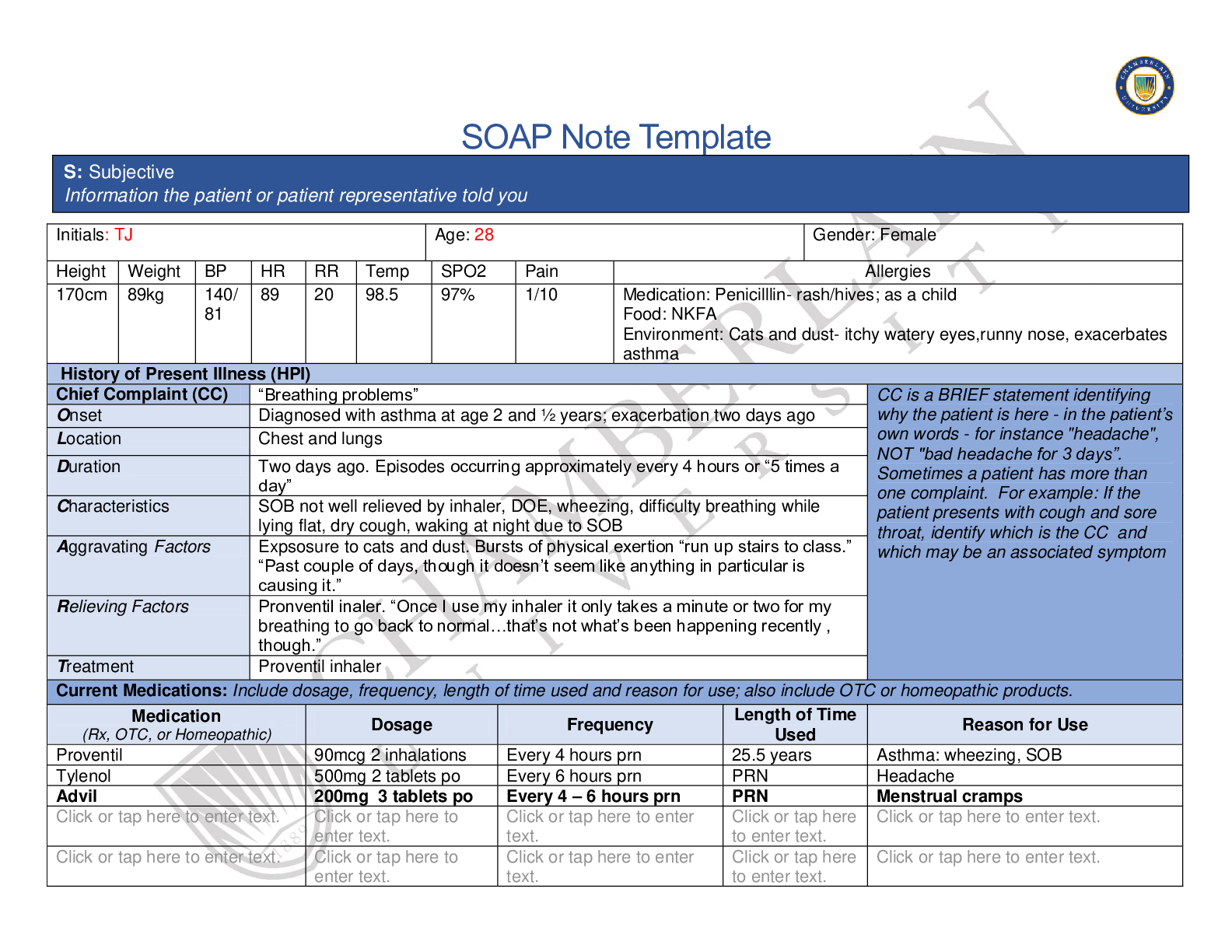
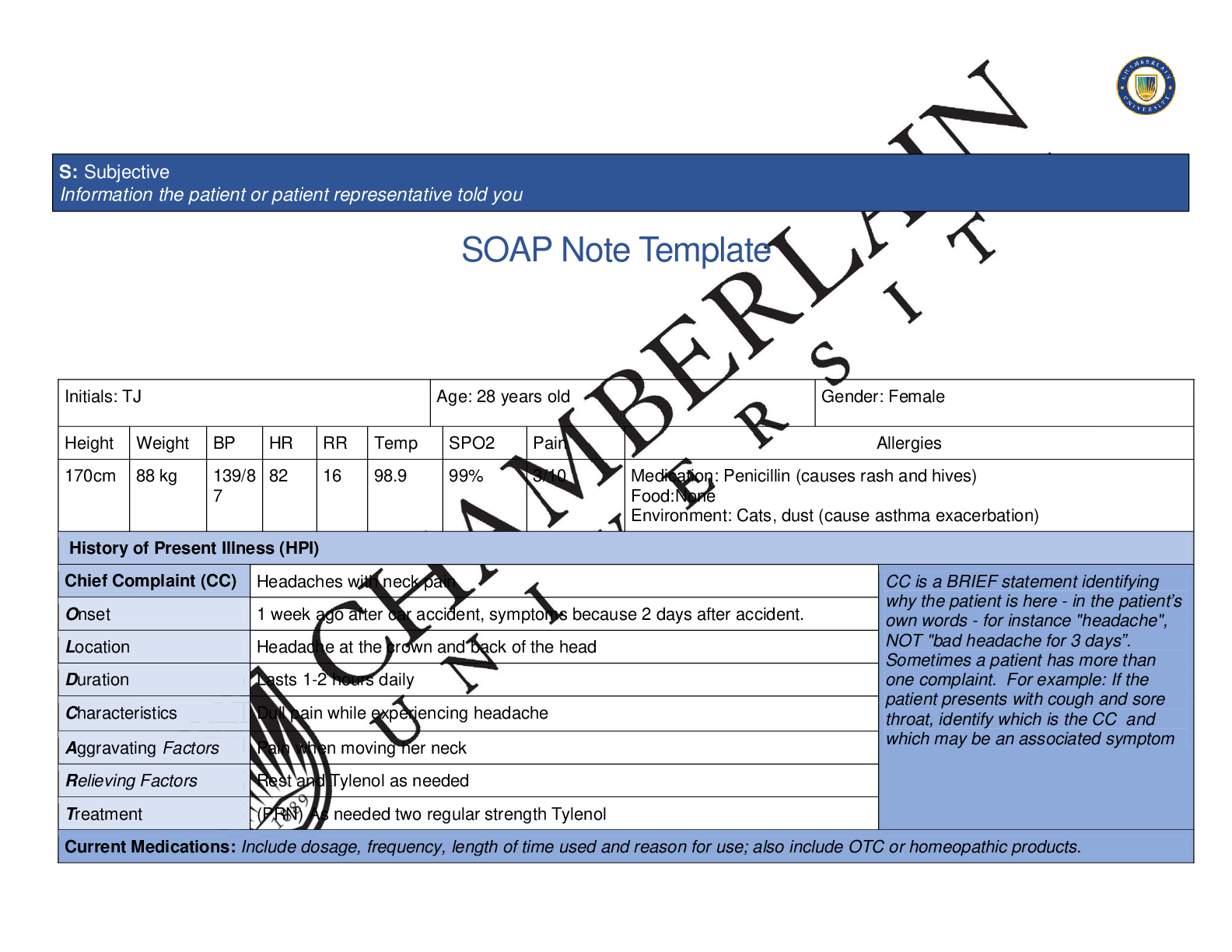
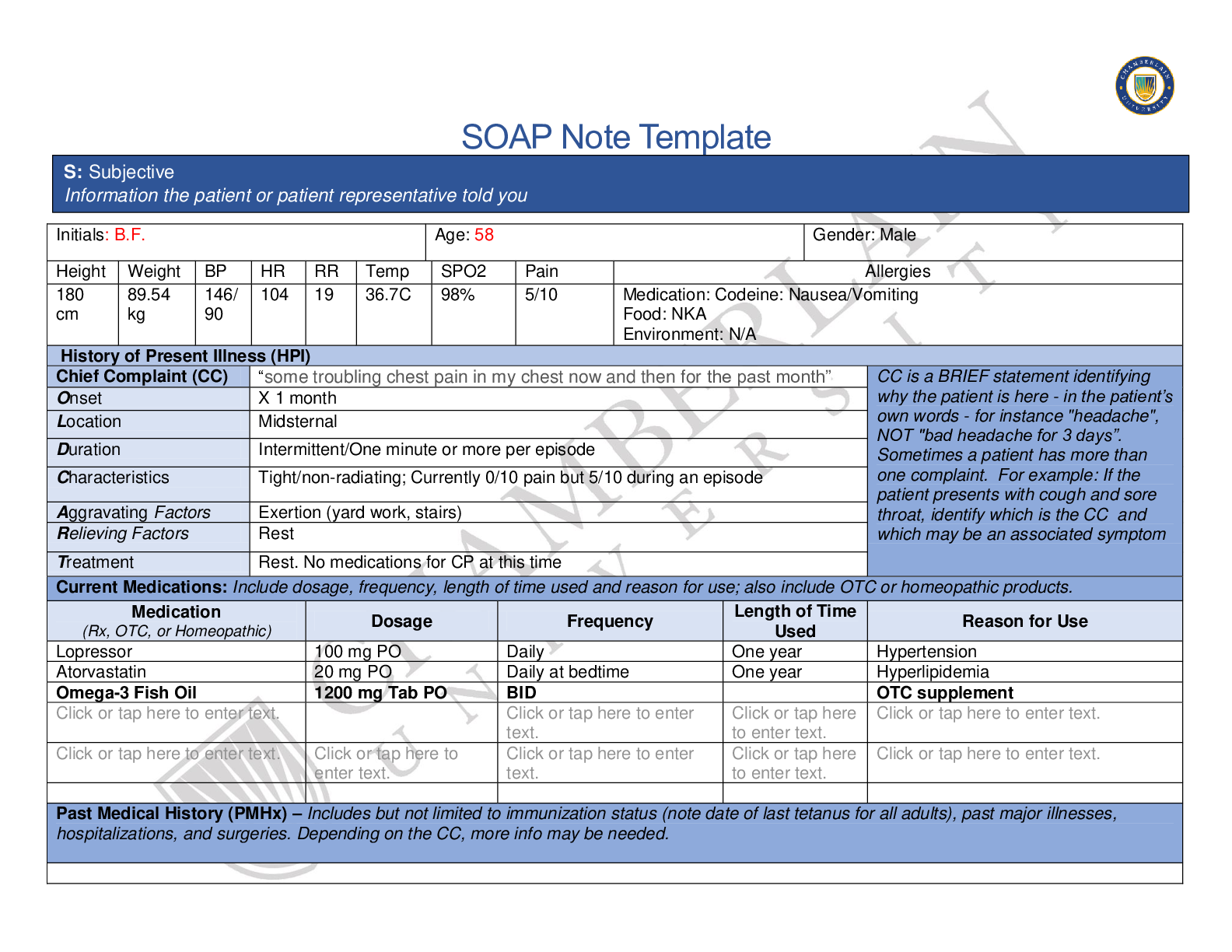
SOAP Note Template Initials: B.F. Age: 58 Gender: Male Height Weight BP HR RR Temp SPO2 Pain Allergies 180 cm 89.54 kg 146/ 90 104 19 36.7C 98% 5/10 Medication: Codeine: Nausea/Vomiting Food... : NKA Environment: N/A History of Present Illness (HPI) Chief Complaint (CC) “some troubling chest pain in my chest now and then for the past month” CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a patient has more than one complaint. For example: If the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom Onset X 1 month Location Midsternal Duration Intermittent/One minute or more per episode Characteristics Tight/non-radiating; Currently 0/10 pain but 5/10 during an episode Aggravating Factors Exertion (yard work, stairs) Relieving Factors Rest Treatment Rest. No medications for CP at this time Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products. Medication (Rx, OTC, or Homeopathic) Dosage Frequency Length of Time Used Reason for Use Lopressor 100 mg PO Daily One year Hypertension Atorvastatin 20 mg PO Daily at bedtime One year Hyperlipidemia Omega-3 Fish Oil 1200 mg Tab PO BID OTC supplement Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses, hospitalizations, and surgeries. Depending on the CC, more info may be needed. S: Subjective Information the patient or patient representative told youStage 2 HTN – dx’ed 1 year ago Hyperlipidemia – dx’ed 1 year ago No surgical history Tdap – 10/2014 Influenza Vaccine - 2019 Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent data. Include health promotion such as use seat belts all the time or working smoke detectors in the house. Married and lives with wife. Has two adult children. Profession: engineer. Participates in home gardening. Pt enjoys riding bicycles but unable to as bicycle stolen. Pt denies stress at home. Diet includes meats and vegetables; big breakfasts on weekends. No past or current hx of smoking Reports drinking 2-3 alcoholic beverages (beer) weekly Denies illicit drug use. Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if pertinent. Mother: DM Type 2, HTN – Living, age 80 Father: HTN, Hyperlipidemia, Colon Cancer, Obesity – Deceased: Colon Cancer; age 75 Paternal Grandfather: Deceased:”Old Age,” age 85 Maternal Grandfather: Deceased: MI; age 54 Paternal Grandmother: Deceased: Pneumonia; age 78 Maternal Grandmother: Deceased: Breast Cancer; age 65 Brother: Deceased: MVC, age 24 Sister: DM Type 2, HTN – Living, age 52 Son: Healthy, age 26 Daughter: Asthma, age 19 Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive symptom and provide additional details.Constitutional Skin HEENT ☐Fatigue /Occasional tiredness ☐Weakness tap here . ☐Fever/Chills tap here . ☒Weight Gain 20 pounds in last 2-3 years ☐Weight Loss tap here . ☐Trouble Sleeping . ☐Night Sweats tap here . ☐Other: text. ☐Itching tap here . ☐Rashes tap here . ☐Nail Changes Click or enter text. ☐Skin Color Changes . ☐Other: . ☐Diplopia tap here . ☐Eye Pain tap here . ☐Eye redness . ☐Vision changes . ☐Photophobia . ☐Eye discharge . ☐Earache . ☐Tinnitus . ☐Epistaxis tap here . ☐Vertigo . ☐Hearing Changes Click or . ☐Hoarseness . ☐Oral Ulcers . ☐Sore Throat . ☐Congestion . ☐Rhinorrhea (Occasional) ☐Other: . Respiratory Neuro Cardiovascular ☐Cough Frequent at night ☐Hemoptysis . ☐Dyspnea text. ☐Wheezing text. ☐Pain on Inspiration . ☐Sputum Production . . . ☒Other: Crackles ☐Syncope or Lightheadedness tap here . ☐Headache Occasional ☐Numbness . ☐Tingling . ☐Sensation Changes LLE ☐Speech Deficits tap here . ☐Other: . ☒Chest pain Midsternal ☐SOB . ☒Exercise Intolerance Chest pain ☐Orthopnea text. ☐Edema . ☐Murmurs text. ☐Palpitations tap here . ☐Faintness . ☐OC Changes tap here . ☐Claudications tap here . ☐PND . ☒Other: S3 heart sounds MSK GI GU PSYCH☐Pain text. ☐Stiffness . ☐Crepitus . ☐Swelling . ☐Limited ROM . ☐Redness . ☐Misalignment . ☐Other: text. ☐Nausea/Vomiting . ☐Dysphasia text. ☐Diarrhea text. ☐Appetite Change Increase in appetite ☐Heartburn text. ☐Blood in Stool . ☐Abdominal Pain . ☐Excessive Flatus . ☐Food Intolerance . ☐Rectal Bleeding . ☐Other: . ☐Urgency . ☐Dysuria . ☐Burning . ☐Hematuria . ☐Polyuria . ☐Nocturia . ☐Incontinence tap here . ☐Other: . ☐Stress . ☐Anxiety . ☐Depression . ☐Suicidal/Homicidal Ideation . ☐Memory Deficits tap here . ☐Mood Changes tap here . ☐Trouble Concentrating Click or . ☐Other: . GYN ☐Rash . ☐Discharge . ☐Itching . ☐Irregular Menses . ☐Dysmenorrhea . ☐Foul Odor . ☐Amenorrhea . ☐LMP: ☐Contraception . ☐Other: . Body System Positive Findings Negative Findings O: Objective Information gathered during the physical examination by inspection, palpation, auscultation, and palpation. If a body system, write “”. Document pertinent positive and negative assessment findings.General . This is a well-developed, well-appearing, well nourished, in no apparent distress. Alert and Oriented x3, normal mood and affect, Ambulates without difficulty. Skin . Normal turgor. Normal color with no rashes, no lesions, and no evidence of cellulitis. Negative lymphadenopathy. HEENT . Respiratory . Crackles in bilateral posterior lower lobes Symmetrical expansion of chest upon inspiration/expiration. Breath sounds found in all areas. Patient denies SOB/cough. Neuro . Oriented x3. clear speech, face symmetric Normal LOC. Memory intact. Attention span, general knowledge, judgment, memory, vocabulary, articulations. No headaches. Cardiovascular . S3 sound heard with gallops. Tachycardic, hypertensive PMI displaced laterally +1 diminished pulses in bilateral popliteal, tibial & dorsalis pedis arteries. Bruit & (+3) thrill at R carotid artery Chest symmetric. Neurovascular intact in bilateral upper and lower extremities. S1 & S2 sounds audible. Femorial, brachial and radial pulses normal (+2) with no audible thrill. No JVD. Musculoskeletal . Gastrointestinal . No palpable masses noted. Normoactive bowel sounds in all 4 quadrants. Abdomen soft, round, no distention noted, tympanic upon palpation. Liver dull and palpable. Spleen were not palpable. No friction rub audible over kidneys. Genitourinary Unable to palpate kidneys bilaterally.Problem List 1 Chest tightness 6 Exertion intolerance 11 2 hypertension 7 hyperlipidemia 12 3 Tachycardia 8 13 . 4 Crackles in bilateral lower lobes 9 14 . 5 Bruit &(+3) thrill in R carotid artery 10 15 . Psychiatric . Pt admits to anxiety during episodes of chest pain. Pt denies anxiety at time of triage. Gynecological . NA NA Diagnosis ICD-10 Code Pertinent Findings Stable angina I20.9 CC chest tightness/pain during physical exertion, resolving with rest; tachycardia, hypertension. Unspecified CHF I50.20 Crackles in bilateral lower lobes, S3 heart sound & gallop, chest pain, intolerance to physical exertion. Artherosclerosis I25.10 Obesity, sedentary lifestyle, HTN, alcohol consumption, male sex, age, stable exertional angina, hyperlipidemia, bruit in R carotid artery, diminished pulses in bilateral lower extremities. P: Plan Address all 5 parts of the comprehensive treatment plan. If you do not wish to order an intervention for any part of the treatment plan, write “None at this time” but do not leave any heading blank. No intervention is self-evident. Provide a rationale and evidence-based in-text citation for each intervention. A: Assessment Medical Diagnoses. Provide 3 differential diagnoses which may provide an etiology for the CC. The first diagnosis (presumptive diagnosis) is the diagnosis with the highest priority. Provide the ICD-10 code and pertinent findings to support each diagnosis.Diagnostics: List tests you will order this visit Test Rationale/Citation Chest X-ray Allows visualization of heart to determine size (possible cardiomegaly); to determine location of any damage to cardiac tissue; to see if fluid is in or around lungs; hardening of a heart valve or aorta (Johns Hopkins Medicine 2019). Stress Test CP reported post-physical exertion. Test will allow visualization of heart wall to reveal areas of inadequate blood flow (Huisin, et al., 2017). Cardiac Profile Cardiac enzymes are used as diagnostic markers for a MI; determines if there has been damage to the cardiac tissue and whether it is trending up or down. Tests include CPK, CK, Troponin. (Mythili & Malathi, 2015). Medications: List medications/treatments including OTC drugs you will order and “continue previous meds” if pertinent. Drug Dosage Length of Treatment Rationale/Citation Nitroglycerin 0.3 mg SL PRN Q5min; Max 3 doses w/in 15 minutes for acute angina Start 5-10 minutes before strenuous activity Relaxes vascular smooth muscle relaxation to enable easier workload for the heart (Epocrates, 2019). Aspirin 81 mg daily PO Continue till F/U appointment in 4 weeks Anticoagulation; anti-inflammatory effects on vasculatory system (Woo & Robinson, 2016). Lisinopril 10 mg daily PO Continue till F/U appointment in 4 weeks Helps lower/maintain blood pressure while reducing workload of heart (Woo & Robinson, 2016). Lopressor 50 mg daily PO Continue til F/U appointment in 4 weeks Helps treat angina, lower/maintain blood pressure and lowering heart rate (Woo & Robinson, 2016). Lipitor Continue as directed Continue til F/U appointment in 4 weeks Maintain dose; lowers levels of cholesterol and fat to prevent angina and heart disease (Woo & Robinson, 2016). Referral/Consults:Cardiology Rationale/Citation Specialize in heart conditions/diseases. Education: Take Nitro SL as needed for chest pain. If pain does not improve after 3rd pill, call 911. Do not take if also taking an erectile dysfunction medication as it can cause extreme hypotension. Take blood pressure at home each morning and record to provide PCP at next visit. Be aware of abnormal bleeding including bruising from falls, cuts, gums, nose as ASA can cause bleeding. Contact PCP if you have abnormal reduced HR, dizziness, fainting or headaches. Instruct patient to continue with a low-fat, high fiber diet rich in Omega- 3’s. Rationale/Citation Mr. Foster needs to understand how each medication works and when it is appropriate to take them, in addition to when it is appropriate to call 911. Education provides Mr. Foster with the tools he needs to be able to take control of his health care plan and be successful with better health outcomes. Follow Up: Indicate when patient should return to clinic and provide detailed instructions indicating if the patient should return sooner than scheduled or seek attention elsewhere. -Return to office for F/U in four weeks to re-assess current plan and make adjustments in care plan and/or medications if indicated. Rationale/Citation -May need to further assess success of prescribed treatment therapy. -To determine and further educate patient on compliancy with prescribed treatment plan. References Include at least one evidence-based peer-reviewed journal article which relates to this case. Use the correct APA 6th edition formatting. Huisin, A., Cullen, L., Mahler, S. A., Backus, B. E., Dezman, Z. D. W., & Mattu, A. (2017). The Fast and the Furious: Low-Risk Chest Pain and the Rapid Rule-Out Protocol. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 18(3), 474–478. http://accessmedicine.mhmedical.comchamberlainuniversity.idm.oclc.org/content.aspx?bookid=2566§ionid=206884926 Johns Hopkins Medicine. (2019). Chest X-Ray. Retrieved from https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/chest-xray. Mythili, S. & Malathi, N. (2015). Diagnostic markers of acute myocardial infarction. Biomedical reports, 3(6), 743-748. doi: 10.3892/br.2015.500) Nitroglycerin. (2019). In Epocrates Plus for Apple iOS (Version 19.10.1) [Mobile application software]. Retrieved from http:itunes.apple.com Woo, T.M., & Robinson, M.V. (2016). Pharmacotherapeutics for Advanced Practice Nurse Prescribers (4th ed.). Philadelphia, PA: F.A. Davis Company. [Show More]
Last updated: 2 years ago
Preview 1 out of 9 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$10.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jun 07, 2020
Number of pages
9
Written in
Additional information
This document has been written for:
Uploaded
Jun 07, 2020
Downloads
0
Views
86






.png)
.png)
.png)
.png)
.png)
.png)
.png)